Novel Fluticasone Propionate and Salmeterol Fixed-Dose Combination Nano-Encapsulated Particles Using Polyamide Based on L-Lysine
Abstract
:1. Introduction
2. Results and Discussion
2.1. Synthesis of Polyamide from Lysine and 2,5-Furyldichloride (Lys-PA)
2.2. Fluticasone Propionate and Salmeterol Xinafoate Polyamide Formula Synthesis ((FP-SAL/Lys-PA) NCs)
2.3. Fourier Transform Infrared (FTIR) Spectroscopy Analysis
2.4. Nuclear Magnetic Resonance (NMR) Spectroscopy
2.4.1. The 1H-NMR Spectrum of the Ly-PA
2.4.2. The 13C-NMR Spectrum of the Ly-PA
2.4.3. 2D-NMR Spectra of the LY-PA
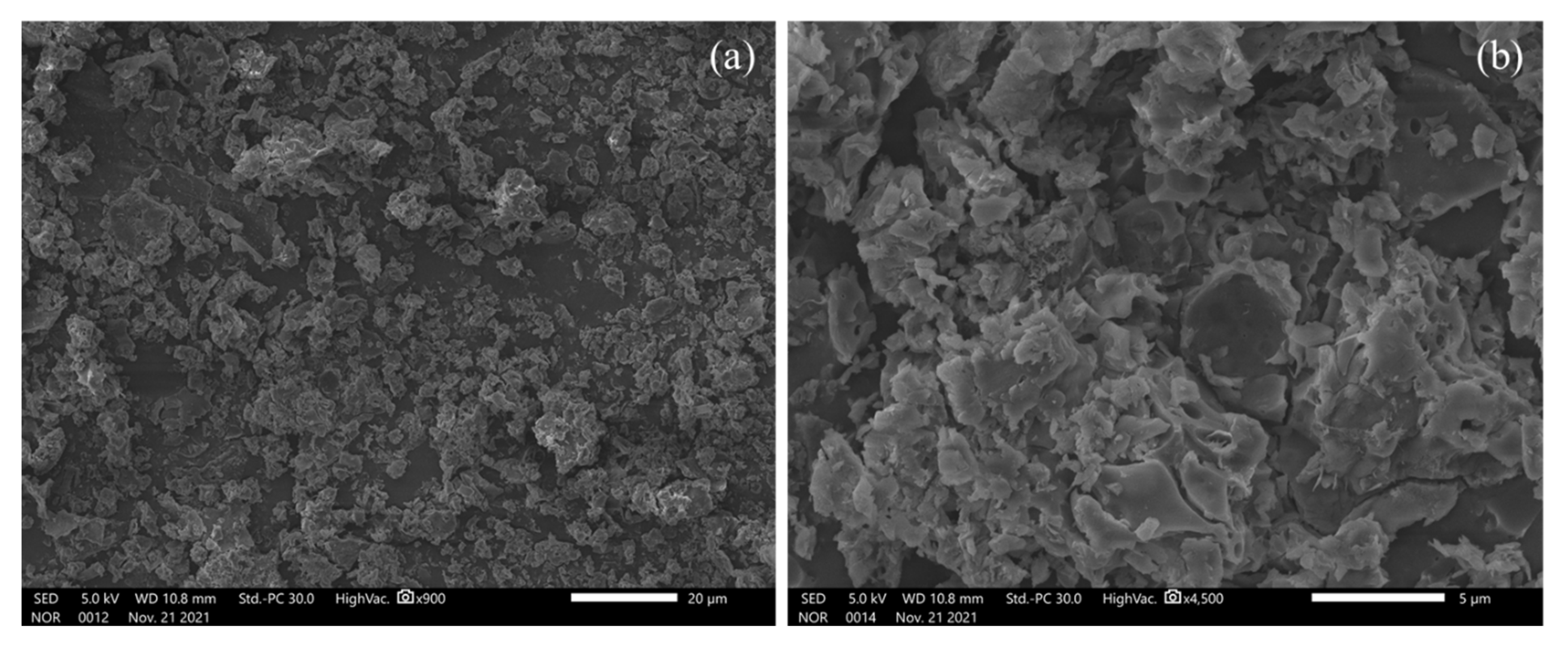
2.5. Particle Size, Zeta Potential and SEM Analysis
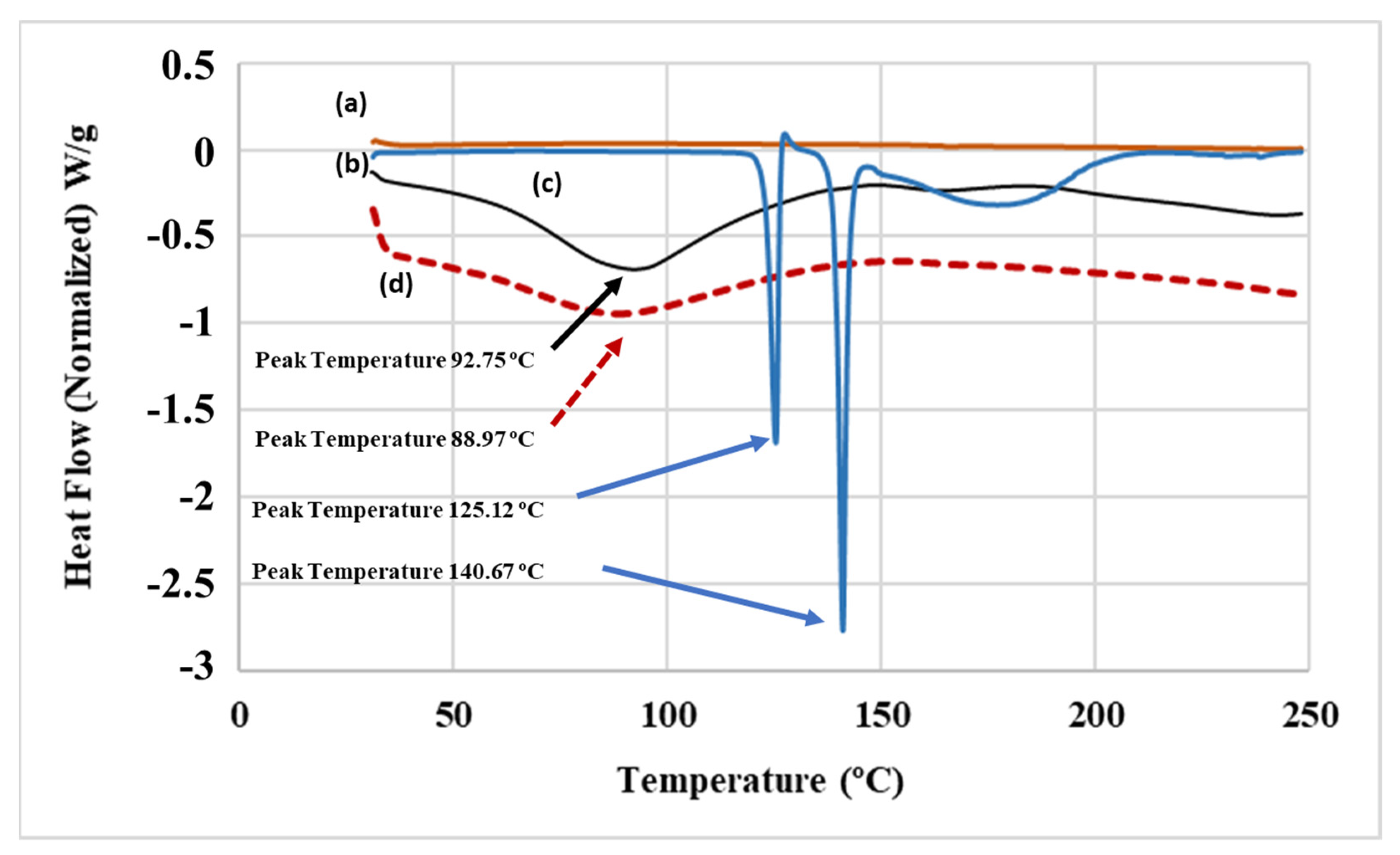
2.6. Differential Scanning Calorimetry (DSC) Analysis
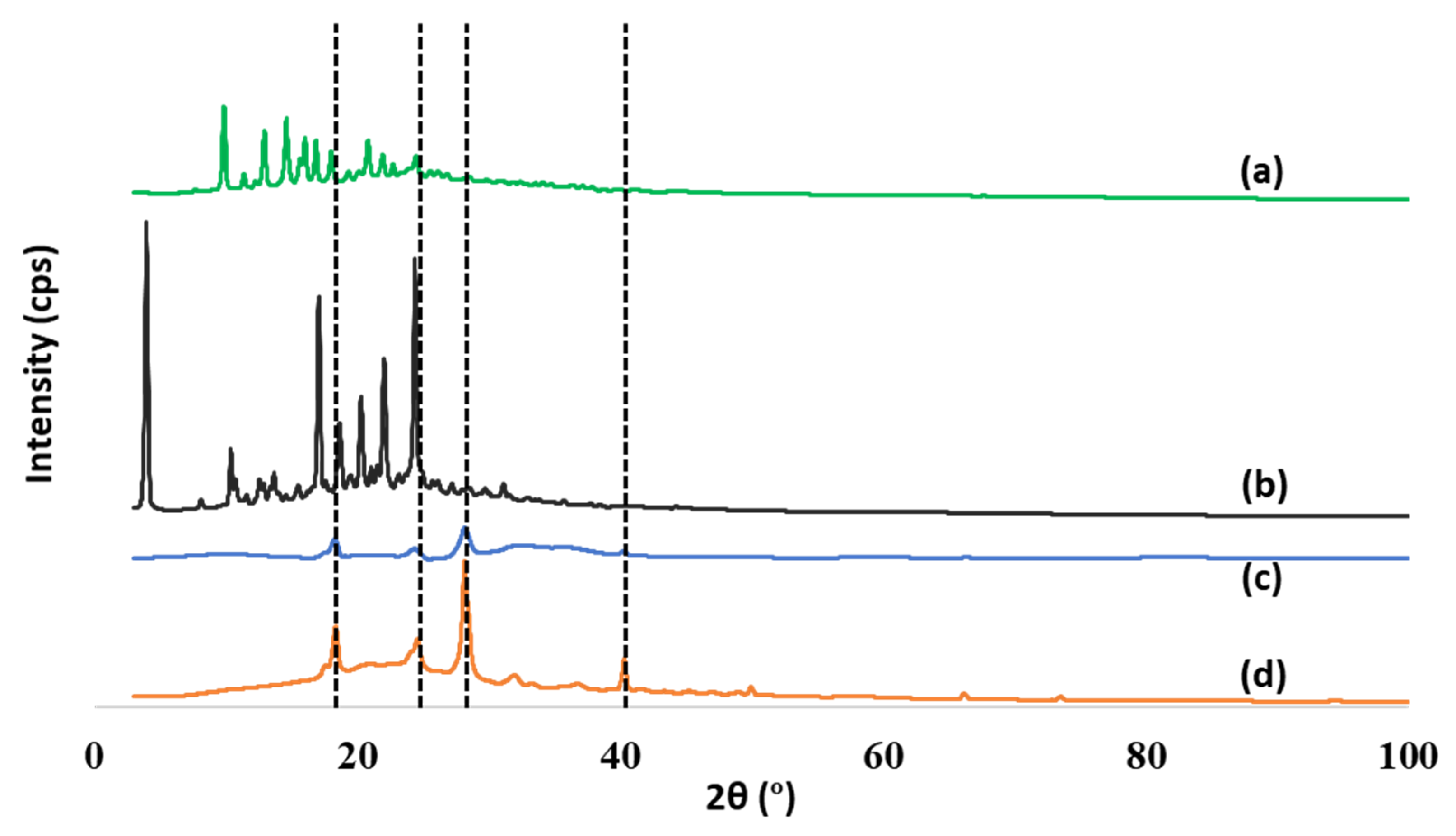
2.7. X-ray Diffraction Analysis
2.8. HPLC Method for Quantification of Thymoquinone
2.9. Pulmonary Application of the Nanocapsules
2.10. In Vitro Assessment of Aerodynamic Performance
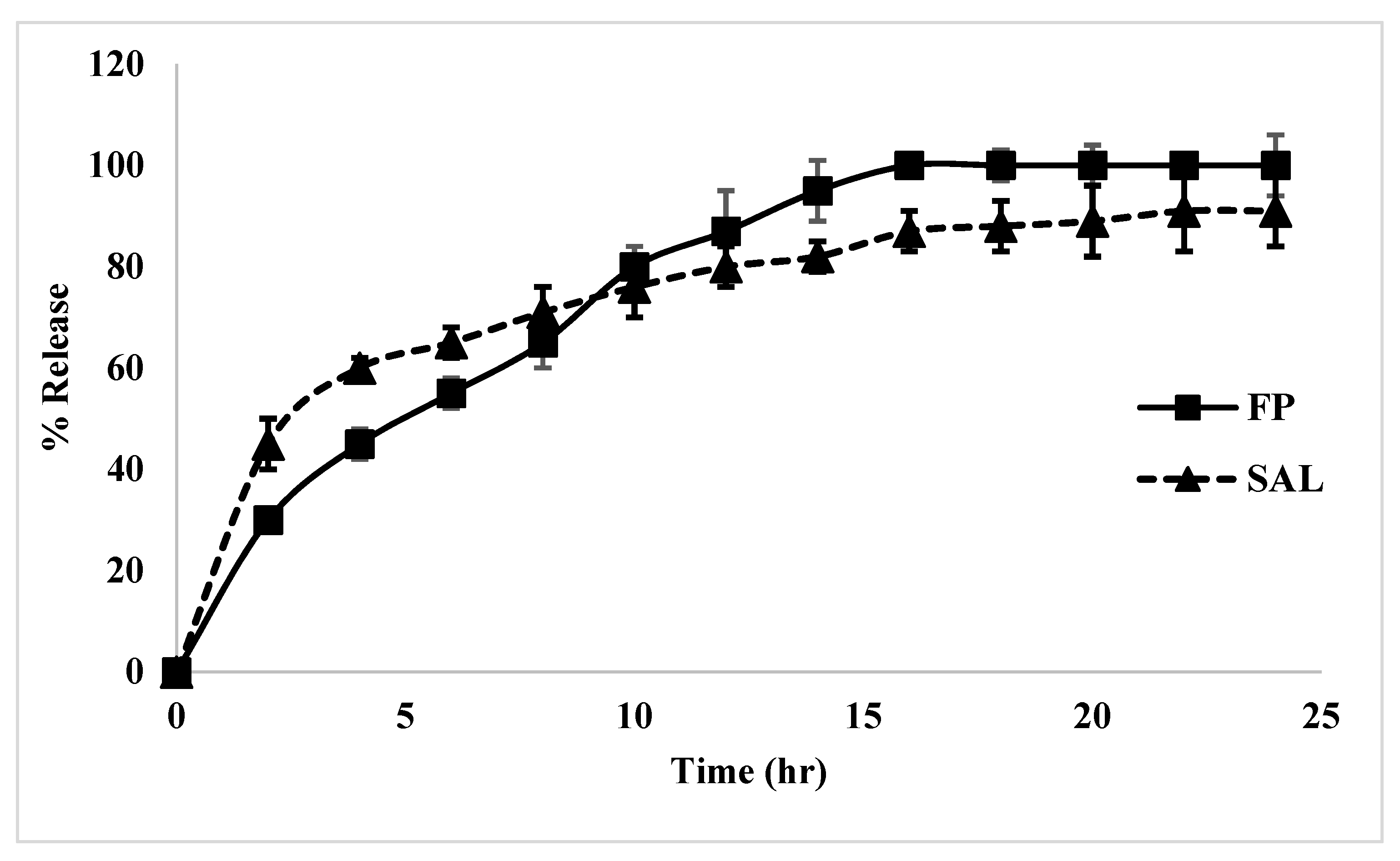
2.11. Release Study
3. Materials and Methods
3.1. Materials
3.2. Synthesis of Polyamide from Lysine and 2,5-Furyldichloride (Lys-PA)
3.3. Fluticasone Propionate and Salmeterol Xinafoate Polyamide Formula Synthesis ((FP-SAL/Lys-PA) NCs)
3.4. Nanocapsules Characterization and Profiling
3.4.1. Fourier Transform Infrared (FTIR) Spectroscopy Analysis
3.4.2. Nuclear Magnetic Resonance (NMR) Spectroscopy
3.4.3. Differential Scanning Calorimetry (DSC) Analysis
3.4.4. Particle Size Analysis
3.4.5. High Performance Liquid Chromatography (HPLC) Assay Method for FP and SAL
3.4.6. Drug Loading Capacity
3.4.7. X-ray Diffraction (XRD) Analysis
3.4.8. Scanning Electron Micrographs (SEM)
3.5. Assessment of the Performance of the (FP-SAL/Lys-PA) NCs
3.5.1. Aerodynamic Performance Using a Next Generation Impactor (NGI)
3.5.2. Release Study
3.6. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Busse, W.W.; Shah, S.R.; Somerville, L.; Parasuraman, B.; Martin, P.; Goldman, M. Comparison of adjustable- and fixed-dose budesonide/formoterol pressurized metered-dose inhaler and fixed-dose fluticasone propionate/salmeterol dry powder inhaler in asthma patients. J. Allergy Clin. Immunol. 2008, 121, 1407–1414. [Google Scholar] [CrossRef] [PubMed]
- Cazzola, M.; Matera, M.G. Fixed-dose combination inhalers. In Pharmacology and Therapeutics of Asthma and COPD; Springer: Berlin/Heidelberg, Germany, 2016; pp. 117–129. [Google Scholar]
- Bender, B.; Milgrom, H.; Rand, C. Nonadherence in asthmatic patients: Is there a solution to the problem? Ann. Allergy Asthma Immunol. 1997, 79, 177–187. [Google Scholar] [CrossRef]
- Stoloff, S.W.; Stempel, D.A.; Meyer, J.; Stanford, R.H.; Rosenzweig, J.R.C. Improved refill persistence with fluticasone propionate and salmeterol in a single inhaler compared with other controller therapies. J. Allergy Clin. Immunol. 2004, 113, 245–251. [Google Scholar] [CrossRef] [PubMed]
- NAEPPCC Expert Panel Working Group. 2020 Focused Updates to the Asthma Management Guidelines; U.S. Department of Health & Human Services: Washington, DC, USA, 2020. [Google Scholar]
- FDA USA. FDA Review Finds no Significant Increase in Risk of Serious Asthma Outcomes with Long-Acting Beta Agonists (LABAs) Used in Combination with Inhaled Corticosteroids (ICS). 2017. Available online: https://www.fda.gov/media/109953/download (accessed on 12 January 2022).
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [Green Version]
- Dahmash, E.Z. Physicians’ Knowledge and Practices Regarding Asthma in Jordan: A Cross-Sectional Study. Front. Public Health 2021, 9, 712255. [Google Scholar] [CrossRef]
- WHO. Asthma; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Muralidharan, P.; Mallory, E.K.; Malapit, M.; Phan, H.; Ledford, J.G.; Hayes, D.; Mansour, H.M. Advanced design and development of nanoparticle/microparticle dual-drug combination lactose carrier-free dry powder inhalation aerosols. RSC Adv. 2020, 10, 41846–41856. [Google Scholar] [CrossRef]
- Price, D.; Bosnic-Anticevich, S.; Briggs, A.; Chrystyn, H.; Rand, C.; Scheuch, G.; Bousquet, J.; Inhaler Error Steering Committee. Inhaler competence in asthma: Common errors, barriers to use and recommended solutions. Respir. Med. 2013, 107, 37–46. [Google Scholar] [CrossRef] [Green Version]
- de Boer, A.H.; Hagedoorn, P.; Hoppentocht, M.; Buttini, F.; Grasmeijer, F.; Frijlink, H.W. Dry powder inhalation: Past, present and future. Expert. Opin. Drug Deliv. 2017, 14, 499–512. [Google Scholar] [CrossRef] [Green Version]
- Shi, L.; Plumley, C.J.; Berkland, C. Biodegradable nanoparticle flocculates for dry powder aerosol formulation. Langmuir 2007, 23, 10897–10901. [Google Scholar] [CrossRef]
- Wyatt, D.A.; Koner, J.S.; Dahmash, E.Z.; Mohammed, A.R. Innovation in manufacturing as applied to dry powder inhaler formulation. J. Aerosol Med. Pulm. Drug Deliv. 2019, 32, A18. [Google Scholar]
- Patil, J.S.; Sarasija, S. Pulmonary drug delivery strategies: A concise, systematic review. Lung India 2012, 29, 44–49. [Google Scholar] [PubMed]
- Fiore, V.F.; Lofton, M.C.; Roser-page, S.; Yang, S.C.; Roman, J.; Murthy, N.; Barker, T.H. Polyketal microparticles for therapeutic delivery to the lung. Biomaterials 2010, 31, 810–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loira-pastoriza, C.; Todoroff, J.; Vanbever, R. Delivery strategies for sustained drug release in the lungs. Adv. Drug Deliv. Rev. 2014, 75, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Muralidharan, P.; Malapit, M.; Mallory, E.; Hayes, D.; Mansour, H.M. Inhalable nanoparticulate powders for respiratory delivery. Nanomedicine Nanotechnology. Biol. Med. 2015, 11, 1189–1199. [Google Scholar]
- Ren, J.; Fu, H.; Ren, T.; Yuan, W. Preparation, characterization and properties of binary and ternary blends with thermoplastic starch, poly (lactic acid) and poly (butylene adipate- co -terephthalate). Carbohydr. Polym. 2009, 77, 576–582. [Google Scholar] [CrossRef]
- Zhou, C.; Li, H.; Zhang, Y.; Xue, F.; Huang, S.; Wen, H.; Li, J.; de Claville Christiansen, J.; Yu, D.; Wu, Z.; et al. Deformation and structure evolutions of glassy poly(lactic acid) below glass transition temperature. CrystEngComm 2015, 17, 5651–5663. [Google Scholar] [CrossRef]
- Garg, U.; Chauhan, S.; Nagaich, U.; Jain, N. Current Advances in Chitosan Nanoparticles Based Drug Delivery and Targeting. Adv. Pharm. Bull. 2019, 9, 195–204. [Google Scholar] [CrossRef]
- Ainali, N.M.; Xanthopoulou, E.; Michailidou, G.; Zamboulis, A.; Bikiaris, D.N. Microencapsulation of Fluticasone Propionate and Salmeterol Xinafoate in Modified Chitosan Microparticles for Release Optimization. Molecules 2020, 25, 3888. [Google Scholar] [CrossRef]
- Tsitlanadze, G.; Kviria, T.; Katsarava, R. In vitro enzymatic biodegradation of amino acid based poly (ester amide) s biomaterials. J. Mater. Sci. Mater. Med. 2004, 15, 185–190. [Google Scholar] [CrossRef]
- Bhagabati, P. Biopolymers and biocomposites-mediated sustainable high-performance materials for automobile applications. In Sustainable Nanocellulose and Nanohydrogels from Natural Sources, 1st ed.; Mohammad, F., Al-Lohedan, H., Jawaid, M., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2020; pp. 197–216. [Google Scholar]
- Ali, D.K.; Al-Zuheiri, A.M.; Sweileh, B.A. pH and reduction sensitive bio-based polyamides derived from renewable dicarboxylic acid monomers and cystine amino acid. Int. J. Polym. Anal. Charact. 2017, 22, 361–373. [Google Scholar] [CrossRef]
- Kumar, A.; Mansour, H.M.; Friedman, A.; Blough, E.R. Nanomedicine in Drug Delivery; CRC Press: Boca Raton, FL, USA, 2013. [Google Scholar]
- Mansour, H.M.; Rhee, Y.-S.; Wu, X. Nanomedicine in pulmonary delivery. Int. J. Nanomed. 2009, 4, 299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Gendy, N.; Bailey, M.M.; Berkland, C. Particle engineering technologies for pulmonary drug delivery. In Controlled Pulmonary Drug Delivery; Springer: Berlin/Heidelberg, Germany, 2011; pp. 283–312. [Google Scholar]
- Koner, J.S.; Wyatt, D.; Lungare, S.; Jones, R.; Mohammed, A.R. Extending the capability of high dose DPI formulation using a new blending technology. J. Aerosol Med. Pulm. Drug Deliv. 2020, 33, A3–A4. [Google Scholar]
- Gradon, L.; Sosnowski, T.R. Formation of particles for dry powder inhalers. Adv. Powder Technol. 2014, 25, 43–55. [Google Scholar] [CrossRef]
- Timsina, M.P.; Martin, G.P.; Marriott, C.; Ganderton, D.; Yianneskis, M. Drug delivery to the respiratory tract using dry powder inhalers. Int. J. Pharm. 1994, 101, 1–13. [Google Scholar] [CrossRef]
- Xu, R.; Xu, G.; Wang, J.; Chen, J. Influence of L -lysine on the permeation and antifouling performance of polyamide thin film. RSC Adv. 2018, 8, 25236–25247. [Google Scholar] [CrossRef] [Green Version]
- Westmeier, R.; Steckel, H. Combination particles containing salmeterol xinafoate and fluticasone propionate: Formulation and aerodynamic assessment. J. Pharm. Sci. 2008, 97, 2299–2310. [Google Scholar] [CrossRef]
- PubChem. Fluticasone Propionate. 2022. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Fluticasone-propionate (accessed on 5 January 2022).
- Amore, E.; Manca, M.L.; Ferraro, M.; Valenti, D.; La Parola, V.; Di Vincenzo, S.; Gjomarkaj, M.; Giammona, G.; Bondì, M.L.; Pace, E. Salmeterol Xinafoate (SX) loaded into mucoadhesive solid lipid microparticles for COPD treatment. Int. J. Pharm. 2019, 562, 351–358. [Google Scholar] [CrossRef]
- Surekha, R.; Sumathi, T. An efficient encapsulation of thymoquinone using solid lipid nanoparticle for brain targeted drug delivery: Physicochemical characterization, pharmacokinetics and bio-distribution studies. Int. J. Pharm. Clin. Res. 2016, 8, 1616–1624. [Google Scholar]
- Amasya, G.; TÜrk, C.T.Ş.; Badilli, U.; Tarimci, N. Development and statistical optimization of solid lipid nanoparticle formulations of fluticasone propionate. Turkish J. Pharm. Sci. 2020, 17, 359. [Google Scholar] [CrossRef]
- El-Gendy, N.; Pornputtapitak, W.; Berkland, C. Nanoparticle agglomerates of fluticasone propionate in combination with albuterol sulfate as dry powder aerosols. Eur. J. Pharm. Sci. 2011, 44, 522–533. [Google Scholar] [CrossRef] [Green Version]
- Murnane, D.; Marriott, C.; Martin, G.P. Crystallization and crystallinity of fluticasone propionate. Cryst. Growth Des. 2008, 8, 2753–2764. [Google Scholar] [CrossRef]
- Shah, N.; Kondawar, M.; Shah, R.; Shah, V. Sustained release of spray-dried combination dry powder inhaler formulation for pulmonary delivery. Asian J. Pharm. Clin. Res. 2011, 4, 112–118. [Google Scholar]
- ICH. Validation of Analytical Procedures: Text and Methodology Q2(R1); ICH Secretariat: Geneva, Switzerland, 2005. [Google Scholar]
- Dash, S.; Murthy, P.N.; Nath, L.; Chowdhury, P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol. Pharm. 2010, 67, 217–223. [Google Scholar] [PubMed]
- Bruschi, M.L. Mathematical models of drug release. In Strategies to Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Sawston, UK, 2015; pp. 63–86. [Google Scholar]
- Gouda, R.; Baishya, H.; Qing, Z. Application of mathematical models in drug release kinetics of carbidopa and levodopa ER tablets. J. Dev. Drugs 2017, 6, 1–8. [Google Scholar]
- Desoqi, M.H.; El-Sawy, H.S.; Kafagy, E.; Ghorab, M.; Gad, S. Fluticasone propionate–loaded solid lipid nanoparticles with augmented anti-inflammatory activity: Optimisation, characterisation and pharmacodynamic evaluation on rats. J. Microencapsul. 2021, 38, 177–191. [Google Scholar] [CrossRef]
- USP General Chapter <601> Aerosols, Nasal Sprays, Metered-Dose Inhalers, and Dry Powder Inhalers; United States Pharmacopea: Rockville, MD, USA, 2008.
- Nielson, D.W.; Goerke, J.; Clements, J.A. Alveolar subphase pH in the lungs of anesthetized rabbits. Proc. Natl. Acad. Sci. USA 1981, 78, 7119–7123. [Google Scholar] [CrossRef] [Green Version]
- Narashimhan, B.; Mallapragada, S.K.; Peppas, N.A. Release kinetics, data interpretation. In Encyclopedia of Controlled Drug Delivery, 1st ed.; Mathiowitz, E., Ed.; Wiley: New York, NY, USA, 1999. [Google Scholar]
- Chakraborty, S.; Pandit, J.K.; Srinatha, A. Development of extended release divalproex sodium tablets containing hypdrophobic and hydrophilic matrix. Curr. Drug Deliv. 2009, 6, 291–296. [Google Scholar] [CrossRef]





| Material | FP | SAL | Polymer | FP-SAL-Polymer Loaded NC | |
|---|---|---|---|---|---|
| Parameter | |||||
| Particle size (nm) | 2230.7 ± 200.3 | 1935.7 ± 188.9 | 199.3 ± 12.5 | 226.7 ± 35.3 | |
| Polydispersity index | 0.91 ± 0.15 | 0.57 ± 0.15 | 0.38 ± 0.21 | 0.32 ± 0.08 | |
| Zeta potential (mV) | −27.2 ± 5.8 | −18.5 ± 0.5 | −28.16 ± 1.6 | −30.6 ± 4.2 | |
| Parameter | FP | SAL |
|---|---|---|
| Calibration curve equation | ||
| Limit of detection (LOD) µg/mL | 2.04 | 0.745 |
| Limit of quantification (LOQ) µg/mL | 6.18 | 2.26 |
| Intraday % Recovery (mean ± SD) (n = 3) | ||
| • 125 µg/mL | 102.85 ± 4.69 | 100.04 ± 3.74 |
| • 31.25 µg/mL | 99.58 ± 4.25 | 99.69 ± 4.32 |
| • 3.9 µg/mL | 97.94 ± 3.02 | 100.15 ± 4.96 |
| Interday % Recovery (mean ± SD) (n = 3) | ||
| • 125 µg/mL | 98.54 ± 5.69 | 102.57 ± 4.27 |
| • 31.25 µg/mL | 101.58 ± 4.98 | 97.27 ± 5.07 |
| • 3.9 µg/mL | 98.98 ± 6.98 | 103.07 ± 4.27 |
| Precision (concentration 62.5 µg/mL) mean ± SD, RSD) (n = 10) | 98.76 ± 2.05, 2.08% | 101.24 ± 3.22, 3.18% |
| Formula | F1 (Single API) | F2 (Single API) | F3 (Double APIs) | |
|---|---|---|---|---|
| Parameter | ||||
| FP (mg, mmol) | 10 | 20 | 20 | |
| SAL (mg) | 5 | 5 | 2 | |
| EE (%) FP-SAL | 91.6–91.2 | 81.13–92.5 | 79.8–99.17 | |
| ECE (%) (FP-SAL) | 1.03–0.63 | 1.66–0.702 | 1.67–0.33 | |
| Recommended formula weight (mg) (FP-SAL) | 24.3–7.9 | 15.1–7.1 | 15 | |
| Formula | F3 | Marketed | |||
|---|---|---|---|---|---|
| Parameter | FP | SAL | FP | SAL | |
| MMAD (µm) | 1.559 | 1.778 | 1.434 | 1.524 | |
| GSD | 0.080 | 0.047 | 0.074 | 0.081 | |
| Mathematical Model | FP-R2 | SAL-R2 | FP-n | SAL-n |
|---|---|---|---|---|
| Zero order | 0.9824 | 0.9326 | ||
| First order | 0.9231 | 0.8744 | ||
| Higuchi model | 0.9935 | 0.9722 | ||
| Hixon Crowell model | 0.8872 | 0.9355 | ||
| Korsmeyer–Peppas model | 0.999 | 0.9838 | 0.5541 | 0.3176 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alyami, M.H.; Dahmash, E.Z.; Ali, D.K.; Alyami, H.S.; AbdulKarim, H.; Alsudir, S.A. Novel Fluticasone Propionate and Salmeterol Fixed-Dose Combination Nano-Encapsulated Particles Using Polyamide Based on L-Lysine. Pharmaceuticals 2022, 15, 321. https://doi.org/10.3390/ph15030321
Alyami MH, Dahmash EZ, Ali DK, Alyami HS, AbdulKarim H, Alsudir SA. Novel Fluticasone Propionate and Salmeterol Fixed-Dose Combination Nano-Encapsulated Particles Using Polyamide Based on L-Lysine. Pharmaceuticals. 2022; 15(3):321. https://doi.org/10.3390/ph15030321
Chicago/Turabian StyleAlyami, Mohammad H., Eman Zmaily Dahmash, Dalia Khalil Ali, Hamad S. Alyami, Hussien AbdulKarim, and Samar A. Alsudir. 2022. "Novel Fluticasone Propionate and Salmeterol Fixed-Dose Combination Nano-Encapsulated Particles Using Polyamide Based on L-Lysine" Pharmaceuticals 15, no. 3: 321. https://doi.org/10.3390/ph15030321







