Design of a Real-Time and Continua-Based Framework for Care Guideline Recommendations
Abstract
:1. Introduction
- A real-time and personalized vital signs state monitoring/predicting model, called vital signs state predictor (VSP), is provided to predict the vital signs states, give alarms when needed, and recommend related care guidelines to caregivers. In addition, data streaming is also integrated into the VSP model so that it always uses the latest data.
- Cagurs can reduce the amount of work that caregivers need to do and can help caregivers improve the efficiency and quality of patient care, and utilizes mobile devices to provide remote care for patients.
- Cagurs streamlines the repetitive process of vital signs measurement, while the interoperability and connectivity of the system enables it to save and transmit the vital signs data automatically.
- Cagurs has undergone a practical evaluation by caregivers at National Cheng Kung University Hospital, and these users then provides some feedback and suggestions about the system. In addition, the effectiveness of VSP has been demonstrated based on vital signs state predictions made using a publicly available vital signs dataset (obtained from the University of Queensland [9]). The results show that Cagurs can successfully deal with the challenging problem of predicting vital signs states.
2. Related Works
2.1. Continua Health Alliance
2.2. Health Device Profile and Bluetooth Low Energy
2.3. Mobile Devices in Patient Care
2.4. Data Mining in Healthcare
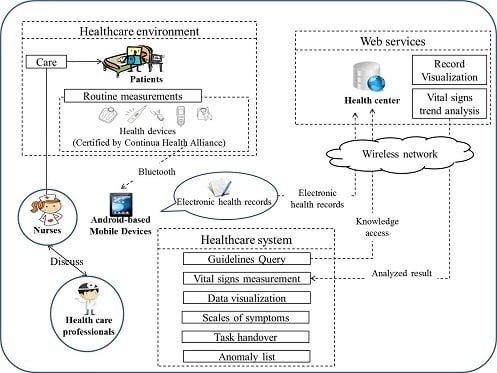
3. Framework Design

3.1. Overview of System Use
3.2. Healthcare System

3.3. Vital Signs State Predictor

3.3.1. Discretization
3.3.2. Mining Frequent Episodes
| Blood Pressure (mmHg) | ||
|---|---|---|
| Systolic | Diastolic | |
| Prehypertension | 120–139 | 80–89 |
| Stage 1 hypertension | 140–159 | 90–99 |
| Stage 2 hypertension | ≥160 | ≥100 |
| Oxygen (%) | ||
| Mild hypoxemia | <94% | |
| Moderate hypoxemia | <89% | |
| Severe hypoxemia | <75% | |
| Heart Rate (bpm) | ||
| Tachycardia | >100 | |
| Bradycardia | <60 | |

3.3.3. The Vital Signs State Predictor

3.3.4. Dynamic Updating of the VSP
- ♦
- Events deletion

- ♦
- Events addition
4. Experiments and Evaluation
4.1. Practical Evaluation of Cagurs
4.2. Experiments on Real Data
| Vital Signs | Abbreviation | Vital Signs | Abbreviation |
|---|---|---|---|
| Prehypertension | BP_HB | Severe hypoxemia | SpO2_Lhard |
| Stage 1 hypertension | BP_H1 | Tachycardia | Pulse_H |
| Stage 2 hypertension | BP_H2 | Bradycardia | Pulse_L |
| Mild hypoxemia | SpO2_Lmicro | Normal | N |
| Moderate hypoxemia | SpO2_Lmid |





| Common Rules |
|---|
| (Tachycardia Prehypertension) → Prehypertension |
| (Tachycardia), (Prehypertension) → Prehypertension |
| (Hypertension_I) → (Hypertension_I) |
| (Tachycardia) → (Prehypertension) |
| (Tachycardia), (Tachycardia) → (Prehypertension) |
| (Tachycardia) → (Tachycardia Prehypertension) |
| Conditional Rules |
| (Prehypertension) → (Tachycardia) |
| (Prehypertension) → (Tachycardia, Prehypertension) |
5. Conclusions and Future Work
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Council for Economic Planning and Development. Available online: http://www.ndc.gov.tw/encontent/ (accessed on 22 March 2014).
- Department of Health, Executive Yuan R.O.C. Available online: http://www.mohw.gov.tw/EN/Ministry/Index.aspx (accessed on 22 March 2014).
- Chen, M.J.; Chen, K.Y.; Chiang, S.J.; Chang, P. Taipei Smart Medical Package. In Proceedings of the 14th IEEE International Conference on e-Health Networking, Applications and Services (Healthcom), Beijing, China, 10–13 October 2012.
- Farmer, A.; Gibson, O.; Hayton, P.; Bryden, K.; Dudley, C.; Neil, A.; Tarassenko, L. A real-time, mobile phone-based telemedicine system to support young adults with type 1 diabetes. Inform. Prim. Care 2005, 13, 171–177. [Google Scholar]
- Lim, J.H.; Park, C.; Park, S.J. Home Healthcare Settop-box for Senior Chronic Care Using ISO/IEEE 11073 PHD Standard. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Buenos Aires, Argentina, 31 August–4 September 2010.
- Matsumoto, T.; Ogata, S.; Kawaji, S. Designing and Implementation of Mobile Terminal for Telehealth Care Life Support System. In Proceedings of the 7th International Conference on Computer Supported Cooperative Work in Design, Rio de Janeiro, Brazil, 25–27 September 2002.
- Tsai, H.; Lin, Y.F.; Yang, Y.C.; Tseng, V.S. A Mobile Framework for Personalized Diabetes Telecare. In Proceedings of the Conference on Technologies and Applications of Artificial Intelligence, Tainan, Taiwan, 16–18 November 2012.
- Su, C.-J.; Chiang, C.-Y. IAServ: An intelligent home care web services platform in a cloud for aging-in-place. Int. J. Environ. Res. Public Health 2013, 10, 6106–6130. [Google Scholar] [CrossRef]
- Liu, D.; Gorges, M.; Jenkins, S.A. University of Queensland vital signs dataset: Development of an accessible repository of anesthesia patient monitoring data for research. Anesth. Analg. 2011, 114, 584–589. [Google Scholar]
- Continua Health Alliance. Available online: http://www.continuaalliance.org/products/design-guidelines (accessed on 22 March 2014).
- IEEE Standards Association Page. Available online: http://standards.ieee.org (accessed on 22 March 2014).
- ISO/IEEE 11073 Personal Health Data. Available online: http://person.hst.aau.dk/ska/MIE2008/ParalleSessions/PresentationsForDownloads/Mon-1530/Sta-30_Clarke.pdf (accessed on 22 March 2014).
- Health Device Profile Implementation Guidance Whitepaper. Available online: https://www.bluetooth.org/docman/handlers/downloaddoc.ashx?doc_id=225927 (accessed on 22 March 2014).
- Park, K.H.; Pak, J.G. Implementation of a handheld compute engine for personal health devices. Int. J. Smart Home 2012, 6, 59–64. [Google Scholar]
- Wu, J.R.; Tsai, Y.S. Building a Home Care System with the ISO/IEEE 11073 Standard. In Proceedings of the International Federation for Medical and Biological Engineering, Budapest, Hungary, 14–18 September 2009; Volume 25, pp. 326–329.
- Latuske, R. Bluetooth Health Device Profile and the IEEE 11073 Medical Device Framework; ARS Software GmbH: Starnberg, Bavaria, Germany, 2009. [Google Scholar]
- Google Inc. Android Developers. Available online: http://www.android.com/ (accessed on 22 March 2014).
- BluetoothHealth. Available online: http://developer.android.com/reference/android/bluetooth/BluetoothHealth.html (accessed on 22 March 2014).
- Bluetooth Low Energy. Available online: http://www.bluetooth.com/Pages/low-energy-tech-info.aspx (accessed on 22 March 2014).
- BLE API. Available online: http://developer.android.com/guide/topics/connectivity/bluetooth-le.html (accessed on 22 March 2014).
- Patel, K.; Chapman, C.G.; Luo, N.; Woodruff, J.N.; Arora, V.M. Impact of mobile tablet computers on internal medicine resident efficiency. Arch. Intern. Med. 2012, 172, 436–438. [Google Scholar]
- Yang, Y.; Liu, X. A Re-examination of Text Categorization Methods. In Proceedings of the 22nd Annual International ACM SIGIR Conference on Research and Development in Information Retrieval, Berkeley, CA, USA, 15–19 August 1999.
- Koh, H.C.; Tan, G. Data mining applications in healthcare. J. Healthc. Inf. Manag. 2005, 19, 64–72. [Google Scholar]
- Mannila, H.; Toivonen, H.; Verkamo, A.I. Discovering frequent episodes in sequences. Data Min. Knowl. Discov. 1997, 1, 259–289. [Google Scholar] [CrossRef]
- Wu, C.-W.; Lin, Y.-F.; Yu, P.S.; Tseng, V.S. Mining High Utility Episodes in Complex Event Sequences. In Proceedings of the 19th ACM SIGKDD Conference on Knowledge Discovery and Data Mining, Chicago, IL, USA, Chicago, 11–14 August 2013; pp. 536–544.
- Patnaik, D.; Patrick, B.; Ramakrishnan, N.; Parida, L.; Keller, B.J.; Hanauer, D.; Hanauer, D.A. Experiences with Mining Temporal Event Sequences from Electronic Medical Records: Initial Successes and Some Challenges. In Proceedings of the 17th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Diego, CA, USA, 21–24 August 2011.
- Ma, X.; Pang, H.H.; Tan, K.L. Finding Constrained Frequent Episodes Using Minimal Occurrences. In Proceedings of the 4th IEEE International Conference on Data Mining, Brighton, UK, 1–4 November 2004.
- Cho, C.W.; Wu, Y.H.; Yen, S.J.; Zheng, Y.; Chen, A.L.P. On-line rule matching for event prediction. VLDB J. 2011, 20, 303–334. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Lin, Y.-F.; Shie, H.-H.; Yang, Y.-C.; Tseng, V.S. Design of a Real-Time and Continua-Based Framework for Care Guideline Recommendations. Int. J. Environ. Res. Public Health 2014, 11, 4262-4279. https://doi.org/10.3390/ijerph110404262
Lin Y-F, Shie H-H, Yang Y-C, Tseng VS. Design of a Real-Time and Continua-Based Framework for Care Guideline Recommendations. International Journal of Environmental Research and Public Health. 2014; 11(4):4262-4279. https://doi.org/10.3390/ijerph110404262
Chicago/Turabian StyleLin, Yu-Feng, Hsin-Han Shie, Yi-Ching Yang, and Vincent S. Tseng. 2014. "Design of a Real-Time and Continua-Based Framework for Care Guideline Recommendations" International Journal of Environmental Research and Public Health 11, no. 4: 4262-4279. https://doi.org/10.3390/ijerph110404262