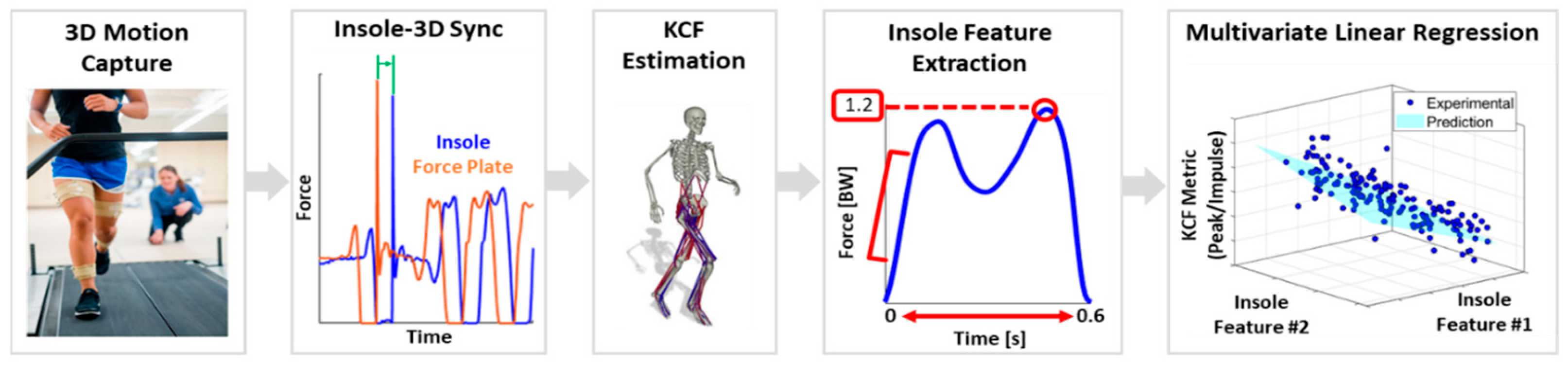
Monitoring Knee Contact Force with Force-Sensing Insoles
Abstract
1. Introduction
2. Materials and Methods
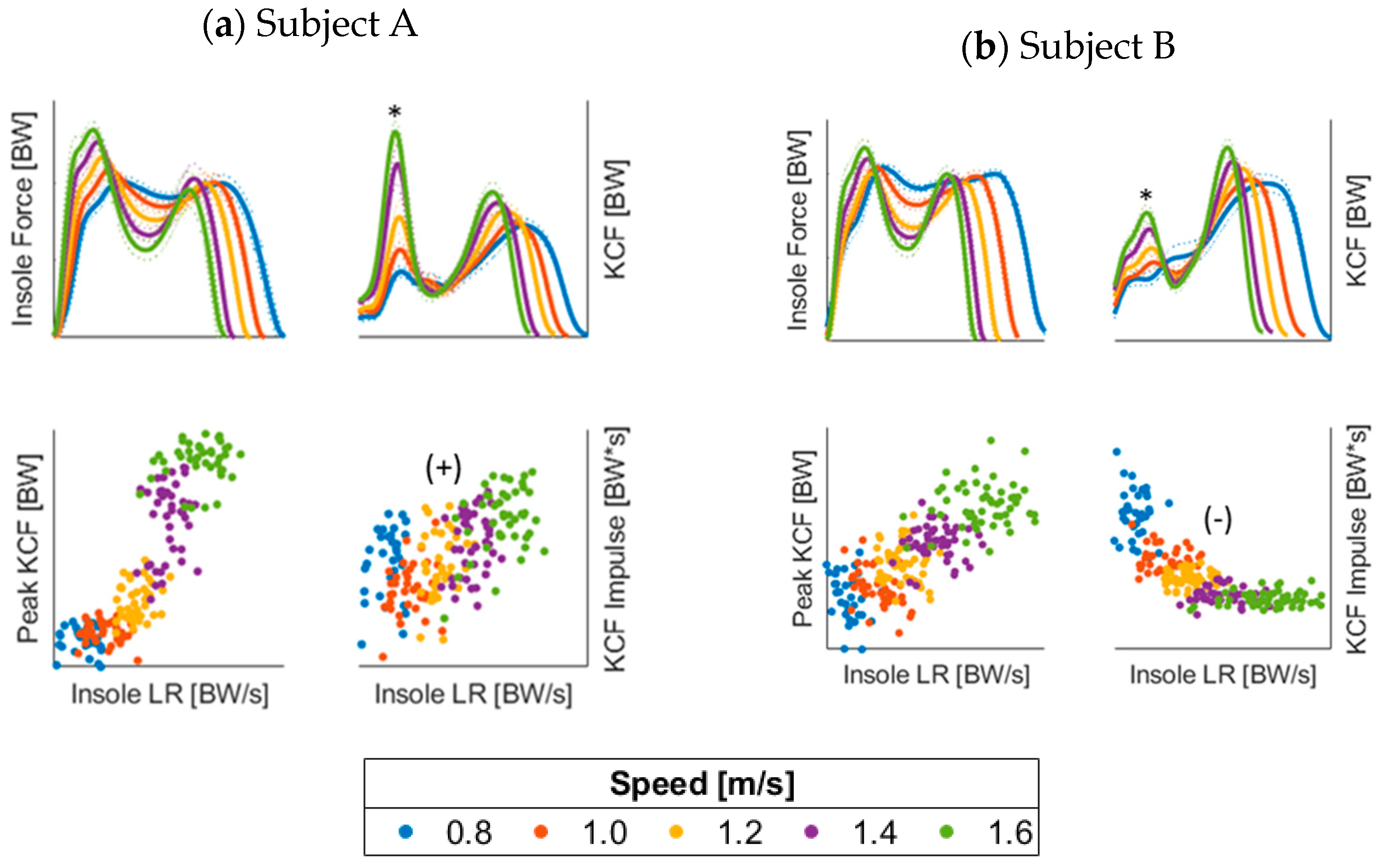
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Feature Descriptions and Illustrations
| 1-Stance Time. | 2-Peak Magnitude | ||
 | Description Total time with force > 20 N | 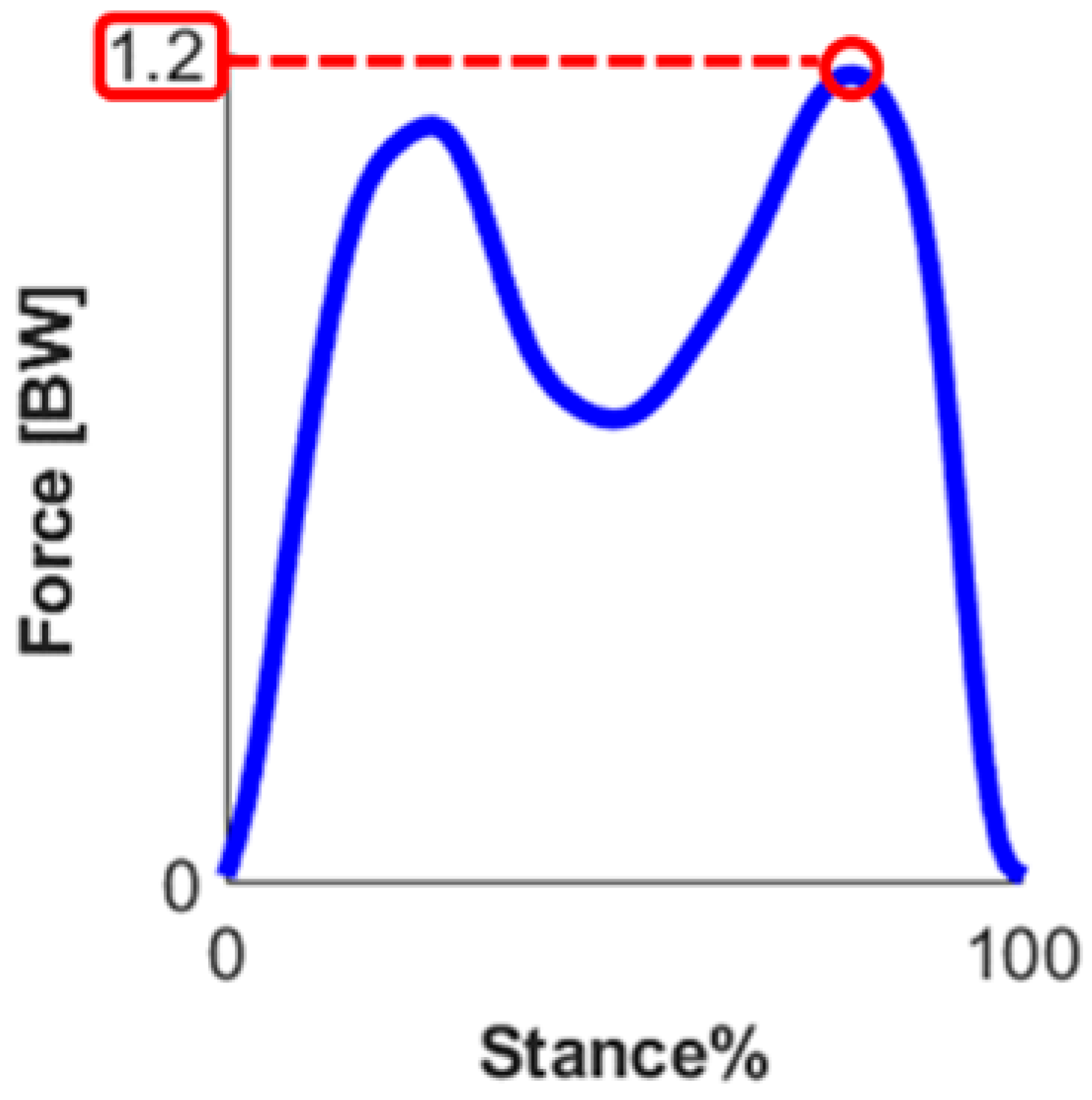 | Description Maximum force during stance |
| Equation | Equation | ||
| Units second | Units Bodyweight | ||
| 3-Impulse | |||
 | Description Total area under force curve during stance | ||
| Equation where | |||
| Units Bodyweight ∗ second | |||
| 4-Loading Rate | |||
 | Description Slope of the foot-contact-force curve from 3–12% of stance | ||
| Equation | |||
| Units Bodyweight/second | |||
| 5-Impact Peak Magnitude | 6-Mid-Drop Magnitude | ||
 | Description Force at impact peak location (if no peak, then 15% of stance) |  | Description Max-normalized force at mid-drop location (local min from 40–60% of stance) |
| Equation | Equation | ||
| Units Bodyweight | Units None (0–1) | ||
| 7-Skewness | |||
 | Description Sample skewness of the force data | ||
| Equation where | |||
| Units None | |||
 | 8- Weight Acceptance (WAC) Impulse | ||
| Description Impulse in weight acceptance phase of gait | |||
| Equation where N = # points during WAC phase | |||
| Units Bodyweight ∗ second | |||
| 9-Propulsive (Prop) Impulse | |||
| Description Impulse in propulsive phase of gait | |||
| Equation where N = # points during Prop phase | |||
| Units Bodyweight ∗ second | |||
| 10-WAC/Prop Impulse Ratio | |||
| Description Ratio of impulse from WAC and Prop phases of gait | |||
| Equation | |||
| Units None | |||
| 11-Symmetry | |||
 | Description Symmetry of insole force signal | ||
| Equation where A = original signal B = flipped signal µ = mean σ = standard deviation | |||
| Units None | |||
| 12-Frequency @ Max DFT Magnitude | 13-Mean Pseudo-Frequency | ||
 | Description Frequency with greatest DFT magnitude | 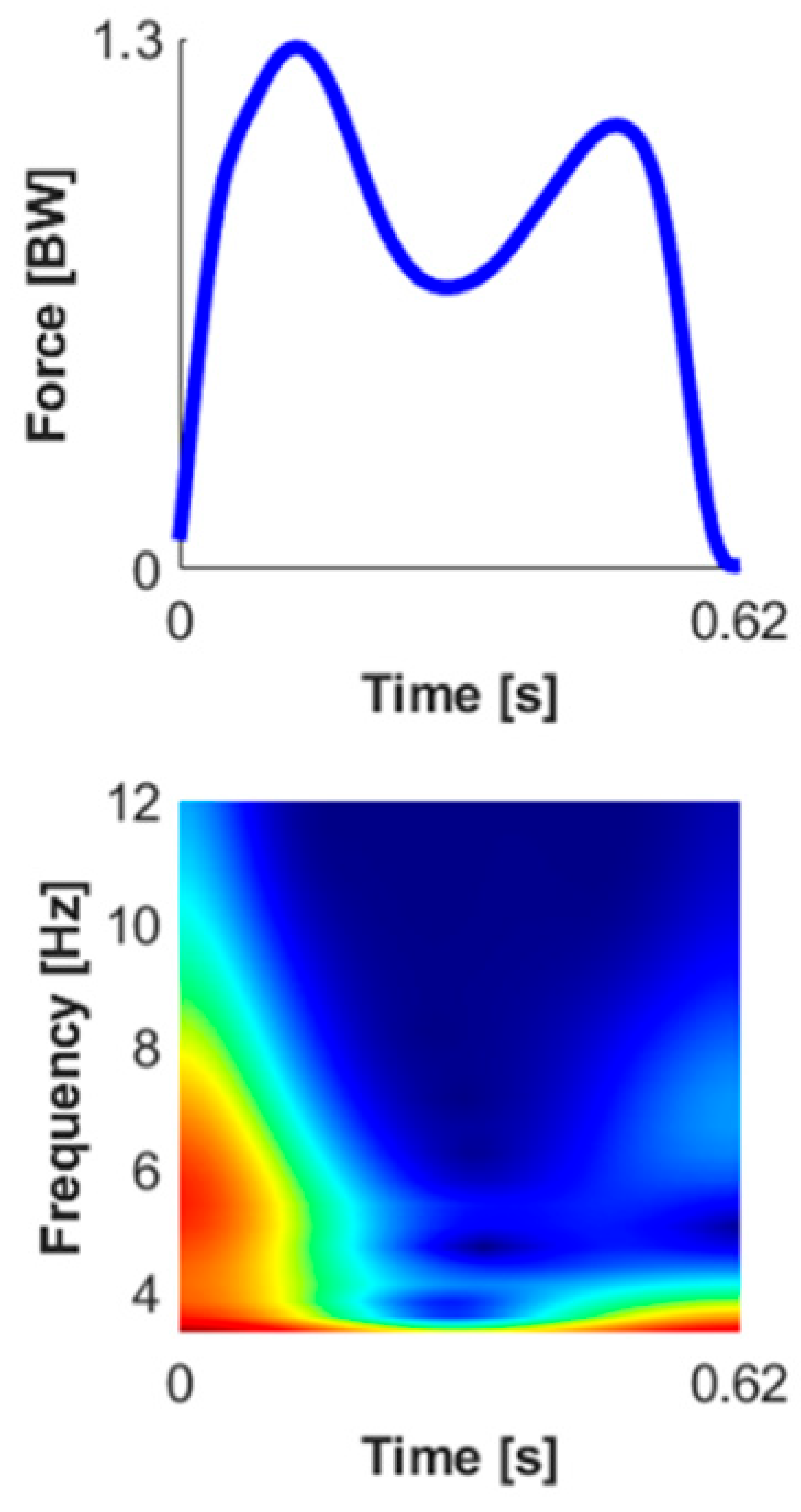 | Description Average pseudo-frequency using Mexican hat wavelet |
| Equation | Equation See [32] | ||
| Units Hz | Units ~Hz | ||
Appendix B. Individual Correlation Coefficients
Appendix B.1. KCF and Traditional Metrics

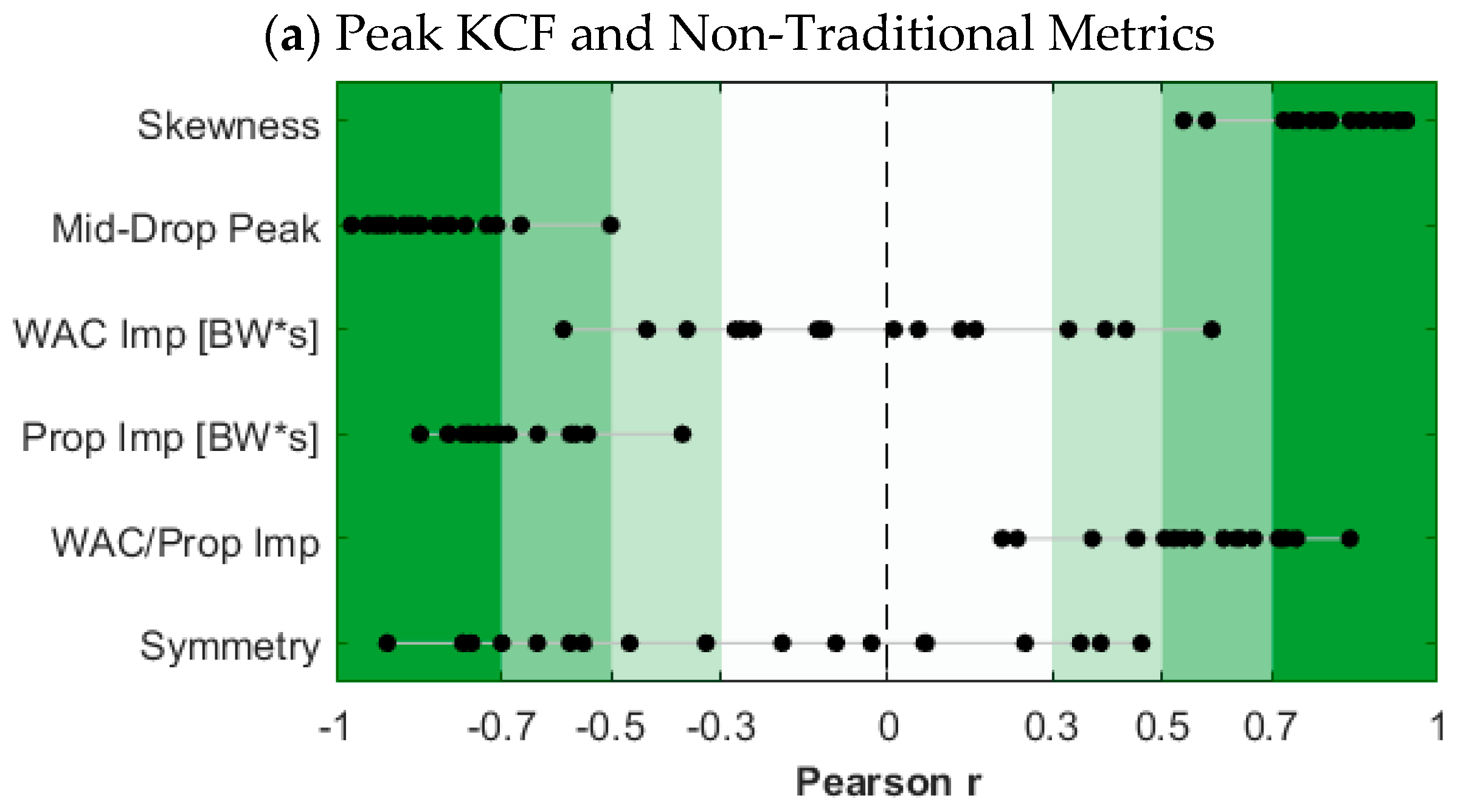
Appendix B.2. KCF and Non-Traditional Metrics

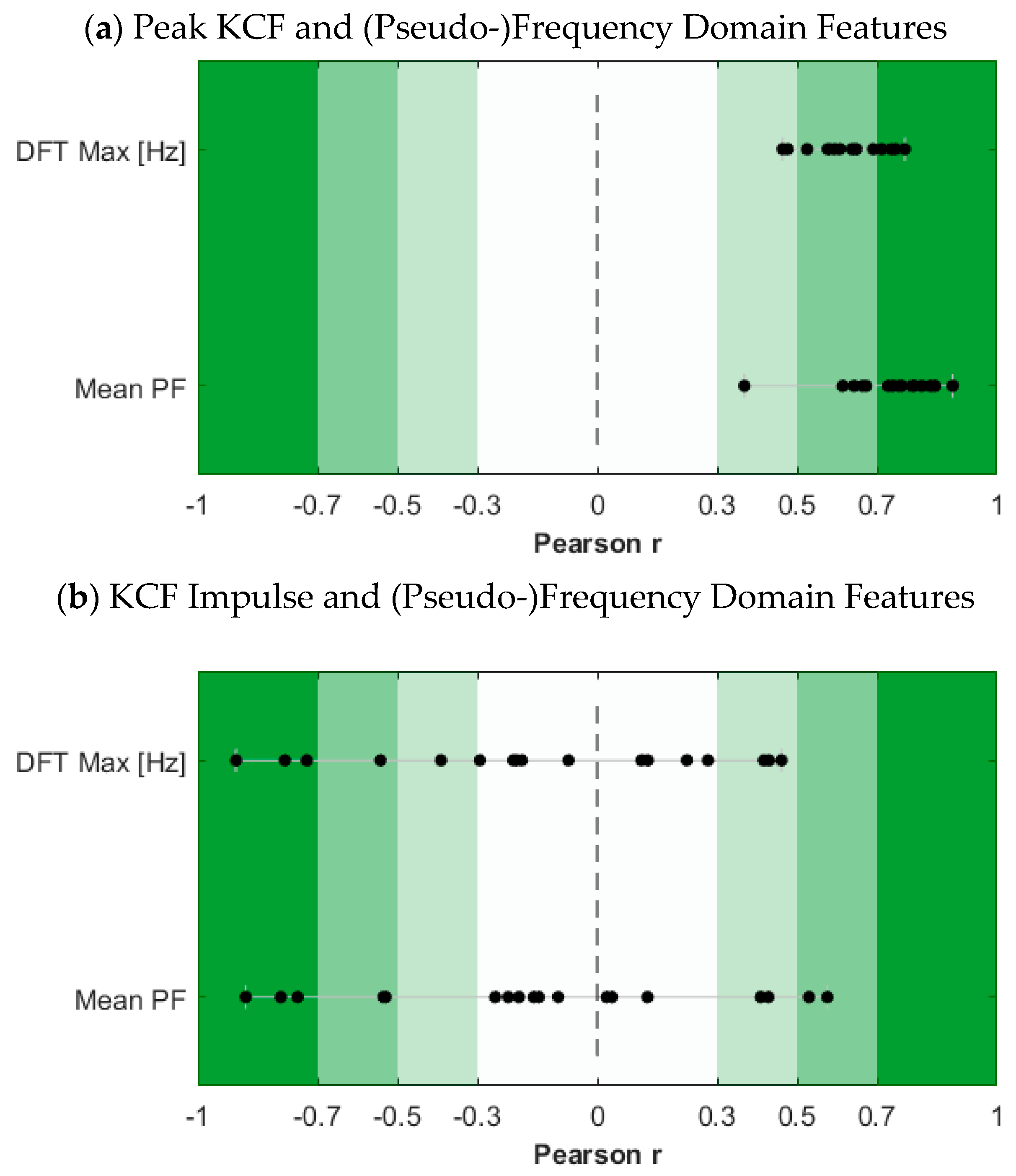
Appendix B.3. Frequency Domain Features
References
- Taylor, S.J.G.; Walker, P.S.; Perry, J.S.; Cannon, S.R.; Woledge, R. The forces in the distal femur and the knee during walking and other activities measured by telemetry. J. Arthroplast. 1998, 13, 428–437. [Google Scholar] [CrossRef] [PubMed]
- D’Lima, D.D.; Patil, S.; Steklov, N.; Slamin, J.E.; Colwell, C.W.J. The Chitranjan Ranawat Award: In Vivo Knee Forces after Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 2005, 440, 45–49. [Google Scholar] [CrossRef]
- D’Lima, D.D.; Steklov, N.; Patil, S.; Colwell, C.W. The Mark Coventry Award: In Vivo Knee Forces During Recreation and Exercise after Knee Arthroplasty. Clin. Orthop. Relat. Res. 2008, 466, 2605–2611. [Google Scholar] [CrossRef]
- D’Lima, D.D.; Patil, S.; Steklov, N.; Slamin, J.E.; Colwell, C.W. Tibial Forces Measured In Vivo After Total Knee Arthroplasty. J. Arthroplast. 2006, 21, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Banks, S.A.; D’Lima, D.D.; Colwell, C.W., Jr.; Fregly, B.J. In vivo medial and lateral tibial loads during dynamic and high flexion activities. J. Orthop. Res. 2007, 25, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Kutzner, I.; Heinlein, B.; Graichen, F.; Bender, A.; Rohlmann, A.; Halder, A.; Beier, A.; Bergmann, G. Loading of the knee joint during activities of daily living measured in vivo in five subjects. J. Biomech. 2010, 43, 2164–2173. [Google Scholar] [CrossRef]
- Kirking, B.; Krevolin, J.; Townsend, C.; Colwell, C.W.; D’Lima, D.D. A multiaxial force-sensing implantable tibial prosthesis. J. Biomech. 2006, 39, 1744–1751. [Google Scholar] [CrossRef]
- Ehlen, K.A.; Ii, R.F.R.; Browning, R.C. Energetics and biomechanics of inclined treadmill walking in obese adults. Med. Sci. Sports Exerc. 2011, 43, 1251–1259. [Google Scholar] [CrossRef]
- DeVita, P.; Hortobágyi, T. Obesity is not associated with increased knee joint torque and power during level walking. J. Biomech. 2003, 36, 1355–1362. [Google Scholar] [CrossRef]
- Zhao, D.; Banks, S.A.; Mitchell, K.H.; D’Lima, D.D.; Colwell, C.W., Jr.; Fregly, B.J. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J. Orthop. Res. 2007, 25, 789–797. [Google Scholar] [CrossRef]
- Lelas, J.L.; Merriman, G.J.; Riley, P.O.; Kerrigan, D.C. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture 2003, 17, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Neptune, R.R. Individual Muscle Contributions to the Axial Knee Joint Contact Force during Normal Walking. J. Biomech. 2010, 43, 2780–2784. [Google Scholar] [CrossRef] [PubMed]
- Shim, V.; Besier, T.; Lloyd, D.; Mithraratne, K.; Fernandez, J. The influence and biomechanical role of cartilage split line pattern on tibiofemoral cartilage stress distribution during the stance phase of gait. Biomech. Model. Mechanobiol. 2015, 15, 195–204. [Google Scholar] [CrossRef]
- Smith, C.R.; Choi, K.W.; Negrut, D.; Thelen, D.G. Efficient Computation of Cartilage Contact Pressures within Dynamic Simulations of Movement. Comput. Methods Biomech. Biomed. Eng. Imaging Vis. 2018, 6, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Atmaca, H.; Kesemenli, C.C.; Memişoğlu, K.; Özkan, A.; Celik, Y. Changes in the loading of tibial articular cartilage following medial meniscectomy: A finite element analysis study. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2667–2673. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Lee, S.; Yoon, J.; Chae, S.-W. Finite element analysis of knee and ankle joint during gait based on motion analysis. Med. Eng. Phys. 2019, 63, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Vaziri, A.; Nayeb-Hashemi, H.; Singh, A.; Tafti, B.A. Comparison between kinetic and kinetic-kinematic driven knee joint finite element models. Sci. Rep. 2018, 8, 17351. [Google Scholar] [CrossRef]
- Qi, Y.; Sun, H.; Fan, Y.; Li, F.; Wang, Y.; Ge, C. Three dimensional finite element analysis of the influence of posterior tibial slope on the anterior cruciate ligament and knee joint forward stability. J. Back Musculoskelet. Rehabil. 2018, 31, 629–636. [Google Scholar] [CrossRef]
- Weng, P.W.; Chen, C.H.; Luo, C.A.; Sun, J.S.; Tsuang, Y.H.; Cheng, C.K.; Lin, S.C. The effects of tibia profile, distraction angle, and knee load on wedge instability and hinge fracture: A finite element study. Med. Eng. Phys. 2017, 42, 48–54. [Google Scholar] [CrossRef]
- Nakamachi, E.; Noma, T.; Nakahara, K.; Tomita, Y.; Morita, Y. Multi-Photon Microscope Measurement Based Biphasic Multi-Scale Analyses of Knee Joint Articular Cartilage and Chondrocyte by Using Visco-Anisotropic Hyperelastic Finite Element Method and Smoothed Particle Hydrodynamics Method: Biphasic Multi-Scale Analyses of Chondrocyte in Articular Cartilage. Int. J. Numer. Methods Biomed. Eng. 2017, 33, e02864. [Google Scholar] [CrossRef]
- Trad, Z.; Barkaoui, A.; Chafra, M.; Tavares, J.M.R. Finite element analysis of the effect of high tibial osteotomy correction angle on articular cartilage loading. Proc. Inst. Mech. Eng. H 2018, 232, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Halonen, K.S.; Mononen, M.E.; Jurvelin, J.S.; Töyräs, J.; Salo, J.; Korhonen, R.K. Deformation of articular cartilage during static loading of a knee joint—Experimental and finite element analysis. J. Biomech. 2014, 47, 2467–2474. [Google Scholar] [CrossRef]
- Kiapour, A.; Kiapour, A.M.; Kaul, V.; Quatman, C.E.; Wordeman, S.C.; Hewett, T.E.; Demetropoulos, C.K.; Goel, V.K. Finite Element Model of the Knee for Investigation of Injury Mechanisms: Development and Validation. J. Biomech. Eng. 2014, 136, 011002. [Google Scholar] [CrossRef] [PubMed]
- Peebles, A.T.; Maguire, L.A.; Renner, K.E.; Queen, R.M. Validity and Repeatability of Single-Sensor Loadsol Insoles during Landing. Sensors 2018, 18, 4082. [Google Scholar] [CrossRef] [PubMed]
- Peebles, A.T.; Ford, K.R.; Taylor, J.B.; Hart, J.M.; Sands, L.P.; Queen, R.M. Using force sensing insoles to predict kinetic knee symmetry during a stop jump. J. Biomech. 2019, 95, 109293. [Google Scholar] [CrossRef]
- Kline, P.W.; Morgan, K.; Johnson, D.L.; Ireland, M.L.; Noehren, B. Impaired quadriceps rate of torque development and knee mechanics after anterior cruciate ligament reconstruction with patellar tendon autograft. Am. J. Sports Med. 2015, 43, 2553–2558. [Google Scholar] [CrossRef]
- Delp, S.L.; Anderson, F.C.; Arnold, A.S.; Loan, P.; Habib, A.; John, C.T.; Guendelman, E.; Thelen, D.G. OpenSim: Open-Source Software to Create and Analyze Dynamic Simulations of Movement. IEEE Trans. Biomed. Eng. 2007, 54, 1940–1950. [Google Scholar] [CrossRef]
- Anderson, F.C.; Pandy, M.G. Static and dynamic optimization solutions for gait are practically equivalent. J. Biomech. 2001, 34, 153–161. [Google Scholar] [CrossRef]
- Steele, K.M.; DeMers, M.S.; Schwartz, M.S.; Delp, S.L. Compressive Tibiofemoral Force during Crouch Gait. Gait Posture 2012, 35, 556–560. [Google Scholar] [CrossRef]
- Morley, S.K.; Brito, T.V.; Welling, D.T. Measures of Model Performance Based On the Log Accuracy Ratio. Space Weather 2018, 16, 69–88. [Google Scholar] [CrossRef]
- Luc-Harkey, B.A.; Franz, J.R.; Losina, E.; Pietrosimone, B. Association between Kinesiophobia and Walking Gait Characteristics in Physically Active Individuals with Anterior Cruciate Ligament Reconstruction. Gait Posture 2018, 64, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Gruber, A.H.; Edwards, W.B.; Hamill, J.; Derrick, T.R.; Boyer, K.A. A comparison of the ground reaction force frequency content during rearfoot and non-rearfoot running patterns. Gait Posture 2017, 56, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Tsai, Y.; Wu, P.; Lien, Y.; Chien, C.; Kuo, C.H.; Hung, J.; Chen, S.; Kuo, C. Predictive modeling of blood pressure during hemodialysis: A comparison of linear model, random forest, support vector regression, XGBoost, LASSO regression and ensemble method. Comput. Methods Programs Biomed. 2020, 195, 105536. [Google Scholar] [CrossRef]
- Shehadeh, A.; Alshboul, O.; Mamlook, R.E.A.; Hamedat, O. Machine learning models for predicting the residual value of heavy construction equipment: An evaluation of modified decision tree, LightGBM, and XGBoost regression. Autom. Constr. 2021, 129, 103827. [Google Scholar] [CrossRef]
- Banga, A.; Ahuja, R.; Sharma, S. Performance analysis of regression algorithms and feature selection techniques to predict PM2.5 in smart cities. Int. J. Syst. Assur. Eng. Manag. 2021. [Google Scholar] [CrossRef]
- Guo, Y.; Ma, H.; Tian, S. Quantitative investment model based on LightGBM algorithm. Acad. J. Comput. Inf. Sci. 2022, 5, 40–46. [Google Scholar] [CrossRef]
- Xiao, F.; Wang, Y.; He, L.; Wang, H.; Li, W.; Zhengshi, L. Motion Estimation From Surface Electromyogram Using Adaboost Regression and Average Feature Values. IEEE Access 2019, 7, 13121–13134. [Google Scholar] [CrossRef]
- Saxby, D.J.; Modenese, L.; Bryant, A.L.; Gerus, P.; Killen, B.; Fortin, K.; Wrigley, T.V.; Bennell, K.L.; Cicuttini, F.M.; Lloyd, D.G. Tibiofemoral contact forces during walking, running and sidestepping. Gait Posture 2016, 49, 78–85. [Google Scholar] [CrossRef]
- Winby, C.R.; Lloyd, D.G.; Besier, T.F.; Kirk, T.B. Muscle and external load contribution to knee joint contact loads during normal gait. J. Biomech. 2009, 42, 2294–2300. [Google Scholar] [CrossRef]
- Tsai, L.-C.; McLean, S.; Colletti, P.M.; Powers, C.M. Greater muscle co-contraction results in increased tibiofemoral compressive forces in females who have undergone anterior cruciate ligament reconstruction. J. Orthop. Res. 2012, 30, 2007–2014. [Google Scholar] [CrossRef]
| Time Domain—Traditional | Time Domain—Other | (Pseudo) Frequency Domain |
|---|---|---|
| Stance Time [s] | Skewness | DFT Max [Hz] |
| Peak Magnitude [BW] | Mid-Drop Peak Magnitude | Mean PF |
| Impulse [BW×s] | WAC Impulse [BW×s] | |
| Loading Rate [BW/s] | Prop. Impulse [BW×s] | |
| IP Magnitude [BW] | WAC/Prop. Impulse Symmetry |
| KCF Impulse | Peak KCF | |||
|---|---|---|---|---|
| MSA [%] | Num. Predictors | MSA [%] | # Predictors | |
| Per Limb | 2.19 (1.65–2.54) | 8.0 (7.0–8.8) | 3.50 (2.78–5.09) | 7.0 (5.3–8.0) |
| Per Subject | 3.40 (2.87–4.24) | 9.0 (7.0–9.0) | 6.47 (5.07–11.06) | 8.0 (7.0–9.0) |
| Peak KCF | KCF Impulse | ||
|---|---|---|---|
| Time Domain [Traditional] | Stance Time [s] | −0.84 ± 0.05 *** | 0.09 ± 0.48 |
| Peak [BW] | 0.87 ± 0.09 *** | 0.14 ± 0.40 | |
| Impulse [BW×s] | −0.76 ± 0.07 *** | 0.11 ± 0.48 | |
| Loading Rate [BW/s] | 0.80 ± 0.24 *** | 0.11 ± 0.44 | |
| IP Magnitude [BW] | 0.62 ± 0.16 ** | 0.09 ± 0.34 | |
| Time Domain [Other] | Skewness | 0.81 ± 0.12 *** | 0.20 ± 0.41 |
| Mid-Drop Peak | −0.82 ± 0.12 *** | −0.10 ± 0.46 | |
| WAC Imp [BW×s] | −0.05 ± 0.34 | 0.08 ± 0.19 | |
| Prop Imp [BW×s] | −0.66 ± 0.14 ** | 0.09 ± 0.42 | |
| WAC/Prop Impulse | 0.56 ± 0.17 ** | −0.02 ± 0.33 | |
| Symmetry | −0.24 ± 0.44 | −0.03 ± 0.25 | |
| (Pseudo) Frequency Domain | DFT Max [Hz] | 0.63 ± 0.09 ** | −0.14 ± 0.42 |
| Mean PF | 0.73 ± 0.12 *** | −0.14 ± 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spencer, A.; Samaan, M.; Noehren, B. Monitoring Knee Contact Force with Force-Sensing Insoles. Sensors 2023, 23, 4900. https://doi.org/10.3390/s23104900
Spencer A, Samaan M, Noehren B. Monitoring Knee Contact Force with Force-Sensing Insoles. Sensors. 2023; 23(10):4900. https://doi.org/10.3390/s23104900
Chicago/Turabian StyleSpencer, Alex, Michael Samaan, and Brian Noehren. 2023. "Monitoring Knee Contact Force with Force-Sensing Insoles" Sensors 23, no. 10: 4900. https://doi.org/10.3390/s23104900
APA StyleSpencer, A., Samaan, M., & Noehren, B. (2023). Monitoring Knee Contact Force with Force-Sensing Insoles. Sensors, 23(10), 4900. https://doi.org/10.3390/s23104900







