Pattern of Visits to Older Family Physicians in Taiwan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Physicians’ Characteristics
3.2. Patients, Visits, and Disease Patterns
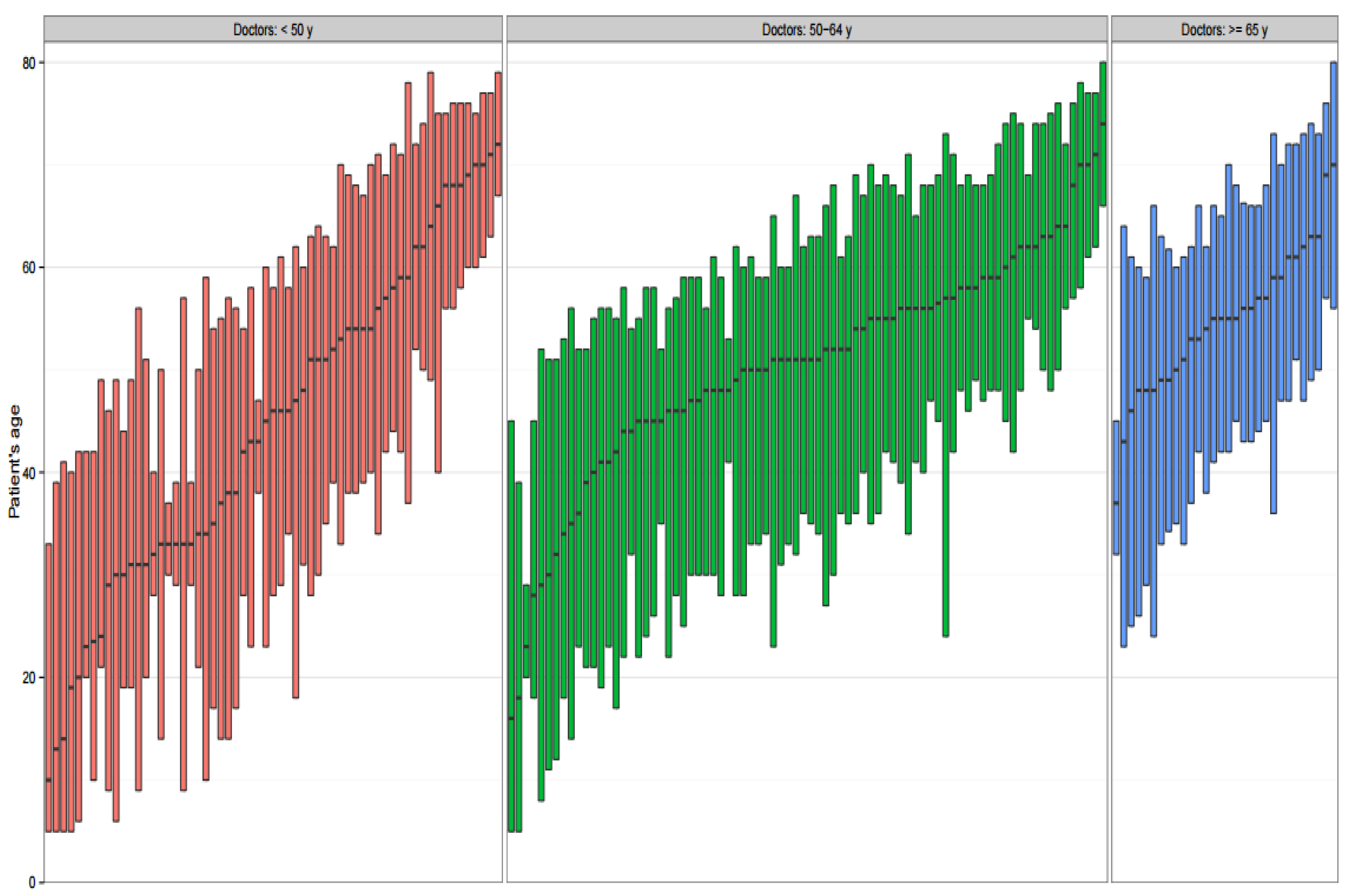
3.3. Patients’ Age Distribution of Visits
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- OECD. The Looming Crisis in the Health Workforce: How Can OECD Countries Respond? OECD Health Policy Stud. 2008. [Google Scholar] [CrossRef]
- Sataloff, R.T.; Hawkshaw, M.; Kutinsky, J.; Maitz, E.A. The aging physician and surgeon. Ear Nose Throat J. 2016, 95, E35–E48. [Google Scholar] [PubMed]
- Simoens, S.; Hurst, J. The Supply of Physician Services in OECD Countries. OECD Health Working Papers, No. 21. Available online: http://www.oecd.org/els/health-systems/35987490.pdf (accessed on 5 May 2017).
- 2015 State Physician Workforce Data Book. Available online: https://members.aamc.org/eweb/upload/2015StateDataBook%20(revised).pdf (accessed on 8 March 2017).
- Visco, A.G.; Barber, M.D.; Myers, E.R. Early physician experience with laparoscopically assisted vaginal hysterectomy and rates of surgical complications and conversion to laparotomy. Am. J. Obstet. Gynecol. 2002, 187, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Adler, R.G.; Constantinou, C. Knowing-or not knowing—When to stop: Cognitive decline in ageing doctors. Med. J. Aust. 2008, 189, 622–624. [Google Scholar] [PubMed]
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic review: The relationship between clinical experience and quality of health care. Ann. Int. Med. 2005, 142, 260–273. [Google Scholar] [CrossRef] [PubMed]
- Drag, L.L.; Bieliauskas, L.A.; Langenecker, S.A.; Greenfield, L.J. Cognitive functioning, retirement status, and age: Results from the Cognitive Changes and Retirement among Senior Surgeons study. J. Am. Coll. Surgeons 2010, 211, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Durning, S.J.; Artino, A.R.; Holmboe, E.; Beckman, T.J.; van der Vleuten, C.; Schuwirth, L. Aging and cognitive performance: Challenges and implications for physicians practicing in the 21st century. J. Contin. Educ. Health Prof. 2010, 30, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Turnbull, J.; Cunnington, J.; Unsal, A.; Norman, G.; Ferguson, B. Competence and cognitive difficulty in physicians: A follow-up study. Acad. Med. 2006, 81, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Survey of America’s Physicians. The Physicians Foundation 2016. Available online: http://www.physiciansfoundation.org/uploads/default/Biennial_Physician_Survey_2016.pdf (accessed on 8 March 2017).
- The Complexities of Physician Supply and Demand: Projections through 2025. Available online: https://www.aamc.org/download/426242/data/ihsreportdownload.pdf?cm_mmc=AAMC-_-ScientificAffairs-_-PDF-_-ihsreport (accessed on 8 March 2017).
- National Physician Survey. National Results by FP/GP or Other Specialist, Sex, Age and All Physicians. Available online: http://nationalphysiciansurvey.ca/wp-content/uploads/2014/11/2014-National-EN.pdf (accessed on 8 March 2017).
- Bieliauskas, L.A.; Langenecker, S.; Graver, C.; Lee, H.J.; O’Neill, J.; Greenfield, L.J. Cognitive changes and retirement among senior surgeons (CCRASS): Results from the CCRASS Study. J. Am. Coll. Surgeons 2008, 207, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care (Abingdon) 2010, 3, 115–119. [Google Scholar] [CrossRef]
- Ho Chan, W.S. Taiwan’s healthcare report 2010. EPMA J. 2010, 1, 563–585. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-Y.; Hung, Y.; Chuang, Y.; Chen, Y.; Weng, W.; Liu, J.; Liang, K. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar]
- Licenced Physicians by Age and Gender in 2011. Taiwan Medical Association. Available online: http://www.tma.tw/stats/stats6.asp (accessed on 23 Arpil 2017).
- Taiwan Medical Association Statistics Report 2015; p. 140 (Table 10). Available online: http://www.tma.tw/tma_stats_2015/2015_stats.pdf (accessed on 8 March 2017).
- Petterson, S.M.; Rayburn, W.F.; Liaw, W.R. When do primary care physicians retire? Implications for workforce projections. Ann. Fam. Med. 2016, 14, 344–349. [Google Scholar] [CrossRef] [PubMed]
- FAA Statement on Pilot Retirement Age. Available online: https://www.faa.gov/other_visit/aviation_industry/airline_operators/airline_safety/info/all_infos/media/age65_qa.pdf (accessed on 8 March 2017).
- Competency and Retirement: Evaluating the Senior Physician. AMA Wire. Available online: http://www.ama-assn.org/ama/ama-wire/post/competency-retirement-evaluating-senior-physician (accessed on 8 March 2017).
- Tuffs, A. Germany abolishes its compulsory retirement age for doctors. BMJ 2009, 338, b97. [Google Scholar] [CrossRef] [PubMed]
- Silver, M.P.; Hamilton, A.D.; Biswas, A.; Warrick, N.I. A systematic review of physician retirement planning. Hum. Resour. Health 2016, 14, 67. [Google Scholar] [CrossRef] [PubMed]
- Van Greuningen, M.; Heiligers, P.J.; Van der Velden, L.F. Motives for early retirement of self-employed GPs in the Netherlands: A comparison of two time periods. BMC Health Serv. Res. 2012, 12, 467. [Google Scholar] [CrossRef] [PubMed]
- Sansom, A.; Calitri, R.; Carter, M.; Campbell, J. Understanding quit decisions in primary care: A qualitative study of older GPs. BMJ Open 2016, 6, e010592. [Google Scholar] [CrossRef] [PubMed]
- Peisah, C.; Wilhelm, K. Physician don’t heal thyself: A descriptive study of impaired older doctors. Int. Psychogeriatr. 2007, 19, 974–984. [Google Scholar] [CrossRef] [PubMed]
- Chambers, M.; Colthart, I.; McKinstry, B. Scottish general practitioners’ willingness to take part in a post-retirement retention scheme: Questionnaire survey. BMJ 2004, 328, 329. [Google Scholar] [CrossRef] [PubMed]
- Krause, K.; Pollak, K.; Gradison, M.; Michener, J. Family Physicians as Team Leaders: “Time” to Share the Care. 2009. Available online: http://www.cdc.gov/pcd/issues/2009/apr/08_0023.htm (accessed on 23 April 2017).
- Yawn, B.; Goodwin, M.A.; Zyzanski, S.J.; Stange, K.C. Time use during acute and chronic illness visits to a family physician. Fam. Pract. 2003, 20, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Family Medicine Facts. Available online: http://www.aafp.org/about/the-aafp/family-medicine-facts.html (accessed on 8 March 2017).
- American Institute in Taiwan. List of Physicians, Dentists and Medical Providers. Available online: http://acs.ait.org.tw/medical-info.html (accessed on 8 March 2017).
- Lynn, A.-M.; Shih, T.-C.; Hung, C.-H.; Lin, M.-H.; Hwang, S.-J.; Chen, T.-J. Characteristics of ambulatory care visits to family medicine specialists in Taiwan: A nationwide analysis. PeerJ 2015, 3, e1145. [Google Scholar] [CrossRef] [PubMed]
- Makaroff, L.A.; Xierali, I.M.; Petterson, S.M.; Shipman, S.A.; Puffer, J.C.; Bazemore, A.W. Factors influencing family physicians’ contribution to the child health care workforce. Ann. Fam. Med. 2014, 12, 427–431. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, A.; Reid, R.O.; Adams, J.L.; Friedberg, M.W.; McGlynn, E.A.; Hussey, P.S. Physicians with the least experience have higher cost profiles than do physicians with the most experience. Health Affairs 2012, 31, 2453–2463. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.A.; Mazmanian, P.E.; Fordis, M.; Van Harrison, R.; Thorpe, K.E.; Perrier, L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA 2006, 296, 1094–1102. [Google Scholar] [CrossRef] [PubMed]
- Konrad, T.R.; Link, C.L.; Shackelton, R.J.; Marceau, L.D.; von dem Knesebeck, O.; Siegrist, J.; Arber, S.; Adams, A.; McKinlay, J.B. It’s about time: Physicians’ perceptions of time constraints in primary care medical practice in three national healthcare systems. Med. Care 2010, 48, 95–100. [Google Scholar] [CrossRef] [PubMed]
| Age Group | Total | |||
|---|---|---|---|---|
| <50 Years Old | 50–64 Years Old | ≥65 Years Old | ||
| Number, n (%) | 61 (35.6) | 80 (46.8) | 30 (17.5) | 171 |
| Median age (years old) | 41 | 58 | 69 | 55 |
| Male, n (%) | 51 (83.6) | 74 (92.5) | 30 (100) | 155 (90.6) |
| Practice location, n (%) | ||||
| Urban | 32 (52.4) | 44 (55.0) | 15 (50.0) | 91 (53.2) |
| Suburban | 21 (34.4) | 22 (27.5) | 10 (33.3) | 53 (30.9) |
| Rural | 8 (13.1) | 14 (17.5) | 5 (16.7) | 27 (15.7) |
| Age Group | Kruskal–Wallis Test | Wilcoxon–Mann–Whitney Test | |||
|---|---|---|---|---|---|
| <50 | 50–64 | ≥65 | p-Value | p-Value | |
| Patients, n | 0.006 | ||||
| Mean | 4058 | 3855 | 2330 | 0.012 (<50 vs. ≥65) | |
| SD | 3073 | 2474 | 2019 | <0.001 (50–64 vs. ≥65) | |
| Visits per year, n | 0.021 | ||||
| Mean | 11,019 | 13,371 | 9220 | 0.289 (<50 vs. ≥65) | |
| SD | 8837 | 8992 | 8600 | 0.006 (50–64 vs. ≥65) | |
| Proportion of acute illness visits | 0.532 | ||||
| Mean | 0.369 | 0.347 | 0.314 | ||
| SD | 0.228 | 0.215 | 0.199 | ||
| Proportion of chronic illness visits | 0.429 | ||||
| Mean | 0.152 | 0.154 | 0.11 | ||
| SD | 0.163 | 0.17 | 0.122 | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.-Y.; Liu, C.-C.; Shen, T.-H.; Wang, Y.-J.; Liu, J.-Y.; Chen, T.-J.; Chou, L.-F.; Hwang, S.-J. Pattern of Visits to Older Family Physicians in Taiwan. Int. J. Environ. Res. Public Health 2017, 14, 499. https://doi.org/10.3390/ijerph14050499
Liu H-Y, Liu C-C, Shen T-H, Wang Y-J, Liu J-Y, Chen T-J, Chou L-F, Hwang S-J. Pattern of Visits to Older Family Physicians in Taiwan. International Journal of Environmental Research and Public Health. 2017; 14(5):499. https://doi.org/10.3390/ijerph14050499
Chicago/Turabian StyleLiu, Hao-Yen, Cheng-Chieh Liu, Tzu-Hsiang Shen, Yi-Jen Wang, Jui-Yao Liu, Tzeng-Ji Chen, Li-Fang Chou, and Shinn-Jang Hwang. 2017. "Pattern of Visits to Older Family Physicians in Taiwan" International Journal of Environmental Research and Public Health 14, no. 5: 499. https://doi.org/10.3390/ijerph14050499






