The Knowledge, Awareness, and Practices of Portuguese General Practitioners Regarding Multimorbidity and its Management: Qualitative Perspectives from Open-Ended Questions
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample and Recruitment
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Definition of Multimorbidity
“Several diseases coexist in the same patient, particularly chronic and of complex clinical management, which may interfere with his quality of life, autonomy, and ultimately longevity.”(Quote 1 Respondent 39)
“Presence of two or more chronic diseases in the same person causing decreased quality of life, increased demand for health resources and also creating challenges in patients’ treatment and counselling.”(Quote 2 Respondent 8)
“[…] means having several pathologies, or in this case, health problems. Partly it is synonymous to multiple pathologies, but in the context of Primary Health Care, goes further than that, because not all health problems are actually diseases.”(Quote 3 Respondent 43)
“Unlike comorbidity this concept [multimorbidity] does not place a disease as central and others as satellites. All have a contributing role.”(Quote 4 Respondent 74)
Definition of Multimorbidity by the European General Practice Research Network (EGPRN)
“It is very important to better identify patients with multimorbidity. It is very complete. I agree with this definition.”(Quote 5 Respondent 52)
3.2. Relevance of Multimorbidity in Daily Practice
“It is very prevalent. In an aging population, there is a large percentage of people who are walking medical textbooks [have every illness you can imagine]. Stress factors, unemployment, poor working conditions, the presence of a dependent elderly [in the household], diseases in family member etc. are factors that aggravate this situation, I believe that single disease patients have no expression in my daily practice.”(Quote 6 Respondent 7)
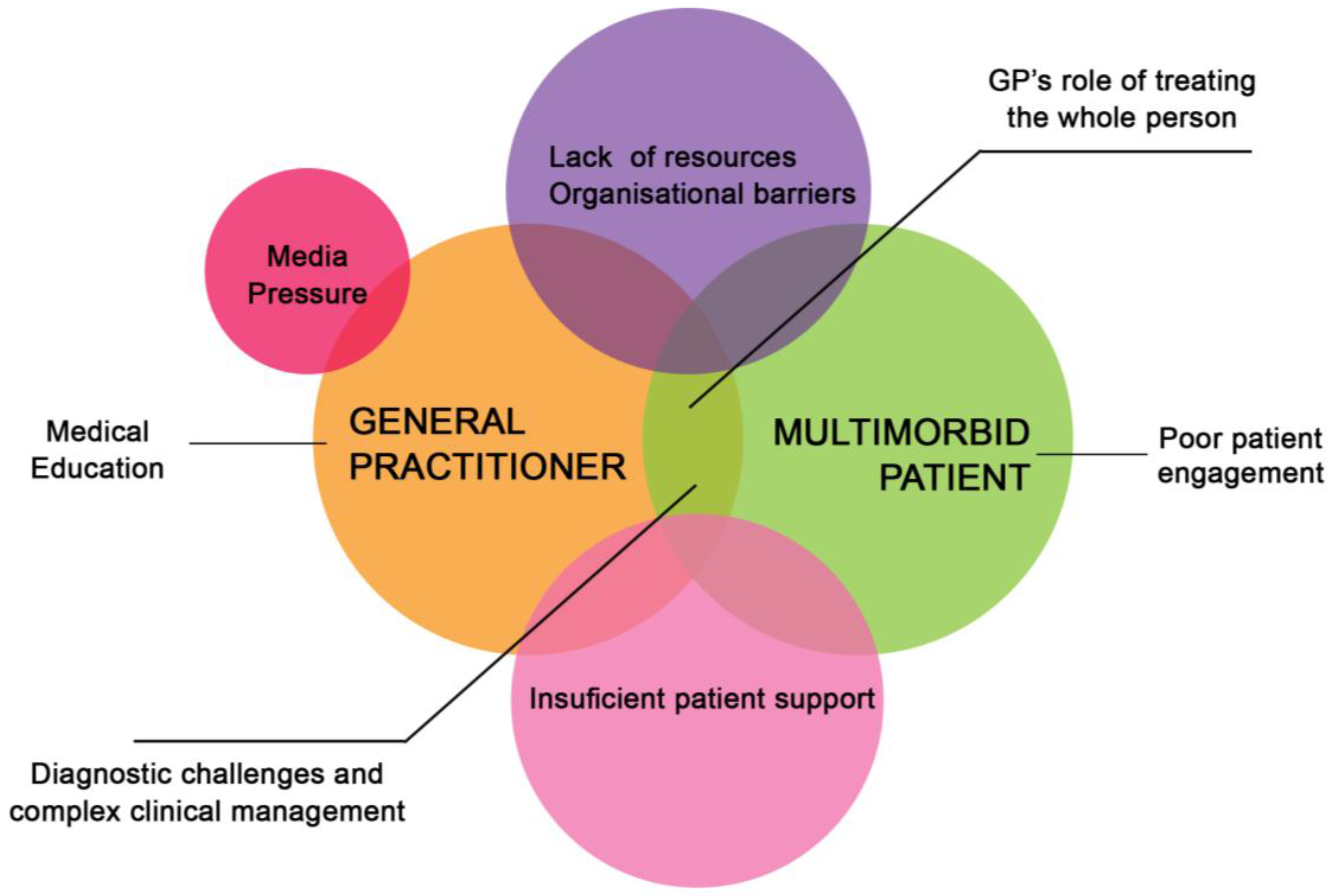
3.3. Perceived Difficulties and Challenges
3.3.1. Difficulties and Challenges Inherent to the Health Care System
Lack of resources:
“Lack of time to be able to see the big picture, ending always to work smaller parts at a time and the results are not always good, it leads to forgetfulness, [treatment] redundancies, delays [in diagnosis]...”(Quote 7 Respondent 17)
Organisational barriers between primary and secondary care providers:
“Secondary care providers do not deliver a global care [for the multimorbid patient], but fragmented [focusing on a specific health problem], because there is no hospital physician (e.g. internist), in straight connection with the GP, to act as a care manager for these patients”(Quote 8 Respondent 10)
3.3.2. Difficulties and Challenges External to the Health Care System
Media pressure:
Insufficient patient support:
“The lack of support [...] to help solve many of the problems (which are not organic diseases) that affect the physical well-being of multimorbid patients creates an excessive demand for the use of primary care services. The GP feels powerless to solve social, work and family related problems.”(Quote 9 Respondent 52)
3.3.3. Difficulties and Challenges Related to the GP
GP’s role of treating the whole person:
“Managing multimorbidity is hard work for GPs because we focus on the health of the whole person. And the whole person is difficult to manage pharmacological and non-pharmacologically.”(Quote 10 Respondent 48)
Medical education:
3.3.4. Difficulties and Challenges Related to the Multimorbid Patient
Diagnostic challenges and complex clinical management:
“Two common areas of difficulty are polypharmacy and health promotion, since taking into account what is best for a condition may worsen another.”(Quote 11 Respondent 8)
Poor patient engagement:
3.4. Management of Multimorbidity
“…with great difficulty and distress due to the [short] consultation times, allied with constant interruptions by various coworkers, patients are often inevitably cut short in the exposure of their concerns. Owing to the lack of existing human resources, family doctors are then required to see to not only their list of patients as well as others whose doctors are absent and in need of urgent care. This situation is not easy to solve.”(Quote 12 Respondent 53)
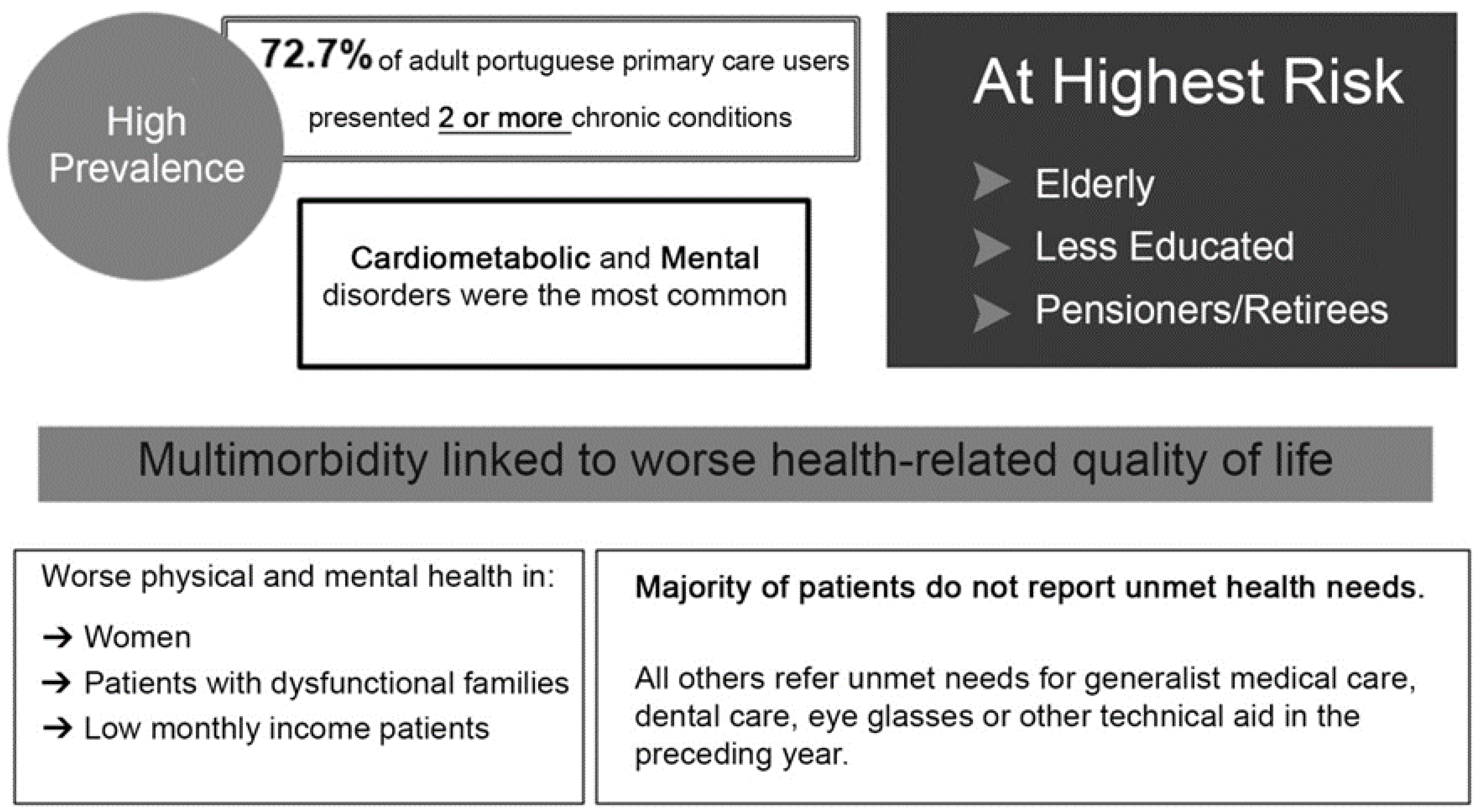
3.5. Informational Material Bearing the Results from Previous Portuguese Multimorbidity Studies
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Ramond-Roquin, A.; Fortin, M. Towards increased visibility of multimorbidity research. J. Comorbidity 2016, 6, 42–45. [Google Scholar] [CrossRef]
- Violan, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Disease priorities. Nature 2011, 477, 250.
- Smith, S.M.; O’Dowd, T. Chronic diseases: What happens when they come in multiples? Br. J. Gen. Pract. 2007, 57, 268–270. [Google Scholar] [PubMed]
- Tinetti, M.E.; Fried, T.R.; Boyd, C.M. Designing health care for the most common chronic condition—Multimorbidity. JAMA 2012, 307, 2493–2494. [Google Scholar] [CrossRef] [PubMed]
- Almirall, J.; Fortin, M. The coexistence of terms to describe the presence of multiple concurrent diseases. J. Comorbidity 2013, 3, 4–9. [Google Scholar] [CrossRef]
- Quam, L.; Smith, R.; Yach, D. Rising to the global challenge of the chronic disease epidemic. Lancet 2006, 368, 1221–1223. [Google Scholar] [CrossRef]
- Navickas, R.; Petric, V.-K.; Feigl, A.B.; Seychell, M. Multimorbidity: What do we know? What should we do? J. Comorbidity 2016, 6, 4–11. [Google Scholar] [CrossRef]
- Anderson, G.; Horvath, J. The growing burden of chronic disease in america. Public Health Rep. 2004, 119, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Prazeres, F.; Santiago, L. Prevalence of multimorbidity in the adult population attending primary care in portugal: A cross-sectional study. BMJ 2015, 5, e009287. [Google Scholar] [CrossRef] [PubMed]
- Glynn, L.G.; Valderas, J.M.; Healy, P.; Burke, E.; Newell, J.; Gillespie, P.; Murphy, A.W. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam. Pract. 2011, 28, 516–523. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Lapointe, L.; Hudon, C.; Vanasse, A.; Ntetu, A.L.; Maltais, D. Multimorbidity and quality of life in primary care: A systematic review. Health Qual. Life Outcomes 2004, 2, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agborsangaya, C.B.; Lau, D.; Lahtinen, M.; Cooke, T.; Johnson, J.A. Health-related quality of life and healthcare utilization in multimorbidity: Results of a cross-sectional survey. Qual. Life Res. 2012, 22, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of primary care to health systems and health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.; Gay, B.; Crebolder, H.; Heyrman, J.; Svab, I.; Maastricht, P.R. The European Definition of General Practice/Family Medicine. Available online: http://www.woncaeurope.org/sites/default/files/documents/Definition%203rd%20ed%202011%20with%20revised%20wonca%20tree.pdf (accessed on 20 August 2016).
- Sinnott, C.; McHugh, S.; Browne, J.; Bradley, C. Gps’ perspectives on the management of patients with multimorbidity: Systematic review and synthesis of qualitative research. BMJ 2013, 3, e003610. [Google Scholar] [CrossRef] [PubMed]
- Luijks, H.D.; Loeffen, M.J.; Lagro-Janssen, A.L.; van Weel, C.; Lucassen, P.L.; Schermer, T.R. Gps’ considerations in multimorbidity management: A qualitative study. Br. J. Gen. Pract. 2012, 62, e503–e510. [Google Scholar] [CrossRef] [PubMed]
- Cottrell, E.; Yardley, S. Lived experiences of multimorbidity: An interpretative meta-synthesis of patients’, general practitioners’ and trainees’ perceptions. Chronic Illn. 2015, 11, 279–303. [Google Scholar] [CrossRef] [PubMed]
- Allender, J.A.; Rector, C.; Warner, K.D. Community and Public Health Nursing: Promoting the Public’s Health, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2014. [Google Scholar]
- Barros, P.P.; Machado, S.R.; Simoes Jde, A. Portugal. Health system review. Health Syst. Transit. 2011, 13, 1–156. [Google Scholar] [PubMed]
- Le Reste, J.Y.; Nabbe, P.; Manceau, B.; Lygidakis, C.; Doerr, C.; Lingner, H.; Czachowski, S.; Munoz, M.; Argyriadou, S.; Claveria, A.; et al. The european general practice research network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. J. Am. Med. Dir. Assoc. 2013, 14, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Prazeres, F.; Santiago, L.M.; Simoes, J.A. Defining multimorbidity: From english to portuguese using a delphi technique. Biomed. Res. Int. 2015, 2015. [Google Scholar] [CrossRef] [PubMed]
- LeReste, J.Y.; Nabbe, P.; Lazic, D.; Assenova, R.; Lingner, H.; Czachowski, S.; Argyriadou, S.; Sowinska, A.; Lygidakis, C.; Doerr, C.; et al. How do general practitioners recognize the definition of multimorbidity? A european qualitative study. Eur. J. Gen. Pract. 2016, 22, 1–10. [Google Scholar]
- Elo, S.; Kaariainen, M.; Kanste, O.; Polkki, T.; Utriainen, K.; Kyngas, H. Qualitative content analysis: A focus on trustworthiness. SAGE Open 2014, 4. [Google Scholar] [CrossRef]
- Prazeres, F.; Santiago, L. Multimorbidity in primary care in portugal (mm-pt): A cross-sectional three-phase observational study protocol. BMJ Open 2014, 4, e004113. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, D.; Emery, J.; de Lusignan, S.; Sutton, S. Using the internet to conduct surveys of health professionals: A valid alternative? Fam Pract 2003, 20, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Coderre, F.; Mathieu, A.; St-Laurent, N. Comparison of the quality of qualitative data obtained through telephone, postal and email surveys. Int. J. Market Res. 2004, 46, 347–357. [Google Scholar]
- World Medical Association. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Acad. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Gentles, S.J.; Charles, C.; Ploeg, J.; McKibbon, K. Sampling in qualitative research: Insights from an overview of the methods literature. Qual. Rep. 2015, 20, 1772–1789. [Google Scholar]
- Patton, M.Q. Qualitative Evaluation and Research Methods, 2nd ed.; Sage Publications: Thousand Oaks, CA, USA, 1990. [Google Scholar]
- Fontanella, B.J.; Ricas, J.; Turato, E.R. Saturation sampling in qualitative health research: Theoretical contributions. Cad. Saude Publica 2008, 24, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Prazeres, F.; Santiago, L. Relationship between health-related quality of life, perceived family support and unmet health needs in adult patients with multimorbidity attending primary care in portugal: A multicentre cross-sectional study. Health Qual. Life Outcomes. (under review).
- Burnard, P.; Gill, P.; Stewart, K.; Treasure, E.; Chadwick, B. Analysing and presenting qualitative data. Br. Dent. J. 2008, 204, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Roberts, M.E.; Stewart, B.M.; Tingley, D.; Lucas, C.; Leder-Luis, J.; Gadarian, S.K.; Albertson, B.; Rand, D.G. Structural topic models for open-ended survey responses. Am. J. Pol. Sci. 2014, 58, 1064–1082. [Google Scholar] [CrossRef]
- Chen, H.Y.; Boore, J.R. Translation and back-translation in qualitative nursing research: Methodological review. J. Clin. Nurs. 2010, 19, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Stewart, M.; Poitras, M.E.; Almirall, J.; Maddocks, H. A systematic review of prevalence studies on multimorbidity: Toward a more uniform methodology. Ann. Fam. Med. 2012, 10, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Willadsen, T.G.; Bebe, A.; Koster-Rasmussen, R.; Jarbol, D.E.; Guassora, A.D.; Waldorff, F.B.; Reventlow, S.; Olivarius Nde, F. The role of diseases, risk factors and symptoms in the definition of multimorbidity—a systematic review. Scand. J. Prim. Health Care 2016, 34, 112–121. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marengoni, A.; Winblad, B.; Karp, A.; Fratiglioni, L. Prevalence of chronic diseases and multimorbidity among the elderly population in sweden. Am. J. Public Health 2008, 98, 1198–1200. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.M.; O’Kelly, S.; O’Dowd, T. Gps’ and pharmacists’ experiences of managing multimorbidity: A “pandora’s box”. Br. J. Gen. Pract. 2010, 60, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Bower, P.; Macdonald, W.; Harkness, E.; Gask, L.; Kendrick, T.; Valderas, J.M.; Dickens, C.; Blakeman, T.; Sibbald, B. Multimorbidity, service organization and clinical decision making in primary care: A qualitative study. Fam. Pract. 2011, 28, 579–587. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, R.; Wyke, S.; Guthrie, B.; Watt, G.; Mercer, S. An “endless struggle”: A qualitative study of general practitioners’ and practice nurses’ experiences of managing multimorbidity in socio-economically deprived areas of scotland. Chronic Illn. 2011, 7, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Sondergaard, E.; Willadsen, T.G.; Guassora, A.D.; Vestergaard, M.; Tomasdottir, M.O.; Borgquist, L.; Holmberg-Marttila, D.; Olivarius Nde, F.; Reventlow, S. Problems and challenges in relation to the treatment of patients with multimorbidity: General practitioners’ views and attitudes. Scand. J. Prim. Health Care 2015, 33, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Blier, P. Media pressure and patient care. J. Psychopharmacol. 2006, 20, 469–470. [Google Scholar] [CrossRef] [PubMed]
- Budhdeo, S.; Watkins, J.; Atun, R.; Williams, C.; Zeltner, T.; Maruthappu, M. Changes in government spending on healthcare and population mortality in the european union, 1995–2010: A cross-sectional ecological study. J. R. Soc. Med. 2015, 108, 490–498. [Google Scholar] [CrossRef] [PubMed]
- PortugalPress. Portugal’s Healthcare under Fire. Available online: http://portugalresident.com/portugal%E2%80%99s-healthcare-under-fire (accessed on 20 August 2016).
- Russell, G.; Thille, P.; Hogg, W.; Lemelin, J. Beyond fighting fires and chasing tails? Chronic illness care plans in ontario, canada. Ann. Fam. Med. 2008, 6, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Miranda, J.A.; Aguiar, P.V. Carga de trabalho, uso do tempo, prescrição de antibióticos e referenciação em consultas de clínica geral. Rev. Port. Clin. Geral 1997, 14, 377–386. [Google Scholar]
- Nogueira, J.N. Duração da consulta: Perspectivas dos médicos e dos pacientes. Rev. Port. Clin. Geral 2002, 18, 303–312. [Google Scholar]
- Deveugele, M.; Derese, A.; van den Brink-Muinen, A.; Bensing, J.; De Maeseneer, J. Consultation length in general practice: Cross sectional study in six european countries. BMJ 2002, 325, 472. [Google Scholar] [CrossRef] [PubMed]
- Ostbye, T.; Yarnall, K.S.; Krause, K.M.; Pollak, K.I.; Gradison, M.; Michener, J.L. Is there time for management of patients with chronic diseases in primary care? Ann. Fam. Med. 2005, 3, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Fitzpatrick, B.; Gourlay, G.; Vojt, G.; McConnachie, A.; Watt, G.C. More time for complex consultations in a high-deprivation practice is associated with increased patient enablement. Br. J. Gen. Pract. 2007, 57, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Lussier, M.T.; Richard, C. Doctor-patient communication. Time to talk. Can. Fam. Physician 2006, 52, 1401–1402. [Google Scholar] [PubMed]
- Montague, E. The promises and challenges of health information technology in primary health care. Prim. Health Care Res. Dev. 2014, 15, 227–230. [Google Scholar] [CrossRef] [PubMed]
- Coleman, K.; Reid, R. Safety Net Medical Home Initiative. Continuous and Team-Based Healing Relationships: Improving Patient Care through Teams. Implementation Guide, 1st ed.; MacColl Center for Health Care Innovation at the Group Health Institute and Qualis Health: Seattle, WA, USA, 2010. [Google Scholar]
- The european study of referrals from primary to secondary care. Concerned action committee of health services research for the european community. Occas. Pap. R. Coll. Gen. Pract. 1992, 56, 1–75. [Google Scholar]
- Janeiro, M. Acesso aos cuidados de saúde secundários numa extensão do centro de saúde de serpa: 10 anos depois. Rev. Port. Clin. Geral 2001, 17, 193–207. [Google Scholar]
- Prieto, L.P.; Olmos, L.G.; Salvanés, F.R.; Puime, A.O. Evaluación de la demanda derivada en atención primaria. Aten. Prim. 2005, 35, 146–151. [Google Scholar] [CrossRef]
- Ponte, C.M.F.; Moura, B.G.; Cerejo, A.C.; Braga, R.; Marques, I.; Teixeira, A.; Jul, A.; Vaz, M.; Trancoso, J. Referenciação aos cuidados de saúde secundários. Rev. Port. Clin. Geral 2006, 22, 555–568. [Google Scholar]
- Barreiro, S. Referenciação e comunicação entre cuidados primários e secundários. Rev. Port. Clin. Geral 2005, 21, 545–553. [Google Scholar]
- Moth, G.; Vestergaard, M.; Vedsted, P. Chronic care management in danish general practice—A cross-sectional study of workload and multimorbidity. BMC Fam. Pract. 2012, 13, 52. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.F.; Longnecker, N. Doctor-patient communication: A review. Ochsner J. 2010, 10, 38–43. [Google Scholar] [PubMed]
- Levenstein, J.H.; McCracken, E.C.; McWhinney, I.R.; Stewart, M.A.; Brown, J.B. The patient-centred clinical method. 1. A model for the doctor-patient interaction in family medicine. Fam. Pract. 1986, 3, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Klemes, A.; Solomon, H. The impact of a personalized preventive care model vs. The conventional healthcare model on patient satisfaction. Open Public Health J. 2015, 8, 1–9. [Google Scholar] [CrossRef]
- Hunter, P. Research and practice coming together. The advent of personalized medicine is bringing clinical research and practice closer together. EMBO Rep. 2012, 13, 109–112. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n (%) | Mean (SD) |
|---|---|---|
| Sex | ||
| Women | 51 (68.92) | |
| Men | 23 (31.08) | |
| Age (years) | 43.73 (13.78) min = 26; max = 64 | |
| Academic degree | ||
| Entry-level medical degree (MD) | 55 (74.32) | |
| Higher medical degrees (Postgraduate/Master/PhD) | 19 (25.68) | |
| Career level | ||
| General practitioner (GP) | 54 (72.97) | |
| GP in training | 20 (27.03) | |
| Experience in primary care (years) | 16.19 (13.29) min = 1; max = 37 | |
| Practice type | ||
| Family Health Unit (family practice based model) | 50 (67.57) | |
| Personalized Healthcare Unit (individual based model) | 24 (32.43) | |
| Place of work (district) | ||
| Coimbra | 35 (47.30) | |
| Aveiro | 39 (52.70) |
| Systemic Level: Health Care System | Inherent to the Healthcare System |
|
| External to the Healthcare System |
| |
| Individual Level: General Practitioner and Multimorbid Patient | General Practitioner related |
|
| Multimorbid Patient related |
|
| (1) person centeredness |
| (2) holistic model |
| (3) effective doctor-patient relationship |
| (4) integrated approach |
| (5) continuing management |
| (6) coordination with others and teamwork |
| (7) problem solving skills |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prazeres, F.; Santiago, L. The Knowledge, Awareness, and Practices of Portuguese General Practitioners Regarding Multimorbidity and its Management: Qualitative Perspectives from Open-Ended Questions. Int. J. Environ. Res. Public Health 2016, 13, 1097. https://doi.org/10.3390/ijerph13111097
Prazeres F, Santiago L. The Knowledge, Awareness, and Practices of Portuguese General Practitioners Regarding Multimorbidity and its Management: Qualitative Perspectives from Open-Ended Questions. International Journal of Environmental Research and Public Health. 2016; 13(11):1097. https://doi.org/10.3390/ijerph13111097
Chicago/Turabian StylePrazeres, Filipe, and Luiz Santiago. 2016. "The Knowledge, Awareness, and Practices of Portuguese General Practitioners Regarding Multimorbidity and its Management: Qualitative Perspectives from Open-Ended Questions" International Journal of Environmental Research and Public Health 13, no. 11: 1097. https://doi.org/10.3390/ijerph13111097
APA StylePrazeres, F., & Santiago, L. (2016). The Knowledge, Awareness, and Practices of Portuguese General Practitioners Regarding Multimorbidity and its Management: Qualitative Perspectives from Open-Ended Questions. International Journal of Environmental Research and Public Health, 13(11), 1097. https://doi.org/10.3390/ijerph13111097






