Due to the placement of the natural ostium and the difficult ascending mucociliary outflow, the maxillary sinus is the sinus most typically impacted by pathology. The function of the maxillary sinus is to significantly warm and humidify the air. Moreover, the maxillary sinus and its floor are utilized in a variety of regenerative procedures that produce a new volume of bone tissue in order to treat bone atrophy [
1]. It is also frequently affected by odontogenic infection neoplastic, traumatic, and allergy disorders. Chronic rhinosinusitis (CRS) represents one of the most prevalent diagnoses seen by an otorhinolaryngologist on a daily basis. Chronic sinusitis refers to repeated episodes of inflammation in the sinus membrane that lines the paranasal canal. This condition lasts for a minimum of 8–12 weeks and is characterized by symptoms such as congested airways, rhinorrhea, facial pain, and a disturbed sense of smell [
2]. The significant detrimental impact of rhinosinusitis on patients’ quality of life is often underestimated and neglected. Many people were previously informed that they simply had to “live with” their sinus disease [
3]. The socioeconomic effect of rhinosinusitis is an increasing subject of study. Conservative estimates US CRS expenses at over USD 30 billion per year, including USD 20 billion in indirect costs. Direct expenditures include medical visits, prescription medications, and surgery, whereas indirect costs entail lost productivity in rhinosinusitis patients [
4]. Current recommendations provide precise therapeutic indications for the treatment of CRS. Regarding surgical indication, sinus surgery should be considered for individuals with CRS who are resistant to medicinal therapy. The choice to operate should be considered in patients with symptomatic illness, excluding those with real or imminent complications, according to the recent guidelines [
5]. Since the 1980s, functional endoscopic sinus surgery (FESS) has had several designations to describe its surgical spectrum. The minimally invasive sinus technique, first published in 1996, involves simple sinus ventilation and has been shown to alleviate situations even with severe disease [
5]. FESS offers the benefit of maintaining sinus ventilation and mucociliary clearance in cases involving inflammation or infection of the sinuses. Resection of the attachment site should be performed in cases of benign sinonasal tumors, such as inverted papillomas or recurrent antrochoanal polyps, in order to prevent earlier recurrence [
6]. In basic situations, a routine uncinectomy and middle meatal antrostomy may be enough for disease visualization and clearance. However, we all too often encounter situations in which we can see substantial maxillary sinus pathology that we do not have a way to eradicate. There are few alternative options in such cases when the usual uncinectomy and middle meatal antrostomy are insufficient [
7]. Complete removal of the lesion is frequently challenging due to the instrument’s restricted reach, despite the improved visibility provided by a 70° or 90° endoscope, particularly in cases involving lesions located in the anterior or inferior wall. [
8] The removal in such case may be executed utilizing either the conventional Caldwell–Luc approach (CLA) or a canine fossa puncture. In total, 75% of patients have experienced complications associated with the canine fossa approach, which comprise pain, dental complications, and facial numbness [
9]. The Caldwell–Luc approach unfortunately, did not provide adequate access to specific maxillary sinus areas and may have resulted in infraorbital nerve injury [
10]. Due to the fact that even with specific curved equipment and angled endoscopes or a wide antrostomy diffuse disease in the maxillary sinus, such as recurring polyposis and pathologies originating from the floor or anterior wall of the maxillary sinus, cannot be eliminated fully endoscopically by middle meatal antrostomy [
11], Zhou and colleagues introduced the endoscopic intranasal prelacrimal recess approach (PLRA) to the maxillary sinus in 2007. This approach allows for broad access to the walls and recesses of the maxillary sinus while preserving the inferior turbinate and nasolacrimal duct [
12]. It affords an uninterrupted view of almost all interior maxillary linings. This enhanced visibility of the operative field may lessen the inherent limitations of endoscopic techniques. PLRA entails surgically generating a passageway by constructing a gap in the medial wall of the prelacrimal recess, which is often one of the most difficult sites to manipulate during conventional middle meatal antrostomy [
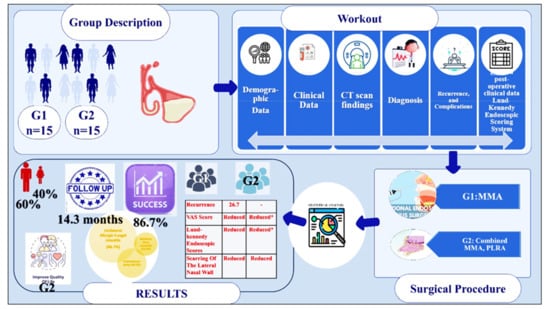
13]. The aim of this study was to assess the efficacy of endoscopic middle meatal antrostomy versus endoscopic prelacrimal recess approach and middle meatal antrostomy in the treatment of unilateral chronic maxillary sinusitis.