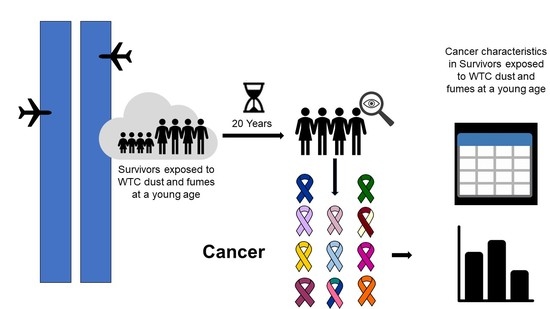
Characteristics of Cancers in Community Members Exposed to the World Trade Center Disaster at a Young Age
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Exposure Assessment
2.3. Cancer Information
2.4. Inclusion Criteria
2.5. Statistical Analysis
3. Results
3.1. Participants
3.2. Cancer Types
3.3. Hematologic Malignancies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| Acronym | Definition |
| BMI | Body mass index |
| CDC | Centers for Disease Control and Prevention |
| EYA | World Trade Center-exposed survivors who were exposed at a young age, age 30 or younger on 11 September 2001 |
| NIOSH | National Institute for Occupational Safety & Health |
| NYS | New York State |
| WTC | World Trade Center |
| WTC EHC | World Trade Center Environmental Health Center |
| WTCHP | World Trade Center Health Program |
| WTCHR | World Trade Center Health Registry |
| WTC EHC PCDB | World Trade Center Environmental Health Center pan-cancer database |
| 9/11 | 11 September 2001 |
Appendix A
| Level | Breast | Thyroid | Brain and Spinal Cord | Colon and Rectum | Head and Neck Sites | Melanoma of the Skin | Kidney | Lung | Pancreas | Soft Tissue Sarcoma | Non-Hodgkin Lymphoma | Hodgkin Lymphoma | Myeloma | Leukemia | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 74 | 42 | 6 | 6 | 4 | 4 | 3 | 3 | 2 | 2 | 11 | 8 | 4 | 3 | |
| Age at 9/11, median [range] | 26 [14, 30] | 23 [1, 30] | 28 [23, 30] | 26 [19, 30] | 21 [16, 22] | 26 [21, 29] | 28 [18, 30] | 28 [28, 29] | 29 [29, 29] | 26 [23, 29] | 27 [15, 30] | 26 [13, 29] | 28 [25, 28] | 27 [20, 30] | |
| Age at diagnosis, median [range] | 40 [27, 48] | 35 [13, 46] | 40 [35, 46] | 41 [29, 44] | 35 [26, 35] | 34 [29, 42] | 45 [32, 46] | 40 [34, 45] | 42 [37, 47] | 43 [39, 47] | 41 [22, 43] | 32 [19, 39] | 42 [38, 47] | 35 [34, 45] | |
| Race/Ethnicity, n (%) | NH-White | 27 (36.5) | 16 (47.1) | 2 (40.0) | 4 (80.0) | 0 (0.0) | 3 (75.0) | 1 (33.3) | 2 (66.7) | 1 (50.0) | 0 (0.0) | 2 (25.0) | 2 (28.6) | 0 (0.0) | 1 (33.3) |
| Hispanic | 14 (18.9) | 9 (26.5) | 1 (20.0) | 1 (20.0) | 1 (25.0) | 1 (25.0) | 2 (66.7) | 1 (33.3) | 1 (50.0) | 0 (0.0) | 3 (37.5) | 4 (57.1) | 2 (50.0) | 1 (33.3) | |
| Asian | 15 (20.3) | 7 (20.6) | 0 (0.0) | 0 (0.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 2 (25.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | |
| NH-Black | 16 (21.6) | 2 (5.9) | 1 (20.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 1 (12.5) | 1 (14.3) | 1 (25.0) | 0 (0.0) | |
| Native American/Other | 2 (2.7) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 0 (0.0) | |
| BMI, n (%) | Normal weight (<25) | 21 (41.2) | 10 (41.7) | 0 (0.0) | 3 (100.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 3 (33.3) | 4 (80.0) | 0 (NaN) | 0 (0.0) |
| Overweight (25–30) | 10 (19.6) | 9 (37.5) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 1 (50.0) | 1 (50.0) | 5 (55.6) | 1 (20.0) | 0 (NaN) | 1 (100.0) | |
| Obese (≥30) | 20 (39.2) | 5 (20.8) | 2 (66.7) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 2 (66.7) | 1 (33.3) | 1 (50.0) | 1 (50.0) | 1 (11.1) | 0 (0.0) | 0 (NaN) | 0 (0.0) | |
| Income, n (%) | ≤$30,000/year | 15 (21.7) | 11 (28.9) | 3 (60.0) | 1 (25.0) | 3 (75.0) | 0 (0.0) | 1 (33.3) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 3 (33.3) | 1 (12.5) | 1 (33.3) | 0 (0.0) |
| >$30,000/year | 54 (78.3) | 27 (71.1) | 2 (40.0) | 3 (75.0) | 1 (25.0) | 4 (100.0) | 2 (66.7) | 2 (66.7) | 2 (100.0) | 2 (100.0) | 6 (66.7) | 7 (87.5) | 2 (66.7) | 3 (100.0) | |
| Caught in WTC dust cloud, n (%) | No | 41 (56.2) | 18 (45.0) | 3 (60.0) | 3 (60.0) | 3 (75.0) | 3 (75.0) | 1 (33.3) | 2 (66.7) | 2 (100.0) | 1 (50.0) | 8 (72.7) | 3 (37.5) | 2 (66.7) | 3 (100.0) |
| Yes | 32 (43.8) | 22 (55.0) | 2 (40.0) | 2 (40.0) | 1 (25.0) | 1 (25.0) | 2 (66.7) | 1 (33.3) | 0 (0.0) | 1 (50.0) | 3 (27.3) | 5 (62.5) | 1 (33.3) | 0 (0.0) | |
| Exposure category, n (%) | Local Worker | 42 (57.5) | 17 (42.5) | 4 (80.0) | 2 (40.0) | 1 (25.0) | 2 (50.0) | 2 (66.7) | 2 (66.7) | 2 (100.0) | 2 (100.0) | 6 (54.5) | 3 (37.5) | 2 (66.7) | 1 (33.3) |
| Resident | 11 (15.1) | 6 (15.0) | 0 (0.0) | 1 (20.0) | 3 (75.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (18.2) | 3 (37.5) | 0 (0.0) | 1 (33.3) | |
| Student | 15 (20.5) | 14 (35.0) | 1 (20.0) | 1 (20.0) | 0 (0.0) | 1 (25.0) | 1 (33.3) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 1 (9.1) | 2 (25.0) | 0 (0.0) | 1 (33.3) | |
| Other | 5 (6.8) | 3 (7.5) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (18.2) | 0 (0.0) | 1 (33.3) | 0 (0.0) | |
| Smoking history, n (%) | Never | 64 (87.7) | 38 (97.4) | 4 (100.0) | 2 (50.0) | 4 (100.0) | 4 (100.0) | 2 (66.7) | 1 (33.3) | 1 (100.0) | 2 (100.0) | 11 (100.0) | 8 (100.0) | 2 (66.7) | 2 (66.7) |
| Former smoker | 9 (12.3) | 1 (2.6) | 0 (0.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 2 (66.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | |
| Current smoker | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) |
| Level | Thyroid | Head and Neck Sites | Testis | Kidney | Colon and Rectum | Brain and Spinal Cord | Prostate | Soft Tissue Sarcoma | Breast | Melanoma of the Skin | Small Intestine | Urinary Bladder | Hodgkin Lymphoma | Leukemia | Non-Hodgkin Lymphoma | Myeloma | Myeloproliferative Neoplasm | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 13 | 11 | 11 | 8 | 6 | 3 | 3 | 3 | 2 | 2 | 2 | 2 | 9 | 8 | 7 | 2 | 2 | |
| Age at 9/11, median [range] | 26 [18, 30] | 27 [20, 30] | 28 [20, 29] | 26 [0, 28] | 24 [16, 27] | 25 [21, 26] | 27 [24, 29] | 28 [22, 29] | 24 [23, 25] | 26 [24, 27] | 26 [23, 29] | 26 [25, 28] | 21 [8, 28] | 21 [3, 28] | 29 [20, 30] | 18 [16, 20] | 22 [19, 26] | |
| Age at diagnosis, median [range] | 37 [26, 45] | 39 [28, 46] | 40 [28, 43] | 40 [7, 43] | 36 [31, 43] | 36 [30, 38] | 45 [40, 47] | 34 [29, 41] | 40 [39, 41] | 36 [28, 45] | 37 [36, 38] | 36 [34, 39] | 35 [14, 43] | 32 [16, 39] | 38 [26, 41] | 32 [28, 35] | 16 [5, 27] | |
| Race/Ethnicity, n (%) | NH-White | 4 (44.4) | 5 (45.5) | 6 (60.0) | 5 (71.4) | 3 (60.0) | 0 (0.0) | 3 (100.0) | 2 (66.7) | 1 (50.0) | 1 (100.0) | 1 (50.0) | 0 (0.0) | 4 (50.0) | 1 (14.3) | 3 (50.0) | 1 (50.0) | 2 (100.0) |
| Hispanic | 0 (0.0) | 0 (0.0) | 3 (30.0) | 0 (0.0) | 1 (20.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (100.0) | 2 (25.0) | 1 (14.3) | 2 (33.3) | 0 (0.0) | 0 (0.0) | |
| Asian | 3 (33.3) | 2 (18.2) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (71.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| NH-Black | 2 (22.2) | 4 (36.4) | 1 (10.0) | 1 (14.3) | 1 (20.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 2 (25.0) | 0 (0.0) | 1 (16.7) | 1 (50.0) | 0 (0.0) | |
| Native American/Other | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| BMI, n (%) | Normal weight (<25) | 2 (22.2) | 4 (50.0) | 2 (20.0) | 3 (42.9) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (NaN) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 4 (57.1) | 0 (0.0) | 1 (50.0) | 0 (0.0) |
| Overweight (25–30) | 6 (66.7) | 1 (12.5) | 4 (40.0) | 2 (28.6) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 1 (50.0) | 0 (0.0) | 0 (NaN) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 2 (28.6) | 4 (66.7) | 1 (50.0) | 2 (100.0) | |
| Obese (≥30) | 1 (11.1) | 3 (37.5) | 4 (40.0) | 2 (28.6) | 4 (100.0) | 1 (100.0) | 1 (33.3) | 0 (0.0) | 1 (100.0) | 0 (NaN) | 1 (100.0) | 2 (100.0) | 0 (0.0) | 1 (14.3) | 2 (33.3) | 0 (0.0) | 0 (0.0) | |
| Income, n (%) | ≤$30,000/year | 4 (44.4) | 2 (20.0) | 3 (30.0) | 0 (0.0) | 1 (16.7) | 1 (33.3) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 1 (50.0) | 1 (14.3) | 3 (50.0) | 2 (33.3) | 1 (50.0) | 1 (50.0) |
| >$30,000/year | 5 (55.6) | 8 (80.0) | 7 (70.0) | 7 (100.0) | 5 (83.3) | 2 (66.7) | 3 (100.0) | 1 (50.0) | 2 (100.0) | 1 (100.0) | 1 (50.0) | 1 (50.0) | 6 (85.7) | 3 (50.0) | 4 (66.7) | 1 (50.0) | 1 (50.0) | |
| Caught in WTC dust cloud, n (%) | No | 4 (33.3) | 5 (45.5) | 6 (60.0) | 4 (57.1) | 5 (83.3) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 2 (100.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 5 (62.5) | 6 (75.0) | 4 (57.1) | 1 (50.0) | 1 (50.0) |
| Yes | 8 (66.7) | 6 (54.5) | 4 (40.0) | 3 (42.9) | 1 (16.7) | 2 (66.7) | 2 (66.7) | 2 (66.7) | 0 (0.0) | 1 (50.0) | 2 (100.0) | 2 (100.0) | 3 (37.5) | 2 (25.0) | 3 (42.9) | 1 (50.0) | 1 (50.0) | |
| Exposure category, n (%) | Local Worker | 5 (41.7) | 6 (54.5) | 5 (50.0) | 5 (71.4) | 2 (33.3) | 1 (33.3) | 2 (66.7) | 1 (33.3) | 1 (50.0) | 1 (50.0) | 2 (100.0) | 2 (100.0) | 6 (75.0) | 2 (25.0) | 7 (100.0) | 1 (50.0) | 1 (50.0) |
| Resident | 2 (16.7) | 3 (27.3) | 2 (20.0) | 0 (0.0) | 2 (33.3) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 1 (50.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 2 (25.0) | 3 (37.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Student | 3 (25.0) | 2 (18.2) | 2 (20.0) | 2 (28.6) | 1 (16.7) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (25.0) | 0 (0.0) | 1 (50.0) | 1 (50.0) | |
| Other | 2 (16.7) | 0 (0.0) | 1 (10.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Smoking history, n (%) | Never | 11 (91.7) | 7 (77.8) | 8 (80.0) | 6 (85.7) | 6 (100.0) | 2 (66.7) | 2 (66.7) | 3 (100.0) | 2 (100.0) | 2 (100.0) | 2 (100.0) | 1 (50.0) | 7 (87.5) | 7 (87.5) | 5 (71.4) | 2 (100.0) | 0 (0.0) |
| Former smoker | 1 (8.3) | 2 (22.2) | 2 (20.0) | 1 (14.3) | 0 (0.0) | 1 (33.3) | 1 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 1 (12.5) | 1 (12.5) | 1 (14.3) | 0 (0.0) | 0 (0.0) | |
| Current smoker | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 1 (100.0) |
References
- Landrigan, P.J.; Lioy, P.J.; Thurston, G.; Berkowitz, G.; Chen, L.C.; Chillrud, S.N.; Gavett, S.H.; Georgopoulos, P.G.; Geyh, A.S.; Levin, S.; et al. Health and environmental consequences of the world trade center disaster. Environ. Health Perspect. 2004, 112, 731–739. [Google Scholar] [CrossRef]
- Lippmann, M.; Cohen, M.D.; Chen, L.C. Health effects of World Trade Center (WTC) Dust: An unprecedented disaster’s inadequate risk management. Crit. Rev. Toxicol. 2015, 45, 492–530. [Google Scholar] [CrossRef]
- Reibman, J.; Levy-Carrick, N.; Miles, T.; Flynn, K.; Hughes, C.; Crane, M.; Lucchini, R.G. Destruction of the World Trade Center Towers. Lessons Learned from an Environmental Health Disaster. Ann. Am. Thorac. Soc. 2016, 13, 577–583. [Google Scholar] [CrossRef] [Green Version]
- Reibman, J.; Liu, M.; Cheng, Q.; Liautaud, S.; Rogers, L.; Lau, S.; Berger, K.; Goldring, R.; Marmor, M.; Fernandez-Beros, M.E.; et al. Characteristics of a Residential and Working Community with Diverse Exposure to World Trade Center Dust, Gas, and Fumes. J. Occup. Environ. Med. 2009, 51, 534–541. [Google Scholar] [CrossRef] [Green Version]
- Reibman, J.; Lin, S.; Hwang, S.A.A.; Gulati, M.; Bowers, J.A.; Rogers, L.; Berger, K.I.; Hoerning, A.; Gomez, M.; Fitzgerald, E.F. The World Trade Center Residents’ Respiratory Health Study: New-Onset Respiratory Symptoms and Pulmonary Function. Environ. Health Perspect. 2005, 113, 406–411. [Google Scholar] [CrossRef] [Green Version]
- Lin, S.; Reibman, J.; Bowers, J.A.; Hwang, S.-A.; Hoerning, A.; Gomez, M.I.; Fitzgerald, E.F. Upper Respiratory Symptoms and Other Health Effects among Residents Living Near the World Trade Center Site after September 11, 2001. Am. J. Epidemiology 2005, 162, 499–507. [Google Scholar] [CrossRef] [Green Version]
- Farfel, M.; DiGrande, L.; Brackbill, R.; Prann, A.; Cone, J.; Friedman, S.; Walker, D.J.; Pezeshki, G.; Thomas, P.; Galea, S.; et al. An Overview of 9/11 Experiences and Respiratory and Mental Health Conditions among World Trade Center Health Registry Enrollees. J. Urban Health 2008, 85, 880–909. [Google Scholar] [CrossRef] [Green Version]
- Thomas, P.A.; Brackbill, R.; Thalji, L.; DiGrande, L.; Campolucci, S.; Thorpe, L.; Henning, K. Respiratory and Other Health Effects Reported in Children Exposed to the World Trade Center Disaster of 11 September 2001. Environ. Health Perspect. 2008, 116, 1383–1390. [Google Scholar] [CrossRef]
- Newman, D.M. Disaster Response and Grassroots Environmental Advocacy: The Example of the World Trade Center Community Labor Coalition. New Solut. 2008, 18, 23–56. [Google Scholar] [CrossRef]
- Lioy, P.J.; Weisel, C.P.; Millette, J.R.; Eisenreich, S.J.; Vallero, D.A.; Offenberg, J.; Buckley, B.; Turpin, B.J.; Zhong, M.; Cohen, M.D.; et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ. Health Perspect. 2002, 110, 703–714. [Google Scholar] [CrossRef]
- Offenberg, J.H.; Eisenreich, S.J.; Gigliotti, C.L.; Chen, L.C.; Xiong, J.Q.; Quan, C.; Lou, X.; Zhong, M.; Gorczynski, J.; Yiin, L.-M.; et al. Persistent organic pollutants in dusts that settled indoors in lower Manhattan after 11 September 2001. J. Expo. Anal. Environ. Epidemiol. 2004, 14, 164–172. [Google Scholar] [CrossRef] [Green Version]
- Perlman, S.E.; Friedman, S.; Galea, S.; Nair, H.P.; Erős-Sarnyai, M.; Stellman, S.D.; Hon, J.; Greene, C.M. Short-term and medium-term health effects of 9/11. Lancet 2011, 378, 925–934. [Google Scholar] [CrossRef] [Green Version]
- Pleil, J.D.; Vette, A.F.; Johnson, B.A.; Rappaport, S.M. Air levels of carcinogenic polycyclic aromatic hydrocarbons after the World Trade Center disaster. Proc. Natl. Acad. Sci. USA 2004, 101, 11685–11688. [Google Scholar] [CrossRef] [Green Version]
- Daniels, R.D.; Kubale, T.L.; Yiin, J.H.; Dahm, M.M.; Hales, T.R.; Baris, D.; Zahm, S.H.; Beaumont, J.J.; Waters, K.M.; Pinkerton, L.E. Mortality and cancer incidence in a pooled cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup. Environ. Med. 2014, 71, 388–397. [Google Scholar] [CrossRef]
- Yu, D.; Berlin, J.A.; Penning, T.M.; Field, J. Reactive Oxygen Species Generated by PAH o-Quinones Cause Change-In-Function Mutations in p53. Chem. Res. Toxicol. 2002, 15, 832–842. [Google Scholar] [CrossRef]
- Kuan, P.-F.; Mi, Z.; Georgopoulos, P.; Hashim, D.; Luft, B.J.; Boffetta, P. Enhanced exposure assessment and genome-wide DNA methylation in World Trade Center disaster responders. Eur. J. Cancer Prev. 2019, 28, 225–233. [Google Scholar] [CrossRef]
- World Trade Center Health Program, 42 CFR Part 88. 2016. Available online: https://www.ecfr.gov/current/title-42/chapter-I/subchapter-G/part-88 (accessed on 11 August 2022).
- WTC Health Program. Regulations. Available online: https://www.cdc.gov/wtc/regulations2.html (accessed on 11 August 2022).
- Leeman, J.E.; McBride, S.M.; Spielsinger, D.; Sherman, E.J.; Wong, R.; Riaz, N.; Lee, N.Y.; Tsai, C.J. Head and neck cancers associated with exposure to the September 11, 2001 World Trade Center terrorist attacks. Int. J. Cancer 2018, 142, 2485–2490. [Google Scholar] [CrossRef]
- Zeig-Owens, R.; Webber, M.P.; Hall, C.B.; Schwartz, T.; Jaber, N.; Weakley, J.; Rohan, T.E.; Cohen, H.W.; Derman, O.; Aldrich, T.K.; et al. Early assessment of cancer outcomes in New York City firefighters after the 9/11 attacks: An observational cohort study. Lancet 2011, 378, 898–905. [Google Scholar] [CrossRef] [Green Version]
- Moline, J.M.; Herbert, R.; Crowley, L.; Troy, K.; Hodgman, E.; Shukla, G.; Udasin, I.; Luft, B.; Wallenstein, S.; Landrigan, P.; et al. Multiple Myeloma in World Trade Center Responders: A Case Series. J. Occup. Environ. Med. 2009, 51, 896–902. [Google Scholar] [CrossRef]
- Li, J.; Cone, J.E.; Kahn, A.R.; Brackbill, R.M.; Farfel, M.R.; Greene, C.M.; Hadler, J.L.; Stayner, L.T.; Stellman, S.D. Association Between World Trade Center Exposure and Excess Cancer Risk. JAMA 2012, 308, 2479–2488. [Google Scholar] [CrossRef]
- Li, J.; Brackbill, R.M.; Liao, T.S.; Qiao, B.; Cone, J.E.; Farfel, M.R.; Hadler, J.L.; Kahn, A.R.; Konty, K.J.; Stayner, L.T.; et al. Ten-year cancer incidence in rescue/recovery workers and civilians exposed to the September 11, 2001 terrorist attacks on the World Trade Center. Am. J. Ind. Med. 2016, 59, 709–721. [Google Scholar] [CrossRef]
- Li, J.; Yung, J.; Qiao, B.; Takemoto, E.; Goldfarb, D.G.; Zeig-Owens, R.; Cone, J.E.; Brackbill, R.M.; Farfel, M.R.; Kahn, A.R.; et al. Cancer Incidence in World Trade Center Rescue and Recovery Workers: 14 Years of Follow-Up. J. Natl. Cancer Inst. 2022, 114, 210–219. [Google Scholar] [CrossRef]
- Shapiro, M.Z.; Wallenstein, S.R.; Dasaro, C.R.; Lucchini, R.G.; Sacks, H.S.; Teitelbaum, S.L.; Thanik, E.S.; Crane, M.A.; Harrison, D.J.; Luft, B.J.; et al. Cancer in General Responders Participating in World Trade Center Health Programs, 2003–2013. JNCI Cancer Spectr. 2020, 4, pkz090. [Google Scholar] [CrossRef]
- Tuminello, S.; Van Gerwen, M.A.G.; Genden, E.; Crane, M.; Lieberman-Cribbin, W.; Taioli, E. Increased Incidence of Thyroid Cancer among World Trade Center First Responders: A Descriptive Epidemiological Assessment. Int. J. Environ. Res. Public Health 2019, 16, 1258. [Google Scholar] [CrossRef] [Green Version]
- Solan, S.; Wallenstein, S.; Shapiro, M.; Teitelbaum, S.L.; Stevenson, L.; Kochman, A.; Kaplan, J.; Dellenbaugh, C.; Kahn, A.; Biro, F.N.; et al. Cancer Incidence in World Trade Center Rescue and Recovery Workers, 2001–2008. Environ. Health Perspect. 2013, 121, 699–704. [Google Scholar] [CrossRef] [Green Version]
- Goldfarb, D.G.; Zeig-Owens, R.; Kristjansson, D.; Li, J.; Brackbill, R.M.; Farfel, M.R.; Cone, J.E.; Yung, J.; Kahn, A.R.; Qiao, B.; et al. Temporal association of prostate cancer incidence with World Trade Center rescue/recovery work. Occup. Environ. Med. 2021, 78, 699–706. [Google Scholar] [CrossRef]
- Durmus, N.; Shao, Y.; Arslan, A.A.; Zhang, Y.; Pehlivan, S.; Fernandez-Beros, M.E.; Umana, L.; Corona, R.; Smyth-Giambanco, S.; Abbott, S.A.; et al. Characteristics of Cancer Patients in the World Trade Center Environmental Health Center. Int. J. Environ. Res. Public Health 2020, 17, 7190. [Google Scholar] [CrossRef]
- Shao, Y.; Durmus, N.; Zhang, Y.; Pehlivan, S.; Fernandez-Beros, M.E.; Umana, L.; Corona, R.; Abbott, S.; Smyth-Giambanco, S.; Arslan, A.A.; et al. The Development of a WTC Environmental Health Center Pan-Cancer Database. Int. J. Environ. Res. Public Health 2021, 18, 1646. [Google Scholar] [CrossRef]
- Arslan, A.; Zhang, Y.; Durmus, N.; Pehlivan, S.; Addessi, A.; Schnabel, F.; Shao, Y.; Reibman, J. Breast Cancer Characteristics in the Population of Survivors Participating in the World Trade Center Environmental Health Center Program 2002–2019. Int. J. Environ. Res. Public Health 2021, 18, 7555. [Google Scholar] [CrossRef]
- Shum, E.; Durmus, N.; Pehlivan, S.; Lu, Y.; Zhang, Y.; Arslan, A.A.; Shao, Y.; Reibman, J. Characteristics of Women with Lung Adenocarcinoma in the World Trade Center Environmental Health Center. Int. J. Environ. Res. Public Health 2022, 19, 7618. [Google Scholar] [CrossRef]
- Koshy, T.T.; Attina, T.M.; Ghassabian, A.; Gilbert, J.; Burdine, L.K.; Marmor, M.; Honda, M.; Chu, D.B.; Han, X.; Shao, Y.; et al. Serum perfluoroalkyl substances and cardiometabolic consequences in adolescents exposed to the World Trade Center disaster and a matched comparison group. Environ. Int. 2017, 109, 128–135. [Google Scholar] [CrossRef]
- Goldfarb, D.G.; Colbeth, H.L.; Skerker, M.; Webber, M.P.; Prezant, D.J.; Dasaro, C.R.; Todd, A.C.; Kristjansson, D.; Li, J.; Brackbill, R.M.; et al. Impact of healthcare services on thyroid cancer incidence among World Trade Center-exposed rescue and recovery workers. Am. J. Ind. Med. 2021, 64, 861–872. [Google Scholar] [CrossRef]
- Trasande, L.; Koshy, T.T.; Gilbert, J.; Burdine, L.K.; Attina, T.M.; Ghassabian, A.; Honda, M.; Marmor, M.; Chu, D.B.; Han, X.; et al. Serum perfluoroalkyl substances in children exposed to the world trade center disaster. Environ. Res. 2017, 154, 212–221. [Google Scholar] [CrossRef] [Green Version]
- Trasande, L.; Fiorino, E.K.; Attina, T.; Berger, K.; Goldring, R.; Chemtob, C.; Levy-Carrick, N.; Shao, Y.; Liu, M.; Urbina, E.; et al. Associations of World Trade Center exposures with pulmonary and cardiometabolic outcomes among children seeking care for health concerns. Sci. Total Environ. 2013, 444, 320–326. [Google Scholar] [CrossRef] [Green Version]
- Trasande, L.; Koshy, T.T.; Gilbert, J.; Burdine, L.K.; Marmor, M.; Han, X.; Shao, Y.; Chemtob, C.; Attina, T.M.; Urbina, E.M. Cardiometabolic profiles of adolescents and young adults exposed to the World Trade Center Disaster. Environ. Res. 2018, 160, 107–114. [Google Scholar] [CrossRef]
- Hubal, E.A.C.; Sheldon, L.S.; Burke, J.M.; McCurdy, T.R.; Berry, M.R.; Rigas, M.L.; Zartarian, V.G.; Freeman, N.C. Children’s exposure assessment: A review of factors influencing Children’s exposure, and the data available to characterize and assess that exposure. Environ. Health Perspect. 2000, 108, 475–486. [Google Scholar] [CrossRef]
- Clarke, M.A.; Joshu, C.E. Early Life Exposures and Adult Cancer Risk. Epidemiol. Rev. 2017, 39, 11–27. [Google Scholar] [CrossRef] [Green Version]
- Paasivirta, M.E.; Duarte, C.S.; Wu, P.; Bin, F.; Goodman, R.F.; Brown, E.J.; Andrews, H.F.; Hoven, C.W. Factor structure of the Youth Coping In Traumatic Times (YCITT) scale. Psychiatry Res. 2010, 179, 357–362. [Google Scholar] [CrossRef]
- Duarte, C.S.; Wu, P.; Cheung, A.; Mandell, D.J.; Fan, B.; Wicks, J.; Musa, G.J.; Hoven, C. Media use by children and adolescents from New York City 6 months after the WTC attack. J. Trauma. Stress 2011, 24, 553–556. [Google Scholar] [CrossRef]
- Hoven, C.W.; Duarte, C.S.; Wu, P.; Doan, T.; Singh, N.; Mandell, N.J.; Bin, F.; Teichman, Y.; Teichman, M.; Wicks, J.; et al. Parental Exposure to Mass Violence and Child Mental Health: The First Responder and WTC Evacuee Study. Clin. Child Fam. Psychol. Rev. 2009, 12, 95–112. [Google Scholar] [CrossRef]
- Cancers Linked to Tobacco Use Make up 40% of all Cancers Diagnosed in the United States. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/media/releases/2016/p1110-vital-signs-cancer-tobacco.html (accessed on 10 November 2016).
- Obesity and Cancer. Centers for Disease Control and Prevention. Updated 13 July 2022. Available online: https://www.cdc.gov/cancer/obesity/index.htm (accessed on 8 September 2022).
- Singh, A.; Zeig-Owens, R.; Moir, W.; Hall, C.B.; Schwartz, T.; Vossbrinck, M.; Jaber, N.; Webber, M.P.; Kelly, K.J.; Ortiz, V.; et al. Estimation of Future Cancer Burden Among Rescue and Recovery Workers Exposed to the World Trade Center Disaster. JAMA Oncol. 2018, 4, 828–831. [Google Scholar] [CrossRef]
- Rana, I.; Dahlberg, S.; Steinmaus, C.; Zhang, L. Benzene exposure and non-Hodgkin lymphoma: A systematic review and meta-analysis of human studies. Lancet Planet. Health 2021, 5, e633–e643. [Google Scholar] [CrossRef]





| Level | Overall | Age at 9/11 0–10 | Age at 9/11 11–20 | Age at 9/11 21–30 | |
|---|---|---|---|---|---|
| n | 269 | 6 | 42 | 221 | |
| Age at 9/11, median [range] | 26 [0, 30] | 6 [0, 10] | 18 [12, 20] | 27 [21, 30] | |
| Gender, n (%) | Female | 172 (63.9) | 2 (33.3) | 27 (64.3) | 143 (64.7) |
| Male | 97 (36.1) | 4 (66.7) | 15 (35.7) | 78 (35.3) | |
| Race/Ethnicity, n (%) | NH-White | 106 (43.8) | 1 (33.3) | 11 (29.7) | 94 (46.5) |
| Hispanic | 52 (21.5) | 0 (0.0) | 13 (35.1) | 39 (19.3) | |
| Asian | 42 (17.4) | 1 (33.3) | 9 (24.3) | 32 (15.8) | |
| NH-Black | 38 (15.7) | 1 (33.3) | 4 (10.8) | 33 (16.3) | |
| Native American/Other | 4 (1.7) | 0 (0.0) | 0 (0.0) | 4 (2.0) | |
| BMI, n (%) | Normal weight (<25) | 62 (34.3) | 1 (100.0) | 12 (42.9) | 49 (32.2) |
| Overweight (25–30) | 61 (33.7) | 0 (0.0) | 10 (35.7) | 51 (33.6) | |
| Obese (≥30) | 58 (32.0) | 0 (0.0) | 6 (21.4) | 52 (34.2) | |
| Income, n (%) | ≤$30,000/year | 64 (26.7) | 0 (0.0) | 12 (30.8) | 52 (26.1) |
| >$30,000/year | 176 (73.3) | 2 (100.0) | 27 (69.2) | 147 (73.9) | |
| Education, n (%) | High school or less | 29 (11.2) | 2 (50.0) | 4 (9.8) | 23 (10.7) |
| More than high school | 231 (88.8) | 2 (50.0) | 37 (90.2) | 192 (89.3) | |
| Caught in WTC dust cloud, n (%) | No | 141 (54.2) | 3 (75.0) | 24 (58.5) | 114 (53.0) |
| Yes | 119 (45.8) | 1 (25.0) | 17 (41.5) | 101 (47.0) | |
| Exposure category, n (%) | Local worker | 141 (54.2) | 0 (0.0) | 6 (14.6) | 135 (62.8) |
| Resident | 52 (20.0) | 3 (75.0) | 9 (22.0) | 40 (18.6) | |
| Student | 49 (18.8) | 1 (25.0) | 23 (56.1) | 25 (11.6) | |
| Other | 18 (6.9) | 0 (0.0) | 3 (7.3) | 15 (7.0) | |
| Smoking history, n (%) | Never | 220 (86.6) | 4 (100.0) | 40 (97.6) | 176 (84.2) |
| Former smoker | 29 (11.4) | 0 (0.0) | 0 (0.0) | 29 (13.9) | |
| Current smoker | 5 (2.0) | 0 (0.0) | 1 (2.4) | 4 (1.9) | |
| Smoking pack-yr, n (%) | ≤5 pack-year | 234 (92.1) | 4 (100.0) | 40 (97.6) | 190 (90.9) |
| >5 pack-year | 20 (7.9) | 0 (0.0) | 1 (2.4) | 19 (9.1) |
| Level | Breast | Thyroid | Head and Neck Sites | Colon and Rectum | Kidney | Testis | Brain and Spinal Cord | Melanoma of the Skin | Soft Tissue Sarcoma | Lung | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 76 | 55 | 15 | 12 | 11 | 11 | 9 | 6 | 5 | 4 | |
| Age at 9/11, median [range] | 26 [14, 30] | 23 [1, 30] | 26 [16, 30] | 24 [16, 30] | 27 [0, 30] | 28 [20, 29] | 26 [21, 30] | 26 [21, 29] | 28 [22, 29] | 28 [25, 29] | |
| Age at diagnosis, median [range] | 40 [27, 48] | 35 [13, 46] | 37 [26, 46] | 38 [29, 44] | 40 [7, 46] | 40 [28, 43] | 38 [30, 46] | 34 [28, 45] | 39 [29, 47] | 39 [34, 45] | |
| Gender, n (%) | Female | 74 (97.4) | 42 (76.4) | 4 (26.7) | 6 (50.0) | 3 (27.3) | 0 (0.0) | 6 (66.7) | 4 (66.7) | 2 (40.0) | 3 (75.0) |
| Male | 2 (2.6) | 13 (23.6) | 11 (73.3) | 6 (50.0) | 8 (72.7) | 11 (100.0) | 3 (33.3) | 2 (33.3) | 3 (60.0) | 1 (25.0) | |
| Race/Ethnicity, n (%) | NH-White | 28 (36.8) | 20 (46.5) | 5 (33.3) | 7 (70.0) | 6 (60.0) | 6 (60.0) | 2 (28.6) | 4 (80.0) | 2 (40.0) | 3 (75.0) |
| Hispanic | 14 (18.4) | 9 (20.9) | 1 (6.7) | 2 (20.0) | 2 (20.0) | 3 (30.0) | 2 (28.6) | 1 (20.0) | 0 (0.0) | 1 (25.0) | |
| Asian | 15 (19.7) | 10 (23.3) | 4 (26.7) | 0 (0.0) | 1 (10.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (40.0) | 0 (0.0) | |
| NH-Black | 17 (22.4) | 4 (9.3) | 5 (33.3) | 1 (10.0) | 1 (10.0) | 1 (10.0) | 2 (28.6) | 0 (0.0) | 1 (20.0) | 0 (0.0) | |
| Native American/Other | 2 (2.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| BMI, n (%) | Normal weight (<25) | 21 (40.4) | 12 (36.4) | 5 (55.6) | 3 (42.9) | 3 (30.0) | 2 (20.0) | 0 (0.0) | 0 (0.0) | 1 (25.0) | 1 (25.0) |
| Overweight (25–30) | 10 (19.2) | 15 (45.5) | 1 (11.1) | 0 (0.0) | 3 (30.0) | 4 (40.0) | 1 (25.0) | 1 (33.3) | 2 (50.0) | 1 (25.0) | |
| Obese (≥30) | 21 (40.4) | 6 (18.2) | 3 (33.3) | 4 (57.1) | 4 (40.0) | 4 (40.0) | 3 (75.0) | 2 (66.7) | 1 (25.0) | 2 (50.0) | |
| Income, n (%) | ≤$30,000/year | 15 (21.1) | 15 (31.9) | 5 (35.7) | 2 (20.0) | 1 (10.0) | 3 (30.0) | 4 (50.0) | 0 (0.0) | 1 (25.0) | 1 (25.0) |
| >$30,000/year | 56 (78.9) | 32 (68.1) | 9 (64.3) | 8 (80.0) | 9 (90.0) | 7 (70.0) | 4 (50.0) | 5 (100.0) | 3 (75.0) | 3 (75.0) | |
| Caught in WTC dust cloud, n (%) | No | 43 (57.3) | 22 (42.3) | 8 (53.3) | 8 (72.7) | 5 (50.0) | 6 (60.0) | 4 (50.0) | 4 (66.7) | 2 (40.0) | 3 (75.0) |
| Yes | 32 (42.7) | 30 (57.7) | 7 (46.7) | 3 (27.3) | 5 (50.0) | 4 (40.0) | 4 (50.0) | 2 (33.3) | 3 (60.0) | 1 (25.0) | |
| Exposure category, n (%) | Local worker | 43 (57.3) | 22 (42.3) | 7 (46.7) | 4 (36.4) | 7 (70.0) | 5 (50.0) | 5 (62.5) | 3 (50.0) | 3 (60.0) | 3 (75.0) |
| Resident | 12 (16.0) | 8 (15.4) | 6 (40.0) | 3 (27.3) | 0 (0.0) | 2 (20.0) | 1 (12.5) | 2 (33.3) | 1 (20.0) | 0 (0.0) | |
| Student | 15 (20.0) | 17 (32.7) | 2 (13.3) | 2 (18.2) | 3 (30.0) | 2 (20.0) | 2 (25.0) | 1 (16.7) | 0 (0.0) | 1 (25.0) | |
| Other | 5 (6.7) | 5 (9.6) | 0 (0.0) | 2 (18.2) | 0 (0.0) | 1 (10.0) | 0 (0.0) | 0 (0.0) | 1 (20.0) | 0 (0.0) | |
| Smoking history, n (%) | Never | 66 (88.0) | 49 (96.1) | 11 (84.6) | 8 (80.0) | 8 (80.0) | 8 (80.0) | 6 (85.7) | 6 (100.0) | 5 (100.0) | 1 (25.0) |
| Former smoker | 9 (12.0) | 2 (3.9) | 2 (15.4) | 2 (20.0) | 2 (20.0) | 2 (20.0) | 1 (14.3) | 0 (0.0) | 0 (0.0) | 3 (75.0) | |
| Current smoker | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Level | Non-Hodgkin Lymphoma | Hodgkin Lymphoma | Multiple Myeloma | ALL | CML | AML | CLL | |
|---|---|---|---|---|---|---|---|---|
| n | 18 | 17 | 6 | 4 | 4 | 2 | 1 | |
| Age at 9/11, median [range] | 27 [15, 30] | 23 [8, 29] | 26 [16, 28] | 21 [3, 27] | 19 [17, 25] | 28 [27, 30] | 28 [28, 28] | |
| Age at diagnosis, median [range] | 39 [22, 43] | 34 [14, 43] | 39 [28, 47] | 29 [16, 45] | 34 [24, 39] | 33 [32, 34] | 38 [38, 38] | |
| Gender, n (%) | Female | 11 (61.1) | 8 (47.1) | 4 (66.7) | 1 (25.0) | 1 (25.0) | 1 (50.0) | 0 (0.0) |
| Male | 7 (38.9) | 9 (52.9) | 2 (33.3) | 3 (75.0) | 3 (75.0) | 1 (50.0) | 1 (100.0) | |
| Race/Ethnicity, n (%) | NH-White | 5 (35.7) | 6 (40.0) | 1 (16.7) | 0 (0.0) | 1 (25.0) | 1 (50.0) | 0 (0.0) |
| Hispanic | 5 (35.7) | 6 (40.0) | 2 (33.3) | 1 (33.3) | 0 (0.0) | 1 (50.0) | 0 (0.0) | |
| Asian | 2 (14.3) | 0 (0.0) | 0 (0.0) | 2 (66.7) | 3 (75.0) | 0 (0.0) | 1 (100.0) | |
| NH-Black | 2 (14.3) | 3 (20.0) | 2 (33.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Native American/Other | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| BMI, n (%) | Normal weight (<25) | 3 (20.0) | 5 (62.5) | 1 (50.0) | 2 (66.7) | 1 (50.0) | 1 (50.0) | 0 (0.0) |
| Overweight (25–30) | 9 (60.0) | 3 (37.5) | 1 (50.0) | 1 (33.3) | 0 (0.0) | 1 (50.0) | 1 (100.0) | |
| Obese (≥30) | 3 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | |
| Income, n (%) | ≤$30,000/year | 5 (33.3) | 2 (13.3) | 2 (40.0) | 2 (66.7) | 1 (25.0) | 0 (0.0) | 0 (0.0) |
| >$30,000/year | 10 (66.7) | 13 (86.7) | 3 (60.0) | 1 (33.3) | 3 (75.0) | 1 (100.0) | 1 (100.0) | |
| Caught in WTC dust cloud, n (%) | No | 12 (66.7) | 8 (50.0) | 3 (60.0) | 4 (100.0) | 3 (75.0) | 1 (50.0) | 1 (100.0) |
| Yes | 6 (33.3) | 8 (50.0) | 2 (40.0) | 0 (0.0) | 1 (25.0) | 1 (50.0) | 0 (0.0) | |
| Exposure category, n (%) | Local worker | 13 (72.2) | 9 (56.2) | 3 (60.0) | 1 (25.0) | 0 (0.0) | 1 (50.0) | 1 (100.0) |
| Resident | 2 (11.1) | 5 (31.2) | 0 (0.0) | 2 (50.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | |
| Student | 1 (5.6) | 2 (12.5) | 1 (20.0) | 1 (25.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | |
| Other | 2 (11.1) | 0 (0.0) | 1 (20.0) | 0 ( 0.0) | 0 (0.0) | 1 (50.0) | 0 (0.0) | |
| Smoking history, n (%) | Never | 16 (88.9) | 15 (93.8) | 4 (80.0) | 3 (75.0) | 3 (75.0) | 2 (100.0) | 1 (100.0) |
| Former smoker | 1 (5.6) | 1 (6.2) | 0 (0.0) | 1 (25.0) | 1 (25.0) | 0 (0.0) | 0 (0.0) | |
| Current smoker | 1 (5.6) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Florsheim, R.L.; Zhang, Q.; Durmus, N.; Zhang, Y.; Pehlivan, S.; Arslan, A.A.; Shao, Y.; Reibman, J. Characteristics of Cancers in Community Members Exposed to the World Trade Center Disaster at a Young Age. Int. J. Environ. Res. Public Health 2022, 19, 15163. https://doi.org/10.3390/ijerph192215163
Florsheim RL, Zhang Q, Durmus N, Zhang Y, Pehlivan S, Arslan AA, Shao Y, Reibman J. Characteristics of Cancers in Community Members Exposed to the World Trade Center Disaster at a Young Age. International Journal of Environmental Research and Public Health. 2022; 19(22):15163. https://doi.org/10.3390/ijerph192215163
Chicago/Turabian StyleFlorsheim, Rebecca Lynn, Qiao Zhang, Nedim Durmus, Yian Zhang, Sultan Pehlivan, Alan A. Arslan, Yongzhao Shao, and Joan Reibman. 2022. "Characteristics of Cancers in Community Members Exposed to the World Trade Center Disaster at a Young Age" International Journal of Environmental Research and Public Health 19, no. 22: 15163. https://doi.org/10.3390/ijerph192215163