The Role of CD4/6 Inhibitors in Breast Cancer Treatment
Abstract
:1. Introduction
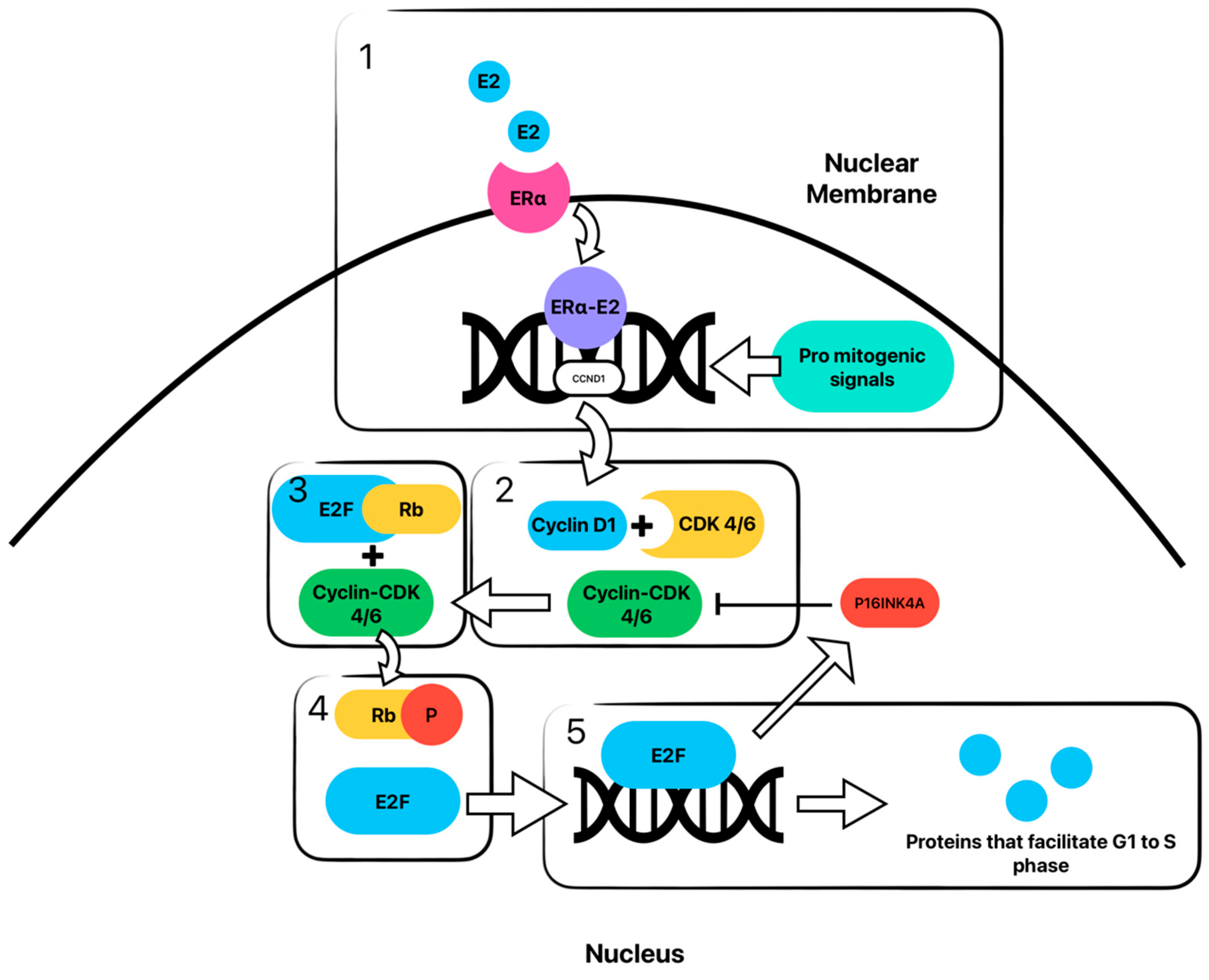
2. CDK Pathway and Inhibition
2.1. The Pathway
2.2. Regulation of the Pathway
2.3. Inhibition of the Dysregulated Pathway
3. Clinical Use of CDK 4/6 Inhibitors
3.1. Metastatic or Advanced ER+/HER2− Breast Cancer
3.2. Considering Endocrine Resistance in Treatment of ER+/HER2− Advanced Breast Cancer
3.3. Determining Sequence of Therapy
3.4. Adjuvant Use of CDK4/6 Inhibitor in Early Breast Cancer (EBC): PENELOPE-B, PALLAS, MonarchE, and NATALEE Trials
3.5. CDK Inhibtor Use in ER+/HER2+ Breast Cancer
4. Search for Biomarkers
4.1. Prediciting Response
4.2. Monitoring Response
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- U.S. Cancer Statistics Data Visualizations Tool|CDC. 9 June 2023. Available online: https://www.cdc.gov/cancer/uscs/dataviz/index.htm (accessed on 1 September 2023).
- Massagué, J. G1 Cell-Cycle Control and Cancer. Nature 2004, 432, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Finn, R.S.; Boer, K.; Bondarenko, I.; Patel, R.; Pinter, T.; Schmidt, M.; Shparyk, Y.V.; Thummala, A.; Voitko, N.; Bananis, E.; et al. Overall Survival Results from the Randomized Phase 2 Study of Palbociclib in Combination with Letrozole versus Letrozole Alone for First-Line Treatment of ER+/HER2− Advanced Breast Cancer (PALOMA-1, TRIO-18). Breast Cancer Res. Treat. 2020, 183, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Rugo, H.S.; Finn, R.S.; Diéras, V.; Ettl, J.; Lipatov, O.; Joy, A.A.; Harbeck, N.; Castrellon, A.; Iyer, S.; Lu, D.R.; et al. Palbociclib plus Letrozole as First-Line Therapy in Estrogen Receptor-Positive/Human Epidermal Growth Factor Receptor 2-Negative Advanced Breast Cancer with Extended Follow-Up. Breast Cancer Res. Treat. 2019, 174, 719–729. [Google Scholar] [CrossRef]
- Cristofanilli, M.; Turner, N.C.; Bondarenko, I.; Ro, J.; Im, S.A.; Masuda, N.; Colleoni, M.; DeMichele, A.; Loi, S.; Verma, S.; et al. Fulvestrant plus Palbociclib versus Fulvestrant plus Placebo for Treatment of Hormone-Receptor-Positive, HER2-Negative Metastatic Breast Cancer That Progressed on Previous Endocrine Therapy (PALOMA-3): Final Analysis of the Multicentre, Double-Blind, Phase 3 Randomised Controlled Trial. Lancet Oncol. 2016, 17, 425–439. [Google Scholar] [CrossRef] [PubMed]
- O’shaughnessy, J.; Petrakova, K.; Sonke, G.S.; Conte, P.; Arteaga, C.L.; Cameron, D.A.; Hart, L.L.; Villanueva, C.; Jakobsen, E.; Beck, J.T.; et al. Ribociclib plus Letrozole versus Letrozole Alone in Patients with de Novo HR+, HER2− Advanced Breast Cancer in the Randomized MONALEESA-2 Trial. Breast Cancer Res. Treat. 2018, 168, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Fasching, P.A.; Beck, J.T.; Chan, A.; De Laurentiis, M.; Esteva, F.J.; Jerusalem, G.; Neven, P.; Pivot, X.; Bianchi, G.V.; Martin, M.; et al. Ribociclib plus Fulvestrant for Advanced Breast Cancer: Health-Related Quality-of-Life Analyses from the MONALEESA-3 Study. Breast Off. J. Eur. Soc. Mastol. 2020, 54, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.S.; Im, S.A.; Colleoni, M.; Franke, F.; Bardia, A.; Cardoso, F.; Harbeck, N.; Hurvitz, S.; Chow, L.; Sohn, J.; et al. Updated Overall Survival of Ribociclib plus Endocrine Therapy versus Endocrine Therapy Alone in Pre- and Perimenopausal Patients with HR+/HER2− Advanced Breast Cancer in MONALEESA-7: A Phase III Randomized Clinical Trial. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2022, 28, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Dickler, M.N.; Tolaney, S.M.; Rugo, H.S.; Cortés, J.; Diéras, V.; Patt, D.; Wildiers, H.; Hudis, C.A.; O’Shaughnessy, J.; Zamora, E.; et al. MONARCH 1, A Phase II Study of Abemaciclib, a CDK4 and CDK6 Inhibitor, as a Single Agent, in Patients with Refractory HR+/HER2− Metastatic Breast Cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, 5218–5224. [Google Scholar] [CrossRef]
- Sledge, G.W., Jr.; Toi, M.; Neven, P.; Sohn, J.; Inoue, K.; Pivot, X.; Burdaeva, O.; Okera, M.; Masuda, N.; Kaufman, P.A.; et al. MONARCH 2: Abemaciclib in Combination With Fulvestrant in Women With HR+/HER2− Advanced Breast Cancer Who Had Progressed While Receiving Endocrine Therapy. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2017, 35, 2875–2884. [Google Scholar] [CrossRef]
- Johnston, S.; Martin, M.; Di Leo, A.; Im, S.A.; Awada, A.; Forrester, T.; Frenzel, M.; Hardebeck, M.C.; Cox, J.; Barriga, S.; et al. MONARCH 3 Final PFS: A Randomized Study of Abemaciclib as Initial Therapy for Advanced Breast Cancer. NPJ Breast Cancer 2019, 5, 5. [Google Scholar] [CrossRef]
- George, M.A.; Qureshi, S.; Omene, C.; Toppmeyer, D.L.; Ganesan, S. Clinical and Pharmacologic Differences of CDK4/6 Inhibitors in Breast Cancer. Front. Oncol. 2021, 11, 693104. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.; Olivier, P.; Diehl, J.A.; Fero, M.; Roussel, M.F.; Roberts, J.M.; Sherr, C.J. The P21(Cip1) and P27(Kip1) CDK ‘inhibitors’ Are Essential Activators of Cyclin D-Dependent Kinases in Murine Fibroblasts. EMBO J. 1999, 18, 1571–1583. [Google Scholar] [CrossRef] [PubMed]
- Paternot, S.; Bockstaele, L.; Bisteau, X.; Kooken, H.; Coulonval, K.; Roger, P. Rb Inactivation in Cell Cycle and Cancer: The Puzzle of Highly Regulated Activating Phosphorylation of CDK4 versus Constitutively Active CDK-Activating Kinase. Cell Cycle 2010, 9, 689–699. [Google Scholar] [CrossRef] [PubMed]
- Harbour, J.W.; Luo, R.X.; Dei Santi, A.; Postigo, A.A.; Dean, D.C. Cdk Phosphorylation Triggers Sequential Intramolecular Interactions That Progressively Block Rb Functions as Cells Move through G1. Cell 1999, 98, 859–869. [Google Scholar] [CrossRef]
- Eeckhoute, J.; Carroll, J.S.; Geistlinger, T.R.; Torres-Arzayus, M.I.; Brown, M. A Cell-Type-Specific Transcriptional Network Required for Estrogen Regulation of Cyclin D1 and Cell Cycle Progression in Breast Cancer. Genes Dev. 2006, 20, 2513–2526. [Google Scholar] [CrossRef]
- Asghar, U.; Witkiewicz, A.K.; Turner, N.C.; Knudsen, E.S. The History and Future of Targeting Cyclin-Dependent Kinases in Cancer Therapy. Nat. Rev. Drug Discov. 2015, 14, 130–146. [Google Scholar] [CrossRef]
- Agarwal, P.; Sandey, M.; DeInnocentes, P.; Bird, R.C. Tumor Suppressor Gene P16/INK4A/CDKN2A-Dependent Regulation into and out of the Cell Cycle in a Spontaneous Canine Model of Breast Cancer. J. Cell. Biochem. 2013, 114, 1355–1363. [Google Scholar] [CrossRef]
- Malumbres, M.; Barbacid, M. To Cycle or Not to Cycle: A Critical Decision in Cancer. Nat. Rev. Cancer 2001, 1, 222–231. [Google Scholar] [CrossRef]
- Goel, S.; DeCristo, M.J.; McAllister, S.S.; Zhao, J.J. CDK4/6 Inhibition in Cancer: Beyond Cell Cycle Arrest. Trends Cell Biol. 2018, 28, 911–925. [Google Scholar] [CrossRef]
- Bose, P.; Simmons, G.L.; Grant, S. Cyclin-Dependent Kinase Inhibitor Therapy for Hematologic Malignancies. Expert Opin. Investig. Drugs 2013, 22, 723–738. [Google Scholar] [CrossRef]
- Whittaker, S.R.; Mallinger, A.; Workman, P.; Clarke, P.A. Inhibitors of Cyclin-Dependent Kinases as Cancer Therapeutics. Pharmacol. Ther. 2017, 173, 83–105. [Google Scholar] [CrossRef]
- Braal, C.L.; Jongbloed, E.M.; Wilting, S.M.; Mathijssen, R.H.; Koolen, S.L.; Jager, A. Inhibiting CDK4/6 in Breast Cancer with Palbociclib, Ribociclib, and Abemaciclib: Similarities and Differences. Drugs 2021, 81, 317–331. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Lee, N.V.; Hu, W.; Xu, M.; Ferre, R.A.; Lam, H.; Bergqvist, S.; Solowiej, J.; Diehl, W.; He, Y.A.; et al. Spectrum and Degree of CDK Drug Interactions Predicts Clinical Performance. Mol. Cancer Ther. 2016, 15, 2273–2281. [Google Scholar] [CrossRef] [PubMed]
- Guarducci, C.; Bonechi, M.; Boccalini, G.; Benelli, M.; Risi, E.; Di Leo, A.; Malorni, L.; Migliaccio, I. Mechanisms of Resistance to CDK4/6 Inhibitors in Breast Cancer and Potential Biomarkers of Response. Breast Care 2017, 12, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Hino, H.; Iriyama, N.; Kokuba, H.; Kazama, H.; Moriya, S.; Takano, N.; Hiramoto, M.; Aizawa, S.; Miyazawa, K. Abemaciclib Induces Atypical Cell Death in Cancer Cells Characterized by Formation of Cytoplasmic Vacuoles Derived from Lysosomes. Cancer Sci. 2020, 111, 2132–2145. [Google Scholar] [CrossRef] [PubMed]
- touchONCOLOGY. Matthew Goetz, ESMO 2022: MONARCH 3 Trial—Interim Overall Survival Results of Abemaciclib + NSAI in Patients with HR+, HER2− Advanced Breast Cancer. 14 September 2022. Available online: https://touchoncology.com/breast-cancer/conference-hub/matthew-goetz-esmo-2022-monarch-3-trial-interim-overall-survival-results-of-abemaciclib-nsai-in-patients-with-hr-HER2-advanced-breast-cancer/ (accessed on 1 September 2023).
- Elgene Lim, M.D.; Metzger-Filho, O.; Winer, E.P. The Natural History of Hormone Receptor-Positive Breast Cancer. Oncology 2012, 26, 688–694, 696. [Google Scholar] [PubMed]
- Jeselsohn, R.; Buchwalter, G.; De Angelis, C.; Brown, M.; Schiff, R. ESR1 Mutations—A Mechanism for Acquired Endocrine Resistance in Breast Cancer. Nat. Rev. Clin. Oncol. 2015, 12, 573–583. [Google Scholar] [CrossRef] [PubMed]
- Dong, C.; Wu, J.; Chen, Y.; Nie, J.; Chen, C. Activation of PI3K/AKT/mTOR Pathway Causes Drug Resistance in Breast Cancer. Front. Pharmacol. 2021, 12, 628690. [Google Scholar] [CrossRef]
- André, F.; Ciruelos, E.M.; Juric, D.; Loibl, S.; Campone, M.; Mayer, I.A.; Rubovszky, G.; Yamashita, T.; Kaufman, B.; Lu, Y.S.; et al. Alpelisib plus Fulvestrant for PIK3CA-Mutated, Hormone Receptor-Positive, Human Epidermal Growth Factor Receptor-2-Negative Advanced Breast Cancer: Final Overall Survival Results from SOLAR-1. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2021, 32, 208–217. [Google Scholar] [CrossRef]
- Sonke, G.S.; Van Ommen-Nijhof, A.; Wortelboer, N.; van der Noort, V.; Swinkels, A.C.; Blommestein, H.M.; Beeker, A.; Beelen, K.; Hamming, L.C.; Heijns, J.B.; et al. Primary Outcome Analysis of the Phase 3 SONIA Trial (BOOG 2017-03) on Selecting the Optimal Position of Cyclin-Dependent Kinases 4 and 6 (CDK4/6) Inhibitors for Patients with Hormone Receptor-Positive (HR+), HER2−Negative (HER2−) Advanced Breast Cancer (ABC). J. Clin. Oncol. 2023, 41 (Suppl. 17), LBA1000. [Google Scholar] [CrossRef]
- Loibl, S.; Marmé, F.; Martin, M.; Untch, M.; Bonnefoi, H.; Kim, S.B.; Bear, H.; McCarthy, N.; Melé Olivé, M.; Gelmon, K.; et al. Palbociclib for Residual High-Risk Invasive HR-Positive and HER2-Negative Early Breast Cancer-The Penelope-B Trial. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2021, 39, 1518–1530. [Google Scholar] [CrossRef]
- Gnant, M.; Dueck, A.C.; Frantal, S.; Martin, M.; Burstein, H.J.; Greil, R.; Fox, P.; Wolff, A.C.; Chan, A.; Winer, E.P.; et al. Adjuvant Palbociclib for Early Breast Cancer: The PALLAS Trial Results (ABCSG-42/AFT-05/BIG-14-03). J. Clin. Oncol. 2022, 40, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Johnston, S.R.D.; Harbeck, N.; Hegg, R.; Toi, M.; Martin, M.; Shao, Z.M.; Zhang, Q.Y.; Martinez Rodriguez, J.L.; Campone, M.; Hamilton, E.; et al. Abemaciclib Combined With Endocrine Therapy for the Adjuvant Treatment of HR+, HER2−, Node-Positive, High-Risk, Early Breast Cancer (monarchE). J. Clin.Oncol. Off. J. Am. Soc. Clin. Oncol. 2020, 38, 3987–3998. [Google Scholar] [CrossRef]
- Slamon, D.J.; Fasching, P.A.; Hurvitz, S.; Chia, S.; Crown, J.; Martín, M.; Barrios, C.H.; Bardia, A.; Im, S.A.; Yardley, D.A.; et al. Rationale and Trial Design of NATALEE: A Phase III Trial of Adjuvant Ribociclib + Endocrine Therapy versus Endocrine Therapy Alone in Patients with HR+/HER2− Early Breast Cancer. Ther. Adv. Med. Oncol. 2023, 15, 17588359231178125. [Google Scholar] [CrossRef] [PubMed]
- Corona, S.P.; Ravelli, A.; Cretella, D.; Cappelletti, M.R.; Zanotti, L.; Dester, M.; Gobbi, A.; Petronini, P.G.; Generali, D. CDK4/6 Inhibitors in HER2-Positive Breast Cancer. Crit. Rev. Oncol./Hematol. 2017, 112, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Koirala, N.; Dey, N.; Aske, J.; De, P. Targeting Cell Cycle Progression in HER2+ Breast Cancer: An Emerging Treatment Opportunity. Int. J. Mol. Sci. 2022, 23, 6547. [Google Scholar] [CrossRef] [PubMed]
- Ciruelos, E.; Villagrasa, P.; Pascual, T.; Oliveira, M.; Pernas, S.; Paré, L.; Escrivá-de-Romaní, S.; Manso, L.; Adamo, B.; Martínez, E.; et al. Palbociclib and Trastuzumab in HER2-Positive Advanced Breast Cancer: Results from the Phase II SOLTI-1303 PATRICIA Trial. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2020, 26, 5820–5829. [Google Scholar] [CrossRef]
- Metzger, O.; Mandrekar, S.; Ciruelos, E.; Loibl, S.; Valagussa, P.; Demichele, A.M.; Lim, E.; Tripathy, D.; Winer, E.; Huang, C.; et al. PATINA: A Randomized Open Label Phase III Trial to Evaluate the Efficacy and Safety of Palbociclib + Anti HER2 Therapy + Endocrine Therapy vs Anti HER2 Therapy + Endocrine Therapy after Induction Treatment for Hormone Receptor Positive, HER2-Positive Metastatic Breast Cancer. Ann. Oncol. 2017, 28, v107–v108. [Google Scholar] [CrossRef]
- Main, S.C.; Cescon, D.W.; Bratman, S.V. Liquid Biopsies to Predict CDK4/6 Inhibitor Efficacy and Resistance in Breast Cancer. Cancer Drug Resist. 2022, 5, 727–748. [Google Scholar] [CrossRef]
- Yang, C.; Li, Z.; Bhatt, T.; Dickler, M.; Giri, D.; Scaltriti, M.; Baselga, J.; Rosen, N.; Chandarlapaty, S. Acquired CDK6 Amplification Promotes Breast Cancer Resistance to CDK4/6 Inhibitors and Loss of ER Signaling and Dependence. Oncogene 2017, 36, 2255–2264. [Google Scholar] [CrossRef]
- Li, Z.; Razavi, P.; Li, Q.; Toy, W.; Liu, B.; Ping, C.; Hsieh, W.; Sanchez-Vega, F.; Brown, D.N.; Paula, A.F.; et al. Loss of the FAT1 Tumor Suppressor Promotes Resistance to CDK4/6 Inhibitors via the Hippo Pathway. Cancer Cell 2018, 34, 893–905.e8. [Google Scholar] [CrossRef] [PubMed]
- Razavi, P.; Chang, M.T.; Xu, G.; Bandlamudi, C.; Ross, D.S.; Vasan, N.; Cai, Y.; Bielski, C.M.; Donoghue, M.T.; Jonsson, P.; et al. The Genomic Landscape of Endocrine-Resistant Advanced Breast Cancers. Cancer Cell 2018, 34, 427–438.e6. [Google Scholar] [CrossRef]
- Palafox, M.; Monserrat, L.; Bellet, M.; Villacampa, G.; Gonzalez-Perez, A.; Oliveira, M.; Brasó-Maristany, F.; Ibrahimi, N.; Kannan, S.; Mina, L.; et al. High P16 Expression and Heterozygous RB1 Loss Are Biomarkers for CDK4/6 Inhibitor Resistance in ER+ Breast Cancer. Nat. Commun. 2022, 13, 5258. [Google Scholar] [CrossRef] [PubMed]
- Gottesman, S.R.; Somma, J.; Tsiperson, V.; Dresner, L.; Govindarajulu, U.; Patel, P.; Blain, S.W. Tyrosine Phosphorylation of p27Kip1 Correlates with Palbociclib Responsiveness in Breast Cancer Tumor Cells Grown in Explant Culture. Mol. Cancer Res. MCR 2019, 17, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Darrigues, L.; Pierga, J.Y.; Bernard-Tessier, A.; Bièche, I.; Silveira, A.B.; Michel, M.; Loirat, D.; Cottu, P.; Cabel, L.; Dubot, C.; et al. Circulating Tumor DNA as a Dynamic Biomarker of Response to Palbociclib and Fulvestrant in Metastatic Breast Cancer Patients. Breast Cancer Res. BCR 2021, 23, 31. [Google Scholar] [CrossRef] [PubMed]
- Bidard, F.C.; Hardy-Bessard, A.C.; Dalenc, F.; Bachelot, T.; Pierga, J.Y.; de la Motte Rouge, T.; Sabatier, R.; Dubot, C.; Frenel, J.S.; Ferrero, J.M.; et al. Switch to Fulvestrant and Palbociclib versus No Switch in Advanced Breast Cancer with Rising ESR1 Mutation during Aromatase Inhibitor and Palbociclib Therapy (PADA-1): A Randomised, Open-Label, Multicentre, Phase 3 Trial. Lancet Oncol. 2022, 23, 1367–1377. [Google Scholar] [CrossRef]
| CDK Inhibitor | Chemical Structure | Adverse Effects |
|---|---|---|
| Palbociclib | 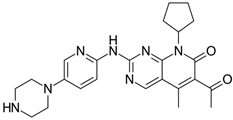 | Myelosuppression |
| Ribociclib | 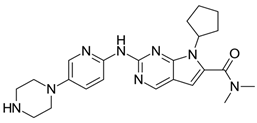 | Myelosuppression QT prolongation |
| Abemaciclib | 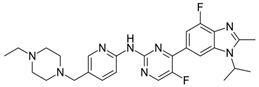 | GI toxicity |
| Trial | N | Regimens | Median OS | Hazard Ratio (95% CI) | p-Value |
|---|---|---|---|---|---|
| PALOMA-3 | 521 | Placebo + fulvestrant | 28.0 months | 0.81 (0.64–1.03) | 0.09 |
| Palbociclib + fulvestrant | 34.9 months | ||||
| MONALEESA-3 | 726 | Placebo + fulvestrant | 51.8 months | 0.72 (0.57–0.92) | 0.004 |
| Ribociclib + fulvestrant | 67.6 months | ||||
| MONALEESA-7 | 672 | Placebo + tamoxifen or NSAI | 48.0 months | 0.71 (0.53–0.95) | 0.009 |
| Ribociclib + tamoxifen or NSAI | 58.7 months | ||||
| MONARCH-2 | 669 | Placebo + fulvestrant | 37.3 months | 0.76 (0.61–0.95) | 0.01 |
| Abemaciclib + fulvestrant | 46.7 months |
| Trial | Year | Status | Patient Population | Intervention | Control Arm | Primary Outcome |
|---|---|---|---|---|---|---|
| PENELOPE-B (NCT01864746) | 2013–2020 | Completed | HR+, HER2− EBC | PAL (125 mg once daily for 13 cycles) + ≥5 years ET | ET + placebo | 42.8-month iDFS: no difference; (HR = 0.93, 95% CI: 0.74–1.17); two-sided weighted log-rank test (Cui, Hung, and Wang) p = 0.525 |
| PALLAS (NCT02513394) | 2015–2020 | Completed | HR+, HER2− EBC | PAL (125 mg orally once daily for 2 years) + ≥5 years ET | ET alone | 31-month iDFS: 8.8% PAL + ET vs. 9.1% ET, iDFS at 4 years: 84.2% vs. 84.5% (HR = 0.96, 95% CI: 0.81–1.14, p = 0.65) |
| MonarchE (NCT03155997) | 2017–2020 | Completed | HR+, HER2− EBC | Abemaciclib (150 mg twice daily for 2 years) + ET ≥5 years | ET alone | 3-year iDFS improved by 5.4% in the abemaciclib group (HR = 0.70, 95% CI: 0.59–0.82) |
| MonarchE (NCT03155997) | 2018–2026 | Active | HR+, HER2− EBC | RIBO (400 mg/day 3 weeks on, 1 week off for 3 years) + ET ≥5 years | ET alone | 34-month iDFS improved by 3.3% in the RIB + ET group; iDFS (HR, 0.748; 95% CI, 0.618–0.906; p = 0.0014); 3-year iDFS rates: 90.4% vs. 87.1% |
| Trial | Phase | Setting | Arms | Primary Outcomes |
|---|---|---|---|---|
| PATINA Clinical study of the targeted therapy, palbociclib, to treat metastatic breast cancer (NCT02947685) | Phase III n = 496 International centers | Metastatic HR+/HER2+ breast cancer |
| Progression-free survival (PFS) |
| PATRICIA II Palbociclib and trastuzumab with endocrine therapy in HER2-positive metastatic breast cancer (NCT02448420) | Phase II n = 102 Spain | Metastatic HR+/HER2+ breast cancer |
| Progression-free survival (PFS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Purohit, L.; Jones, C.; Gonzalez, T.; Castrellon, A.; Hussein, A. The Role of CD4/6 Inhibitors in Breast Cancer Treatment. Int. J. Mol. Sci. 2024, 25, 1242. https://doi.org/10.3390/ijms25021242
Purohit L, Jones C, Gonzalez T, Castrellon A, Hussein A. The Role of CD4/6 Inhibitors in Breast Cancer Treatment. International Journal of Molecular Sciences. 2024; 25(2):1242. https://doi.org/10.3390/ijms25021242
Chicago/Turabian StylePurohit, Luv, Can Jones, Teresita Gonzalez, Aurelio Castrellon, and Atif Hussein. 2024. "The Role of CD4/6 Inhibitors in Breast Cancer Treatment" International Journal of Molecular Sciences 25, no. 2: 1242. https://doi.org/10.3390/ijms25021242




