Biodegradable Microspheres for Transarterial Chemoembolization in Malignant Liver Disease
Abstract
:1. Introduction
2. Indications and Patient Selection
3. Product Profile and Pathophysiology
- Starch microspheres (EmboCept DMS 35/50, Embocept® (Sirtex Medical Inc., Woburn, MA, USA)): a degradable short-term embolic agent composed of starch microspheres with an average diameter of 50 micrometers. The microspheres have a half-life of about 35–50 min and are broken down by serum alpha-amylases in the blood [8,12,31]. Most currently available clinical data on DMS-TACE are based on this product.
- Gelatin microspheres (Gel-Bead, Teleflex, Morrisville, NC, USA): available in various diameters (100–300; 300–500; 500–700; and 7000–1000 μm) and presenting a degradation period between 4 and 12 weeks.
- Polylactic-co-glycolic acid (PLGA) Microspheres (Occlusin® 500 Artificial Embolization Device, IMBiotechnologies, Edmonton, AL, Canada): a hydrophobic, degradable polymer available in 150–210 μm diameter, but presenting a long-term complete degradation time (6 to 12 months). The product has obtained FDA approval for use in hypervascularized tumors with no surgical options [32].
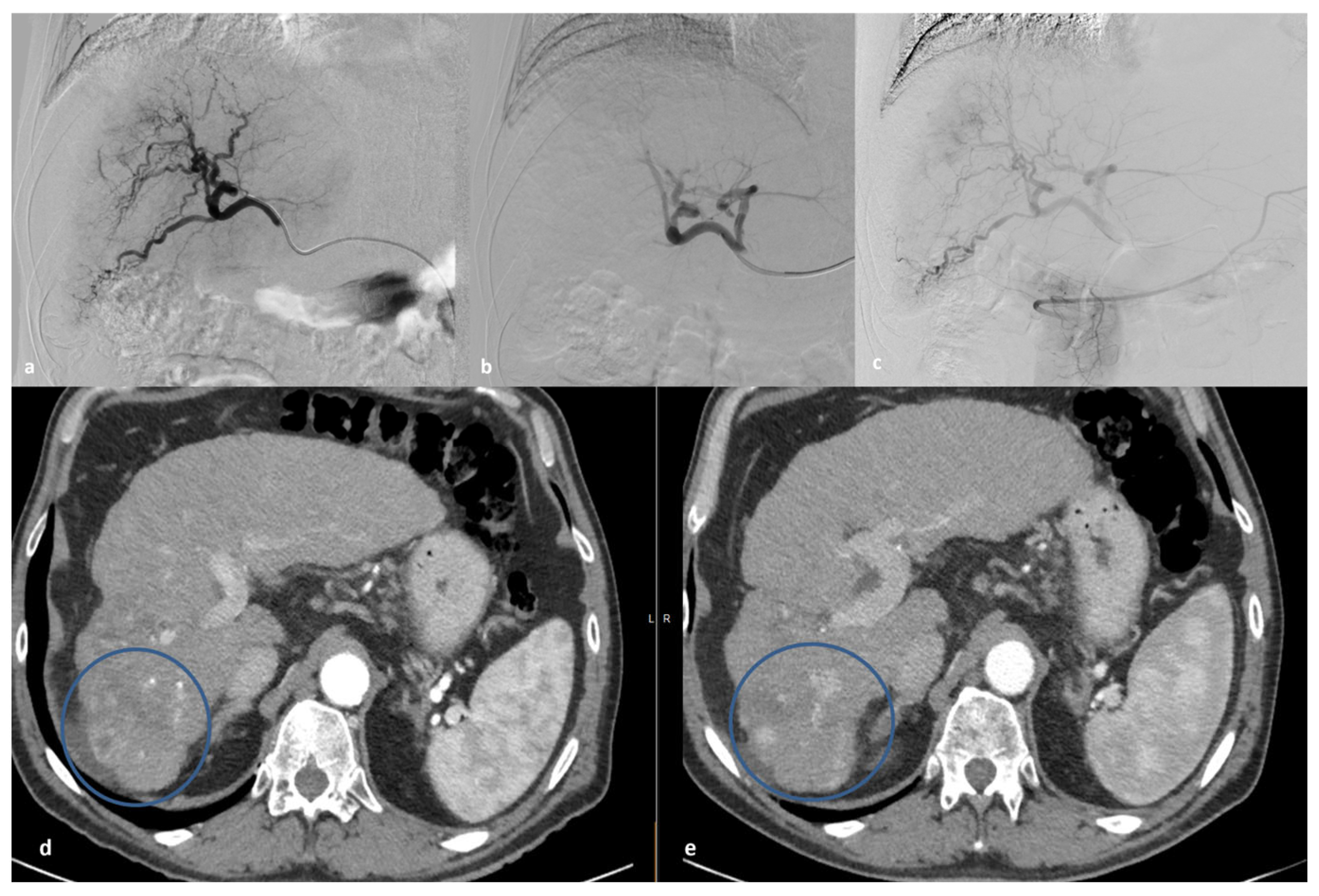
4. DMS-TACE Procedure
5. DMS-TACE Treatment: Adverse Events—Results
6. DMS-TACE Efficacy and Tumor Response—Results
6.1. HCC
6.2. ICC
6.3. Metastases
7. DMS-TACE versus Others
8. Discussion
9. Future Directions
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Håkansson, L.; Håkansson, A.; Morales, O.; Thorelius, L.; Warfving, T. Spherex (degradable starch microspheres) chemo-occlusion—Enhancement of tumor drug concentration and therapeutic efficacy: An overview. Semin. Oncol. 1997, 24, S6-100. [Google Scholar] [PubMed]
- Niessen, C.; Unterpaintner, E.; Goessmann, H.; Schlitt, H.J.; Mueller-Schilling, M.; Wohlgemuth, W.A.; Stroszczynski, C.; Wiggermann, P. Degradable Starch Microspheres versus Ethiodol and Doxorubicin in Transarterial Chemoembolization of Hepatocellular Carcinoma. J. Vasc. Interv. Radiol. 2014, 25, 240–247. [Google Scholar] [CrossRef] [PubMed]
- El-Serag, H.B. Hepatocellular Carcinoma. N. Engl. J. Med. 2011, 365, 1118–1127. [Google Scholar] [CrossRef] [PubMed]
- Aljiffry, M.; Walsh, M.J.; Molinari, M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990–2009. World J. Gastroenterol. 2009, 15, 4240. [Google Scholar] [CrossRef]
- Lencioni, R.; de Baere, T.; Soulen, M.C.; Rilling, W.S.; Geschwind, J.H. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: A systematic review of efficacy and safety data. Hepatology 2016, 64, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Chegai, F.; Orlacchio, A.; Merolla, S.; Monti, S.; Mannelli, L. Intermediate hepatocellular carcinoma: The role of transarterial therapy. Hepatic Oncol. 2015, 2, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Pieper, C.C.; Meyer, C.; Vollmar, B.; Hauenstein, K.; Schild, H.H.; Wilhelm, K.E. Temporary Arterial Embolization of Liver Parenchyma with Degradable Starch Microspheres (EmboCept®S) in a Swine Model. Cardiovasc. Interv. Radiol. 2015, 38, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Iezzi, R.; Pompili, M.; Rinninella, E.; Annicchiarico, E.; Garcovich, M.; Cerrito, L.; Ponziani, F.; De Gaetano, A.; Siciliano, M.; Basso, M.; et al. TACE with degradable starch microspheres (DSM TACE) as second-line treatment in HCC patients dismissing or ineligible for sorafenib. Eur. Radiol. 2019, 29, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.; Albrecht, T. Transarterial Chemoembolisation (TACE) with Degradable Starch Microspheres (DSM) and Anthracycline in Patients with Locally Extensive Hepatocellular Carcinoma (HCC): Safety and Efficacy. Cardiovasc. Interv. Radiol. 2020, 43, 402–410. [Google Scholar] [CrossRef]
- Schicho, A.; Pereira, P.L.; Haimerl, M.; Niessen, C.; Michalik, K.; Beyer, L.P.; Stroszczynski, C.; Wiggermann, P. Transarterial chemoembolization (TACE) with degradable starch microspheres (DSM) in hepatocellular carcinoma (HCC): Multi-center results on safety and efficacy. Oncotarget 2017, 8, 72613–72620. [Google Scholar] [CrossRef]
- Goerg, F.; Zimmermann, M.; Bruners, P.; Neumann, U.; Luedde, T.; Kuhl, C. Chemoembolization with Degradable Starch Microspheres for Treatment of Patients with Primary or Recurrent Unresectable, Locally Advanced Intrahepatic Cholangiocarcinoma: A Pilot Study. Cardiovasc. Interv. Radiol. 2019, 42, 1709–1717. [Google Scholar] [CrossRef] [PubMed]
- Schicho, A.; Pereira, P.L.; Michalik, K.; Beyer, L.P.; Stroszczynski, C.; Wiggermann, P. Safety and efficacy of transarterial chemoembolization with degradable starch microspheres (DSM-TACE) in the treatment of secondary liver malignancies. Onco Targets Ther. 2018, 11, 345–350. [Google Scholar] [CrossRef] [PubMed]
- Orlacchio, A.; Chegai, F.; Roma, S.; Merolla, S.; Bosa, A.; Francioso, S. Degradable starch microspheres transarterial chemoembolization (DSMs-TACE) in patients with unresectable hepatocellular carcinoma (HCC): Long-term results from a single-center 137-patient cohort prospective study. Radiol. Med. 2020, 125, 98–106. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, J.M.; Iezzi, R.; Theysohn, J.M.; Albrecht, T.; Posa, A.; Gross, A. European Multicenter Study on Degradable Starch Microsphere TACE: The Digestible Way to Conquer HCC in Patients with High Tumor Burden. Cancers 2021, 13, 5122. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, T.; Hamabe, S.; Saeki, I.; Harima, Y.; Yamaguchi, Y.; Uchida, K.; Terai, S.; Sakaida, I. A novel transcatheter arterial infusion chemotherapy using iodized oil and degradable starch microspheres for hepatocellular carcinoma: A prospective randomized trial. J. Gastroenterol. 2011, 46, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Minici, R.; Ammendola, M.; Manti, F.; Siciliano, M.A.; Giglio, E.; Minici, M.; Melina, M.; Currò, G.; Laganà, D. Safety and Efficacy of Degradable Starch Microspheres Transcatheter Arterial Chemoembolization as a Bridging Therapy in Patients with Early Stage Hepatocellular Carcinoma and Child-Pugh Stage B Eligible for Liver Transplant. Front. Pharmacol. 2021, 12, 634084. [Google Scholar] [CrossRef] [PubMed]
- Spiliopoulos, S.; Moschovaki-Zeiger, O.; Sethi, A.; Festas, G.; Reppas, L.; Filippiadis, D.; Kelekis, N. An update on locoregional percutaneous treatment technologies in colorectal cancer liver metastatic disease. Expert Rev. Med. Devices 2023, 20, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Varela, M.; Real, M.I.; Burrel, M.; Forner, A.; Sala, M.; Brunet, M.; Ayuso, C.; Castells, L.; Montañá, X.; Llovet, J.M.; et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: Efficacy and doxorubicin pharmacokinetics. J. Hepatol. 2007, 46, 474–481. [Google Scholar] [CrossRef]
- Ebert, M.; Ebert, J.; Berger, G. Intravital microscopic research of microembolization with degradable starch microspheres. J. Drug Deliv. 2013, 2013, 242060. [Google Scholar] [CrossRef]
- Huang, X.; Molema, G.; King, S.; Watkins, L.; Edgington, T.S.; Thorpe, P.E. Tumor infarction in mice by antibody-directed targeting of tissue factor to tumor vasculature. Science 1997, 275, 547–550. [Google Scholar] [CrossRef]
- Meredith, A.-M.; Dass, C.R. Increasing role of the cancer chemotherapeutic doxorubicin in cellular metabolism. J. Pharm. Pharmacol. 2016, 68, 729–741. [Google Scholar] [CrossRef] [PubMed]
- Galle, P.R.; Forner, A.; Llovet, J.M.; Mazzaferro, V.; Piscaglia, F.; Raoul, J.-L.; Schirmacher, P.; Vilgrain, V. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Raoul, J.-L.; Forner, A.; Bolondi, L.; Cheung, T.T.; Kloeckner, R.; de Baere, T. Updated use of TACE for hepatocellular carcinoma treatment: How and when to use it based on clinical evidence. Cancer Treat. Rev. 2019, 72, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Poon, R.T.-P.; Lau, C.; Yu, W.-C.; Fan, S.-T.; Wong, J. High serum levels of vascular endothelial growth factor predict poor response to transarterial chemoembolization in hepatocellular carcinoma: A prospective study. Oncol. Rep. 2004, 11, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Sergio, A.; Cristofori, C.; Cardin, R.; Pivetta, G.; Ragazzi, R.; Baldan, A.; Girardi, L.; Cillo, U.; Burra, P.; Giacomin, A.; et al. Transcatheter Arterial Chemoembolization (TACE) in Hepatocellular Carcinoma (HCC): The Role of Angiogenesis and Invasiveness. Am. J. Gastroenterol. 2008, 103, 914–921. [Google Scholar] [CrossRef]
- Lencioni, R.; Petruzzi, P.; Crocetti, L. Chemoembolization of Hepatocellular Carcinoma. Semin. Interv. Radiol. 2013, 30, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Min, X.-L.; Peng, J.; Yang, K.; Yang, L.; Zhang, X.-M. The Changes of HIF-1α and VEGF Expression After TACE in Patients With Hepatocellular Carcinoma. J. Clin. Med. Res. 2016, 8, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Wiggermann, P.; Wohlgemuth, W.A.; Heibl, M.; Vasilj, A.; Loss, M.; Schreyer, A.G.; Stroszczynski, C.; Jung, E.M. Dynamic evaluation and quantification of microvascularization during degradable starch microspheres transarterial Chemoembolisation (DSM-TACE) of HCC lesions using contrast enhanced ultrasound (CEUS): A feasibility study. Clin. Hemorheol. Microcirc. 2013, 53, 337–348. [Google Scholar] [CrossRef]
- Taguchi, T. Chemo-Occlusion for the Treatment of Liver Cancer. Clin. Pharmacokinet. 1994, 26, 275–291. [Google Scholar] [CrossRef]
- Haubold, J.; Reinboldt, M.P.; Wetter, A.; Li, Y.; Ludwig, J.M.; Lange, C.; Wedemeyer, H.; Schotten, C.; Umutlu, L.; Theysohn, J. DMS-TACE of HCC: Evaluation of Tumor Response in Patients Ineligible for Other Systemic or Loco-Regional Therapies. In RöFo—Fortschritte auf dem Gebiet der Röntgenstrahlen und der Bildgebenden; Verfahren: Stuttgart, Germany, 2020; Volume 192, pp. 862–869. [Google Scholar]
- Aronsen, K.F.; Hellekant, C.; Holmberg, J.; Rothman, U.; Teder, H. Controlled Blocking of Hepatic Artery Flow with Enzymatically Degradable Microspheres Combined with Oncolytic Drugs. Eur. Surg. Res. 1979, 11, 99–106. [Google Scholar] [CrossRef]
- Doucet, J.; Kiri, L.; O’Connell, K.; Kehoe, S.; Lewandowski, R.; Liu, D.; Abraham, R.; Boyd, D. Advances in Degradable Embolic Microspheres: A State of the Art Review. J. Funct. Biomater. 2018, 9, 14. [Google Scholar] [CrossRef] [PubMed]
- Lucatelli, P.; De Rubeis, G.; Basilico, F.; Ginanni Corradini, L.; Corona, M.; Bezzi, M.; Catalano, C. Sequential dual-phase cone-beam CT is able to intra-procedurally predict the one-month treatment outcome of multi-focal HCC, in course of degradable starch microsphere TACE. Radiol. Med. 2019, 124, 1212–1219. [Google Scholar] [CrossRef] [PubMed]
- Orlacchio, A. Downstaging disease in patients with hepatocellular carcinoma outside up-to-seven criteria: Strategies using degradable starch microspheres transcatheter arterial chemo-embolization. World J. Hepatol. 2015, 7, 1694. [Google Scholar] [CrossRef] [PubMed]
- Lucatelli, P.; Burrel, M.; Guiu, B.; de Rubeis, G.; van Delden, O.; Helmberger, T. CIRSE Standards of Practice on Hepatic Transarterial Chemoembolisation. Cardiovasc. Interv. Radiol. 2021, 44, 1851–1867. [Google Scholar] [CrossRef] [PubMed]
- Georgiades, C.; Geschwind, J.-F.; Harrison, N.; Hines-Peralta, A.; Liapi, E.; Hong, K.; Wu, Z.; Kamel, I.; Frangakis, C. Lack of Response after Initial Chemoembolization for Hepatocellular Carcinoma: Does It Predict Failure of Subsequent Treatment? Radiology 2012, 265, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Schicho, A.; Pereira, P.L.; Pützler, M.; Michalik, K.; Albrecht, T.; Nolte-Ernsting, C.; Stroszczynski, C.; Wiggermann, P. Degradable Starch Microspheres Transcatheter Arterial Chemoembolization (DSM-TACE) in Intrahepatic Cholangiocellular Carcinoma (ICC): Results from a National Multi-Center Study on Safety and Efficacy. Med. Sci. Monit. 2017, 23, 796–800. [Google Scholar] [CrossRef] [PubMed]
- Yamakado, K.; Inaba, Y.; Sato, Y.; Yasumoto, T.; Hayashi, S.; Yamanaka, T.; Nobata, K.; Takaki, H.; Nakatsuka, A. Radiofrequency Ablation Combined with Hepatic Arterial Chemoembolization Using Degradable Starch Microsphere Mixed with Mitomycin C for the Treatment of Liver Metastasis from Colorectal Cancer: A Prospective Multicenter Study. Cardiovasc. Interv. Radiol. 2017, 40, 560–567. [Google Scholar] [CrossRef]
- Yoshihara, T.; Hasegawa, T.; Sato, Y.; Yamaura, H.; Murata, S.; Chatani, S.; Tsukii, R.; Nagasawa, K.; Tsushima, Y.; Inaba, Y. Clinical Outcomes of Radiofrequency Ablation Combined with Transarterial Chemoembolization Using Degradable Starch Microsphere Mixed with Mitomycin C for the Treatment of Non-hepatocellular Carcinoma Malignant Liver Tumors. Interv. Radiol. 2023, 8, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Golzarian, J. Locoregional Therapies in the Treatment of 3- to 5-cm Hepatocellular Carcinoma: Critical Review of the Literature. Am. J. Roentgenol. 2020, 215, 223–234. [Google Scholar] [CrossRef]
- Lucatelli, P.; Argirò, R.; Crocetti, L.; Rocco, B.; Bozzi, E.; Gasparrini, F.; Tanzilli, A.; Catalano, C.; Iezzi, R. Percutaneous Thermal Segmentectomy: Proof of Concept. Cardiovasc. Interv. Radiol. 2022, 45, 665–676. [Google Scholar] [CrossRef]
- Orlacchio, A.; Chegai, F.; Francioso, S.; Merolla, S.; Monti, S.; Angelico, M.; Tisone, G.; Mannelli, L. Repeated Transarterial Chemoembolization with Degradable Starch Microspheres (DSMs-TACE) of Unresectable Hepatocellular Carcinoma: A Prospective Pilot Study. Curr. Med. Imaging Rev. 2018, 14, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Sacco, R.; Faggioni, L.; Bargellini, I.; Ginanni, B.; Battaglia, V.; Romano, A.; Bertini, M.; Bresci, G.; Bartolozzi, C. Assessment of response to sorafenib in advanced hepatocellular carcinoma using perfusion computed tomography: Results of a pilot study. Dig. Liver Dis. 2013, 45, 776–781. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.M.; Real, M.I.; Montaña, X.; Planas, R.; Coll, S.; Aponte, J.; Ayuso, C.; Sala, M.; Muchart, J.; Solà, R.; et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: A randomised controlled trial. Lancet 2002, 359, 1734–1739. [Google Scholar] [CrossRef] [PubMed]
- Llovet, J.; Brú, C.; Bruix, J. Prognosis of Hepatocellular Carcinoma: The BCLC Staging Classification. Semin. Liver Dis. 1999, 19, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Forner, A.; Reig, M.E.; Rodriguez de Lope, C.; Bruix, J. Current Strategy for Staging and Treatment: The BCLC Update and Future Prospects. Semin. Liver Dis. 2010, 30, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Parikh, N.D.; Waljee, A.K.; Singal, A.G. Downstaging hepatocellular carcinoma: A systematic review and pooled analysis. Liver Transplant. 2015, 21, 1142–1152. [Google Scholar] [CrossRef] [PubMed]
- Bryce, K.; Tsochatzis, E.A. Downstaging for hepatocellular cancer: Harm or benefit? Transl. Gastroenterol. Hepatol. 2017, 2, 106. [Google Scholar] [CrossRef] [PubMed]
- Affonso, B.B.; Galastri, F.L.; da Motta Leal Filho, J.M.; Nasser, F.; Falsarella, P.M.; Cavalcante, R.N.; de Almeida, M.D.; Felga, G.E.G.; Valle, L.G.M.; Wolosker, N. Long-term outcomes of hepatocellular carcinoma that underwent chemoembolization for bridging or downstaging. World J. Gastroenterol. 2019, 25, 5687–5701. [Google Scholar] [CrossRef] [PubMed]
- Bruix, J.; Sherman, M. Management of hepatocellular carcinoma: An update. Hepatology 2011, 53, 1020–1022. [Google Scholar] [CrossRef]
- Kirchhoff, T.D.; Rudolph, K.L.; Layer, G.; Chavan, A.; Greten, T.F.; Rosenthal, H.; Kubicka, S.; Galanski, M.; Manns, M.P.; Schild, H.; et al. Chemoocclusion vs chemoperfusion for treatment of advanced hepatocellular carcinoma: A randomised trial. Eur. J. Surg. Oncol. (EJSO) 2006, 32, 201–207. [Google Scholar] [CrossRef]
- Vogl, T.J.; Langenbach, M.C.; Hammerstingl, R.; Albrecht, M.H.; Chatterjee, A.R.; Gruber-Rouh, T. Evaluation of two different transarterial chemoembolization protocols using Lipiodol and degradable starch microspheres in therapy of hepatocellular carcinoma: A prospective trial. Hepatol. Int. 2021, 15, 685–694. [Google Scholar] [CrossRef]
- Yildiz, I.; Deniz, S.; Ozer, A.; Caliskan, K. Trans-Arterial Chemoembolization with 50 μm Degradable Starch Microspheres Versus 300–500 μm Drug Eluting Beads in Hepatocellular Carcinoma: A Comparative Analysis of Initial Treatment Outcomes. J. Belg. Soc. Radiol. 2022, 106, 10. [Google Scholar] [CrossRef]
- Ray, C.E.; Edwards, A.; Smith, M.T.; Leong, S.; Kondo, K.; Gipson, M.; Rochon, P.J.; Gupta, R.; Messersmith, W.; Purcell, T.; et al. Metaanalysis of Survival, Complications, and Imaging Response following Chemotherapy-based Transarterial Therapy in Patients with Unresectable Intrahepatic Cholangiocarcinoma. J. Vasc. Interv. Radiol. 2013, 24, 1218–1226. [Google Scholar] [CrossRef]
- Vogl, T.J.; Marko, C.; Langenbach, M.C.; Naguib, N.N.N.; Filmann, N.; Hammerstingl, R.; Gruber-Rouh, T. Transarterial chemoembolization of colorectal cancer liver metastasis: Improved tumor response by DSM-TACE versus conventional TACE, a prospective, randomized, single-center trial. Eur. Radiol. 2021, 31, 2242–2251. [Google Scholar] [CrossRef] [PubMed]
- Wasser, K.; Giebel, F.; Fischbach, R.; Tesch, H.; Landwehr, P. Transarterielle Chemoembolisation von Lebermetastasen kolorektaler Karzinome mit abbaubaren Stärkepartikeln (Spherex®). Radiologe 2005, 45, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Lammer, J.; Malagari, K.; Vogl, T.; Pilleul, F.; Denys, A.; Watkinson, A.; Pitton, M.; Sergent, G.; Pfammatter, T.; Terraz, S.; et al. Prospective Randomized Study of Doxorubicin-Eluting-Bead Embolization in the Treatment of Hepatocellular Carcinoma: Results of the PRECISION V Study. Cardiovasc. Interv. Radiol. 2010, 33, 41–52. [Google Scholar] [CrossRef]
- Vogl, T.J.; Lammer, J.; Lencioni, R.; Malagari, K.; Watkinson, A.; Pilleul, F.; Denys, A.; Lee, C. Liver, Gastrointestinal, and Cardiac Toxicity in Intermediate Hepatocellular Carcinoma Treated with PRECISION TACE With Drug-Eluting Beads: Results From the PRECISION V Randomized Trial. Am. J. Roentgenol. 2011, 197, W562–W570. [Google Scholar] [CrossRef]
- Zhu, A.X.; Duda, D.G.; Sahani, D.V.; Jain, R.K. HCC and angiogenesis: Possible targets and future directions. Nat. Rev. Clin. Oncol. 2011, 8, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Minata, M.; Harada, K.H.; Kudo, M.; Ikai, I.; Nishida, N. The Prognostic Value of Vascular Endothelial Growth Factor in Hepatocellular Carcinoma for Predicting Metastasis after Curative Resection. Oncology 2013, 84, 75–81. [Google Scholar] [CrossRef]
- Iezzi, R.; Pompili, M.; Nestola, M.; Siciliano, M.; Annicchiarico, E.; Zocco, M.A.; Rinninella, E.; Posa, A.; Antonuccio, G.E.M.; Gasbarrini, A.; et al. Transarterial chemoembolization with degradable starch microspheres (DSM-TACE): An alternative option for advanced HCC patients? Preliminary results. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 2872–2877. [Google Scholar]
| Study | Year | Number of Patients | Minor Adverse Events/Toxicity | Major Adverse Events/Toxicity |
|---|---|---|---|---|
| Minici et al. [16] | 2021 | 54 | Pain, post-embolization syndrome, transient nausea, vomiting: 25.9% | Cholecystitis: 3.7% |
| Schicho et al. [37] | 2017 | 7 | Nausea, vomiting, epigastric pain: 32% | Thrombocytopenia: 4% |
| Schicho et al. [10] | 2017 | 50 | Epigastric pain, nausea, vomiting, diarrhea, transient neutropenia, thrombocytopenia: 48% | Allergic reaction: 4% |
| Haubold et al. [30] | 2020 | 28 | CIRSE Grade 1: 11%; CIRSE Grade 2: 9% | CIRSE Grade 3: 2% |
| Goerg et al. [11] | 2019 | 21 | Asymptomatic peribiliary necrosis: 9.5% | Hepatobiliary abscess: 4.8%; Death: 9.5% |
| Orlacchio et al. [13] | 2020 | 137 | Post embolization syndrome: 73.7% | Cholecystitis, hepatic abscess, massive portal vein thrombosis: 68%; Death: 1.4% |
| Gross et al. [9] | 2020 | 37 | Pain: 23%; Nausea: 11%; Vomiting: 3% | Duodenal ulcer: 0.4% |
| Study | Year | Malignancy | Outcomes |
|---|---|---|---|
| Kirchhof et al. [51] | 2006 | HCC | PR: 26%; SD: 41%; PD: 33% |
| Gross et al. [9] | 2020 | HCC | Objective response rate: 49%; Disease control rate: 83% |
| Haubold et al. [30] | 2020 | HCC | CR: 14.3%; PR: 25%; SD: 39.3%; PD: 21.4% |
| Yamazaki et al. [15] | 2011 | HCC | Tumor response rate: 80% |
| Minici et al. [16] | 2021 | HCC | Overall survival rate: 96% at 6 months, 92% at 12 months |
| Schicho et al. [10] | 2017 | HCC | Objective response rate: 44%; Disease control rate: 70% |
| Orlacchio et al. [42] | 2018 | HCC | Complete response rates: 20.8%, 23.5%, and 41.6% after the first, second, and third procedures, respectively |
| Schico et al. [37] | 2017 | ICC | PR: 12%; SD: 32% |
| Goerg et al. [11] | 2019 | ICC | Complete remission: 11.1%; PR: 50%; SD: 38.9% |
| Schicho et al. [12] | 2018 | CRLM | Disease control rate: 44%; Objective response: 40% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moschovaki-Zeiger, O.; Arkoudis, N.-A.; Giannakis, A.; Grigoriadis, S.; Anagnostopoulos, F.; Spiliopoulos, S. Biodegradable Microspheres for Transarterial Chemoembolization in Malignant Liver Disease. Medicina 2024, 60, 678. https://doi.org/10.3390/medicina60040678
Moschovaki-Zeiger O, Arkoudis N-A, Giannakis A, Grigoriadis S, Anagnostopoulos F, Spiliopoulos S. Biodegradable Microspheres for Transarterial Chemoembolization in Malignant Liver Disease. Medicina. 2024; 60(4):678. https://doi.org/10.3390/medicina60040678
Chicago/Turabian StyleMoschovaki-Zeiger, Ornella, Nikolaos-Achilleas Arkoudis, Athanasios Giannakis, Stavros Grigoriadis, Fotis Anagnostopoulos, and Stavros Spiliopoulos. 2024. "Biodegradable Microspheres for Transarterial Chemoembolization in Malignant Liver Disease" Medicina 60, no. 4: 678. https://doi.org/10.3390/medicina60040678








