Valuing a Lifestyle Intervention for Middle Eastern Immigrants at Risk of Diabetes
Abstract
:1. Introduction
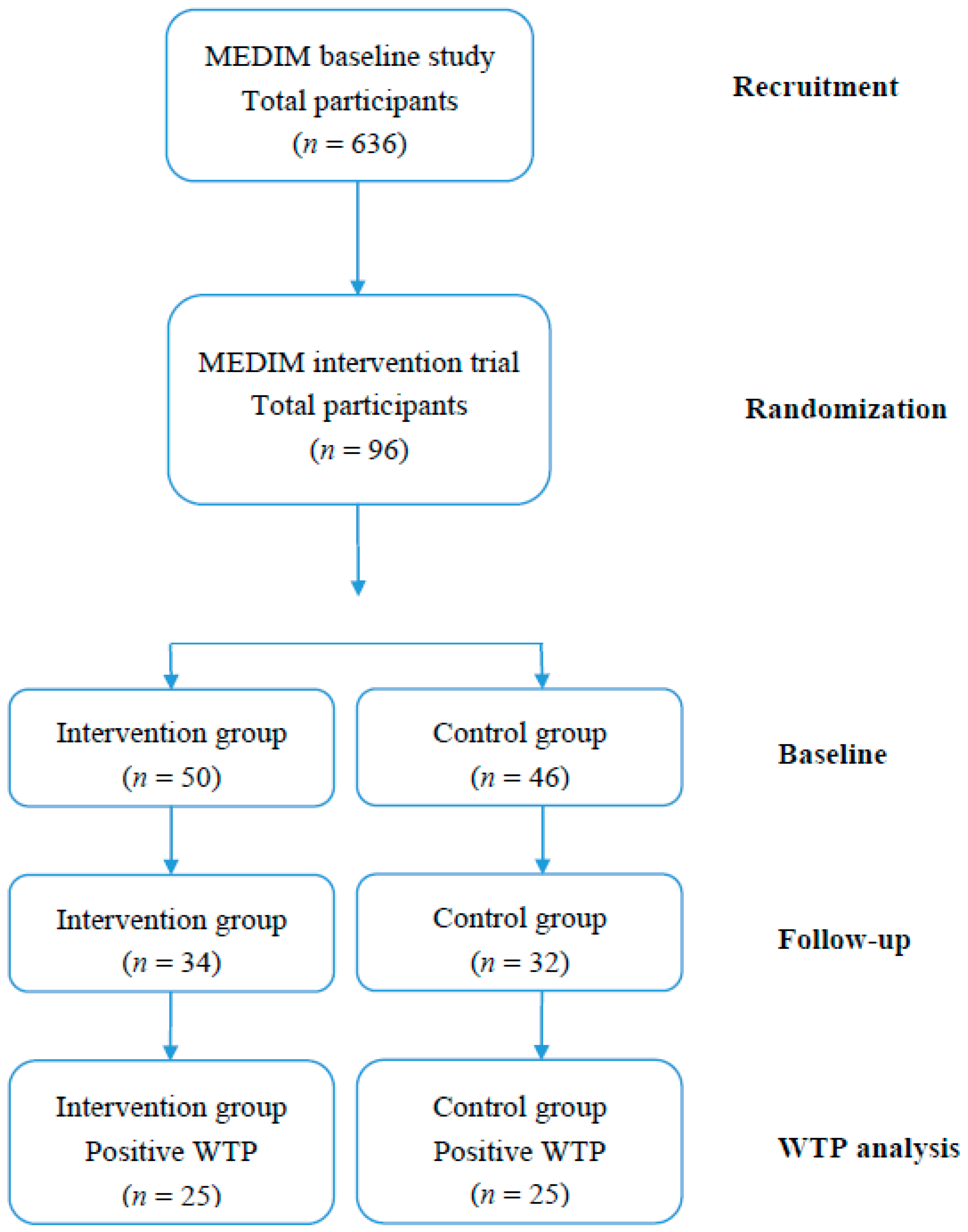
2. Materials and Methods
2.1. The Intervention
2.2. Willingness to Pay (WTP)
2.3. Variables Studied
2.4. Statistical Analyses
2.5. Ethical Approval
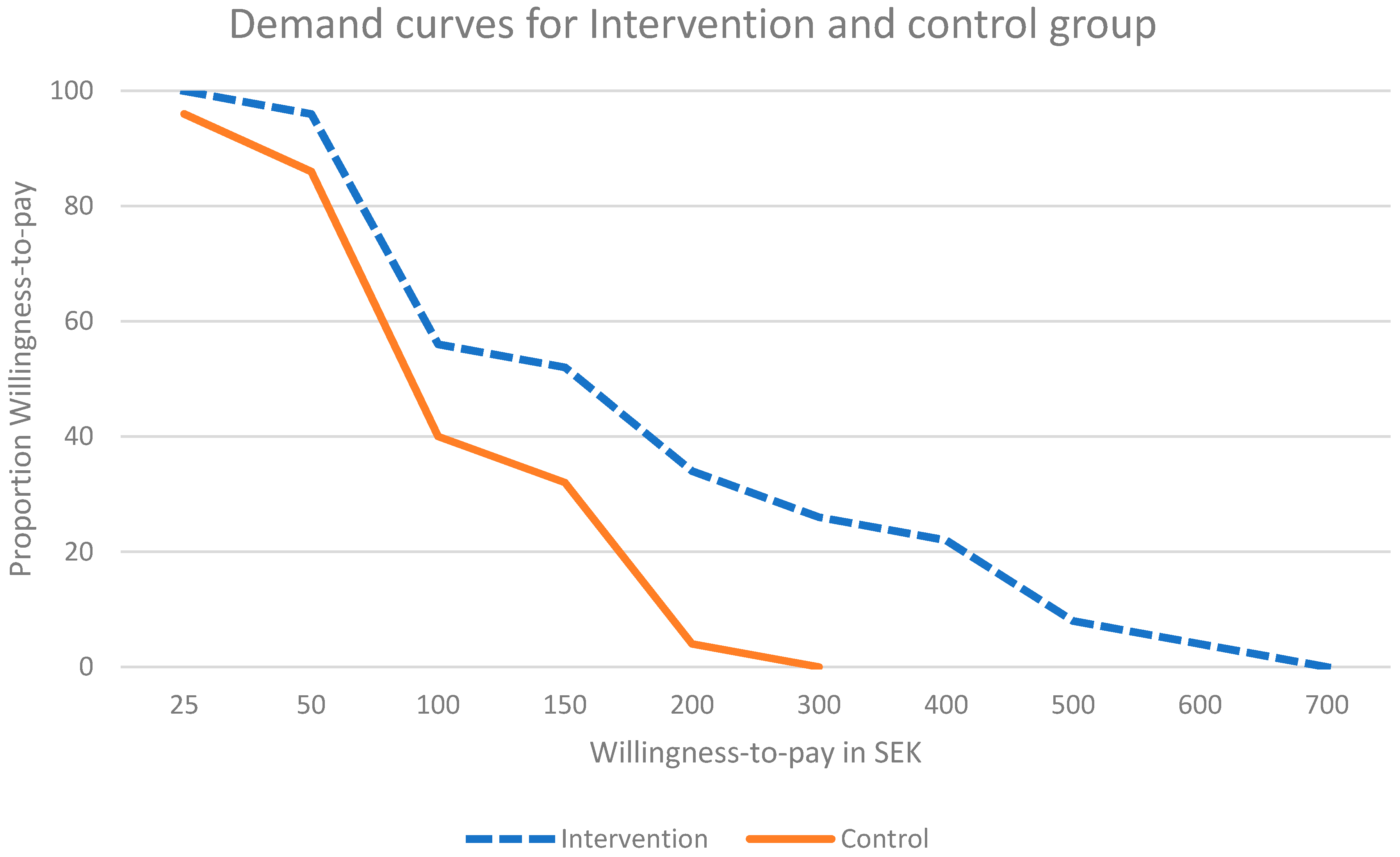
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Schellenberg, E.S.; Dryden, D.M.; Vandermeer, B.; Ha, C.; Korownyk, C. Lifestyle interventions for patients with and at risk for type 2 diabetesa systematic review and meta-analysis. Ann. Intern. Med. 2013, 159, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Gerdtham, U.G.; Johansson, P. Economic evaluation of lifestyle interventions for prevention of diabetes and cardiovascular diseases. Int. J. Environ. Res. Public Health 2010, 7, 3150–3159. [Google Scholar] [CrossRef] [PubMed]
- Bennet, L.; Groop, L.; Lindblad, U.; Agardh, C.D.; Franks, P.W. Ethnicity is an independent risk indicator when estimating diabetes risk with findrisc scores: A cross sectional study comparing immigrants from the middle east and native swedes. Prim. Care Diabetes 2014, 8, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Ballotari, P.; Caroli, S.; Ferrari, F.; Romani, G.; Marina, G.; Chiarenza, A.; Manicardi, V.; Giorgi Rossi, P. Differences in diabetes prevalence and inequalities in disease management and glycaemic control by immigrant status: A population-based study (Italy). BMC Public Health 2015, 15, 9. [Google Scholar] [CrossRef] [PubMed]
- Thabit, H.; Shah, S.; Nash, M.; Brema, I.; Nolan, J.; Martin, G. Globalization, immigration and diabetes self-management: An empirical study amongst immigrants with type 2 diabetes mellitus in Ireland. QJM Mon. J. Assoc. Physician 2009, 102, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Bennet, L.; Groop, L.; Franks, P.W. Ethnic differences in the contribution of insulin action and secretion to type 2 diabetes in immigrants from the middle east compared to native Swedes. Diabetes Res. Clin. Pract. 2014, 105, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Rechel, B.; Mladovsky, P.; Ingleby, D.; Mackenbach, J.P.; McKee, M. Migration and health in an increasingly diverse Europe. Lancet 2013, 381, 1235–1245. [Google Scholar] [CrossRef]
- Caperchione, C.M.; Kolt, G.S.; Mummery, W.K. Physical activity in culturally and linguistically diverse migrant groups to western society. Sports Med. 2009, 39, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Jaber, L.A.; Pinelli, N.R.; Brown, M.B.; Funnell, M.M.; Anderson, R.; Hammad, A.; Herman, W.H. Feasibility of group lifestyle intervention for diabetes prevention in Arab Americans. Diabetes Res. Clin. Pract. 2011, 91, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Saha, S.; Leijon, M.; Gerdtham, U.; Sundquist, K.; Sundquist, J.; Arvidsson, D.; Bennet, L. A culturally adapted lifestyle intervention addressing a middle eastern immigrant population at risk of diabetes, the MEDIM (impact of Migration and Ethnicity on Diabetes in Malmö): Study protocol for a randomized controlled trial. Trials 2013, 14, 279. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, F.; Kurbasic, A.; Lindblad, U.; Nilsson, P.M.; Bennet, L. Effects of a culturally adapted lifestyle intervention on cardio-metabolic outcomes: A randomised controlled trial in iraqi immigrants to Sweden at high risk of type 2 diabetes. Metabolism 2017, 66, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Van Gils, P.F.; Lambooij, M.S.; Flanderijn, M.; van den Berg, M.; de Wit, G.A.; Schuit, A.J.; Struijs, J.N. Willingness to participate in a lifestyle intervention program of patients with type 2 diabetes mellitus: A conjoint analysis. Patient Prefer. Adherence 2011, 5, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Veldwijk, J.; Lambooij, M.S.; van Gils, P.F.; Struijs, J.N.; Smit, H.A.; de Wit, G.A. Type 2 diabetes patients’ preferences and willingness to pay for lifestyle programs: A discrete choice experiment. BMC Public Health 2013, 13, 1099. [Google Scholar] [CrossRef] [PubMed]
- Johnson, F.R.; Manjunath, R.; Mansfield, C.A.; Clayton, L.J.; Hoerger, T.J.; Zhang, P. High-risk individuals’ willingness to pay for diabetes risk-reduction programs. Diabetes Care 2006, 29, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.f. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; world Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Diabetes Prevention Program (DPP) Research Group. The diabetes prevention program (DPP): Description of lifestyle intervention. Diabetes Care 2002, 25, 2165–2171. [Google Scholar]
- Siddiqui, F.; Winther, V.; Kurbasic, A.; Sonestedt, E.; Lundgren, K.B.; Lindeberg, S.; Nilsson, P.M.; Bennet, L. Changes in dietary intake following a culturally adapted lifestyle intervention among Iraqi immigrants to Sweden at high risk of type 2 diabetes: A randomised trial. Public Health Nutr. 2017, 20, 2827–2838. [Google Scholar] [CrossRef] [PubMed]
- Gafni, A. Willingness to pay. PharmacoEconomics 1998, 14, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Klose, T. The contingent valuation method in health care. Health Policy 1999, 47, 97–123. [Google Scholar] [CrossRef]
- Frew, E.J.; Whynes, D.K.; Wolstenholme, J.L. Eliciting willingness to pay: Comparing closed-ended with open-ended and payment scale formats. Med. Decis. Making 2003, 23, 150–159. [Google Scholar] [CrossRef] [PubMed]
- McIntosh, E. Applied Methods of Cost-Benefit Analysis in Health Care; Oxford University Press: Oxford, UK, 2010; Volume 4. [Google Scholar]
- Sveriges Riskbank. Available online: https://www.riksbank.se/en-gb/statistics/search-interest--exchange-rates/annual-average-exchange-rates/?y=2015&m=12&s=Comma&f=y (accessed on 26 February 2018).
- Laroche, M. Health status and health services utilization of Canada’s immigrant and non-immigrant populations. Can. Public Pol.-Anal. Polit. 2000, 26, 51–75. [Google Scholar] [CrossRef]
- Shah, M.; Zhu, K.; Wu, H.; Potter, J. Hispanic acculturation and utilization of cervical cancer screening in the U.S. Prev. Med. 2006, 42, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Fu, T.-T.; Lin, Y.-M.; Huang, C.L. Willingness to pay for obesity prevention. Econ. Hum. Biol. 2011, 9, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Romé, Å.; Persson, U.; Ekdahl, C.; Gard, G. Willingness to pay for health improvements of physical activity on prescription. Scand. J. Public Health 2010, 38, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Agardh, E.E.; Sidorchuk, A.; Hallqvist, J.; Ljung, R.; Peterson, S.; Moradi, T.; Allebeck, P. Burden of type 2 diabetes attributed to lower educational levels in Sweden. Popul. Health Metr. 2011, 9, 60. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M. Ethnic differences in social participation and social capital in Malmö, Sweden: A population-based study. Soc. Sci. Med. 2005, 60, 1527–1546. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.D. Construction of the contingent valuation market in health care: A critical assessment. Health Econ. 2003, 12, 609–628. [Google Scholar] [CrossRef] [PubMed]
- Carson, R.T.; Groves, T. Incentive and informational properties of preference questions. Environ. Resour. Econ. 2007, 37, 181–210. [Google Scholar] [CrossRef]
- Heinzen, R.R.; Bridges, J.F.P. Comparison of four contingent valuation methods to estimate the economic value of a pneumococcal vaccine in Bangladesh. Int. J. Technol. Assess. Health Care 2008, 24, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.D. Contingent valuation in health care: Does it matter how the “good” is described? Health Econ. 2008, 17, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Andreoni, J. Impure altruism and donations to public goods: A theory of warm-glow giving. Econ. J. 1990, 100, 464–477. [Google Scholar] [CrossRef]
- Shiell, A.; Gold, L. Contingent valuation in health care and the persistence of embedding effects without the warm glow. J. Econ. Psychol. 2002, 23, 251–262. [Google Scholar] [CrossRef]
- Donaldson, C.; Jones, A.M.; Mapp, T.J.; Olson, J.A. Limited dependent variables in willingness to pay studies: Applications in health care. Appl. Econ. 1998, 30, 667–677. [Google Scholar] [CrossRef]
- Frew, E.; Wolstenholme, J.L.; Whynes, D.K. Willingness-to-pay for colorectal cancer screening. Eur. J. Cancer 2001, 37, 1746–1751. [Google Scholar] [CrossRef]
- Diamond, P.A.; Hausman, J.A. Contingent valuation: Is some number better than no number? J. Econ. Perspect. 1994, 8, 45–64. [Google Scholar] [CrossRef]
- Nilsen, V.; Bakke, P.S.; Rohde, G.; Gallefoss, F. Predictors of health-related quality of life changes after lifestyle intervention in persons at risk of type 2 diabetes mellitus. Qual. Life Res. 2014, 23, 2585–2593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martín-Fernández, J.; del Cura-González, M.I.; Gómez-Gascón, T.; Oliva-Moreno, J.; Domínguez-Bidagor, J.; Beamud-Lagos, M.; Pérez-Rivas, F.J. Differences between willingness to pay and willingness to accept for visits by a family physician: A contingent valuation study. BMC Public Health 2010, 10, 11. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, B.; Bleichrodt, H.; Eeckhoudt, L. The economic value of informal care: A study of informal caregivers’ and patients’ willingness to pay and willingness to accept for informal care. Health Econ. 2005, 14, 363–376. [Google Scholar] [CrossRef] [PubMed]
| Variables | Control Group (n = 32) | Intervention Group (n = 34) | p Value |
|---|---|---|---|
| Age a | 48.78 (8.54) | 50.76 (10.40) | 0.402 |
| Body mass index (BMI) b | |||
| ≥30 | 17 (53%) | 18 (53%) | 0.98 |
| <30 | 15 (47%) | 16 47%) | |
| Sex b | |||
| Male | 17 (53%) | 19 (56%) | 0.46 |
| Female | 15 (47%) | 15 (44%) | |
| Education b | |||
| High | 22 (69%) | 29 (85%) | 0.11 |
| Low | 10 (31%) | 5 (15%) | |
| Marital status b | |||
| Married or living together | 26 (81%) | 29 (85%) | 0.66 |
| Single | 6 (19%) | 5 (15%) | |
| Job in last 12 months b | |||
| Yes | 18 (56%) | 16 (47%) | 0.46 |
| No | 14 (44%) | 18 (53%) | |
| Job type c | |||
| Self-employed | 3 (9%) | 4 (12%) | 0.53 |
| Permanent/temporary | 29 (91%) | 30 (88%) | |
| Migration duration b | |||
| ≤10 years | 7 (22%) | 12 (35%) | 0.23 |
| >10 years | 25 (78%) | 22 (65%) | |
| Language(s) spoken at home b | |||
| Mother tongue only | 23 (72%) | 28 (82%) | 0.31 |
| Swedish and mother tongue | 9 (28%) | 6 (18%) | |
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (SE) | p | OR (SE) | p | OR (SE) | p | OR (SE) | p | OR (SE) | p | OR (SE) | p | |
| Intervention group | 0.777 (0.45) | 0.66 | 0.777 (0.45) | 0.66 | 0.49 (0.33) | 0.30 | 0.85 (0.51) | 0.79 | 0.85 (0.50) | 0.79 | 0.49 (0.36) | 0.33 |
| BMI at baseline (<30) | 0.85 (0.49) | 0.78 | 1.07 (0.7) | 0.91 | ||||||||
| Age | 0.96 (0.03) | 0.23 | 0.95 (0.04) | 0.17 | ||||||||
| Sex (male) | 4.1 (0.17) | 0.04 | 0.22 (1.7) | 0.047 | ||||||||
| Education (high) | 4.6 (3.43) | 0.04 | 4.21 (3.5) | 0.08 | ||||||||
| Marital status (single) | 0.50 (0.42) | 0.42 | 0.43 (0.4) | 0.36 | ||||||||
| Language at home (mother tongue) | 2.40 (1.9) | 0.29 | 2.85 (2.7) | 0.27 | ||||||||
| Migration duration (>10 years) | 1.12 (0.72) | 0.86 | 1.71 (1.4) | 0.51 | ||||||||
| Job in last 12 months (no) | 0.39 (0.26) | 0.16 | 0.54 (0.44) | 0.45 | ||||||||
| Types of job (self-employed) | 2.26 (2.25) | 0.416 | 1.72 (1.93) | 0.63 | ||||||||
| Adjusted R squared | 0.02 | 0.00 | 0.20 | 0.06 | 0.03 | 0.27 | ||||||
| Statistics | All Participants (n = 50) | Intervention (n = 25) | Control (n = 25) |
|---|---|---|---|
| Mean a | 171.50 | 216 | 127 |
| Standard error of mean | 19.09 | 33.63 | 13.84 |
| Mean (5% trimmed) | 154 | 199 | 124 |
| Median | 100 | 200 | 100 |
| Mode | 100 | 100 | 100 |
| Coefficients of skewness | 0.529 | 0.689 | 0.390 |
| Percentiles | |||
| 25 | 100 | 100 | 75 |
| 50 | 100 | 200 | 100 |
| 75 | 200 | 250 | 200 |
| 90 | 300 | 540 | 200 |
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p | |
| Intervention group | 0.463 (0.18) | 0.014 | 0.429 (0.18) | 0.021 | 0.455 (0.19) | 0.023 | 0.548 (0.18) | 0.004 | 0.43 (0.17) | 0.013 | 0.38 (0.18) | 0.045 |
| BMI at baseline (<30) | −0.28 (0.18) | 0.120 | −0.21 (0.18) | 0.25 | ||||||||
| Age | 0.003 (0.01) | 0.76 | 0.004 (0.01) | 0.63 | ||||||||
| Sex (male) | 0.024 (0.19) | 0.90 | −0.28 (0.18) | 0.14 | ||||||||
| Education (high) | 0.017 (0.25) | 0.90 | −0.21 (0.25) | 0.40 | ||||||||
| Marital status (single) | 0.20 (0.26) | 0.45 | 0.32 (0.24) | 0.18 | ||||||||
| Language at home (mother tongue) | 0.412 (0.2) | 0.045 | 0.22 (0.22) | 0.31 | ||||||||
| Migration duration (>10 years) | 0.204 (0.2) | 0.320 | −0.06 (0.24) | 0.79 | ||||||||
| Job in last 12 months (no) | −0.05 (0.17) | 0.771 | −0.09 (0.2) | 0.65 | ||||||||
| Types of job (self-employed) | −0.926 (0.29) | 0.003 | −1.06 (0.32) | 0.002 | ||||||||
| Adjusted R squared | 0.10 | 0.14 | 0.04 | 0.16 | 0.26 | 0.27 | ||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saha, S.; Gerdtham, U.-G.; Siddiqui, F.; Bennet, L. Valuing a Lifestyle Intervention for Middle Eastern Immigrants at Risk of Diabetes. Int. J. Environ. Res. Public Health 2018, 15, 413. https://doi.org/10.3390/ijerph15030413
Saha S, Gerdtham U-G, Siddiqui F, Bennet L. Valuing a Lifestyle Intervention for Middle Eastern Immigrants at Risk of Diabetes. International Journal of Environmental Research and Public Health. 2018; 15(3):413. https://doi.org/10.3390/ijerph15030413
Chicago/Turabian StyleSaha, Sanjib, Ulf-G. Gerdtham, Faiza Siddiqui, and Louise Bennet. 2018. "Valuing a Lifestyle Intervention for Middle Eastern Immigrants at Risk of Diabetes" International Journal of Environmental Research and Public Health 15, no. 3: 413. https://doi.org/10.3390/ijerph15030413
APA StyleSaha, S., Gerdtham, U.-G., Siddiqui, F., & Bennet, L. (2018). Valuing a Lifestyle Intervention for Middle Eastern Immigrants at Risk of Diabetes. International Journal of Environmental Research and Public Health, 15(3), 413. https://doi.org/10.3390/ijerph15030413





