Benefits of Applying Nanotechnologies to Hydrogels in Efficacy Tests in Osteoarthritis Models—A Systematic Review of Preclinical Studies
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Data Extraction
2.3. Risk of Bias Assessment
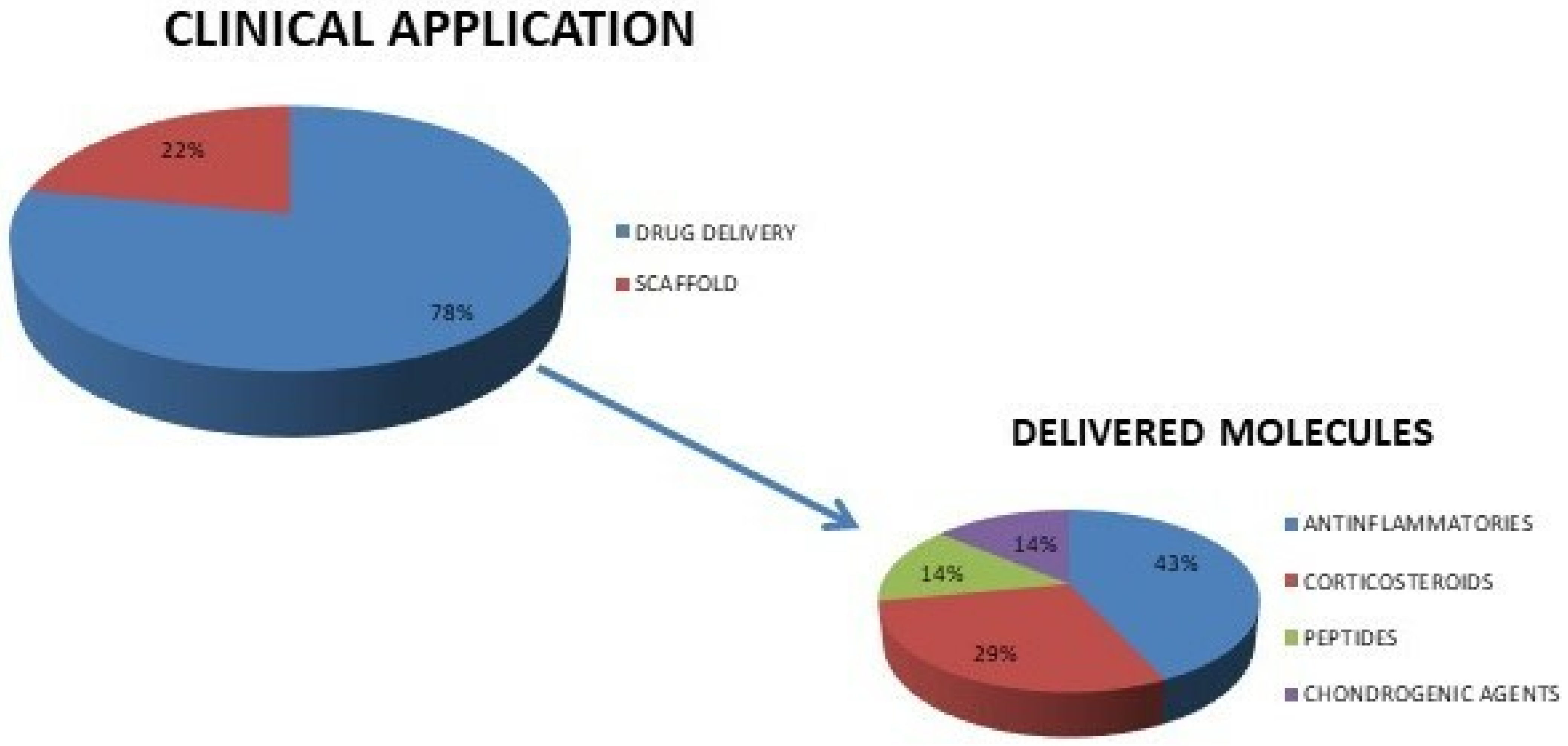
3. Results
3.1. Search Strategy
3.2. In Vitro Preclinical Studies
3.2.1. Hyaluronic Acid Hydrogels
3.2.2. Chitosan Hydrogels
3.2.3. Copolymeric Matrices
3.3. In Vivo Preclinical Studies
3.3.1. Mice
3.3.2. Rats

3.3.3. Risk of Bias Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACLT | Anterior cruciate ligament transection |
| CHI-KGN | Chitosan-kartogenin |
| COLL I | Collagen type I |
| COLL II | Collagen type II |
| COLL X | Collagen type X |
| COX-2 | Cyclooxygenase 2 |
| DBCO | Dibenzocyclooctyne |
| DEX | Dexamethasone |
| DMM | Medial meniscus destabilization |
| ECM | Extracellular matrix |
| EDS | Energy-dispersive X-ray spectroscopy |
| GAG | Glycosaminoglycan |
| HA | Hydroxyapatite |
| hBMMSC | Human bone marrow mesenchymal stem cells |
| HCOAs | Human osteoarthritic chondrocytes |
| Hep/EPL | Heparin/ε-poly-L-lysine |
| i.a. | Intra-articular |
| IL-1β | Interleukin 1β |
| IL-6 | Interleukin 6 |
| IVIS | In vivo imaging |
| KGN | Kartogenin |
| MIA | Monoiodoacetate |
| Micro-CT | Micro-computed tomography |
| MMP-13 | Matrix metallopeptidase 13 |
| MSCs | Mesenchymal stem cells |
| MSNs | Mesoporous silica nanoparticles |
| MMT | Medial meniscal transection |
| NPs | Nanoparticles |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| PBS | Phosphate buffered saline |
| PEGDA | Poly (ethylene glycol) diacrylate |
| PLA | Poly(D,L)-lactide |
| PLGA | Poly(lactic-coglycolic) acid |
| pNiPAM | poly(N-isopropylacrylamide) |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PTOA | Post-traumatic osteoarthritis |
| OA | Osteoarthritis |
| OARSI | Osteoarthritis Research Society International |
| RT-PCR | Real-time polymerase chain reaction |
| RUNX2 | Runt-related transcription factor 2 |
| SYRCLE | Systematic Review Centre for Laboratory Animal Experimentation |
| SOX9 | SRY-box transcription factor 9 |
| TCA | triamcinolone acetonide |
| TePNs | TCA-encapsulated polymeric nanoparticles |
| TNF-α | Tumor necrosis factor α |
| VEGF | Vascular endothelial growth factor |
References
- Fuggle, N.R.; Cooper, C.; Oreffo, R.O.C.; Price, A.J.; Kaux, J.F.; Maheu, E.; Cutolo, M.; Honvo, G.; Conaghan, P.G.; Berenbaum, F.; et al. Alternative and Complementary Therapies in Osteoarthritis and Cartilage Repair. Aging Clin. Exp. Res. 2020, 32, 547–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puig-Junoy, J.; Ruiz Zamora, A. Socio-Economic Costs of Osteoarthritis: A Systematic Review of Cost-of-Illness Studies. Semin. Arthritis Rheum. 2015, 44, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Osteoarthritis Is a Serious Disease. Available online: https://www.clinexprheumatol.org/abstract.asp?a=14780 (accessed on 10 May 2022).
- Colombo, G.L.; Heiman, F.; Peduto, I. Utilization of Healthcare Resources in Osteoarthritis: A Cost of Illness Analysis Based on Real-World Data in Italy. Ther. Clin. Risk Manag. 2021, 17, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Salmon, J.H.; Rat, A.C.; Achit, H.; Ngueyon-Sime, W.; Gard, C.; Guillemin, F.; Jolly, D.; Fautrel, B. Health Resource Use and Costs of Symptomatic Knee and/or Hip Osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1011–1017. [Google Scholar] [CrossRef]
- Allen, K.D.; Thoma, L.M.; Golightly, Y.M. Epidemiology of Osteoarthritis. Osteoarthr. Cartil. 2022, 30, 184–195. [Google Scholar] [CrossRef] [PubMed]
- Palazzo, C.; Nguyen, C.; Lefevre-Colau, M.-M.; Rannou, F.; Poiraudeau, S. Risk Factors and Burden of Osteoarthritis. Ann. Phys. Rehabil. Med. 2016, 59, 134–138. [Google Scholar] [CrossRef]
- Tschon, M.; Contartese, D.; Pagani, S.; Borsari, V.; Fini, M. Gender and Sex Are Key Determinants in Osteoarthritis Not Only Confounding Variables. A Systematic Review of Clinical Data. J. Clin. Med. 2021, 10, 3178. [Google Scholar] [CrossRef]
- Contartese, D.; Tschon, M.; De Mattei, M.; Fini, M. Sex Specific Determinants in Osteoarthritis: A Systematic Review of Preclinical Studies. Int. J. Mol. Sci. 2020, 21, 3696. [Google Scholar] [CrossRef]
- Peck, J.; Slovek, A.; Miro, P.; Vij, N.; Traube, B.; Lee, C.; Berger, A.A.; Kassem, H.; Kaye, A.D.; Sherman, W.F.; et al. A Comprehensive Review of Viscosupplementation in Osteoarthritis of the Knee. Orthop. Rev. 2021, 13, 25549. [Google Scholar] [CrossRef]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and Treatment of Hip and Knee Osteoarthritis: A Review. JAMA 2021, 325, 568. [Google Scholar] [CrossRef]
- Bannuru, R.R.; Osani, M.C.; Vaysbrot, E.E.; Arden, N.K.; Bennell, K.; Bierma-Zeinstra, S.M.A.; Kraus, V.B.; Lohmander, L.S.; Abbott, J.H.; Bhandari, M.; et al. OARSI Guidelines for the Non-Surgical Management of Knee, Hip, and Polyarticular Osteoarthritis. Osteoarthr. Cartil. 2019, 27, 1578–1589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mou, D.; Yu, Q.; Zhang, J.; Zhou, J.; Li, X.; Zhuang, W.; Yang, X. Intra-Articular Injection of Chitosan-Based Supramolecular Hydrogel for Osteoarthritis Treatment. Tissue Eng. Regen. Med. 2021, 18, 113–125. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Wang, B.; Hu, C.; Zhao, J. An Overview of Hydrogel-Based Intra-Articular Drug Delivery for the Treatment of Osteoarthritis. Colloids Surf. B Biointerfaces 2017, 154, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Salamanna, F.; Giavaresi, G.; Parrilli, A.; Martini, L.; Nicoli Aldini, N.; Abatangelo, G.; Frizziero, A.; Fini, M. Effects of Intra-articular Hyaluronic Acid Associated to Chitlac (Arty-duo®) in a Rat Knee Osteoarthritis Model. J. Orthop. Res. 2019, 37, 867–876. [Google Scholar] [CrossRef]
- Affatato, S.; Trucco, D.; Taddei, P.; Vannozzi, L.; Ricotti, L.; Nessim, G.; Lisignoli, G. Wear Behavior Characterization of Hydrogels Constructs for Cartilage Tissue Replacement. Materials 2021, 14, 428. [Google Scholar] [CrossRef]
- Øvrebø, Ø.; Perale, G.; Wojciechowski, J.P.; Echalier, C.; Jeffers, J.R.T.; Stevens, M.M.; Haugen, H.J.; Rossi, F. Design and Clinical Application of Injectable Hydrogels for Musculoskeletal Therapy. Bioeng. Transl. Med. 2022, 7, e10295. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Qiu, Y.; Qu, L.; Wang, Q.; Zhou, Q. Hydrogels for Treatment of Different Degrees of Osteoarthritis. Front. Bioeng. Biotechnol. 2022, 10, 858656. [Google Scholar] [CrossRef]
- Trucco, D.; Sharma, A.; Manferdini, C.; Gabusi, E.; Petretta, M.; Desando, G.; Ricotti, L.; Chakraborty, J.; Ghosh, S.; Lisignoli, G. Modeling and Fabrication of Silk Fibroin–Gelatin-Based Constructs Using Extrusion-Based Three-Dimensional Bioprinting. ACS Biomater. Sci. Eng. 2021, 7, 3306–3320. [Google Scholar] [CrossRef]
- Di Francesco, M.; Fragassi, A.; Pannuzzo, M.; Ferreira, M.; Brahmachari, S.; Decuzzi, P. Management of Osteoarthritis: From Drug Molecules to Nano/micromedicines. WIREs Nanomed. Nanobiotechnol. 2022, 14, e1780. [Google Scholar] [CrossRef] [PubMed]
- Nabizadeh, Z.; Nasrollahzadeh, M.; Daemi, H.; Eslaminejad, M.B.; Shabani, A.A.; Dadashpour, M.; Mirmohammadkhani, M.; Nasrabadi, D. Micro- and Nanotechnology in Biomedical Engineering for Cartilage Tissue Regeneration in Osteoarthritis. Beilstein J. Nanotechnol. 2022, 13, 363–389. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Lou, J.; Wang, F.; Fan, D.; Qin, Z. Recent Advances in Nano-Therapeutic Strategies for Osteoarthritis. Front. Pharmacol. 2022, 13, 924387. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, S.; Wang, K.; Wu, X.; Tu, C.; Gao, C. Stimuli-Sensitive Nanotherapies for the Treatment of Osteoarthritis. Macromol. Biosci. 2021, 21, 2100280. [Google Scholar] [CrossRef]
- Farokhzad, O.C.; Langer, R. Impact of Nanotechnology on Drug Delivery. ACS Nano 2009, 3, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Zhang, Y.; Zhang, Q.; Zhang, L. Nanoparticle-Hydrogel: A Hybrid Biomaterial System for Localized Drug Delivery. Ann. Biomed. Eng. 2016, 44, 2049–2061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, Y.; Xu, X.; Xu, L.; Prasadam, I.; Duan, L.; Xiao, Y.; Xia, J. Non-Surgical Osteoarthritis Therapy, Intra-Articular Drug Delivery towards Clinical Applications. J. Drug Target. 2021, 29, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Trucco, D.; Vannozzi, L.; Teblum, E.; Telkhozhayeva, M.; Nessim, G.D.; Affatato, S.; Al-Haddad, H.; Lisignoli, G.; Ricotti, L. Graphene Oxide-Doped Gellan Gum–PEGDA Bilayered Hydrogel Mimicking the Mechanical and Lubrication Properties of Articular Cartilage. Adv. Healthc. Mater. 2021, 10, 2001434. [Google Scholar] [CrossRef] [PubMed]
- Im, G.-I. Perspective on Intra-Articular Injection Cell Therapy for Osteoarthritis Treatment. Tissue Eng. Regen. Med. 2019, 16, 357–363. [Google Scholar] [CrossRef]
- Hooijmans, C.R.; Rovers, M.M.; de Vries, R.B.; Leenaars, M.; Ritskes-Hoitinga, M.; Langendam, M.W. SYRCLE’s Risk of Bias Tool for Animal Studies. BMC Med. Res. Methodol. 2014, 14, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pradal, J.; Maudens, P.; Gabay, C.; Seemayer, C.A.; Jordan, O.; Allémann, E. Effect of Particle Size on the Biodistribution of Nano- and Microparticles Following Intra-Articular Injection in Mice. Int. J. Pharm. 2016, 498, 119–129. [Google Scholar] [CrossRef] [PubMed]
- Maudens, P.; Meyer, S.; Seemayer, C.A.; Jordan, O.; Allémann, E. Self-Assembled Thermoresponsive Nanostructures of Hyaluronic Acid Conjugates for Osteoarthritis Therapy. Nanoscale 2018, 10, 1845–1854. [Google Scholar] [CrossRef] [Green Version]
- Kang, M.L.; Ko, J.-Y.; Kim, J.E.; Im, G.-I. Intra-Articular Delivery of Kartogenin-Conjugated Chitosan Nano/Microparticles for Cartilage Regeneration. Biomaterials 2014, 35, 9984–9994. [Google Scholar] [CrossRef] [PubMed]
- Dua, R.; Comella, K.; Butler, R.; Castellanos, G.; Brazille, B.; Claude, A.; Agarwal, A.; Liao, J.; Ramaswamy, S. Integration of Stem Cell to Chondrocyte-Derived Cartilage Matrix in Healthy and Osteoarthritic States in the Presence of Hydroxyapatite Nanoparticles. PLoS ONE 2016, 11, e0149121. [Google Scholar] [CrossRef] [PubMed]
- Karliana, D.; Anwar, E.; Bahtiar, A. Formulation and Evaluation of Quercetin Nanoparticle Gel for Osteoarthritis. Int. J. App. Pharm. 2019, 11, 54–59. [Google Scholar] [CrossRef]
- Permatasari, D.; Karliana, D.; Iskandarsyah, I.; Arsianti, A.; Bahtiar, A. Quercetin Prevent Proteoglycan Destruction by Inhibits Matrix Metalloproteinase-9, Matrix Metalloproteinase-13, a Disintegrin and Metalloproteinase with Thrombospondin Motifs-5 Expressions on Osteoarthritis Model Rats. J. Adv. Pharm. Technol. Res. 2019, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, A.L.; Elmotasem, H.; Salama, A.A.A. Colchicine Mesoporous Silica Nanoparticles/Hydrogel Composite Loaded Cotton Patches as a New Encapsulator System for Transdermal Osteoarthritis Management. Int. J. Biol. Macromol. 2020, 164, 1149–1163. [Google Scholar] [CrossRef] [PubMed]
- Mancipe Castro, L.M.; Sequeira, A.; García, A.J.; Guldberg, R.E. Articular Cartilage- and Synoviocyte-Binding Poly(Ethylene Glycol) Nanocomposite Microgels as Intra-Articular Drug Delivery Vehicles for the Treatment of Osteoarthritis. ACS Biomater. Sci. Eng. 2020, 6, 5084–5095. [Google Scholar] [CrossRef]
- Holyoak, D.T.; Wheeler, T.A.; van der Meulen, M.C.H.; Singh, A. Injectable Mechanical Pillows for Attenuation of Load-Induced Post-Traumatic Osteoarthritis. Regen. Biomater. 2019, 6, 211–219. [Google Scholar] [CrossRef]
- Tang, Q.; Lim, T.; Shen, L.-Y.; Zheng, G.; Wei, X.-J.; Zhang, C.-Q.; Zhu, Z.-Z. Well-Dispersed Platelet Lysate Entrapped Nanoparticles Incorporate with Injectable PDLLA-PEG-PDLLA Triblock for Preferable Cartilage Engineering Application. Biomaterials 2021, 268, 120605. [Google Scholar] [CrossRef] [PubMed]
- Seo, B.-B.; Kwon, Y.; Kim, J.; Hong, K.H.; Kim, S.-E.; Song, H.-R.; Kim, Y.-M.; Song, S.-C. Injectable Polymeric Nanoparticle Hydrogel System for Long-Term Anti-Inflammatory Effect to Treat Osteoarthritis. Bioact. Mater. 2022, 7, 14–25. [Google Scholar] [CrossRef]
- Zhao, T.; Wei, Z.; Zhu, W.; Weng, X. Recent Developments and Current Applications of Hydrogels in Osteoarthritis. Bioengineering 2022, 9, 132. [Google Scholar] [CrossRef] [PubMed]
- Tarricone, E.; Mattiuzzo, E.; Belluzzi, E.; Elia, R.; Benetti, A.; Venerando, R.; Vindigni, V.; Ruggieri, P.; Brun, P. Anti-Inflammatory Performance of Lactose-Modified Chitosan and Hyaluronic Acid Mixtures in an In Vitro Macrophage-Mediated Inflammation Osteoarthritis Model. Cells 2020, 9, 1328. [Google Scholar] [CrossRef] [PubMed]
- Ummarino, A.; Gambaro, F.M.; Kon, E.; Torres Andón, F. Therapeutic Manipulation of Macrophages Using Nanotechnological Approaches for the Treatment of Osteoarthritis. Nanomaterials 2020, 10, 1562. [Google Scholar] [CrossRef]
- Fini, M.; Salamanna, F.; Veronesi, F.; Torricelli, P.; Nicolini, A.; Benedicenti, S.; Carpi, A.; Giavaresi, G. Role of Obesity, Alcohol and Smoking on Bone Health. Front. Biosci. (Elite Ed) 2012, 4, 2586–2606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fini, M.; Giavaresi, G.; Salamanna, F.; Veronesi, F.; Martini, L.; De Mattei, M.; Tschon, M. Harmful Lifestyles on Orthopedic Implantation Surgery: A Descriptive Review on Alcohol and Tobacco Use. J. Bone Miner. Metab. 2011, 29, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Pagani, S.; Borsari, V.; Veronesi, F.; Ferrari, A.; Cepollaro, S.; Torricelli, P.; Filardo, G.; Fini, M. Increased Chondrogenic Potential of Mesenchymal Cells from Adipose Tissue Versus Bone Marrow-Derived Cells in Osteoarthritic In Vitro Models. J. Cell. Physiol. 2017, 232, 1478–1488. [Google Scholar] [CrossRef] [PubMed]
- Pagani, S.; Veronesi, F.; Giavaresi, G.; Filardo, G.; Papio, T.; Romandini, I.; Fini, M. Autologous Protein Solution Effect on Chondrogenic Differentiation of Mesenchymal Stem Cells from Adipose Tissue and Bone Marrow in an Osteoarthritic Environment. Cartilage 2021, 13, 225S–237S. [Google Scholar] [CrossRef] [PubMed]
- Singh, Y.P.; Moses, J.C.; Bhardwaj, N.; Mandal, B.B. Overcoming the Dependence on Animal Models for Osteoarthritis Therapeutics—The Promises and Prospects of In Vitro Models. Adv. Healthc. Mater. 2021, 10, 2100961. [Google Scholar] [CrossRef]
- Samvelyan, H.J.; Hughes, D.; Stevens, C.; Staines, K.A. Models of Osteoarthritis: Relevance and New Insights. Calcif. Tissue Int. 2021, 109, 243–256. [Google Scholar] [CrossRef] [Green Version]
- Im, G.-I. Application of Kartogenin for Musculoskeletal Regeneration: Application of Kartogenin for Musculoskeletal Regeneration. J. Biomed. Mater. Res. 2018, 106, 1141–1148. [Google Scholar] [CrossRef]
- Cai, G.; Liu, W.; He, Y.; Huang, J.; Duan, L.; Xiong, J.; Liu, L.; Wang, D. Recent Advances in Kartogenin for Cartilage Regeneration. J. Drug Target. 2019, 27, 28–32. [Google Scholar] [CrossRef]
- Guan, F.; Wang, Q.; Bao, Y.; Chao, Y. Anti-Rheumatic Effect of Quercetin and Recent Developments in Nano Formulation. RSC Adv. 2021, 11, 7280–7293. [Google Scholar] [CrossRef] [PubMed]
- Leung, Y.Y.; Hui, L.L.Y.; Kraus, V.B. Colchicine—Update on Mechanisms of Action and Therapeutic Uses. Semin. Arthritis Rheum. 2015, 45, 341–350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laverty, S.; Girard, C.A.; Williams, J.M.; Hunziker, E.B.; Pritzker, K.P.H. The OARSI Histopathology Initiative—Recommendations for Histological Assessments of Osteoarthritis in the Rabbit. Osteoarthr. Cartil. 2010, 18, S53–S65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, C.B.; Smith, M.M.; Cake, M.A.; Read, R.A.; Murphy, M.J.; Barry, F.P. The OARSI Histopathology Initiative—Recommendations for Histological Assessments of Osteoarthritis in Sheep and Goats. Osteoarthr. Cartil. 2010, 18, S80–S92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peshkova, M.; Lychagin, A.; Lipina, M.; Di Matteo, B.; Anzillotti, G.; Ronzoni, F.; Kosheleva, N.; Shpichka, A.; Royuk, V.; Fomin, V.; et al. Gender-Related Aspects in Osteoarthritis Development and Progression: A Review. Int. J. Mol. Sci. 2022, 23, 2767. [Google Scholar] [CrossRef]
- Laitner, M.H.; Erickson, L.C.; Society for Women’s Health Research Osteoarthritis and Chronic Pain Working Group; Ortman, E. Understanding the Impact of Sex and Gender in Osteoarthritis: Assessing Research Gaps and Unmet Needs. J. Women’s Health 2021, 30, 634–641. [Google Scholar] [CrossRef]
- Kriegova, E.; Manukyan, G.; Mikulkova, Z.; Gabcova, G.; Kudelka, M.; Gajdos, P.; Gallo, J. Gender-Related Differences Observed among Immune Cells in Synovial Fluid in Knee Osteoarthritis. Osteoarthr. Cartil. 2018, 26, 1247–1256. [Google Scholar] [CrossRef] [Green Version]
- Mohammadpour, R.; Yazdimamaghani, M.; Cheney, D.L.; Jedrzkiewicz, J.; Ghandehari, H. Subchronic Toxicity of Silica Nanoparticles as a Function of Size and Porosity. J. Control. Release 2019, 304, 216–232. [Google Scholar] [CrossRef]
- Mohammadpour, R.; Dobrovolskaia, M.A.; Cheney, D.L.; Greish, K.F.; Ghandehari, H. Subchronic and Chronic Toxicity Evaluation of Inorganic Nanoparticles for Delivery Applications. Adv. Drug Deliv. Rev. 2019, 144, 112–132. [Google Scholar] [CrossRef] [PubMed]
- Van der Kraan, P.M. Factors That Influence Outcome in Experimental Osteoarthritis. Osteoarthr. Cartil. 2017, 25, 369–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Temp, J.; Labuz, D.; Negrete, R.; Sunkara, V.; Machelska, H. Pain and Knee Damage in Male and Female Mice in the Medial Meniscal Transection-Induced Osteoarthritis. Osteoarthr. Cartil. 2020, 28, 475–485. [Google Scholar] [CrossRef]
- Loga, I.S.; Batchelor, V.; Driscoll, C.; Burleigh, A.; Chia, S.L.; Stott, B.; Miotla-Zarebska, J.; Riley, D.; Dell’Accio, F.; Vincent, T.L. Does Pain at an Earlier Stage of Chondropathy Protect Female Mice Against Structural Progression After Surgically Induced Osteoarthritis? Arthritis Rheumatol. 2020, 72, 2083–2093. [Google Scholar] [CrossRef]
- Ro, J.Y.; Zhang, Y.; Tricou, C.; Yang, D.; da Silva, J.T.; Zhang, R. Age and Sex Differences in Acute and Osteoarthritis-Like Pain Responses in Rats. J. Gerontol. Ser. A 2020, 75, 1465–1472. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, R.C. Bioethics and Animal Use in Programs of Research, Teaching, and Testing. In Management of Animal Care and Use Programs in Research, Education, and Testing; Weichbrod, R.H., Thompson, G.A., Norton, J.N., Eds.; CRC Press: Boca Raton, FL, USA; Taylor & Francis: Abingdon, UK, 2018; ISBN 978-149-874-844-5. [Google Scholar]
- Russell, W.M.S.; Burch, R.L. The Principles of Humane Experimental Technique; Methuen: London, UK, 1959. [Google Scholar]
- Altman, R.; Hochberg, M.; Gibofsky, A.; Jaros, M.; Young, C. Efficacy and Safety of Low-Dose SoluMatrix Meloxicam in the Treatment of Osteoarthritis Pain: A 12-Week, Phase 3 Study. Curr. Med. Res. Opin. 2015, 31, 2331–2343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altman, R.D.; Strand, V.; Hochberg, M.C.; Gibofsky, A.; Markenson, J.A.; Hopkins, W.E.; Cryer, B.; Kivitz, A.; Nezzer, J.; Imasogie, O.; et al. Low-Dose SoluMatrix Diclofenac in the Treatment of Osteoarthritis: A 1-Year, Open-Label, Phase III Safety Study. Postgrad. Med. 2015, 127, 517–528. [Google Scholar] [CrossRef]
- Argoff, C.; McCarberg, B.; Gudin, J.; Nalamachu, S.; Young, C. SoluMatrix® Diclofenac: Sustained Opioid-Sparing Effects in a Phase 3 Study in Patients with Postoperative Pain. Pain Med. 2016, 17, 1933–1941. [Google Scholar] [CrossRef] [Green Version]
- Strand, V.; Bergman, M.; Singh, J.A.; Gibofsky, A.; Kivitz, A.; Young, C. Low-Dose SoluMatrix Diclofenac in Patients with Osteoarthritis Pain: Impact on Quality of Life in a Controlled Trial. Clin. Rheumatol. 2017, 36, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- Gibofsky, A.; Altman, R.; Daniels, S.; Imasogie, O.; Young, C. Low-Dose SoluMatrix Diclofenac: A Review of Safety across Two Phase III Studies in Patients with Acute and Osteoarthritis Pain. Expert Opin. Drug Saf. 2015, 14, 1327–1339. [Google Scholar] [CrossRef] [PubMed]
- Gibofsky, A.; Hochberg, M.C.; Jaros, M.J.; Young, C.L. Efficacy and Safety of Low-Dose Submicron Diclofenac for the Treatment of Osteoarthritis Pain: A 12 Week, Phase 3 Study. Curr. Med. Res. Opin. 2014, 30, 1883–1893. [Google Scholar] [CrossRef]
- Gibofsky, A.; Silberstein, S.; Argoff, C.; Daniels, S.; Jensen, S.; Young, C.L. Lower-Dose Diclofenac Submicron Particle Capsules Provide Early and Sustained Acute Patient Pain Relief in a Phase 3 Study. Postgrad. Med. 2013, 125, 130–138. [Google Scholar] [CrossRef]
- Hussaini, A.; Solorio, D.; Young, C. Pharmacokinetic Properties of Low-Dose SoluMatrix Meloxicam in Healthy Adults. Clin. Rheumatol. 2016, 35, 1099–1104. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.; Eskandar, N.G.; Rao, S.; Prestidge, C.A. First in Man Bioavailability and Tolerability Studies of a Silica–Lipid Hybrid (Lipoceramic) Formulation: A Phase I Study with Ibuprofen. Drug Deliv. Transl. Res. 2014, 4, 212–221. [Google Scholar] [CrossRef] [PubMed]



| Hydrogel Nanoparticles System | Clinical Application | Cell Phenotype | Cell Source | Experimental Analyses (Experimental Times) | Main Findings | Ref. |
|---|---|---|---|---|---|---|
| Chitosan-kartogenin NPs (size 150 ± 39 nm, spherical) | Drug delivery (kartogenin) | hBMMSCs from bone marrow cultured in pellets (passages 3–5) and chondrocytes from articular cartilage (passage 3) | hBMMSCs: 3 patients undergoing hip prosthesis (age range: 54–72 years); chondrocytes: 3 patients undergoing knee arthroplasties (age range: 59–65 years) | hBMMSCs: DNA, GAG measure, and RT-PCR for COLL I, COLL II, COLL X, aggrecan (28 days), and histology (21 days); chondrocytes: MTT and IL-6 release (7 days) | hBMMSCs: no differences in DNA quantity, COLL I, and COLL X expression; increase in GAG contents, COLL II, and aggrecan; Safranin-O/Alcian Blue staining; chondrocytes: normal cell proliferation and no increase in IL-6 after treatment | Kang 2014 [32] |
| PLA nanoparticles (size 300 nm) in 0.6% hyaluronic acid | Drug delivery (DiD fluorescent stain) | Human synovial fibroblasts (below passage 10) | 1 patient undergoing joint replacement (76 years) | Cell viability: MTT (24 h) | No reduction in cell viability after treatment | Pradal 2016 [30] |
| Hyaluronic acid nanoparticles (size 203–261 nm) 1% and 0.5% in hyaluronic acid-DBCO linker-pNiPAM | Scaffold | Human synovial fibroblasts isolated from synovial tissue (passage 8) | Synovial fibroblasts from 1 OA patient | Cell viability: MTT (24 h) | No reduction in cell viability after treatment | Maudens 2017 [31] |
| HA NPsin two-layer constructs: HCOAs in agar gel, hBMMSCs in PEGDA | Scaffold | HCOAs from cell applications (passage 4), hBMMSCs from Science Cell, Carlsbad, CA (passage 3) | Cells commercially available from OA patients | Cell viability: live and dead assay (1, 7, 14, and 28 days); mechanical testing: shear strength; histology and EDS: Von-Kossa and Alcian Blue stains (1 and 28 days); RT-PCR for aggrecan, SOX9, COLL II, MMP-13, RUNX2, COLL X, COLL I, and osteocalcin (after 28 days of culture) | Cell viability: ~86% viability of the HCOAs after 28 days; mechanical testing: higher shear strength in the NPs-gel system; histology and EDS: formation of a thin transition zone made of calcium and phosphorus; RT-PCR: lower expression of COLL I; maintaining expression of aggrecan, SOX9, and COLL II; no expression of MMP-13, RUNX2, and COLL X | Dua 2016 [33] |
| Hydrogel Nanoparticles System | Clinical Application | Animal Model of OA (Number, Sex and Strain) | Administration Route and Timing of Delivery | Experimental Analyses | Main Findings | Experimental Times | Ref. |
|---|---|---|---|---|---|---|---|
| Quercetin NPs (size 212–242 nm, spherical) in chitosan | Drug delivery (3 doses of quercetin) | DMM and 3 mg/0.05 mL MIA in rats (5 male Sprague-Dawley rats for each group) | Topical application for 42 consecutive days | Edema volume measurements | MIA model: at day 14, significant differences using the higher dose of quercetin; DMM model: at day 42, significant differences using the higher dose of quercetin | 7, 14, 21, 28, 35, 42, 49, 56, 63 and 70 days after OA induction | Karliana 2019 [34] |
| PLGA NPs (size 338 ± 91 nm) in PEG-4MAL macromer reacted with cartilage-(WYR), synoviocyte-(HAP-1), or integrin-(RGD) binding peptides | Drug delivery (cartilage-(WYR), synoviocyte-(HAP-1), or integrin-(RGD) binding peptides) | Unilateral MMT in rats (9 male Lewis rats for each group) | i.a injections 21 days after MMT | IVIS; micro-CT (volume, roughness and osteophyte volume); histology; in vivo localization of NP-gels | IVIS: NP-gel system increased in vivo intra-articular retention; micro-CT: WYR- and HAP-1 gels did not affect cartilage and OA progression; histology: no cartilage damage and synovial membrane thickening; in vivo localization: gel accumulation in the synovial membrane | IVIS: before and after 1, 3, 5, 7, 10, 13, 16, 19, and 26 days post-treatment; micro-CT: day 26; histology: at days 14 and 26 | Mancipe Castro 2020 [37] |
| Chitosan-kartogenin NPs (size 150 ± 39 nm, spherical) | Drug delivery (kartogenin) | Bilateral ACLT in rats (8 male Sprague Dawley rats for each group) | Two i.a. applications after 42 and 63 days after ACLT | In vivo retention time; histology (OARSI score) | In vivo retention time: NPs showed long retention in the OA joint; histology: lower OARSI score in treated joints | In vivo retention time: 2, 4, 7, 14, and 24 days after treatment; histology: 35 days post-treatment | Kang 2014 [32] |
| Quercetin NPs (size 212.2 nm, spherical) in lecithin-chitosan | Drug delivery (3 doses of quercetin) | DMM and 3 mg/0.05 mL MIA in rats (5 male Sprague-Dawley rats for each group) | Topical application for 42 consecutive days | Histology; immunoenzymatic assays on blood (IL-1β, MMP-9, MMP-13, and ADAMTS5) | Improved histology; immunoenzymatic assays: all doses decreased IL-1β, MMP-9, MMP-13, and ADAMTS5 levels | Histology and immunoenzymatic assays on blood: 42 days after treatment | Permatasari 2019 [35] |
| DEX-loaded PLGA NPs (size 203 ± 7 nm) in PEG-4MAL macromers | Drug delivery (DEX) and mechanical pillow function | PTOA in mice by daily cyclic loading compression (9 N) on tibia for 42 days (5 male C57BL/6 mice for each group) | i.a. injections 48 h after compression | Histology (OARSI score, osteophyte dimensions) | NP-gel attenuated load-induced cartilage damage and osteophyte size | 14 days after treatment | Holyoak 2019 [38] |
| Colchicine-loaded MSNs (size 167.1 ± 51.36 nm, spherical) in carboxyethyl chitosan and oxidized pullulan | Drug delivery (colchicine) | Unilateral 3 mg/joint MIA in rats (8 male Wister albino rats for each group) | Daily topical application of transdermal patches for 21 days (drug dose: 5 mg/kg/day) | Locomotor activity; immunoenzymatic assays on blood (TNF-α and COX-2); histology | Locomotor activity: NP-gel increased locomotor activity; immunoenzymatic assays: NP-gel reduced serum level of TNF-α and COX-2; histology: protective effects of NP-gel | Locomotor activity: 7 days before experiments; immunoenzymatic assays and histopathology: 21 days after MIA | Mohamed 2020 [36] |
| Hep/EPL NPs (size 387.81 ± 65.16 nm) dispersed in human PL and encapsulated in thermosensitive PLEL hydrogel | Scaffold | Bilateral ACLT in rats (4 Sprague-Dawley rats for each group) | Single i.a. injection | Histology and immunostaining (COLL II, MMP-13, and CD68, Mankin and synovitis scores) | Histology and immunostaining: NP-gel showed lower Mankin scores and better synovitis; immunostaining: treatment with NP-gel inhibited ECM degradation and prevented collagen loss | 56 days after ACLT | Tang 2021 [39] |
| Poly (organosphosphazenes) NPs (size 140 ± 5 nm) encapsulated in polymeric hydrogel system | Drug delivery (3 doses of TCA) | 0.5 mg/50 μL MIA in rats (6 male Sprague Dawley rats for each group) | i.a. injections of 0.3 mL, TePN solutions 7 days after OA induction | X-ray; microCT (distance of destroyed cartilages); histology; RT-PCR on blood (MMP-3, MMP-13, IL-6, TNF-α, IL-4, IL-10, and IL-13) | X-ray, histology, and micro-CT: NP-gel showed significant improvement in anti-OA effects; RT PCR: decrease in MMP-3, MMP-13, IL-6, and TNF-α levels, increase in IL-4, IL-10, and IL-13, in NP-gel | X-ray, micro-CT. and histology: 56 days after treatment; RT PCR: at days 7, 28, and 56 | Seo 2021 [40] |
| HA nano (size 203–261, 377–435 by SEM) in DBCO linker-pNiPAM | Visco-supplementation | Unilateral DMM in mice (6-week-old male C57BL/6 mice, 7 for each group) | i.a. injections on days 7 and 35 after OA surgery | Intravital fluorescence and microscopic fluorescence; micro-CT (for medial/lateral tibial epiphysis thickness); histology (OARSI score); iImmunoenzymatic assays on blood (IL-1β, TNF-α, and VEGF) | Intravital and microscopic fluorescence: the residence time of HA nano exceeded 21 days near the injection site; micro-CT: NP-gel induced higher epiphysis thickness; histology: improved OARSI; immunoenzymatic assays on blood: NP-gel inhibited VEGF and reduced IL-1β and TNF-α | Histology, micro-CT, microscopic fluorescence, and blood analyses: day 63 after OA induction; intravital fluorescence: at days 0, 1, 7, and 21 after i.a. treatment | Maudens 2017 [31] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delbaldo, C.; Tschon, M.; Martini, L.; Fini, M.; Codispoti, G. Benefits of Applying Nanotechnologies to Hydrogels in Efficacy Tests in Osteoarthritis Models—A Systematic Review of Preclinical Studies. Int. J. Mol. Sci. 2022, 23, 8236. https://doi.org/10.3390/ijms23158236
Delbaldo C, Tschon M, Martini L, Fini M, Codispoti G. Benefits of Applying Nanotechnologies to Hydrogels in Efficacy Tests in Osteoarthritis Models—A Systematic Review of Preclinical Studies. International Journal of Molecular Sciences. 2022; 23(15):8236. https://doi.org/10.3390/ijms23158236
Chicago/Turabian StyleDelbaldo, Chiara, Matilde Tschon, Lucia Martini, Milena Fini, and Giorgia Codispoti. 2022. "Benefits of Applying Nanotechnologies to Hydrogels in Efficacy Tests in Osteoarthritis Models—A Systematic Review of Preclinical Studies" International Journal of Molecular Sciences 23, no. 15: 8236. https://doi.org/10.3390/ijms23158236






