Impact of Systemic Delays for Patient Access to Oncology Drugs on Clinical, Economic, and Quality of Life Outcomes in Canada: A Call to Action
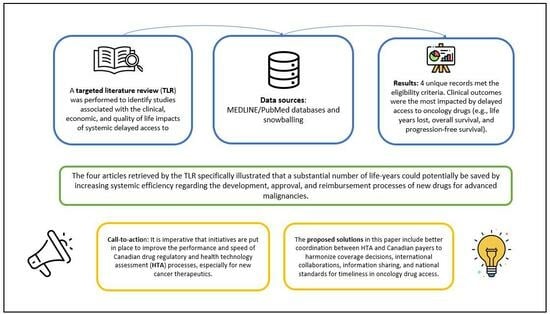
Abstract
:1. Introduction
2. Materials and Methods
3. Results
Search Results
4. Discussion
4.1. Call to Action
4.2. Potential Solutions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Canadian Cancer Society. Cancer Statistics at a Glance. Available online: https://cancer.ca/en/research/cancer-statistics/cancer-statistics-at-a-glance (accessed on 1 June 2023).
- Government of Canada. Patented Medicine Prices Review Board (PMPRB)—Compendium of Policies, Guidelines and Procedures—Updated February 2017; Government of Canada: Ottawa, ON, Canada, 2017.
- Institut National d’Excellence en Sante et en Services Sociaux (INESSS). Available online: https://www.inesss.qc.ca/ (accessed on 29 February 2024).
- Canadian Association of Drugs and Technologies in Health (CADTH). CADTH pan-Canadian Oncology Drug Review; Canadian Association of Drugs and Technologies in Health (CADTH): Toronto, ON, Canada, 2023. [Google Scholar]
- Pan-Canadian Pharmaceutical Alliance (pCPA). 2023. Available online: https://www.pcpacanada.ca/ (accessed on 1 December 2023).
- Jackson, E.B.; Hotte, S.J. Disparity in public funding of systemic therapy for metastatic renal cell carcinoma in Canada. Can. Urol. Assoc. J. 2022, 16, E516–E522. [Google Scholar] [CrossRef]
- MacPhail, C.; Snow, S. Not All Canadian Cancer Patients Are Equal-Disparities in Public Cancer Drug Funding across Canada. Curr. Oncol. 2022, 29, 2064–2072. [Google Scholar] [CrossRef] [PubMed]
- Woon, D.T.S.; Chandrasekar, T.; Aaron, L.; Basappa, N.S.; Chi, K.N.; Conter, H.J.; Gotto, G.; Hotte, S.J.; Malone, S.; Saad, F.; et al. Disparity in public funding of therapies for metastatic castrate-resistant prostate cancer across Canadian provinces. Can. Urol. Assoc. J. 2018, 12, 328–336. [Google Scholar] [CrossRef]
- Hanna, T.P.; King, W.D.; Thibodeau, S.; Jalink, M.; Paulin, G.A.; Harvey-Jones, E.; O’Sullivan, D.E.; Booth, C.M.; Sullivan, R.; Aggarwal, A. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ 2020, 371, m4087. [Google Scholar] [CrossRef] [PubMed]
- Schoonbeek, R.C.; Festen, S.; van der Laan, B.; Plaat, B.E.C.; Langendijk, J.A.; van Dijk, B.A.C.; Halmos, G.B. The effect of delayed primary treatment initiation on adverse events and recurrence in older head and neck cancer patients. Radiother. Oncol. 2022, 173, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Hoskyn, S.L. Patient Access to New Medicines in Canada: An International Comparison of Launch and Public Reimbursement Performance. 2019. Available online: https://innovativemedicines.ca/wp-content/uploads/2019/04/2019-CADTH-Poster-EN.pdf (accessed on 1 February 2023).
- Bartol, A.; Dressler, K.; Kaskel, P.; Landsberg, C.; Lechner, C.; Petschulies, M. Ten years of AMNOG from an oncological perspective: New horizons and continuing expansion. J. Cancer Res. Clin. Oncol. 2022, 149, 2637–2645. [Google Scholar] [CrossRef]
- Stewart, D.J.; Stewart, A.A.; Wheatley-Price, P.; Batist, G.; Kantarjian, H.M.; Schiller, J.; Clemons, M.; Bradford, J.P.; Gillespie, L.; Kurzrock, R. The importance of greater speed in drug development for advanced malignancies. Cancer Med. 2018, 7, 1824–1836. [Google Scholar] [CrossRef] [PubMed]
- Gotfrit, J.; Shin, J.J.W.; Mallick, R.; Stewart, D.J.; Wheatley-Price, P. Potential Life-Years Lost: The Impact of the Cancer Drug Regulatory and Funding Process in Canada. Oncologist 2020, 25, e130–e137. [Google Scholar] [CrossRef] [PubMed]
- Uyl-de Groot, C.A.; Heine, R.; Krol, M.; Verweij, J. Unequal Access to Newly Registered Cancer Drugs Leads to Potential Loss of Life-Years in Europe. Cancers 2020, 12, 2313. [Google Scholar] [CrossRef] [PubMed]
- Vanderpuye-Orgle, J.; Erim, D.; Qian, Y.; Boyne, D.J.; Cheung, W.Y.; Bebb, G.; Shah, A.; Pericleous, L.; Maruszczak, M.; Brenner, D.R. Estimating the Impact of Delayed Access to Oncology Drugs on Patient Outcomes in Canada. Oncol. Ther. 2022, 10, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Salek, S.; Lussier Hoskyn, S.; Johns, J.R.; Allen, N.; Sehgal, C. Factors Influencing Delays in Patient Access to New Medicines in Canada: A Retrospective Study of Reimbursement Processes in Public Drug Plans. Front. Pharmacol. 2019, 10, 196. [Google Scholar] [CrossRef] [PubMed]
- Millson, B. Access to New Medicines in Public Drug Plans: Canada and Comparable Countries. 2016. Available online: https://innovativemedicines.ca/wp-content/uploads/2016/05/20160524_Access_to_Medicines_Report_EN_Web.pdf (accessed on 1 December 2023).
- Gotfrit, J.; Dempster, W.; Chambers, J.; Wheatley-Price, P. The Pathway for New Cancer Drug Access in Canada. Curr. Oncol. 2022, 29, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Gotfrit, J.; Jackson, A.; Shin, J.J.W.; Stewart, D.J.; Mallick, R.; Wheatley-Price, P. Determinants of the Cancer Drug Funding Process in Canada. Curr. Oncol. 2022, 29, 1997–2007. [Google Scholar] [CrossRef]
- de Claro, R.A.; Spillman, D.; Hotaki, L.T.; Shum, M.; Mouawad, L.S.; Santos, G.M.L.; Robinson, K.; Hunt, M.; Healy, C.; Chan, A.; et al. Project Orbis: Global Collaborative Review Program. Clin. Cancer Res. 2020, 26, 6412–6416. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Project Orbis. Available online: https://www.canada.ca/en/health-canada/services/drugs-health-products/international-activities/project-orbis.html (accessed on 1 February 2023).
- Hwang, T.J.; Kesselheim, A.S.; Tibau, A.; Lee, C.C.; Vokinger, K.N. Clinical Benefit and Expedited Approval of Cancer Drugs in the United States, European Union, Switzerland, Japan, Canada, and Australia. JCO Oncol. Pract. 2022, 18, e1522–e1532. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. The Government of Canada Announces the Creation of the Canadian Drug Agency. Available online: https://www.canada.ca/en/health-canada/news/2023/12/the-government-of-canada-announces-the-creation-of-the-canadian-drug-agency---helping-make-canadas-drug-system-more-sustainable-and-better-prepared.html (accessed on 2 December 2023).
- Bussgen, M.; Stargardt, T. Does health technology assessment compromise access to pharmaceuticals? Eur. J. Health Econ. 2023, 24, 1245–1248. [Google Scholar] [CrossRef] [PubMed]
- Julian, E.; Gianfrate, F.; Sola-Morales, O.; Mol, P.; Bergmann, J.F.; Salmonson, T.; Hebborn, A.; Grande, M.; Ruof, J. How can a joint European health technology assessment provide an ‘additional benefit’ over the current standard of national assessments?: Insights generated from a multi-stakeholder survey in hematology/oncology. Health Econ. Rev. 2022, 12, 30. [Google Scholar] [CrossRef] [PubMed]
- Beneluxa. The Beneluxa Initiative. Available online: https://beneluxa.org/ (accessed on 1 February 2023).
- O’Mahony, J.F. Beneluxa: What are the Prospects for Collective Bargaining on Pharmaceutical Prices Given Diverse Health Technology Assessment Processes? PharmacoEconomics 2019, 37, 627–630. [Google Scholar] [CrossRef] [PubMed]
- Medicines Australia. Reforming Australia’s Health Technology Assessment (HTA) System; Medicines Australia: Deakin, ACT, Australia, 2022. [Google Scholar]
- Pham, F.Y.; Jacquet, E.; Taleb, A.; Monard, A.; Kerouani-Lafaye, G.; Turcry, F.; Brunel, L.; Grude, F.; Yoldjian, I.; Sainte-Marie, I.; et al. Survival, cost and added therapeutic benefit of drugs granted early access through the French temporary authorization for use program in solid tumors from 2009 to 2019. Int. J. Cancer 2022, 151, 1345–1354. [Google Scholar] [CrossRef] [PubMed]
- European Pharmaceutical Review. France’s ATU Reform: Early Access Remains Possible, but Not All Diseases Are Equal; European Pharmaceutical Review: Kent, UK, 2022. [Google Scholar]
- Skinner, B. New cancer drugs in Canada 2012 to 2021: An economic analysis of cost, benefit, availability, and public insurance coverage. Can. Health Policy 2023. Available online: https://www.canadianhealthpolicy.com/product/new-cancer-drugs-in-canada-2012-to-2021-an-economic-analysis-of-cost-benefit-availability-and-public-insurance-coverage/ (accessed on 1 February 2023).
- Canada’s Drug and Health Technology Agency. CADTH Consultation: Proposed Process for Time-Limited Reimbursement Recommendations—March 2023; Canada’s Drug and Health Technology Agency: Ottawa, ON, Canada, 2023; Available online: https://www.cadth.ca/news/consultation-time-limited-reimbursement-recommendations (accessed on 15 December 2023).
- Sutherland, G. Understanding the Gap. A Pan-Canadian Analysis of Prescription Drug Insurance Coverage. 2017. Available online: http://innovativemedicines.ca/wp-content/uploads/2017/12/20170712-understanding-the-gap.pdf (accessed on 1 February 2023).

| First Author, Year, Location | Objective | Study Design | Type(s) of Cancer | Types of Treatment | Outcomes Reported |
|---|---|---|---|---|---|
| Gotfrit, 2020 [14], Canada | To quantify the potential life years lost during Health Canada drug approval and funding process | Public data analysis | Lung, breast, and colorectal cancers | Drugs submitted to pCODR | OS, PFS, life years lost |
| Stewart, 2018 [13], Canada | To calculate life years potentially saved if selected agents were approved more rapidly | Public data analysis | Advanced malignancies | New therapies for metastatic cancers | Life years saved |
| Uyl-de Groot, 2020 [15], Europe | To assess the access in Europe to newly registered cancer drugs and to obtain more insight in the implications of these variations for patients | Retrospective database study | Breast cancer, gastric cancer, prostate cancer, and melanoma | Chemotherapy and targeted therapy | Life years lost |
| Vanderpuye-Orgle, 2022, Global [16] | To better understand the impact of any additional delays on NSCLC patients | Analysis of literature and empirical modelling | NSCLC | Chemotherapy, drugs for NSCLC | Health care costs, QALY |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sehdev, S.; Gotfrit, J.; Elias, M.; Stein, B.D. Impact of Systemic Delays for Patient Access to Oncology Drugs on Clinical, Economic, and Quality of Life Outcomes in Canada: A Call to Action. Curr. Oncol. 2024, 31, 1460-1469. https://doi.org/10.3390/curroncol31030110
Sehdev S, Gotfrit J, Elias M, Stein BD. Impact of Systemic Delays for Patient Access to Oncology Drugs on Clinical, Economic, and Quality of Life Outcomes in Canada: A Call to Action. Current Oncology. 2024; 31(3):1460-1469. https://doi.org/10.3390/curroncol31030110
Chicago/Turabian StyleSehdev, Sandeep, Joanna Gotfrit, Martine Elias, and Barry D. Stein. 2024. "Impact of Systemic Delays for Patient Access to Oncology Drugs on Clinical, Economic, and Quality of Life Outcomes in Canada: A Call to Action" Current Oncology 31, no. 3: 1460-1469. https://doi.org/10.3390/curroncol31030110