A Genetically Engineered Bivalent Vaccine Coexpressing a Molecular Adjuvant against Classical Swine Fever and Porcine Epidemic Diarrhea
Abstract
:1. Introduction
2. Results
2.1. Amino Acid Substitution D136N in Npro of CSFV C-Strain Inhibited IRF3 Degradation and Upregulated VISA-Mediated IFN-β Induction
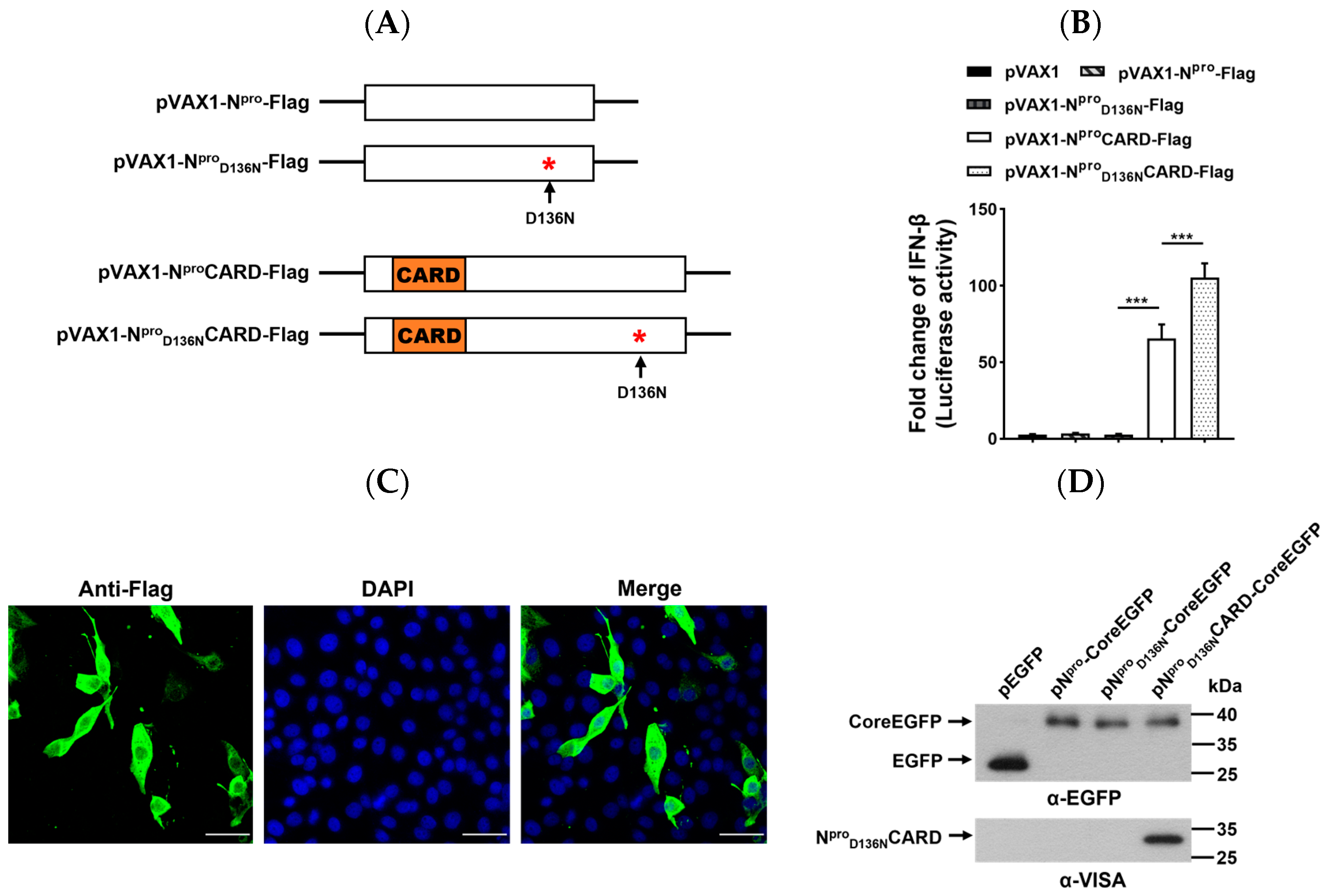
2.2. Expression of Npro or Its Variant Fused with CARD Domain of VISA and Activation of the IFN-β Promoter
2.3. Generation and Identification of Recombinant CSFVs Expressing CARD and S1NCOE Peptides
2.4. Characterization of Recombinant CSFVs Expressing CARD and S1NCOE Peptides
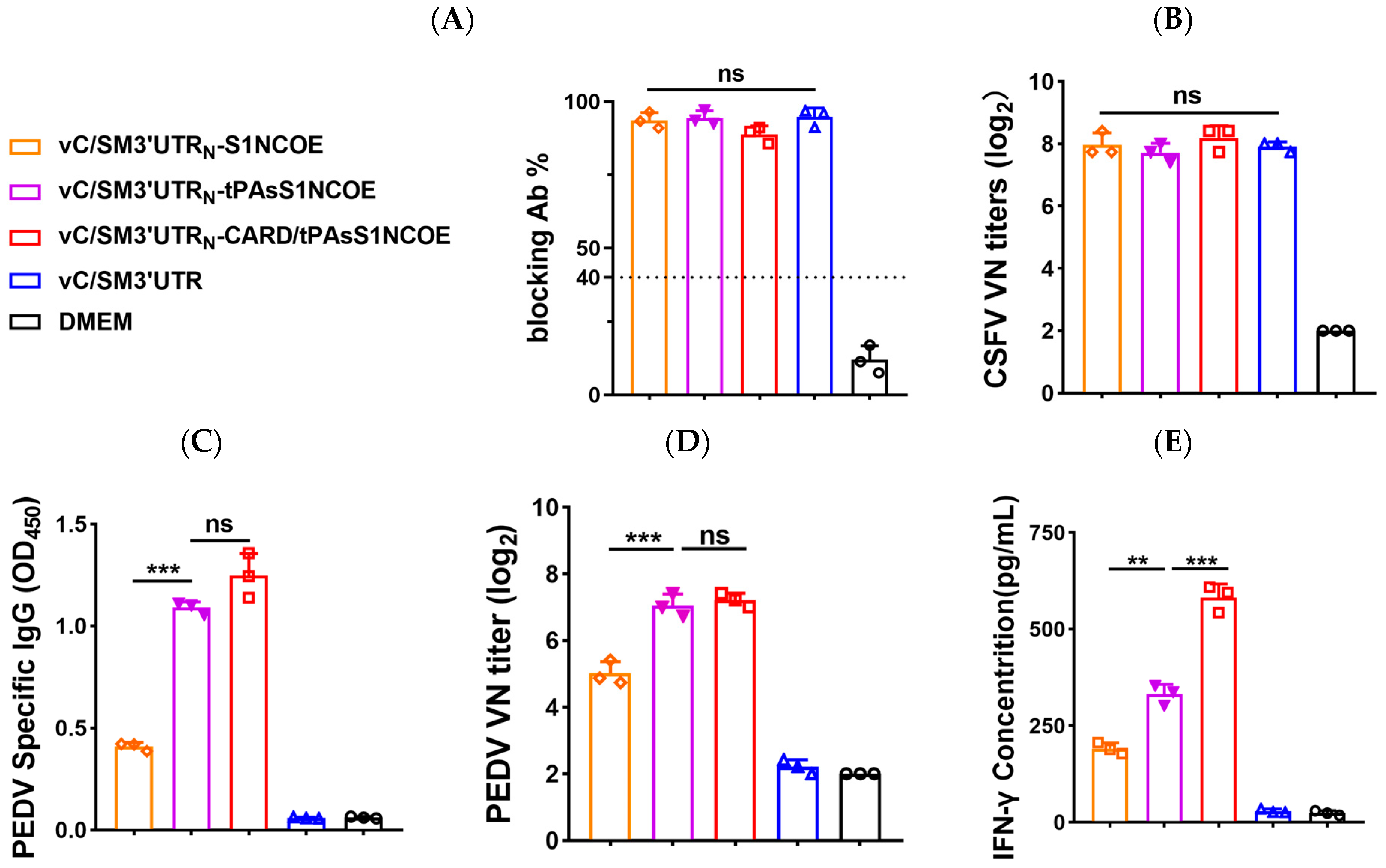
2.5. Humoral Responses and PEDV-Specific IFN-γ Production Induced by the Recombinant CSFVs in Experimental Animals
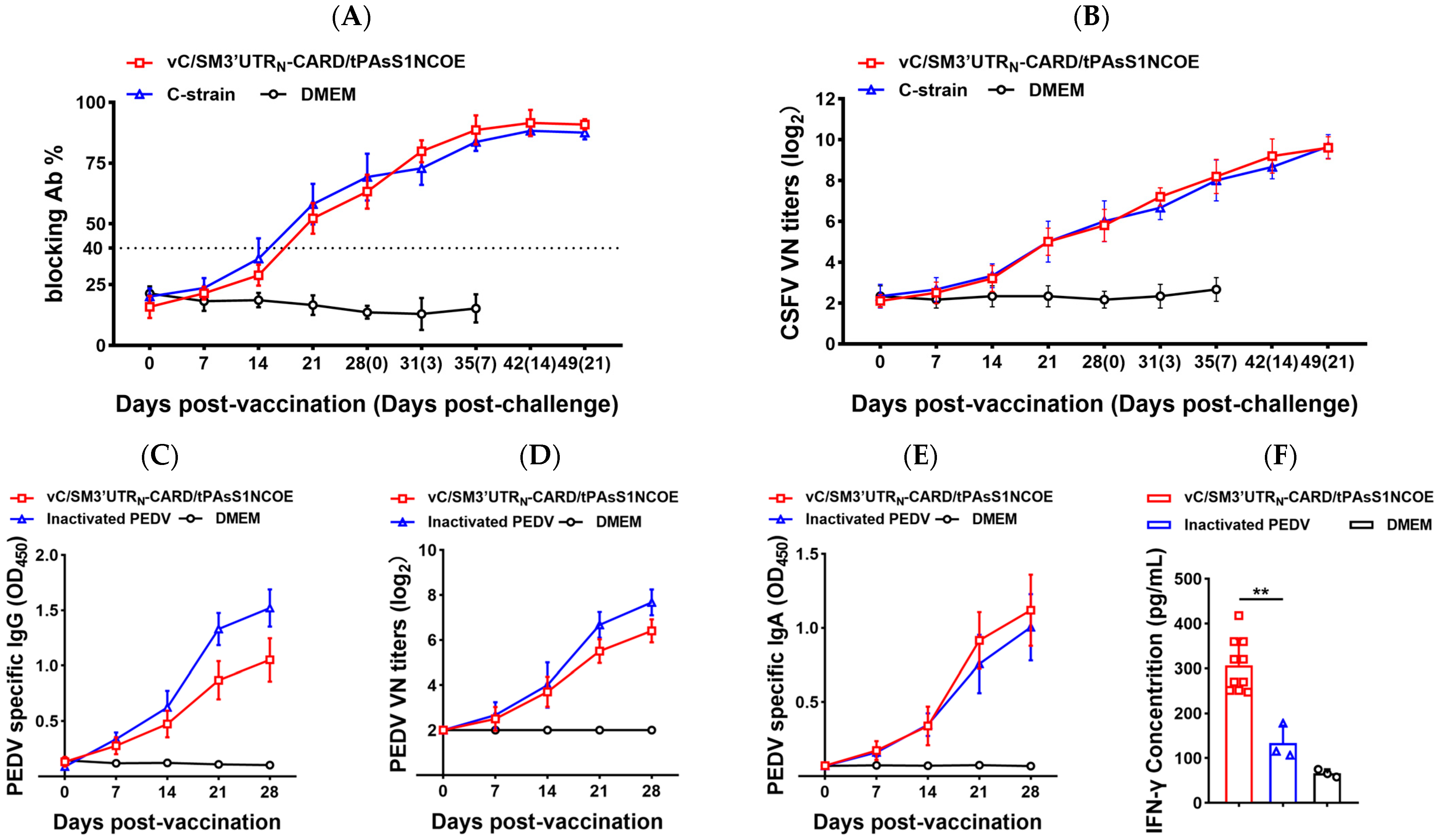
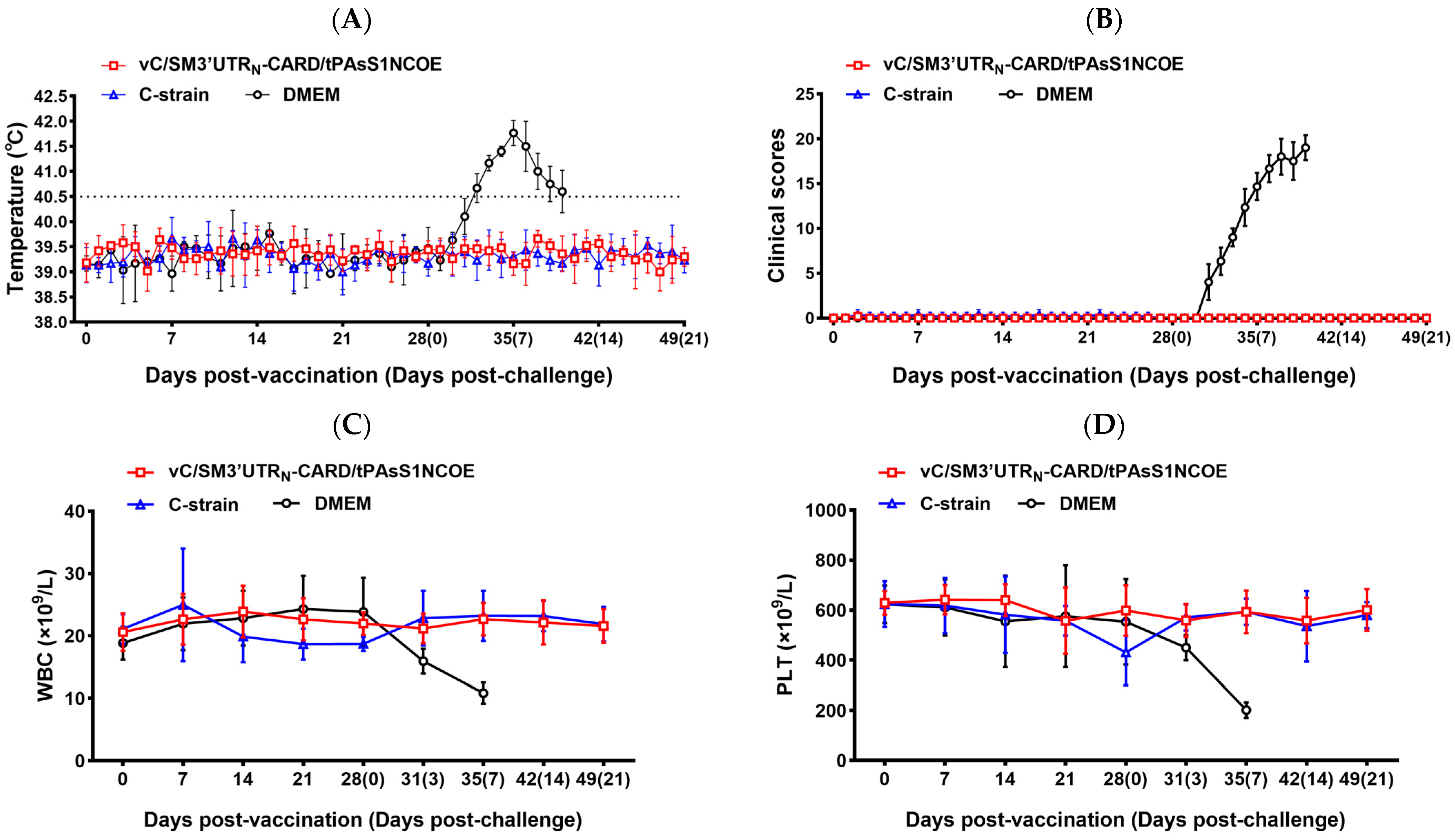
2.6. Vaccination with vC/SM3′UTRN-CARD/tPAsS1NCOE Protected Pigs against Virulent CSFV and PEDV Challenge Infection
3. Discussion
4. Materials and Methods
4.1. Cells and Viruses
4.2. Construction of Recombinant Plasmids
4.3. Construction of Chimeric cDNA Clones and Virus Rescue
4.4. Indirect Immunofluorescence Assay and Western Blotting
4.5. Virus Titration and Plaque Assay
4.6. Luciferase Reporter Assay
4.7. Animal Experiments
4.8. ELISA
4.9. Serum Neutralization Test
4.10. RT–qPCR
4.11. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ji, W.; Guo, Z.; Ding, N.Z.; He, C.Q. Studying classical swine fever virus: Making the best of a bad virus. Virus Res. 2015, 197, 35–47. [Google Scholar] [CrossRef]
- Edwards, S.; Fukusho, A.; Lefevre, P.C.; Lipowski, A.; Pejsak, Z.; Roehe, P.; Westergaard, J. Classical swine fever: The global situation. Vet. Microbiol. 2000, 73, 103–119. [Google Scholar] [CrossRef]
- Li, W.; Li, H.; Liu, Y.; Pan, Y.; Deng, F.; Song, Y.; Tang, X.; He, Q. New variants of porcine epidemic diarrhea virus, China, 2011. Emerg. Infect Dis. 2012, 18, 1350–1353. [Google Scholar] [CrossRef]
- Sun, R.Q.; Cai, R.J.; Chen, Y.Q.; Liang, P.S.; Chen, D.K.; Song, C.X. Outbreak of porcine epidemic diarrhea in suckling piglets, China. Emerg. Infect. Dis. 2012, 18, 161–163. [Google Scholar] [CrossRef]
- Blome, S.; Staubach, C.; Henke, J.; Carlson, J.; Beer, M. Classical Swine Fever-An Updated Review. Viruses 2017, 9, 86. [Google Scholar] [CrossRef] [Green Version]
- Collett, M.S.; Moennig, V.; Horzinek, M.C. Recent advances in pestivirus research. J. Gen. Virol. 1989, 70 Pt 2, 253–266. [Google Scholar] [CrossRef]
- Zheng, F.; Lu, G.; Li, L.; Gong, P.; Pan, Z. Uncoupling of Protease trans-Cleavage and Helicase Activities in Pestivirus NS3. J. Virol. 2017, 91, 01094-17. [Google Scholar] [CrossRef] [Green Version]
- Lamp, B.; Riedel, C.; Roman-Sosa, G.; Heimann, M.; Jacobi, S.; Becher, P.; Thiel, H.J.; Rumenapf, T. Biosynthesis of classical swine fever virus nonstructural proteins. J. Virol. 2011, 85, 3607–3620. [Google Scholar] [CrossRef] [Green Version]
- Moulin, H.R.; Seuberlich, T.; Bauhofer, O.; Bennett, L.C.; Tratschin, J.D.; Hofmann, M.A.; Ruggli, N. Nonstructural proteins NS2-3 and NS4A of classical swine fever virus: Essential features for infectious particle formation. Virology 2007, 365, 376–389. [Google Scholar] [CrossRef] [Green Version]
- Stark, R.; Meyers, G.; Rumenapf, T.; Thiel, H.J. Processing of pestivirus polyprotein: Cleavage site between autoprotease and nucleocapsid protein of classical swine fever virus. J. Virol. 1993, 67, 7088–7095. [Google Scholar] [CrossRef] [Green Version]
- Ruggli, N.; Summerfield, A.; Fiebach, A.R.; Guzylack-Piriou, L.; Bauhofer, O.; Lamm, C.G.; Waltersperger, S.; Matsuno, K.; Liu, L.; Gerber, M.; et al. Classical swine fever virus can remain virulent after specific elimination of the interferon regulatory factor 3-degrading function of Npro. J. Virol. 2009, 83, 817–829. [Google Scholar] [CrossRef] [Green Version]
- Tamura, T.; Nagashima, N.; Ruggli, N.; Summerfield, A.; Kida, H.; Sakoda, Y. Npro of classical swine fever virus contributes to pathogenicity in pigs by preventing type I interferon induction at local replication sites. Vet. Res. 2014, 45, 47. [Google Scholar] [CrossRef] [Green Version]
- Mine, J.; Tamura, T.; Mitsuhashi, K.; Okamatsu, M.; Parchariyanon, S.; Pinyochon, W.; Ruggli, N.; Tratschin, J.D.; Kida, H.; Sakoda, Y. The N-terminal domain of Npro of classical swine fever virus determines its stability and regulates type I IFN production. J. Gen. Virol. 2015, 96, 1746–1756. [Google Scholar] [CrossRef]
- Rumenapf, T.; Stark, R.; Heimann, M.; Thiel, H.J. N-terminal protease of pestiviruses: Identification of putative catalytic residues by site-directed mutagenesis. J. Virol. 1998, 72, 2544–2547. [Google Scholar] [CrossRef]
- Graham, S.P.; Everett, H.E.; Haines, F.J.; Johns, H.L.; Sosan, O.A.; Salguero, F.J.; Clifford, D.J.; Steinbach, F.; Drew, T.W.; Crooke, H.R. Challenge of Pigs with Classical Swine Fever Viruses after C-Strain Vaccination Reveals Remarkably Rapid Protection and Insights into Early Immunity. PLoS ONE 2012, 7, e29310. [Google Scholar] [CrossRef] [Green Version]
- Luo, Y.Z.; Li, S.; Sun, Y.; Qiu, H.J. Classical swine fever in China: A minireview. Vet. Microbiol. 2014, 172, 1–6. [Google Scholar] [CrossRef]
- Soldevila, F.; Edwards, J.C.; Graham, S.P.; Crooke, H.R.; Werling, D.; Steinbach, F. Activation of Dendritic Cells in Tonsils Is Associated with CD8 T Cell Responses following Vaccination with Live Attenuated Classical Swine Fever Virus. Int. J. Mol. Sci. 2021, 22, 8795. [Google Scholar] [CrossRef]
- Zhang, L.; Li, Y.; Xie, L.; Wang, X.; Gao, X.; Sun, Y.; Qiu, H.J. Secreted Expression of the Cap Gene of Porcine Circovirus Type 2 in Classical Swine Fever Virus C-Strain: Potential of C-Strain Used as a Vaccine Vector. Viruses 2017, 9, 298. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.F.; Wang, X.; Sun, Y.; Li, L.F.; Zhang, L.K.; Li, S.; Luo, Y.Z.; Qiu, H.J. Generation and evaluation of a chimeric classical swine fever virus expressing a visible marker gene. Arch. Virol. 2016, 161, 563–571. [Google Scholar] [CrossRef]
- Kocherhans, R.; Bridgen, A.; Ackermann, M.; Tobler, K. Completion of the porcine epidemic diarrhoea coronavirus (PEDV) genome sequence. Virus Genes 2001, 23, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Duarte, M.; Tobler, K.; Bridgen, A.; Rasschaert, D.; Ackermann, M.; Laude, H. Sequence analysis of the porcine epidemic diarrhea virus genome between the nucleocapsid and spike protein genes reveals a polymorphic ORF. Virology 1994, 198, 466–476. [Google Scholar] [CrossRef]
- Duarte, M.; Laude, H. Sequence of the spike protein of the porcine epidemic diarrhoea virus. J. Gen. Virol. 1994, 75 Pt 5, 1195–1200. [Google Scholar] [CrossRef]
- Liu, J.; Shi, H.; Chen, J.; Zhang, X.; Shi, D.; Ji, Z.; Jing, Z.; Feng, L. A New Neutralization Epitope in the Spike Protein of Porcine Epidemic Diarrhea Virus. Int. J. Mol. Sci. 2022, 23, 9674. [Google Scholar] [CrossRef]
- Walls, A.C.; Tortorici, M.A.; Bosch, B.J.; Frenz, B.; Rottier, P.J.M.; DiMaio, F.; Rey, F.A.; Veesler, D. Cryo-electron microscopy structure of a coronavirus spike glycoprotein trimer. Nature 2016, 531, 114–117. [Google Scholar] [CrossRef] [Green Version]
- Reguera, J.; Mudgal, G.; Santiago, C.; Casasnovas, J.M. A structural view of coronavirus-receptor interactions. Virus Res. 2014, 194, 3–15. [Google Scholar] [CrossRef]
- Walls, A.C.; Park, Y.J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292.e6. [Google Scholar] [CrossRef]
- Li, C.; Li, W.; Lucio de Esesarte, E.; Guo, H.; van den Elzen, P.; Aarts, E.; van den Born, E.; Rottier, P.J.M.; Bosch, B.J. Cell Attachment Domains of the Porcine Epidemic Diarrhea Virus Spike Protein Are Key Targets of Neutralizing Antibodies. J. Virol. 2017, 91, 00273-1. [Google Scholar] [CrossRef] [Green Version]
- Chang, S.H.; Bae, J.L.; Kang, T.J.; Kim, J.; Chung, G.H.; Lim, C.W.; Laude, H.; Yang, M.S.; Jang, Y.S. Identification of the epitope region capable of inducing neutralizing antibodies against the porcine epidemic diarrhea virus. Mol. Cells 2002, 14, 295–299. [Google Scholar]
- Song, D.; Moon, H.; Kang, B. Porcine epidemic diarrhea: A review of current epidemiology and available vaccines. Clin. Exp. Vaccine Res. 2015, 4, 166–176. [Google Scholar] [CrossRef] [Green Version]
- Schulz, L.L.; Tonsor, G.T. Assessment of the economic impacts of porcine epidemic diarrhea virus in the United States. J. Anim. Sci. 2015, 93, 5111–5118. [Google Scholar] [CrossRef] [Green Version]
- Su, M.; Li, C.; Qi, S.; Yang, D.; Jiang, N.; Yin, B.; Guo, D.; Kong, F.; Yuan, D.; Feng, L.; et al. A molecular epidemiological investigation of PEDV in China: Characterization of co-infection and genetic diversity of S1-based genes. Transbound. Emerg. Dis. 2020, 67, 1129–1140. [Google Scholar] [CrossRef] [Green Version]
- Luo, Y.; Ji, S.; Lei, J.L.; Xiang, G.T.; Liu, Y.; Gao, Y.; Meng, X.Y.; Zheng, G.; Zhang, E.Y.; Wang, Y.; et al. Efficacy evaluation of the C-strain-based vaccines against the subgenotype 2.1d classical swine fever virus emerging in China. Vet. Microbiol. 2017, 201, 154–161. [Google Scholar] [CrossRef]
- Gerdts, V.; Zakhartchouk, A. Vaccines for porcine epidemic diarrhea virus and other swine coronaviruses. Vet. Microbiol. 2017, 206, 45–51. [Google Scholar] [CrossRef]
- Reed, S.G.; Orr, M.T.; Fox, C.B. Key roles of adjuvants in modern vaccines. Nat. Med. 2013, 19, 1597–1608. [Google Scholar] [CrossRef]
- Kobiyama, K.; Takeshita, F.; Ishii, K.J.; Koyama, S.; Aoshi, T.; Akira, S.; Sakaue-Sawano, A.; Miyawaki, A.; Yamanaka, Y.; Hirano, H.; et al. A signaling polypeptide derived from an innate immune adaptor molecule can be harnessed as a new class of vaccine adjuvant. J. Immunol. 2009, 182, 1593–1601. [Google Scholar] [CrossRef] [Green Version]
- Cao, T.; Li, X.; Xu, Y.; Zhang, S.; Wang, Z.; Shan, Y.; Sun, J.; Fang, W.; Li, X. Npro of Classical Swine Fever Virus Suppresses Type III Interferon Production by Inhibiting IRF1 Expression and Its Nuclear Translocation. Viruses 2019, 11, 998. [Google Scholar] [CrossRef] [Green Version]
- Pang, H.; Li, L.; Liu, H.; Pan, Z. Proline to Threonine Mutation at Position 162 of NS5B of Classical Swine Fever Virus Vaccine C Strain Promoted Genome Replication and Infectious Virus Production by Facilitating Initiation of RNA Synthesis. Viruses 2021, 13, 1523. [Google Scholar] [CrossRef]
- Park, Y.; Oh, Y.; Wang, M.; Ganges, L.; Bohorquez, J.A.; Park, S.; Gu, S.; Park, J.; Lee, S.; Kim, J.; et al. A Novel E2 Glycoprotein Subunit Marker Vaccine Produced in Plant Is Able to Prevent Classical Swine Fever Virus Vertical Transmission after Double Vaccination. Vaccines 2021, 9, 418. [Google Scholar] [CrossRef]
- Jang, G.; Lee, D.; Lee, C. Development of a Next-Generation Vaccine Platform for Porcine Epidemic Diarrhea Virus Using a Reverse Genetics System. Viruses 2022, 14, 2319. [Google Scholar] [CrossRef]
- Chenut, G.; Saintilan, A.F.; Burger, C.; Rosenthal, F.; Cruciere, C.; Picard, M.; Bruyere, V.; Albina, E. Oral immunisation of swine with a classical swine fever vaccine (Chinese strain) and transmission studies in rabbits and sheep. Vet. Microbiol. 1999, 64, 265–276. [Google Scholar] [CrossRef]
- Yang, Z.; Wu, R.; Li, R.W.; Li, L.; Xiong, Z.; Zhao, H.; Guo, D.; Pan, Z. Chimeric classical swine fever (CSF)-Japanese encephalitis (JE) viral replicon as a non-transmissible vaccine candidate against CSF and JE infections. Virus Res. 2012, 165, 61–70. [Google Scholar] [CrossRef]
- Chen, J.; Liu, X.; Shi, D.; Shi, H.; Zhang, X.; Li, C.; Chi, Y.; Feng, L. Detection and molecular diversity of spike gene of porcine epidemic diarrhea virus in China. Viruses 2013, 5, 2601–2613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, J.; Fang, L.; Ye, X.; Chen, J.; Xu, S.; Zhu, X.; Miao, Y.; Wang, D.; Xiao, S. Evolutionary and genotypic analyses of global porcine epidemic diarrhea virus strains. Transbound. Emerg. Dis. 2019, 66, 111–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qin, Y.; Lu, B.; He, Y.; Li, B.; Duan, Q.; Liang, J.; Chen, Z.; Su, Q.; Bi, B.; Zhao, W. Full-Length Genome Sequence of Porcine Epidemic Diarrhea Virus Strain CH/GX/2015/750A. Genom. Announc. 2017, 5, 00361-17. [Google Scholar] [CrossRef] [Green Version]
- Park, S.J.; Song, D.S.; Ha, G.W.; Park, B.K. Cloning and further sequence analysis of the spike gene of attenuated porcine epidemic diarrhea virus DR13. Virus Genes 2007, 35, 55–64. [Google Scholar] [CrossRef]
- Mei, X.; Guo, J.; Fang, P.; Ma, J.; Li, M.; Fang, L. The Characterization and Pathogenicity of a Recombinant Porcine Epidemic Diarrhea Virus Variant ECQ1. Viruses 2023, 15, 1492. [Google Scholar] [CrossRef]
- Hou, Y.; Wang, Q. Emerging Highly Virulent Porcine Epidemic Diarrhea Virus: Molecular Mechanisms of Attenuation and Rational Design of Live Attenuated Vaccines. Int. J. Mol. Sci. 2019, 20, 5478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Z.; Liu, Q.; Sun, Y.; Li, J.; Liu, J.; Pan, R.; Cao, L.; Chen, X.; Li, Y.; Zhang, Y.; et al. Live attenuated coronavirus vaccines deficient in N7-Methyltransferase activity induce both humoral and cellular immune responses in mice. Emerg. Microbes Infect. 2021, 10, 1626–1637. [Google Scholar] [CrossRef] [PubMed]
- Pan, R.; Kindler, E.; Cao, L.; Zhou, Y.; Zhang, Z.; Liu, Q.; Ebert, N.; Zust, R.; Sun, Y.; Gorbalenya, A.E.; et al. N7-Methylation of the Coronavirus RNA Cap Is Required for Maximal Virulence by Preventing Innate Immune Recognition. mBio 2022, 13, e03662-21. [Google Scholar] [CrossRef]
- Walsh, E.P.; Baron, M.D.; Rennie, L.F.; Monaghan, P.; Anderson, J.; Barrett, T. Recombinant rinderpest vaccines expressing membrane-anchored proteins as genetic markers: Evidence of exclusion of marker protein from the virus envelope. J. Virol. 2000, 74, 10165–10175. [Google Scholar] [CrossRef] [Green Version]
- Thomson, S.A.; Burrows, S.R.; Misko, I.S.; Moss, D.J.; Coupar, B.E.; Khanna, R. Targeting a polyepitope protein incorporating multiple class II-restricted viral epitopes to the secretory/endocytic pathway facilitates immune recognition by CD4+ cytotoxic T lymphocytes: A novel approach to vaccine design. J. Virol. 1998, 72, 2246–2252. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Howard, A.; Kelley, C.; Delogu, G.; Collins, F.; Morris, S. Immunogenicity of DNA vaccines expressing tuberculosis proteins fused to tissue plasminogen activator signal sequences. Infect. Immun. 1999, 67, 4780–4786. [Google Scholar] [CrossRef] [PubMed]
- Proietti, E.; Bracci, L.; Puzelli, S.; Di Pucchio, T.; Sestili, P.; De Vincenzi, E.; Venditti, M.; Capone, I.; Seif, I.; De Maeyer, E.; et al. Type I IFN as a natural adjuvant for a protective immune response: Lessons from the influenza vaccine model. J. Immunol. 2002, 169, 375–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seth, R.B.; Sun, L.; Ea, C.K.; Chen, Z.J. Identification and characterization of MAVS, a mitochondrial antiviral signaling protein that activates NF-kappaB and IRF 3. Cell 2005, 122, 669–682. [Google Scholar] [CrossRef] [Green Version]
- Xu, L.G.; Wang, Y.Y.; Han, K.J.; Li, L.Y.; Zhai, Z.; Shu, H.B. VISA is an adapter protein required for virus-triggered IFN-beta signaling. Mol. Cell 2005, 19, 727–740. [Google Scholar] [CrossRef]
- Kawai, T.; Akira, S. Antiviral signaling through pattern recognition receptors. J. Biochem. 2007, 141, 137–145. [Google Scholar] [CrossRef]
- Zhang, Y.; Qiao, L.; Hu, X.; Zhao, K.; Zhang, Y.; Chai, F.; Pan, Z. Baculovirus vectors expressing F proteins in combination with virus-induced signaling adaptor (VISA) molecules confer protection against respiratory syncytial virus infection. Vaccine 2016, 34, 252–260. [Google Scholar] [CrossRef]
- Luo, M.; Qu, X.; Pan, R.; Zhu, D.; Zhang, Y.; Wu, J.; Pan, Z. The virus-induced signaling adaptor molecule enhances DNA-raised immune protection against H5N1 influenza virus infection in mice. Vaccine 2011, 29, 2561–2567. [Google Scholar] [CrossRef]
- Li, L.; Pang, H.; Wu, R.; Zhang, Y.; Tan, Y.; Pan, Z. Development of a novel single-step reverse genetics system for the generation of classical swine fever virus. Arch. Virol. 2016, 161, 1831–1838. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent end points. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Xie, L.; Han, Y.; Ma, Y.; Yuan, M.; Li, W.; Li, L.F.; Li, M.; Sun, Y.; Luo, Y.; Li, S.; et al. P108 and T109 on E2 Glycoprotein Domain I Are Critical for the Adaptation of Classical Swine Fever Virus to Rabbits but Not for Virulence in Pigs. J. Virol. 2020, 94, 01104-20. [Google Scholar] [CrossRef]
- Yi, W.; Wang, H.; Qin, H.; Wang, Q.; Guo, R.; Wen, G.; Pan, Z. Construction and efficacy of a new live chimeric C-strain vaccine with DIVA characteristics against classical swine fever. Vaccine 2023, 41, 2003–2012. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.Y.; Hsu, W.T.; Chao, Y.C.; Chang, H.W. Display of Porcine Epidemic Diarrhea Virus Spike Protein on Baculovirus to Improve Immunogenicity and Protective Efficacy. Viruses 2018, 10, 346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mittelholzer, C.; Moser, C.; Tratschin, J.D.; Hofmann, M.A. Analysis of classical swine fever virus replication kinetics allows differentiation of highly virulent from avirulent strains. Vet. Microbiol. 2000, 74, 293–308. [Google Scholar] [CrossRef] [PubMed]



| Inocula | Sample | N.E.P a | Days Post-Vaccination (Days Post-Challenge) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 7 | 14 | 21 | 28(0) | 31(3) | 35(7) | 42(14) | 49(21) | |||
| vC/SM3′UTRN-CARD/tPAsS1NCOE | Blood | 158 | – b | – | – | – | – | – | – | – | – |
| 169 | – | – | – | – | – | – | – | – | – | ||
| 181 | – | – | – | – | – | – | – | – | – | ||
| 182 | – | – | – | – | – | – | – | – | – | ||
| 192 | – | – | – | – | – | – | – | – | – | ||
| Oral swab | 158 | – | – | – | – | – | – | – | – | – | |
| 169 | – | – | – | – | – | – | – | – | – | ||
| 181 | – | – | – | – | – | – | – | – | – | ||
| 182 | – | – | – | – | – | – | – | – | – | ||
| 192 | – | – | – | – | – | – | – | – | – | ||
| Fecal swab | 158 | – | – | – | – | – | – | – | – | – | |
| 169 | – | – | – | – | – | – | – | – | – | ||
| 181 | – | – | – | – | – | – | – | – | – | ||
| 182 | – | – | – | – | – | – | – | – | – | ||
| 192 | – | – | – | – | – | – | – | – | – | ||
| C-strain | Blood | 174 | – | – | – | – | – | – | – | – | – |
| 186 | – | – | – | – | – | – | – | – | – | ||
| 209 | – | – | – | – | – | – | – | – | – | ||
| Oral swab | 174 | – | – | – | – | – | – | – | – | – | |
| 186 | – | – | – | – | – | – | – | – | – | ||
| 209 | – | – | – | – | – | – | – | – | – | ||
| Fecal swab | 174 | – | – | – | – | – | – | – | – | – | |
| 186 | – | – | – | – | – | – | – | – | – | ||
| 209 | – | – | – | – | – | – | – | – | – | ||
| DMEM | Blood | 157 | – | – | – | – | – | 1.41 × 103 | 1.66 × 107 | / c | / |
| 204 | – | – | – | – | – | 1.83 × 103 | 1.72 × 106 | / | / | ||
| 208 | – | – | – | – | – | 3.24 × 102 | 1.49 × 105 | / | / | ||
| Oral swab | 157 | – | – | – | – | – | 1.26 × 103 | 1.27 × 107 | / | / | |
| 204 | – | – | – | – | – | 2.12 × 103 | 4.56 × 106 | / | / | ||
| 208 | – | – | – | – | – | 3.95 × 103 | 1.45 × 106 | / | / | ||
| Fecal swab | 157 | – | – | – | – | – | 1.70 × 103 | 1.24 × 105 | / | / | |
| 204 | – | – | – | – | – | 1.26 × 103 | 2.01 × 105 | / | / | ||
| 208 | – | – | – | – | – | 5.41 × 102 | 9.37 × 104 | / | / | ||
| Inocula | vC/SM3′UTRN-CARD/tPAsS1NCOE (n = 5) | C-Strain (n = 3) | DMEM (n = 3) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N.E.P a | 158 | 169 | 181 | 182 | 192 | 174 | 186 | 209 | 157 | 204 | 208 |
| Tissues | |||||||||||
| Tonsil | – b | – | – | – | – | – | – | – | 3.56 × 107 | 4.66 × 106 | 3.77 × 106 |
| Submandibular lymph node | – | – | – | – | – | – | – | – | 6.26 × 107 | 6.02 × 106 | 4.47 × 106 |
| Spleen | – | – | – | – | – | – | – | – | 4.73 × 106 | 7.19 × 105 | 6.01 × 105 |
| Kidney | – | – | – | – | – | – | – | – | 4.94 × 105 | 5.95 × 104 | 9.87 × 104 |
| Inocula | vC/SM3′UTRN-CARD/tPAsS1NCOE (n = 5) | Inactivated PEDV (n = 3) | DMEM (n = 3) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N.E.P a 156 | 160 | 205 | 210 | 217 | 161 | 202 | 203 | 152 | 155 | 214 | ||||
| dpc b | Viral RNA Copies | CS c | Viral RNA Copies | CS | Viral RNA Copies | CS | ||||||||
| 0 | – d | – | – | – | – | 0/0/0/0/0 | – | – | – | 0/0/0 | – | – | – | 0/0/0 |
| 3 | – | – | – | 9.81 × 102 | 2.94 × 103 | 0/0/0/0/1 | 1.01 × 103 | – | 1.94 × 103 | 0/0/1 | 9.59 × 105 | 6.94 × 106 | 6.79 × 105 | 2/3/2 |
| 5 | – | 1.87 × 103 | 2.98 × 103 | 3.56 × 103 | 4.91 × 103 | 0/0/1/1/1 | 1.51 × 104 | 2.75 × 104 | 3.63 × 104 | 1/1/1 | 7.17 × 107 | 1.01 × 108 | 9.51 × 106 | 3/3/3 |
| 7 | – | – | – | 1.61 × 103 | 1.61 × 103 | 0/0/0/1/1 | – | 9.08 × 103 | 1.10 × 103 | 0/1/0 | 1.06 × 106 | 7.49 × 106 | 5.87 × 105 | 2/3/2 |
| 9 | – | – | – | – | – | 0/0/0/0/0 | – | – | – | 0/0/0 | 1.09 × 106 | 4.31 × 106 | 6.95 × 103 | 2/2/1 |
| 11 | – | – | – | – | – | 0/0/0/0/0 | – | – | – | 0/0/0 | 3.64 × 105 | 6.69 × 105 | 8.10 × 103 | 1/1/0 |
| 14 | – | – | – | – | – | 0/0/0/0/0 | – | – | – | 0/0/0 | 7.88 × 103 | 2.97 × 104 | 1.98 × 103 | 0/0/0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; Yi, W.; Qin, H.; Wang, Q.; Guo, R.; Pan, Z. A Genetically Engineered Bivalent Vaccine Coexpressing a Molecular Adjuvant against Classical Swine Fever and Porcine Epidemic Diarrhea. Int. J. Mol. Sci. 2023, 24, 11954. https://doi.org/10.3390/ijms241511954
Wang H, Yi W, Qin H, Wang Q, Guo R, Pan Z. A Genetically Engineered Bivalent Vaccine Coexpressing a Molecular Adjuvant against Classical Swine Fever and Porcine Epidemic Diarrhea. International Journal of Molecular Sciences. 2023; 24(15):11954. https://doi.org/10.3390/ijms241511954
Chicago/Turabian StyleWang, Hao, Weicheng Yi, Huan Qin, Qin Wang, Rui Guo, and Zishu Pan. 2023. "A Genetically Engineered Bivalent Vaccine Coexpressing a Molecular Adjuvant against Classical Swine Fever and Porcine Epidemic Diarrhea" International Journal of Molecular Sciences 24, no. 15: 11954. https://doi.org/10.3390/ijms241511954




