Development of a New Ankle Joint Hybrid Assistive Limb
Abstract
:1. Introduction
2. Materials and Methods
2.1. Development and Structure of the Ankle HAL
2.2. Procedure and Function of the Ankle HAL
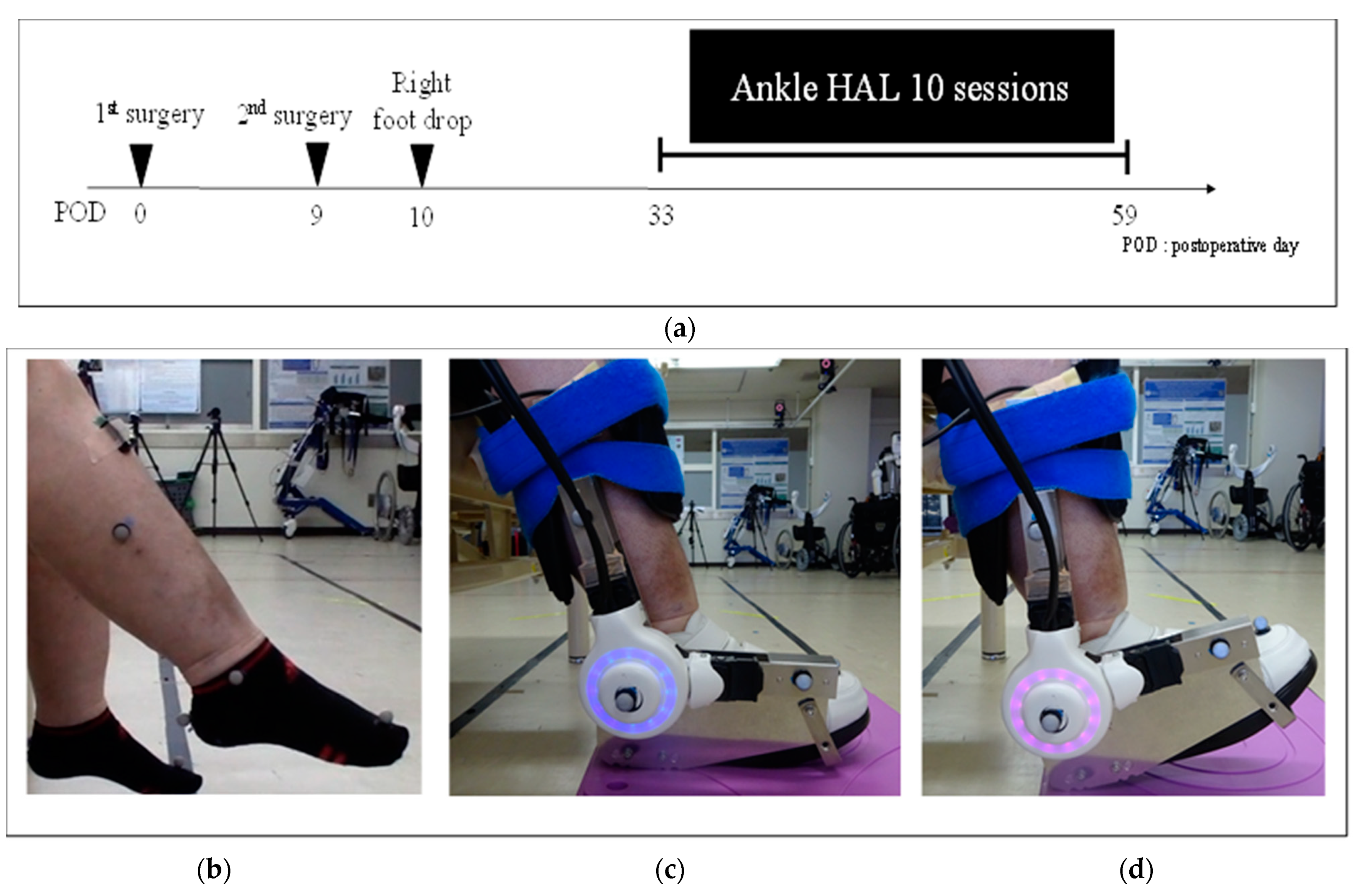
2.3. Case Presentation
2.4. Dorsiflexion Training Using the Ankle HAL
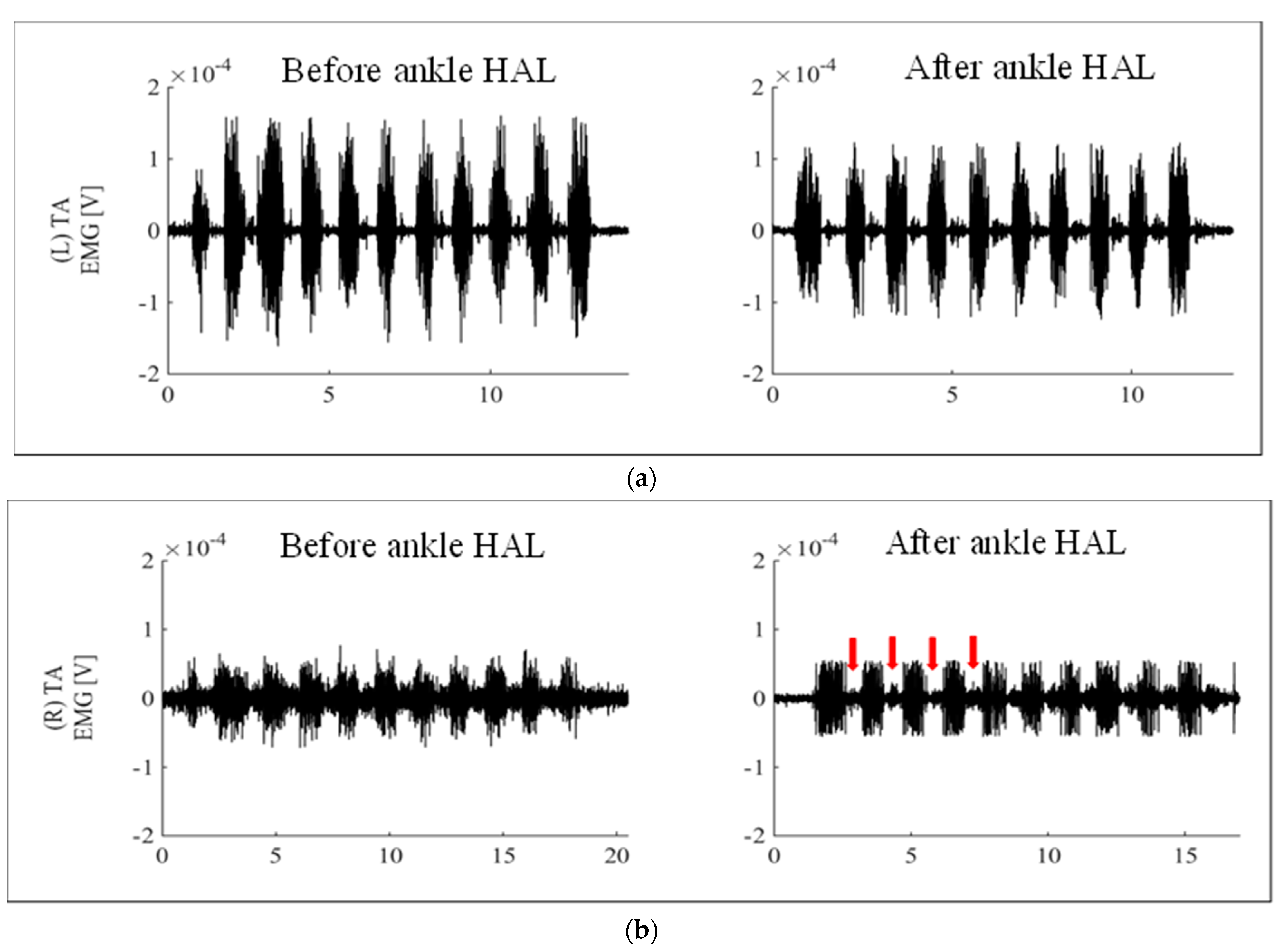
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Carolus, A.E.; Becker, M.; Cuny, J.; Smektala, R.; Schmieder, K.; Brenke, C. The interdisciplinary management of foot drop. Dtsch. Ärzteblatt Int. 2019, 116, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Lamontagne, A.; Malouin, F.; Richards, C.; Dumas, F. Mechanisms of disturbed motor control in ankle weakness during gait after stroke. Gait Posture 2002, 15, 244–255. [Google Scholar] [CrossRef]
- Stewart, J.D. Foot drop: Where, why and what to do? Pr. Neurol. 2008, 8, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Poage, C.; Roth, C.; Scott, B. Peroneal nerve palsy: Evaluation and management. J. Am. Acad. Orthop. Surg. 2016, 24, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Li, S. Ankle and foot spasticity patterns in chronic stroke survivors with abnormal gait. Toxins 2020, 12, 646. [Google Scholar] [CrossRef]
- Sankai, Y.; Sakurai, T. Exoskeletal cyborg-type robot. Sci. Robot. 2018, 3, eaat3912. [Google Scholar] [CrossRef]
- Kubota, S.; Abe, T.; Kadone, H.; Shimizu, Y.; Funayama, T.; Watanabe, H.; Marushima, A.; Koda, M.; Hada, Y.; Sankai, Y.; et al. Hybrid assistive limb (HAL) treatment for patients with severe thoracic myelopathy due to ossification of the posterior longitudinal ligament (OPLL) in the postoperative acute/subacute phase: A clinical trial. J. Spinal Cord Med. 2019, 42, 517–525. [Google Scholar] [CrossRef]
- Watanabe, H.; Marushima, A.; Kadone, H.; Ueno, T.; Shimizu, Y.; Kubota, S.; Hino, T.; Sato, M.; Ito, Y.; Hayakawa, M.; et al. Effects of gait treatment with a single-leg hybrid assistive limb system after acute stroke: A Non-randomized clinical trial. Front. Neurosci. 2020, 13, 1389. [Google Scholar] [CrossRef]
- Kubota, S.; Kadone, H.; Shimizu, Y.; Abe, T.; Makihara, T.; Kubo, T.; Watanabe, H.; Marushima, A.; Koda, M.; Hada, Y.; et al. Shoulder training using shoulder assistive robot in a patient with shoulder elevation dysfunction: A case report. J. Orthop. Sci. 2020, S0949-2658, 30002–30006. [Google Scholar] [CrossRef]
- Kubota, S.; Kadone, H.; Shimizu, Y.; Hara, Y.; Kubo, T.; Watanabe, H.; Hada, Y.; Ochiai, N.; Sankai, Y.; Yamazaki, M. Robotic rehabilitation training with a newly developed upper limb single-joint Hybrid Assistive Limb (HAL-SJ) for elbow flexor reconstruction after brachial plexus injury: A report of two cases. J. Orthop. Surg. 2018, 26, 2309499018777887. [Google Scholar] [CrossRef] [PubMed]
- Soma, Y.; Mutsuzaki, H.; Yoshioka, T.; Kubota, S.; Shimizu, Y.; Kanamori, A.; Yamazaki, M. Rehabilitation training using a single-joint type hybrid assistive limb for the knee after anterior cruciate ligament reconstruction: An initial case report indicating safety and feasibility. J. Phys. Ther. Sci. 2021, 33, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Miura, K.; Kadone, H.; Koda, M.; Abe, T.; Kumagai, H.; Nagashima, K.; Mataki, K.; Fujii, K.; Noguchi, H.; Funayama, T.; et al. The hybrid assistive limb (HAL) for Care Support successfully reduced lumbar load in repetitive lifting movements. J. Clin. Neurosci. 2018, 53, 276–279. [Google Scholar] [CrossRef] [PubMed]
- Liberson, W.T.; Holmquest, H.J.; Scot, D.; Dow, M. Functional electrotherapy: Stimulation of the peroneal nerve synchronized with the swing phase of the gait of hemiplegic patients. Arch. Phys. Med. Rehabil. 1961, 42, 101–105. [Google Scholar]
- Kafri, M.; Laufer, Y. Therapeutic effects of functional electrical stimulation on gait in individuals post-stroke. Ann. Biomed. Eng. 2014, 43, 451–466. [Google Scholar] [CrossRef]
- Bosch, P.R.; Harris, J.E.; Wing, K; American Congress of Rehabilitation Medicine (ACRM) Stroke Movement Interventions Subcommittee. Review of therapeutic electrical stimulation for dorsiflexion assist and orthotic substitution from the american congress of rehabilitation medicine stroke movement interventions subcommittee. Arch. Phys. Med. Rehabil. 2014, 95, 390–396. [Google Scholar] [CrossRef]
- Fatone, S.; Gard, S.; Malas, B.S. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch. Phys. Med. Rehabil. 2009, 90, 810–818. [Google Scholar] [CrossRef]
- Mulroy, S.J.; Eberly, V.J.; Gronely, J.K.; Weiss, W.; Newsam, C.J. Effect of AFO design on walking after stroke: Impact of ankle plantar flexion contracture. Prosthet. Orthot. Int. 2010, 34, 277–292. [Google Scholar] [CrossRef] [Green Version]
- Wall, A.; Borg, J.; Vreede, K.; Palmcrantz, S. A randomized controlled study incorporating an electromechanical gait machine, the Hybrid Assistive Limb, in gait training of patients with severe limitations in walking in the subacute phase after stroke. PLoS ONE 2020, 15, e0229707. [Google Scholar] [CrossRef] [Green Version]
- Wall, A.; Borg, J.; Palmcrantz, S. Clinical application of the Hybrid Assistive Limb (HAL) for gait training a systematic review. Front. Syst. Neurosci. 2015, 9, 48. [Google Scholar] [CrossRef] [Green Version]
- Yoshikawa, K.; Mizukami, M.; Kawamoto, H.; Sano, A.; Koseki, K.; Sano, K.; Asakawa, Y.; Kohno, Y.; Nakai, K.; Gosho, M.; et al. Gait training with Hybrid Assistive Limb enhances the gait functions in subacute stroke patients: A pilot study. Neurorehabilitation 2017, 40, 87–97. [Google Scholar] [CrossRef]
- Raˇdulescu, A.; Cox, K.; Adams, P. Hebbian errors in learning: An analysis using the Oja model. J. Theor. Biol. 2009, 258, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Pennycott, A.; Wyss, D.; Vallery, H.; Klamroth-Marganska, V.; Riener, R. Towards more effective robotic gait training for stroke rehabilitation: A review. J. Neuroeng. Rehabil. 2012, 9, 65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lotze, M.; Braun, C.; Birbaumer, N.; Anders, S.; Cohen, L.G. Motor learning elicited by voluntary drive. Brain 2003, 126, 866–872. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Parameter | Before Ankle HAL | After Ankle HAL |
|---|---|---|
| Dorsiflexion power (TA) (MMT) | 1 | 1 |
| Dorsiflexion power (EHL) (MMT) | 1 | 1 |
| Dorsiflexion active ROM (°) | −50 | −50 |
| Dorsiflexion passive ROM (°) | −15 | 0 |
| Gait speed (m/s) | 0.28 ± 0.04 | 0.47 ± 0.04 |
| Step length (m) | 0.23 ± 0.02 | 0.31 ± 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kubota, S.; Kadone, H.; Shimizu, Y.; Koda, M.; Noguchi, H.; Takahashi, H.; Watanabe, H.; Hada, Y.; Sankai, Y.; Yamazaki, M. Development of a New Ankle Joint Hybrid Assistive Limb. Medicina 2022, 58, 395. https://doi.org/10.3390/medicina58030395
Kubota S, Kadone H, Shimizu Y, Koda M, Noguchi H, Takahashi H, Watanabe H, Hada Y, Sankai Y, Yamazaki M. Development of a New Ankle Joint Hybrid Assistive Limb. Medicina. 2022; 58(3):395. https://doi.org/10.3390/medicina58030395
Chicago/Turabian StyleKubota, Shigeki, Hideki Kadone, Yukiyo Shimizu, Masao Koda, Hiroshi Noguchi, Hiroshi Takahashi, Hiroki Watanabe, Yasushi Hada, Yoshiyuki Sankai, and Masashi Yamazaki. 2022. "Development of a New Ankle Joint Hybrid Assistive Limb" Medicina 58, no. 3: 395. https://doi.org/10.3390/medicina58030395






