Heat-Polymerized Resin Containing Dimethylaminododecyl Methacrylate Inhibits Candida albicans Biofilm
Abstract
:1. Introduction
2. Materials and Methods
2.1. Synthesis of Antibacterial Monomer
2.2. Specimen Fabrication
- DMADDM was added to heat-polymerizable liquid blending to a certain mass fraction (5%, 10%, and 20%).
- Untreated heat-polymerizable liquid was mixed with untreated powder, reacting until the paste stage.
- Treated heat-polymerizable liquid was mixed with untreated powder, reacting until the paste stage.
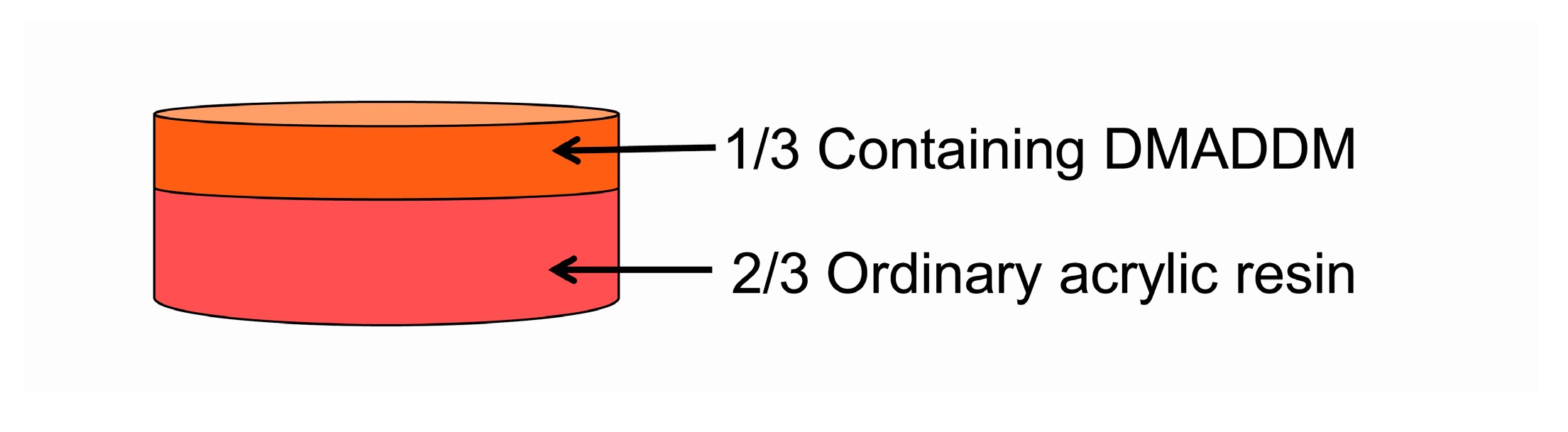
- One-third treated acrylic resin and two-thirds untreated acrylic resin in the lower, were placed into the upper and lower portions of cavity die box, respectively, and filled with gypsum at the same time (Figure 1). Pressure was used for polymerization by tightening bolts on the cavity die box and excess material was removed.
- The box was put into an incubator, reacting at 72 °C for 90 min and then at 100 °C for 60 min.
- Once the die box cooled down, acrylic resin was taken out and cut into certain size specimens (11 × 11 × 3 mm3) by a diamond-coated band saw (Struers Minitom).
- In turn, treated acrylic resin surface was polished with different particle of standard metallographic sandpaper (P400, P800, P1000, P1500, P2000, P2400, and P4000) (Struers Minitom).
2.3. Mechanical Testing
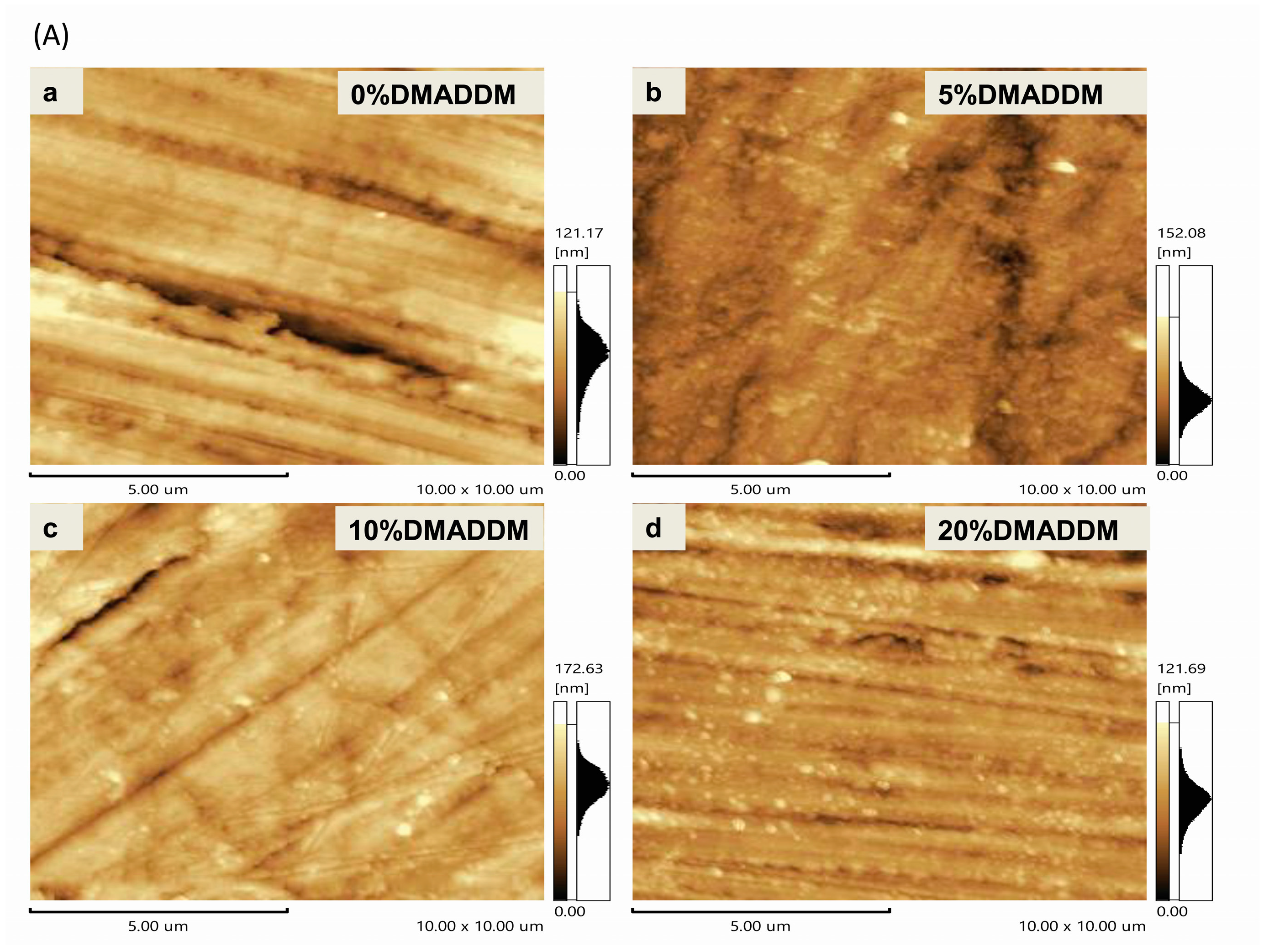
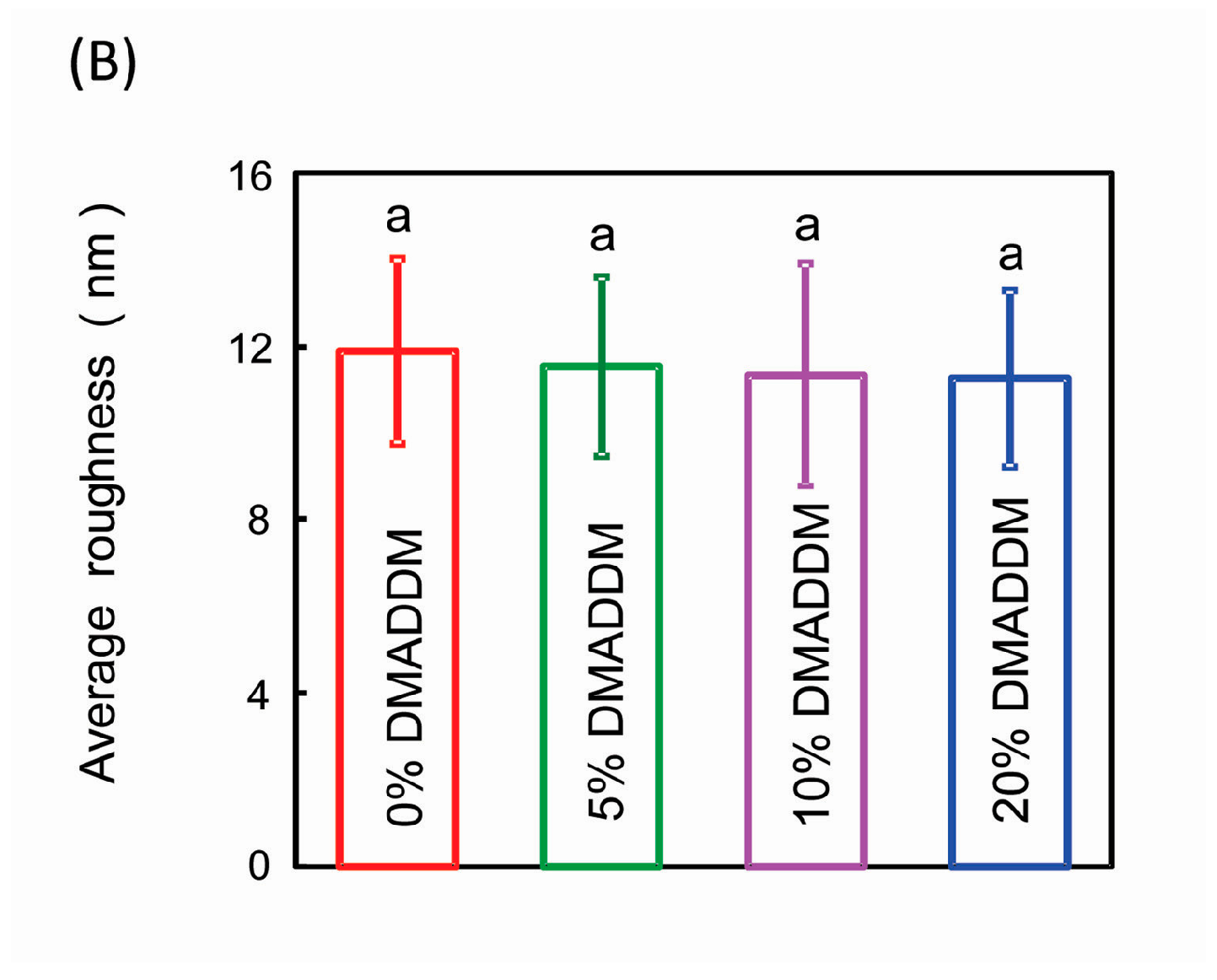
2.4. Surface Roughness Observation
2.5. Charge Density Testing
2.6. Biofilm Formation Assay
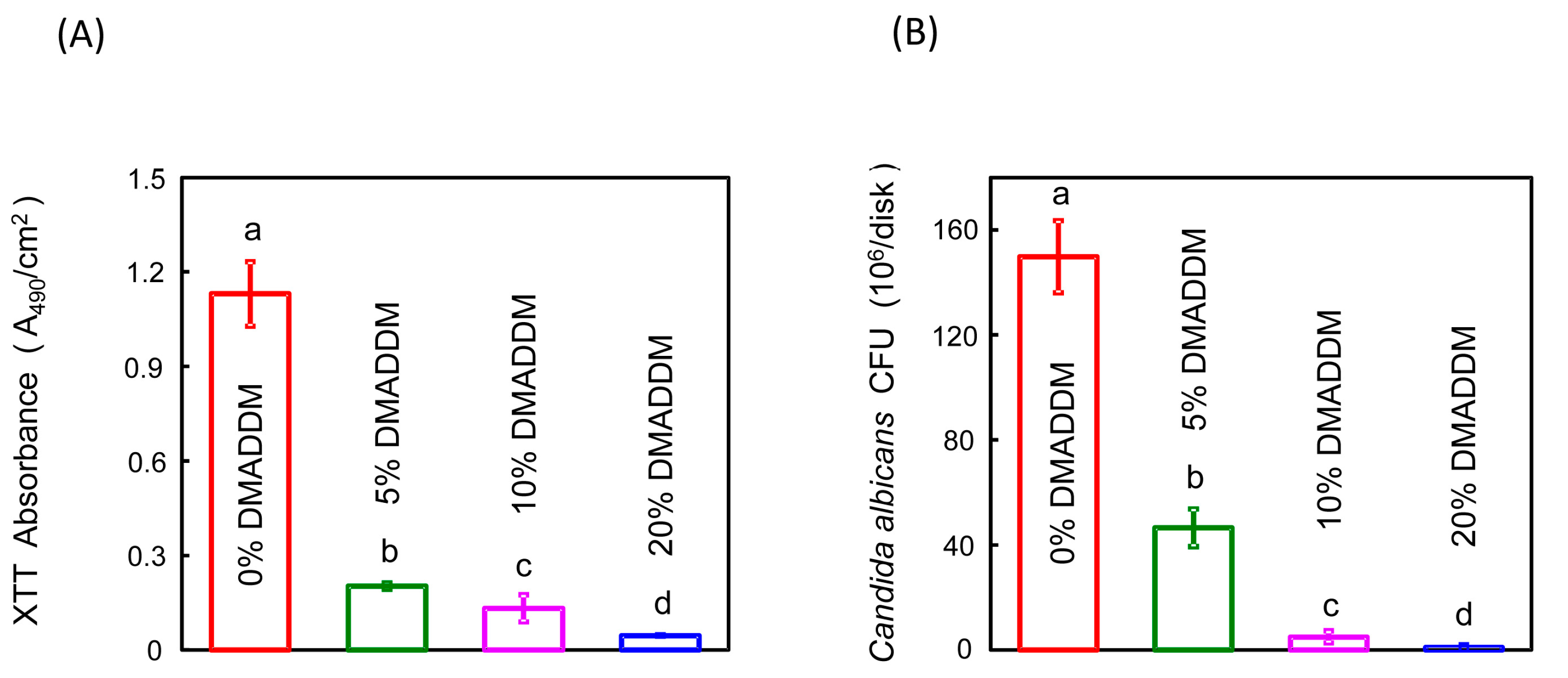
2.7. C. albicans Biofilm Metabolic Activity and Biomass Assay
2.8. Biomass Calculation
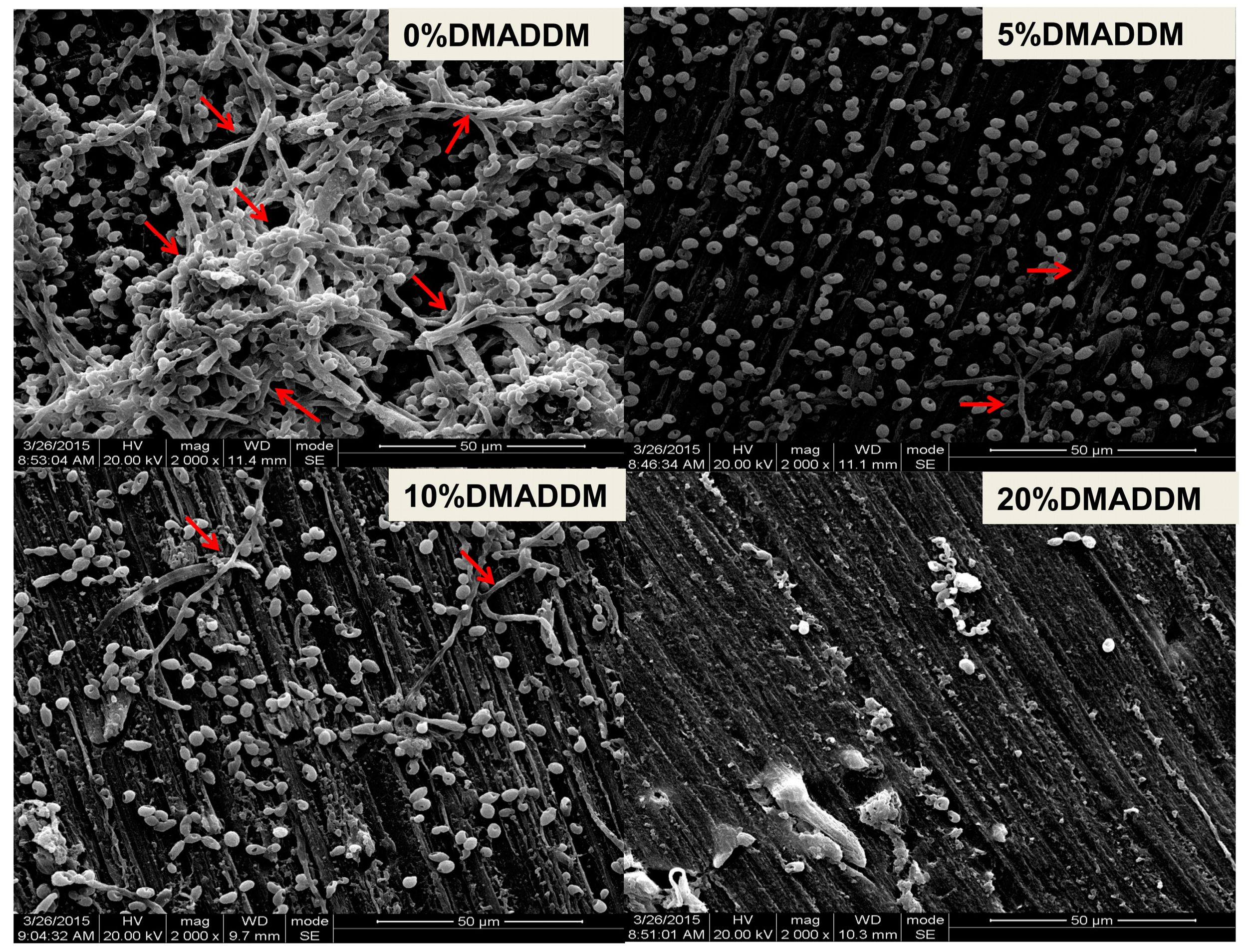
2.9. Observation of Biofilm Structure
2.10. Statistical Analysis
3. Results
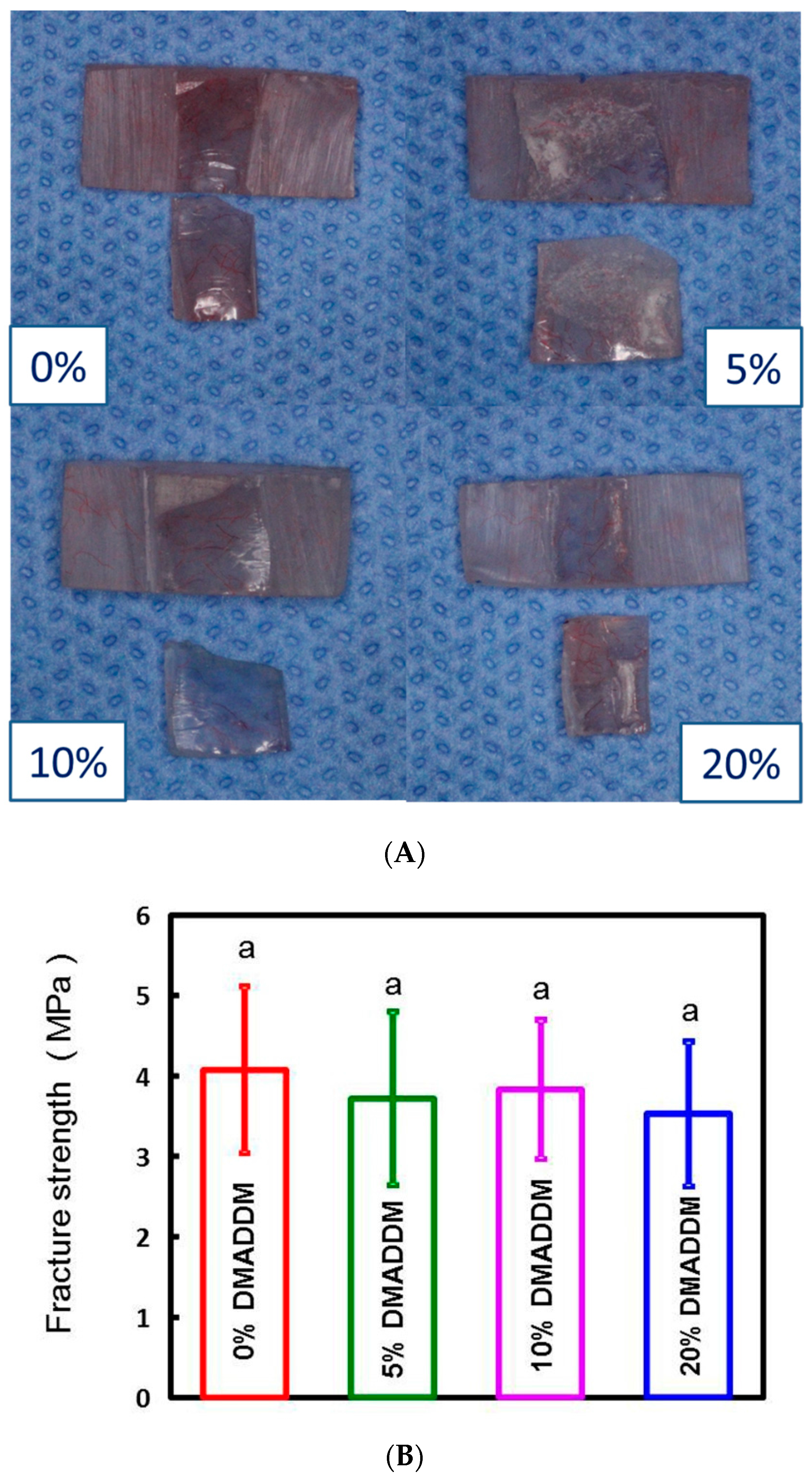
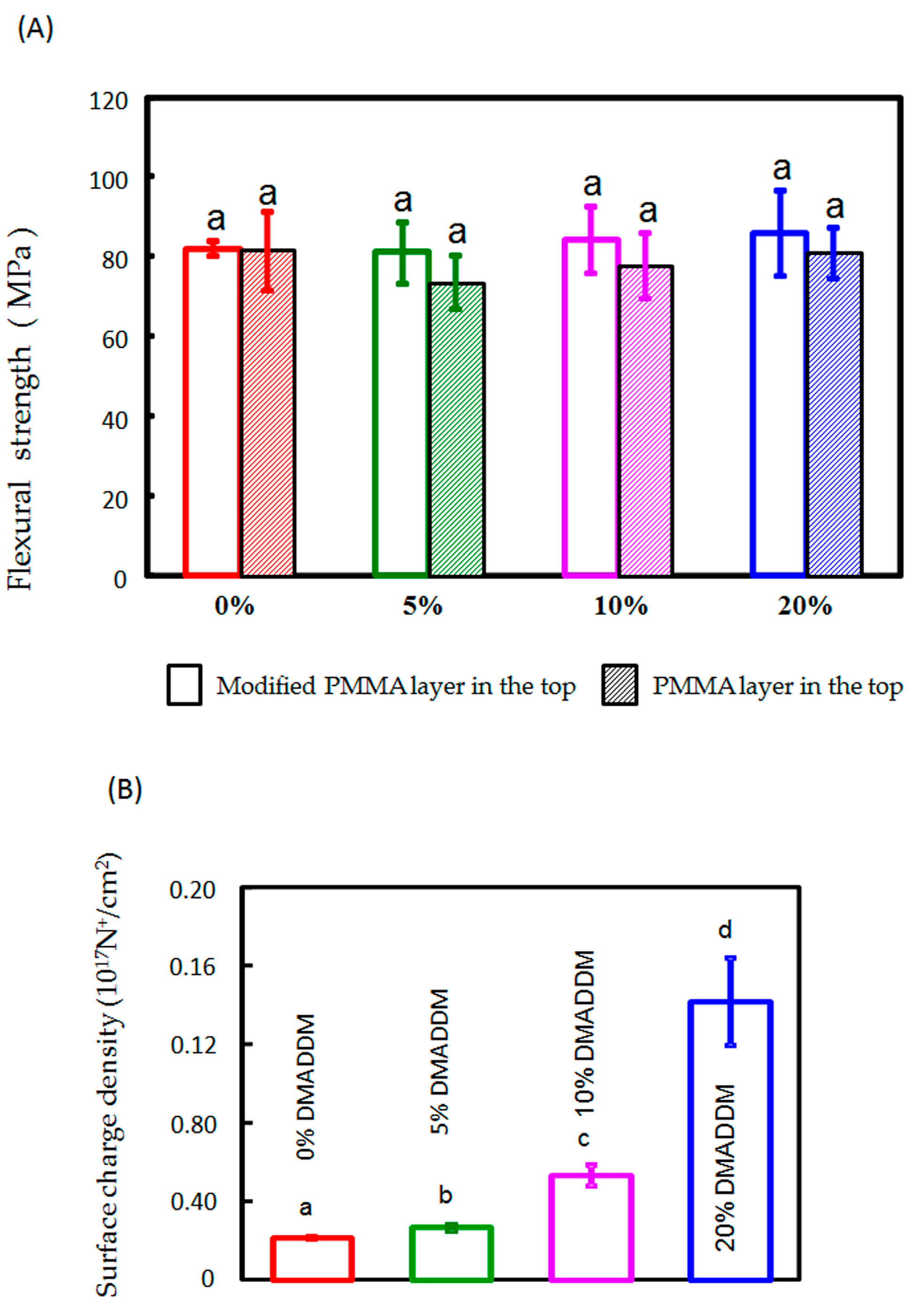
3.1. Physical Performance of Double-Decked Acrylic Resin
3.2. The Antifungal Properties of Double-Decked Acrylic Resin
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Arendorf, T.M.; Walker, D.M. Denture stomatitis: A review. J. Oral Rehabil. 1987, 14, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Altarawneh, S.; Bencharit, S.; Mendoza, L.; Curran, A.; Barrow, D.; Barros, S.; Preisser, J.; Loewy, Z.G.; Gendreau, L.; Offenbacher, S. Clinical and histological findings of denture stomatitis as related to intraoral colonization patterns of Candida albicans, salivary flow, and dry mouth. J. Prosthodont. 2013, 22, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Emami, E.; Taraf, H.; de Grandmont, P.; Gauthier, G.; de Koninck, L.; Lamarche, C.; de Souza, R.F. The association of denture stomatitis and partial removable dental prostheses: A systematic review. Int. J. Prosthodont. 2012, 25, 113–119. [Google Scholar] [PubMed]
- Vanden Abbeele, A.; de Meel, H.; Ahariz, M.; Perraudin, J.P.; Beyer, I.; Courtois, P. Denture contamination by yeasts in the elderly. Gerodontology 2008, 25, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Ramage, G.; Tomsett, K.; Wickes, B.L.; Lopez-Ribot, J.L.; Redding, S.W. Denture stomatitis: A role for Candida biofilms. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodont. 2004, 98, 53–59. [Google Scholar] [CrossRef]
- Pan, H.; Wang, G.; Pan, J.; Ye, G.; Sun, K.; Zhang, J.; Wang, J. Cold plasma-induced surface modification of heat-polymerized acrylic resin and prevention of early adherence of Candida albicans. Dent. Mater. J. 2015, 34, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Cross, L.J.; Williams, D.W.; Sweeney, C.P.; Jackson, M.S.; Lewis, M.A.; Bagg, J. Evaluation of the recurrence of denture stomatitis and Candida colonization in a small group of patients who received itraconazole. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodont. 2004, 97, 351–358. [Google Scholar] [CrossRef]
- Nawasrah, A.; AlNimr, A.; Ali, A.A. Antifungal effect of Henna against Candida albicans adhered to acrylic resin as a possible method for prevention of denture stomatitis. Int. J. Environ. Res. Public Health 2016, 13. [Google Scholar] [CrossRef] [PubMed]
- Cuellar-Cruz, M.; Vega-Gonzalez, A.; Mendoza-Novelo, B.; Lopez-Romero, E.; Ruiz-Baca, E.; Quintanar-Escorza, M.A.; Villagomez-Castro, J.C. The effect of biomaterials and antifungals on biofilm formation by Candida species: A review. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 2513–2527. [Google Scholar] [CrossRef] [PubMed]
- Oblak, E.; Piecuch, A.; Krasowska, A.; Luczynski, J. Antifungal activity of gemini quaternary ammonium salts. Microbiol. Res. 2013, 168, 630–638. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, Y.W.; Morse, D.J.; da Silva, W.J.; Del-Bel-Cury, A.A.; Wei, X.; Wilson, M.; Milward, P.; Lewis, M.; Bradshaw, D.; Williams, D.W. Virulence and pathogenicity of Candida albicans is enhanced in biofilms containing oral bacteria. Biofouling 2015, 31, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Alavarce, R.A.; Saldanha, L.L.; Almeida, N.L.; Porto, V.C.; Dokkedal, A.L.; Lara, V.S. The beneficial effect of Equisetum giganteum L. Against Candida biofilm formation: New approaches to denture stomatitis. Evid.-Based Complement. Altern. Med. 2015, 2015, 939625. [Google Scholar] [CrossRef] [PubMed]
- Antunes, D.P.; Salvia, A.C.; de Araujo, R.M.; di Nicolo, R.; Koga Ito, C.Y.; de Araujo, M.A. Effect of green tea extract and mouthwash without alcohol on Candida albicans biofilm on acrylic resin. Gerodontology 2015, 32, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Acosta-Torres, L.S.; Mendieta, I.; Nunez-Anita, R.E.; Cajero-Juarez, M.; Castano, V.M. Cytocompatible antifungal acrylic resin containing silver nanoparticles for dentures. Int. J. Nanomed. 2012, 7, 4777–4786. [Google Scholar]
- Chatzimoschou, A.; Simitsopoulou, M.; Antachopoulos, C.; Walsh, T.J.; Roilides, E. Differential effects of antifungal agents on expression of genes related to formation of Candida albicans biofilms. Mycoses 2016, 59, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Dalwai, S.; Rodrigues, S.J.; Baliga, S.; Shenoy, V.K.; Shetty, T.B.; Pai, U.Y.; Saldanha, S. Comparative evaluation of antifungal action of tea tree oil, chlorhexidine gluconate and fluconazole on heat polymerized acrylic denture base resin—An in vitro study. Gerodontology 2016, 33, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Sun, J.; Lan, J.; Qi, Q. Effect of a denture base acrylic resin containing silver nanoparticles on Candida albicans adhesion and biofilm formation. Gerodontology 2016, 33, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Weir, M.D.; Xu, H.H.; Antonucci, J.M.; Kraigsley, A.M.; Lin, N.J.; Lin-Gibson, S.; Zhou, X. Antibacterial amorphous calcium phosphate nanocomposites with a quaternary ammonium dimethacrylate and silver nanoparticles. Dent. Mater. 2012, 28, 561–572. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.J.; Zeiger, D.N.; Howarter, J.A.; Zhang, X.; Lin, N.J.; Antonucci, J.M.; Lin-Gibson, S. In situ formation of silver nanoparticles in photocrosslinking polymers. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011, 97, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Kasraei, S.; Sami, L.; Hendi, S.; Alikhani, M.Y.; Rezaei-Soufi, L.; Khamverdi, Z. Antibacterial properties of composite resins incorporating silver and zinc oxide nanoparticles on streptococcus mutans and lactobacillus. Restor. Dent. Endodont. 2014, 39, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Shtyrlin, N.V.; Sapozhnikov, S.V.; Koshkin, S.A.; Iksanova, A.G.; Sabirov, A.H.; Kayumov, A.R.; Nureeva, A.A.; Zeldi, M.I.; Shtyrlin, Y.G. Synthesis and antibacterial activity of novel quaternary ammonium pyridoxine derivatives. Med. Chem. 2015, 11, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Sekhavat Pour, Z.; Makvandi, P.; Ghaemy, M. Performance properties and antibacterial activity of crosslinked films of quaternary ammonium modified starch and poly(vinyl alcohol). Int. J. Biol. Macromol. 2015, 80, 596–604. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Soderling, E.; Lassila, L.V.; Vallittu, P.K. Preparation of antibacterial and radio-opaque dental resin with new polymerizable quaternary ammonium monomer. Dent. Mater. 2015, 31, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Carta, G.; Cagetti, M.G.; Cocco, F.; Sale, S.; Lingstrom, P.; Campus, G. Caries-risk profiles in Italian adults using computer caries assessment system and icdas. Braz. Oral Res. 2015, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.P.; Ge, Y.; Zhou, X.D.; Xu, H.H.; Weir, M.D.; Zhang, K.K.; Wang, H.H.; Hannig, M.; Rupf, S.; Li, Q.; et al. Effect of anti-biofilm glass-ionomer cement on streptococcus mutans biofilms. Int. J. Oral Sci. 2016, 8, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, K.; Zhou, X.; Xu, N.; Xu, H.H.; Weir, M.D.; Ge, Y.; Wang, S.; Li, M.; Li, Y.; et al. Antibacterial effect of dental adhesive containing dimethylaminododecyl methacrylate on the development of streptococcus mutans biofilm. Int. J. Mol. Sci. 2014, 15, 12791–12806. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Weir, M.D.; Zhang, K.; Arola, D.D.; Zhou, X.; Xu, H.H. Dental primer and adhesive containing a new antibacterial quaternary ammonium monomer dimethylaminododecyl methacrylate. J. Dent. 2013, 41, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Cheng, L.; Zhou, X.; Xu, H.H.; Weir, M.D.; Meyer, M.; Maurer, H.; Li, Q.; Hannig, M.; Rupf, S. In situ antibiofilm effect of glass-ionomer cement containing dimethylaminododecyl methacrylate. Dent. Mater. 2015, 31, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S.; Imai, T.; Russell, R.R.; Torii, M.; Ebisu, S. Antibacterial activity of cured dental resin incorporating the antibacterial monomer mdpb and an adhesion-promoting monomer. J. Biomed. Mater. Res. 1998, 39, 511–515. [Google Scholar] [CrossRef]
- Imazato, S.; Kinomoto, Y.; Tarumi, H.; Ebisu, S.; Tay, F.R. Antibacterial activity and bonding characteristics of an adhesive resin containing antibacterial monomer mdpb. Dent. Mater. 2003, 19, 313–319. [Google Scholar] [CrossRef]
- Zanini, S.; Polissi, A.; Maccagni, E.A.; Dell’Orto, E.C.; Liberatore, C.; Riccardi, C. Development of antibacterial quaternary ammonium silane coatings on polyurethane catheters. J. Colloid Interface Sci. 2015, 451, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Pesci-Bardon, C.; Fosse, T.; Madinier, I.; Serre, D. In vitro new dialysis protocol to assay the antiseptic properties of a quaternary ammonium compound polymerized with denture acrylic resin. Lett. Appl. Microbiol. 2004, 39, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Zhong, Z.; Lin, L. Evaluation of chitosan quaternary ammonium salt-modified resin denture base material. Int. J. Biol. Macromol. 2015, 85, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Weir, M.D.; Fouad, A.F.; Xu, H.H. Effect of salivary pellicle on antibacterial activity of novel antibacterial dental adhesives using a dental plaque microcosm biofilm model. Dent. Mater. 2014, 30, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Kubochi, K.; Komine, F.; Fushiki, R.; Yagawa, S.; Mori, S.; Matsumura, H. Shear bond strength of a denture base acrylic resin and gingiva-colored indirect composite material to zirconia ceramics. J. Prosthodont. Res. 2016. [Google Scholar] [CrossRef] [PubMed]
- Nahas, P.; Zeinoun, T.; Majzoub, Z.; Corbani, K.; Nammour, S. The effect of energy densities on the shear bond strength of self-adhering flowable composite to er:Yag pretreated dentin. BioMed Res. Int. 2016, 2016, 6507924. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Cheng, L.; Imazato, S.; Antonucci, J.M.; Lin, N.J.; Lin-Gibson, S.; Bai, Y.; Xu, H.H. Effects of dual antibacterial agents mdpb and nano-silver in primer on microcosm biofilm, cytotoxicity and dentine bond properties. J. Dent. 2013, 41, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Cheng, L.; Wu, E.J.; Weir, M.D.; Bai, Y.; Xu, H.H. Effect of water-ageing on dentine bond strength and anti-biofilm activity of bonding agent containing new monomer dimethylaminododecyl methacrylate. J. Dent. 2013, 41, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Weir, M.D.; Chen, J.; Xu, H.H. Effect of charge density of bonding agent containing a new quaternary ammonium methacrylate on antibacterial and bonding properties. Dent. Mater. 2014, 30, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, C.; Takakuda, K.; Wakabayashi, N. Reduction of Candida biofilm adhesion by incorporation of prereacted glass ionomer filler in denture base resin. J. Dent. 2016, 44, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Ramage, G.; Jose, A.; Coco, B.; Rajendran, R.; Rautemaa, R.; Murray, C.; Lappin, D.F.; Bagg, J. Commercial mouthwashes are more effective than azole antifungals against Candida albicans biofilms in vitro. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodont. 2011, 111, 456–460. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Weir, M.D.; Limkangwalmongkol, P.; Hack, G.D.; Xu, H.H.; Chen, Q.; Zhou, X. Tetracalcium phosphate composite containing quaternary ammonium dimethacrylate with antibacterial properties. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Arai, T.; Ueda, T.; Sugiyama, T.; Sakurai, K. Inhibiting microbial adhesion to denture base acrylic resin by titanium dioxide coating. J. Oral Rehabil. 2009, 36, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Lazarin, A.A.; Machado, A.L.; Zamperini, C.A.; Wady, A.F.; Spolidorio, D.M.; Vergani, C.E. Effect of experimental photopolymerized coatings on the hydrophobicity of a denture base acrylic resin and on Candida albicans adhesion. Arch. Oral Biol. 2013, 58, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Azuma, A.; Akiba, N.; Minakuchi, S. Hydrophilic surface modification of acrylic denture base material by silica coating and its influence on Candida albicans adherence. J. Med. Dent. Sci. 2012, 59, 1–7. [Google Scholar] [PubMed]
- Verran, J.; Maryan, C.J. Retention of Candida albicans on acrylic resin and silicone of different surface topography. J. Prosthet. Dent. 1997, 77, 535–539. [Google Scholar] [CrossRef]
- Chen, C.; Weir, M.D.; Cheng, L.; Lin, N.J.; Lin-Gibson, S.; Chow, L.C.; Zhou, X.; Xu, H.H. Antibacterial activity and ion release of bonding agent containing amorphous calcium phosphate nanoparticles. Dent. Mater. 2014, 30, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Beyth, N.; Yudovin-Farber, I.; Bahir, R.; Domb, A.J.; Weiss, E.I. Antibacterial activity of dental composites containing quaternary ammonium polyethylenimine nanoparticles against streptococcus mutans. Biomaterials 2006, 27, 3995–4002. [Google Scholar] [CrossRef] [PubMed]
- Namba, N.; Yoshida, Y.; Nagaoka, N.; Takashima, S.; Matsuura-Yoshimoto, K.; Maeda, H.; Van Meerbeek, B.; Suzuki, K.; Takashiba, S. Antibacterial effect of bactericide immobilized in resin matrix. Dent. Mater. 2009, 25, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Shirai, A.; Sumitomo, T.; Kurimoto, M.; Maseda, H.; Kourai, H. The mode of the antifungal activity of gemini-pyridinium salt against yeast. Biocontrol Sci. 2009, 14, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Palermo, E.F.; Lee, D.K.; Ramamoorthy, A.; Kuroda, K. Role of cationic group structure in membrane binding and disruption by amphiphilic copolymers. J. Phys. Chem. B 2011, 115, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Klotz, S.A.; Drutz, D.J.; Zajic, J.E. Factors governing adherence of Candida species to plastic surfaces. Infect. Immun. 1985, 50, 97–101. [Google Scholar] [PubMed]
- Puri, G.; Berzins, D.W.; Dhuru, V.B.; Raj, P.A.; Rambhia, S.K.; Dhir, G.; Dentino, A.R. Effect of phosphate group addition on the properties of denture base resins. J. Prosthet. Dent. 2008, 100, 302–308. [Google Scholar] [CrossRef]
- Yoshijima, Y.; Murakami, K.; Kayama, S.; Liu, D.; Hirota, K.; Ichikawa, T.; Miyake, Y. Effect of substrate surface hydrophobicity on the adherence of yeast and hyphal Candida. Mycoses 2010, 53, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Weir, M.D.; Fouad, A.F.; Xu, H.H. Time-kill behaviour against eight bacterial species and cytotoxicity of antibacterial monomers. J. Dent. 2013, 41, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Ren, B.; Zhou, X.; Xu, H.H.; Chen, Y.; Han, Q.; Li, B.; Weir, M.D.; Li, M.; Feng, M.; et al. Effect of antimicrobial denture base resin on multi-species biofilm formation. Int. J. Mol. Sci. 2016, 17. [Google Scholar] [CrossRef] [PubMed]
- Beyth, N.; Yudovin-Farber, I.; Perez-Davidi, M.; Domb, A.J.; Weiss, E.I. Polyethyleneimine nanoparticles incorporated into resin composite cause cell death and trigger biofilm stress in vivo. Proc. Natl. Acad. Sci. USA 2010, 107, 22038–22043. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Liu, H.; Weir, M.D.; Reynolds, M.A.; Zhang, K.; Xu, H.H. Three-dimensional biofilm properties on dental bonding agent with varying quaternary ammonium charge densities. J. Dent. 2016, 53, 73–81. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.; Han, Q.; Zhou, X.; Zhang, K.; Wang, S.; Xu, H.H.K.; Weir, M.D.; Feng, M.; Li, M.; Peng, X.; et al. Heat-Polymerized Resin Containing Dimethylaminododecyl Methacrylate Inhibits Candida albicans Biofilm. Materials 2017, 10, 431. https://doi.org/10.3390/ma10040431
Chen H, Han Q, Zhou X, Zhang K, Wang S, Xu HHK, Weir MD, Feng M, Li M, Peng X, et al. Heat-Polymerized Resin Containing Dimethylaminododecyl Methacrylate Inhibits Candida albicans Biofilm. Materials. 2017; 10(4):431. https://doi.org/10.3390/ma10040431
Chicago/Turabian StyleChen, Hui, Qi Han, Xuedong Zhou, Keke Zhang, Suping Wang, Hockin H. K. Xu, Michael D. Weir, Mingye Feng, Mingyun Li, Xian Peng, and et al. 2017. "Heat-Polymerized Resin Containing Dimethylaminododecyl Methacrylate Inhibits Candida albicans Biofilm" Materials 10, no. 4: 431. https://doi.org/10.3390/ma10040431




