Symptom Structure of Depression in Older Adults on the Qinghai–Tibet Plateau: A Network Analysis
Abstract
:1. Introduction
2. Materials and Methods
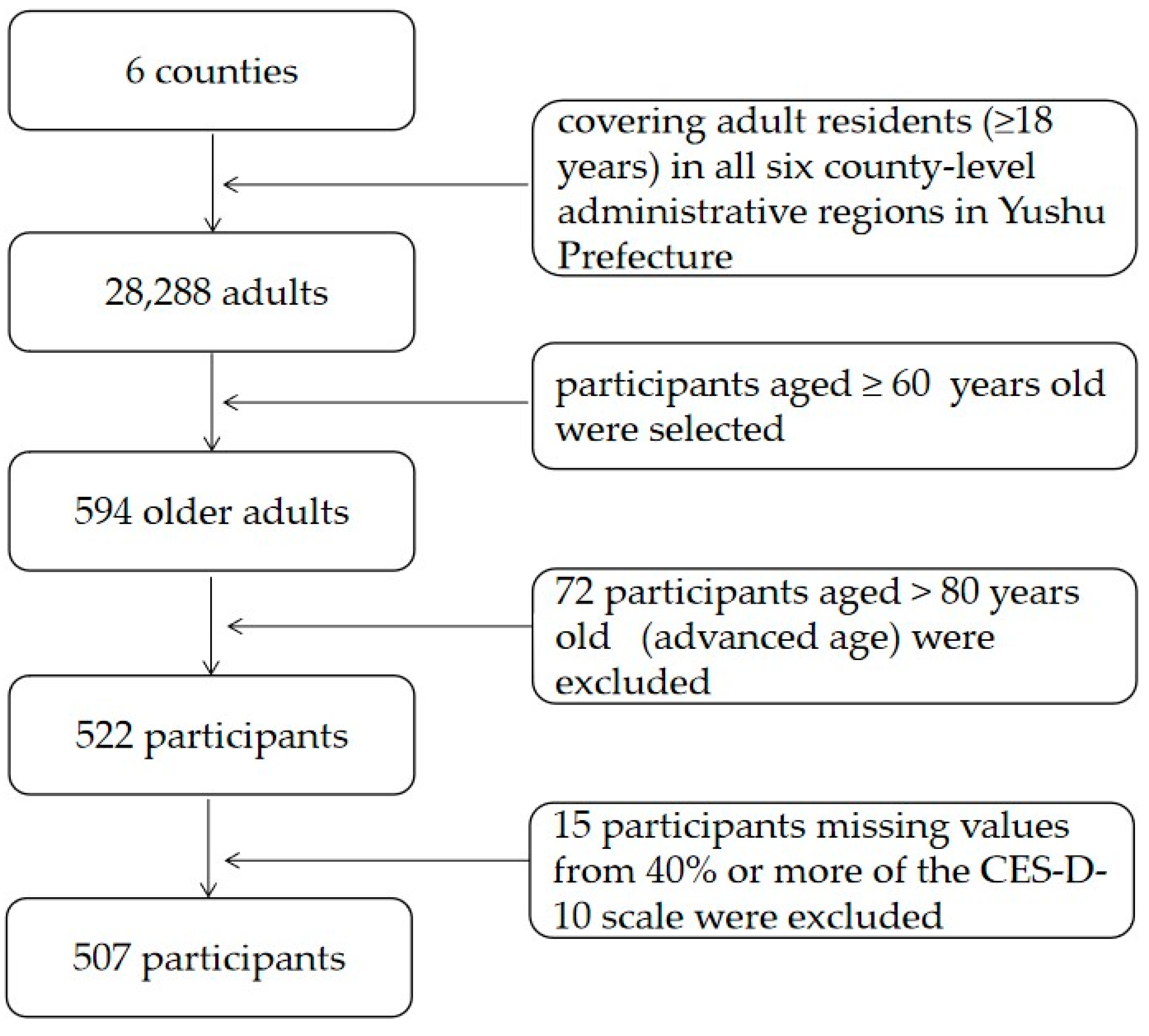
2.1. Participants
2.2. Procedure
2.3. Measures
2.4. Statistical Analyses
2.4.1. Network Estimation
2.4.2. Centrality Estimation
2.4.3. Network Accuracy, Stability, and Significance Testing
3. Results
3.1. Descriptive Analyses
3.2. Network Structure and Centrality Estimation
3.3. Network Accuracy and Stability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hernández-Vásquez, A.; Vargas-Fernández, R.; Rojas-Roque, C.; Gamboa-Unsihuay, J.E. Association between altitude and depression in Peru: An 8-year pooled analysis of population-based surveys. J. Affect. Disord. 2022, 299, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Yamanaka, G.; Yamamoto, N.; Nakaoka, T.; Okumiya, K.; Matsubayashi, K.; Otsuka, K.; Sakura, H. Depression and altitude: Cross-sectional community-based study among elderly high-altitude residents in the Himalayan regions. Cult. Med. Psychiatry 2016, 40, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Eli, B.; Zhou, Y.; Liang, Y.; Cheng, J.; Wang, J.; Huang, C.; Xuan, X.; Liu, Z. Depression in children and adolescents on the Qinghai-Tibet plateau: Associations with resilience and prosocial behavior. Int. J. Environ. Res. Public Health 2021, 18, 440. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, Y.; Liang, Y.; Liu, Z. A large sample survey of Tibetan people on the Qinghai–Tibet plateau: Current situation of depression and risk factors. Int. J. Environ. Res. Public Health 2020, 17, 289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kious, B.M.; Bakian, A.; Zhao, J.; Mickey, B.; Guille, C.; Renshaw, P.; Sen, S. Altitude and risk of depression and anxiety: Findings from the intern health study. Int. Rev. Psychiatry 2019, 31, 637–645. [Google Scholar] [CrossRef] [Green Version]
- Krsteska, R.; Pejoska, V.G. The association of poor economic condition and family relations in childhood with late-life depression. Psychiatr. Danub. 2013, 25, 241–247. [Google Scholar] [PubMed]
- Maldonado, M.D.; Reiter, R.J.; Pérez-San-Gregorio, M.A. Melatonin as a potential therapeutic agent in psychiatric illness. Hum. Psychopharmacol. Clin. 2009, 24, 391–400. [Google Scholar] [CrossRef]
- Ray, K.; Dutta, A.; Panjwani, U.; Thakur, L.; Kumar, S. Hypobaric hypoxia modulates brain biogenic amines and disturbs sleep architecture. Neurochem. Int. 2011, 58, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.B.; Fang, Y.P.; Yang, X.T.; Qiu, X.P.; Hu, Y. Effects of altitude on county economic development in China. J. Mt. Sci. 2018, 15, 406–418. [Google Scholar] [CrossRef]
- Schaakxs, R.; Comijs, H.C.; Van Der Mast, R.C.; Schoevers, R.A.; Beekman, A.T.F.; Penninx, B.W.J.H. Risk factors for depression: Differential across age? Am. J. Geriatr. Psychiatry 2017, 25, 966–977. [Google Scholar] [CrossRef]
- Amha, H.; Fente, W.; Sintayehu, M.; Tesfaye, B.; Yitayih, M. Depression and associated factors among old age population in Dega damot district, North West Ethiopia. A cross-sectional study. J. Affect. Disord. Rep. 2020, 2, 100034. [Google Scholar]
- Luppa, M.; Sikorski, C.; Luck, T.; Ehreke, L.; Konnopka, A.; Wiese, B.; Weyerer, S.; König, H.-H.; Riedel-Heller, S. Age-and gender-specific prevalence of depression in latest-life–systematic review and meta-analysis. J. Affect. Disord. 2012, 136, 212–221. [Google Scholar] [CrossRef] [PubMed]
- Brandão, D.J.; Fontenelle, L.F.; Da Silva, S.A.; Menezes, P.R.; Pastor-Valero, M.A. Depression and excess mortality in the elderly living in low- and middle-income countries: Systematic review and meta-analysis. Int. J. Geriatr. Psychiatry 2018, 34, 22–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, L.; Wei, G.; Yan, X.U.; Huang, Y.; Liu, X.; Li, T.; Guo, W.J. Psychiatric epidemiology and mental health service in the Tibet autonomous region of the People’s Republic of China. Shanghai Arch. Psychiatry 2018, 30, 127–130. [Google Scholar] [PubMed]
- Wang, F.; Liu, S.; Zhang, Q.; Ng, C.H.; Cui, X.; Zhang, D.; Xiang, Y.-T. Prevalence of depression in older nursing home residents in high and low altitude regions: A comparative study. Front. Psychiatry 2021, 12, 669234. [Google Scholar] [CrossRef] [PubMed]
- Fried, E.I. Problematic assumptions have slowed down depression research: Why symptoms, not syndromes are the way forward. Front. Psychol. 2015, 6, 309. [Google Scholar] [CrossRef] [Green Version]
- Schmittmann, V.D.; Cramer, A.O.; Waldorp, L.; Epskamp, S.; Kievit, R.A.; Borsboom, D. Deconstructing the construct: A network perspective on psychological phenomena. New Ideas Psychol. 2013, 31, 43–53. [Google Scholar] [CrossRef]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boschloo, L.; Van Borkulo, C.D.; Borsboom, D.; Schoevers, R.A. A prospective study on how symptoms in a network predict the onset of depression. Psychother. Psychosom. 2016, 85, 183–184. [Google Scholar] [CrossRef]
- Langera, J.K.; Tongea, N.A.; Piccirilloa, M.; Rodebaugha, T.L.; Thompsona, R.J.; Gotlibb, I.H. Symptoms of social anxiety disorder and major depressive disorder: A network perspective. J. Affect. Disord. 2019, 243, 531–538. [Google Scholar] [CrossRef]
- Van Loo, H.; Van Borkulo, C.; Peterson, R.; Fried, E.; Aggen, S.; Borsboom, D.; Kendler, K. Robust symptom networks in recurrent major depression across different levels of genetic and environmental risk. J. Affect. Disord. 2018, 227, 313–322. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mullarkey, M.C.; Igor Marchetti, I.; Beevers, C.G. Using network analysis to identify central symptoms of adolescent depression. J. Clin. Child Adolesc. Psychol. 2019, 48, 656–668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rubin, M.; Bicki, A.; Papini, S.; Smits, J.A.J.; Telch, M.J.; Gray, J.S. Distinct trajectories of depression symptoms in early and middle adolescence: Preliminary evidence from longitudinal network analysis. J. Psychiatr. Res. 2021, 142, 198–203. [Google Scholar] [CrossRef]
- Schweren, L.; Van Borkulo, C.D.; Fried, E.; Goodyer, I.M. Assessment of symptom network density as a prognostic marker of treatment response in adolescent depression. JAMA Psychiatry 2018, 75, 98–100. [Google Scholar] [CrossRef] [Green Version]
- Fried, E.I.; Epskamp, S.; Nesse, R.M.; Tuerlinckx, F.; Borsboom, D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord. 2016, 189, 314–320. [Google Scholar]
- Hartung, T.J.; Fried, E.I.; Mehnert, A.; Hinz, H.; Vehling, S. Frequency and network analysis of depressive symptoms in patients with cancer compared to the general population. J. Affect. Disord. 2019, 256, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Herniman, S.E.; Phillips, L.J.; Wood, S.J.; Cotton, S.M.; Liemburg, E.J.; Allott, K.A. Interrelationships between depressive symptoms and positive and negative symptoms of recent onset schizophrenia spectrum disorders: A network analytical approach. J. Psychiatr. Res. 2021, 140, 373–380. [Google Scholar] [CrossRef]
- Pan, H.; Liu, Q. Difference of depression between widowed and non-widowed older people in China: A network analysis approach. J. Affect. Disord. 2021, 280, 68–76. [Google Scholar] [CrossRef]
- Forbes, M.K.; Wright, A.; Markon, K.E.; Krueger, R.F. Evidence that psychopathology symptom networks have limited replicability. J. Abnorm. Psychol. 2017, 126, 969–988. [Google Scholar] [CrossRef]
- Qinghai Daily Digital. Qinghai Provincial Seventh National Population Census Bulletin. Qinghai Daily, 16 June 2021; p. 1. [Google Scholar]
- Andresen, E.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Huang, Q.; Wang, X.; Chen, G. Reliability and validity of 10-item CES-D among middle aged and older adults in China. China J. Health Psychol. 2015, 23, 1036–1041. [Google Scholar]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fruchterman, T.M.J.; Reingold, M. Graph drawing by force-directed placement. Softw. Pract. Exp. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Heeren, A.; Jones, P.J.; Mcnally, R.J. Mapping network connectivity among symptoms of social anxiety and comorbid depression in people with social anxiety disorder. J. Affect. Disord. 2018, 228, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Hallquist, M.; Wright, A.G.C.; Molenaar, P.C.M. Problems with centrality measures in psychopathology symptom networks: Why network psychometrics cannot escape psychometric theory. Multivar. Behav. Res. 2019, 56, 199–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bringmann, L.F.; Elmer, T.; Epskamp, S.; Krause, R.W.; Snippe, E. What do centrality measures measure in psychological networks? J. Abnorm. Psychol. 2018, 128, 892–903. [Google Scholar] [CrossRef] [Green Version]
- Fried, E.I.; Eidhof, M.B.; Palic, S.; Costantini, G.; Huisman-Van Dijk, H.M.; Bockting, C.L.H.; Engelhard, I.; Armour, C.; Nielsen, A.B.S.; Karstoft, K.-I. Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clin. Psychol. Sci. 2018, 6, 335–351. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Chow, I.; Lu, L.; Ren, Y.M.; Xiang, Y.T. Comparison of sleep disturbances between older nursing home residents in high- and low-altitude areas. J. Geriatr. Psychiatry Neurol. 2019, 33, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.; Ga, Q.; Li, R.; Bai, Z.-Z.; Wuren, T.; Wang, J.; Yang, Y.-Z.; Li, Y.-H.; Ge, R.-L. Sleep disturbances in long-term immigrants with chronic mountain sickness: A comparison with healthy immigrants at high altitude. Respir. Physiol. Neurobiol. 2015, 206, 4–10. [Google Scholar] [CrossRef]
- Sakamoto, R.; Okumiya, K.; Norboo, T.; Tsering, N.; Yamaguchi, T.; Nose, M. Sleep quality among elderly high-altitude dwellers in ladakh. Psychiatry Res. 2017, 249, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Paunio, T.; Korhonen, T.; Hublin, C.; Partinen, M.; Koskenvuo, K.; Koskenvuo, M.; Kaprio, J. Poor sleep predicts symptoms of depression and disability retirement due to depression. J. Affect. Disord. 2015, 172, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Eli, B.; Zhou, Y.; Liang, Y.; Fu, L.; Zheng, H.; Liu, Z. A profile analysis of post-traumatic stress disorder and depressive symptoms among Chinese Shidu parents. Eur. J. Psychotraumatol. 2020, 11, 1766770. [Google Scholar] [CrossRef]
- Stafford, M.; Bendayan, R.; Tymoszuk, U.; Kuh, D. Social support from the closest person and sleep quality in later life: Evidence from a British birth cohort study. J. Psychosom. Res. 2017, 98, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.; Warren, L. Hopes, fears and expectations about the future: What do older people’s stories tell us about active ageing? Ageing Soc. 2007, 27, 465–488. [Google Scholar] [CrossRef]
- Synowiec-Piat, M.; Paga, A. Fear of cancer and older people’s beliefs about cancer treatment in Poland. J. Psychosoc. Oncol. 2017, 36, 97–112. [Google Scholar] [CrossRef]
- Lloyd-Sherlock, P.; Agrawal, S.; Minicuci, N. Fear of crime and older people in low- and middle-income countries. Ageing Soc. 2016, 1, 1083–1108. [Google Scholar] [CrossRef]
- Ni Mhaolain, A.M.; Fan, C.W.; Romero-Ortuno, R.; Cogan, L.; Cunningham, C.; Lawlor, B.; Kenny, R.A. Depression: A modifiable factor in fearful older fallers transitioning to frailty? Int. J. Geriatr. Psychiatry 2012, 27, 727–733. [Google Scholar] [CrossRef]
- Miranda, R.; Mennin, D.S. Depression, generalized anxiety disorder, and certainty in pessimistic predictions about the future. Cognit. Ther. Res. 2007, 31, 71–82. [Google Scholar] [CrossRef]
- Sabute, E. Chapter 6.15: Depression in Young People and the Elderly. In Priority Medicines for Europe and World. “A Public Health Aproach to Innovation”; Background paper; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Mcnally, R.J.; Robinaugh, D.J.; Wu, G.W.Y.; Wang, L.; Deserno, M.K.; Borsboom, D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clin. Psychol. Sci. 2015, 3, 836–849. [Google Scholar] [CrossRef] [Green Version]
- Chen, X.; Liu, J.; Wang, J.; Xin, Z.; Zhang, Q.; Zhang, W.; Xi, Y.; Zhu, Y.; Li, C.; Li, J.; et al. Altered resting-state networks may explain the executive impairment in young health immigrants into high-altitude area. Brain Imaging Behav. 2021, 15, 147–156. [Google Scholar] [CrossRef]
- Moreira, H.S.; Costa, A.S.; Castro, S.L.; Lima, C.F.; Vicente, S.G. Assessing executive dysfunction in neurodegenerative disorders: A critical review of brief neuropsychological tools. Front. Aging Neurosci. 2017, 9, 369. [Google Scholar] [CrossRef]
- Schraegle, W.A.; Titus, J.B. Executive function and health-related quality of life in pediatric epilepsy. Epilepsy Behav. 2016, 62, 20–26. [Google Scholar] [CrossRef] [PubMed]


| Sociodemographic Characteristic | Category | n | % |
|---|---|---|---|
| a Sex | Male | 199 | 39.3 |
| Female | 300 | 59.2 | |
| a Education level | Never went to school | 368 | 72.6 |
| Primary school | 78 | 15.4 | |
| Junior high school | 37 | 7.3 | |
| High school or above | 18 | 3.6 | |
| a Marital status | First marriage | 441 | 87.0 |
| b Other | 57 | 11.2 | |
| a Marriage satisfaction | Dissatisfied | 8 | 1.6 |
| Neutral | 23 | 4.5 | |
| Satisfied | 438 | 86.4 | |
| a Monthly family income (RMB) | ≤2000 | 235 | 46.4 |
| >2000 | 254 | 50.0 | |
| a Number of people living together | 1–3 | 249 | 49.1 |
| 4–6 | 226 | 44.6 | |
| 7–12 | 31 | 6.1 | |
| CES-D-10 total score | ≥10 | 154 | 30.4 |
| <10 | 353 | 69.6 | |
| M | SD | ||
| Age | - | 67.42 | 5.61 |
| CES-D-10 total score | - | 7.83 | 5.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eli, B.; Zhou, Y.; Chen, Y.; Huang, X.; Liu, Z. Symptom Structure of Depression in Older Adults on the Qinghai–Tibet Plateau: A Network Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13810. https://doi.org/10.3390/ijerph192113810
Eli B, Zhou Y, Chen Y, Huang X, Liu Z. Symptom Structure of Depression in Older Adults on the Qinghai–Tibet Plateau: A Network Analysis. International Journal of Environmental Research and Public Health. 2022; 19(21):13810. https://doi.org/10.3390/ijerph192113810
Chicago/Turabian StyleEli, Buzohre, Yueyue Zhou, Yaru Chen, Xin Huang, and Zhengkui Liu. 2022. "Symptom Structure of Depression in Older Adults on the Qinghai–Tibet Plateau: A Network Analysis" International Journal of Environmental Research and Public Health 19, no. 21: 13810. https://doi.org/10.3390/ijerph192113810






