The Effect of Er:YAG Lasers on the Reduction of Aerosol Formation for Dental Workers
Abstract
:1. Introduction
2. Materials and Methods
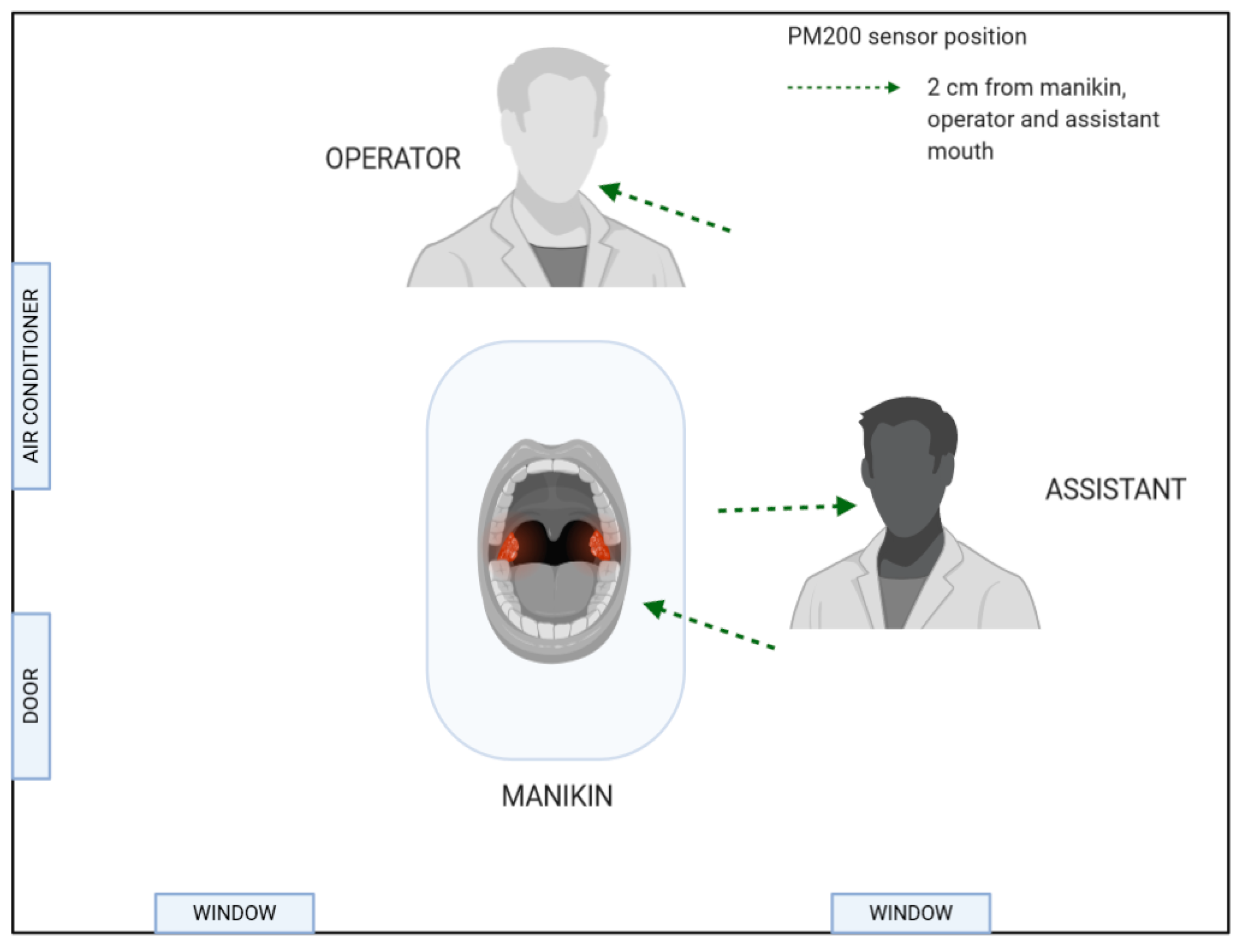
2.1. Aerosol Measurement Protocol
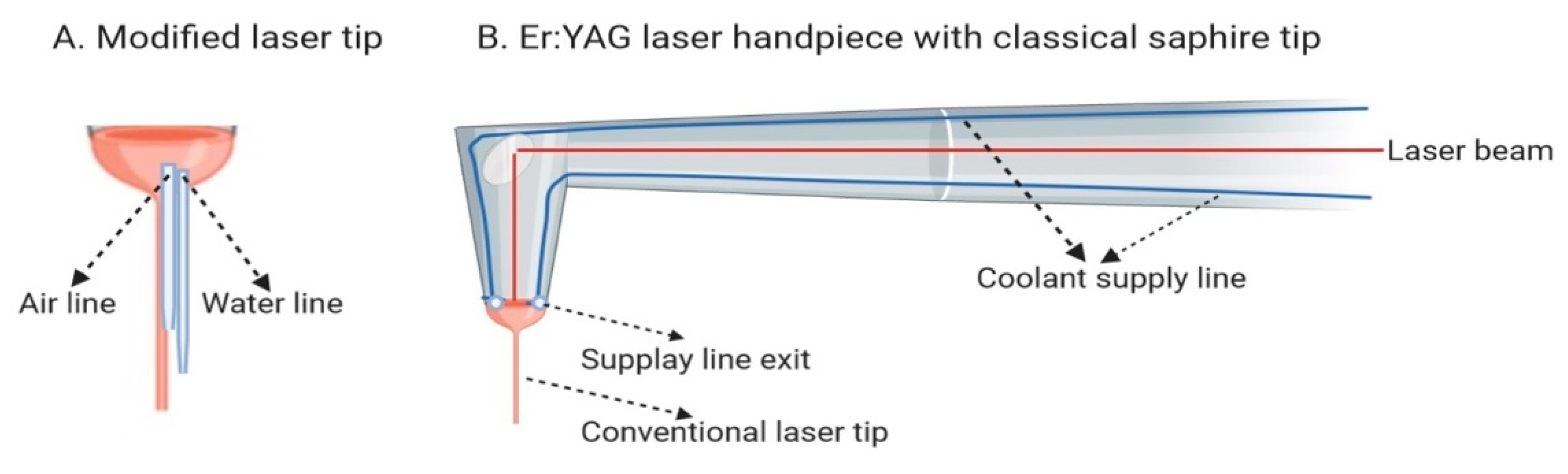
2.2. Technical Features of Er:YAG Lasers and Cooling System Applied in These Devices
2.3. Dental Treatment Procedures and Suction Systems Used in the Study
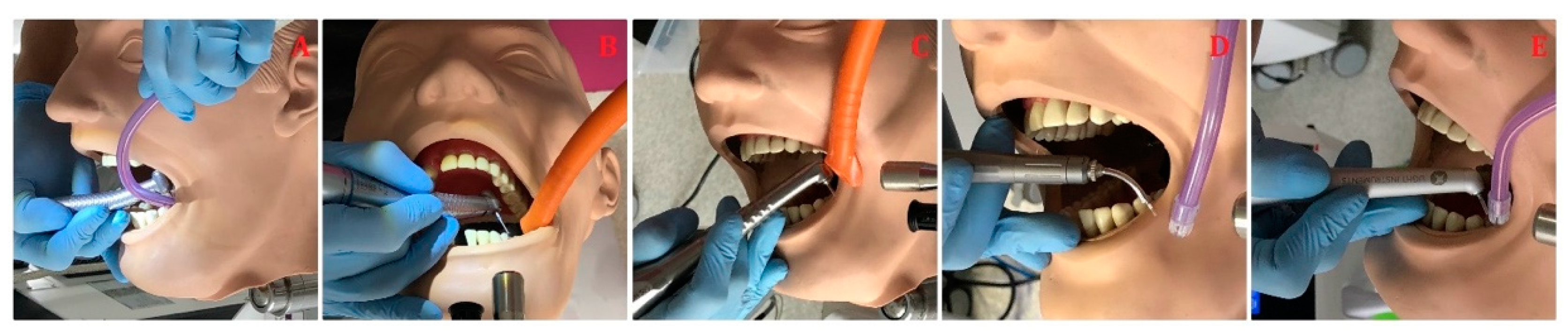
2.3.1. Caries’ Removal
2.3.2. Crown Laser Debonding
- (1)
- The contra-angle handpiece H14 of Er:YAG laser (LightWalker, Fotona, Slovenia) with laser parameters of energy 300 mJ, frequency 15 Hz, power 4.5 W, MSP mode, tip diameter of 1 mm, and water/air coolant 4/4;
- (2)
- The contra-angle handpiece of Er:YAG laser (AdvErL EVO, Morita, Japan) with laser parameters of energy 350 mJ, frequency 10 Hz, power 3.5 W, tip diameter: of 1 mm, and water/air coolant 4/4;
- (3)
- The contra-angle handpiece of Er:YAG laser (LiteTouch, LightInstruments, Israel) with laser parameters of energy 300 mJ, frequency 15 Hz, power 4.5 W, tip diameter of 1 mm, and water/air coolant 8/8 (Figure 4).
2.3.3. Orthodontic Brackets’ Debonding
- (1)
- The contra-angle handpiece H14 of Er:YAG laser (LightWalker, Fotona, Slovenia) with laser parameters of energy 170 mJ, frequency 20 Hz, power 3.4 W, MSP mode, tip diameter of 1 mm, and water/air coolant 3/3;
- (2)
- The contra-angle handpiece of Er:YAG laser (AdvErL EVO, Morita, Japan) with laser parameters of energy 170 mJ, frequency 20 Hz, power 3.4 W, tip diameter of 1 mm, and water/air coolant 3/3;
- (3)
- The contra-angle handpiece of Er:YAG laser (LiteTouch, LightInstruments, Israel) with laser parameters of energy 150 mJ, frequency 25 Hz, power 3.75 W, tip diameter of 1 mm, and water/air coolant 2/2 (Figure 5).
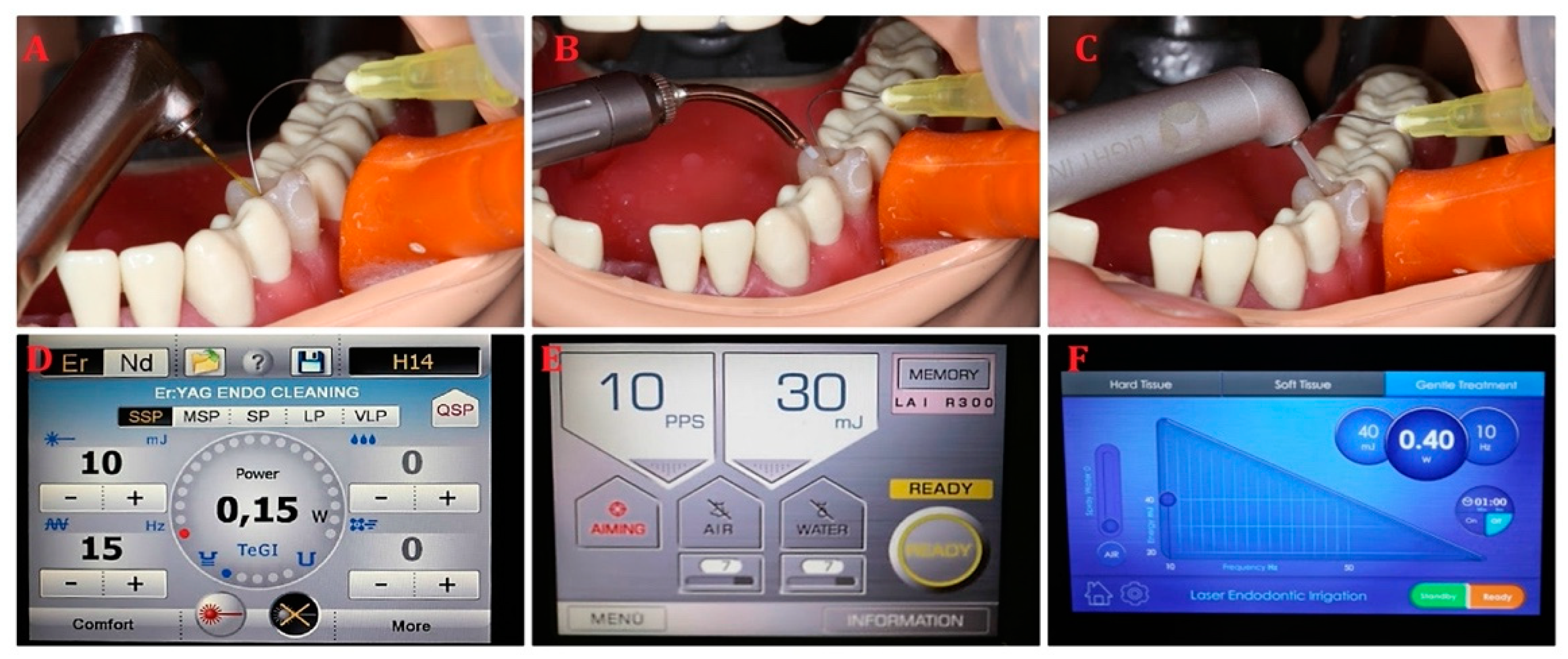
2.3.4. Endodontic Treatment
- (1)
- The contra-angle handpiece H14 of Er:YAG laser (LightWalker, Fotona, Slovenia) with laser parameters of energy 10 mJ, frequency 15 Hz, power 0.15 W, SSP mode, tip diameter of 0.6 mm, and water/air coolant 0/0;
- (2)
- The contra-angle handpiece of Er:YAG laser (AdvErL EVO, Morita, Japan) with laser parameters of energy 30 mJ, frequency 10 Hz, power 0.3 W, tip diameter of 0.6 mm, and water/air coolant 0/0;
- (3)
- The contra-angle handpiece of Er:YAG laser (LiteTouch, LightInstruments, Israel) with laser parameters of energy 40 mJ, frequency 10 Hz, power 0.4 W, tip diameter of 0.6 mm, and water/air coolant 0/0 (Figure 6).
2.4. Spray/Aerosol Evacuators
2.5. The Office Air Standardization
2.6. Statistical Analysis
3. Results
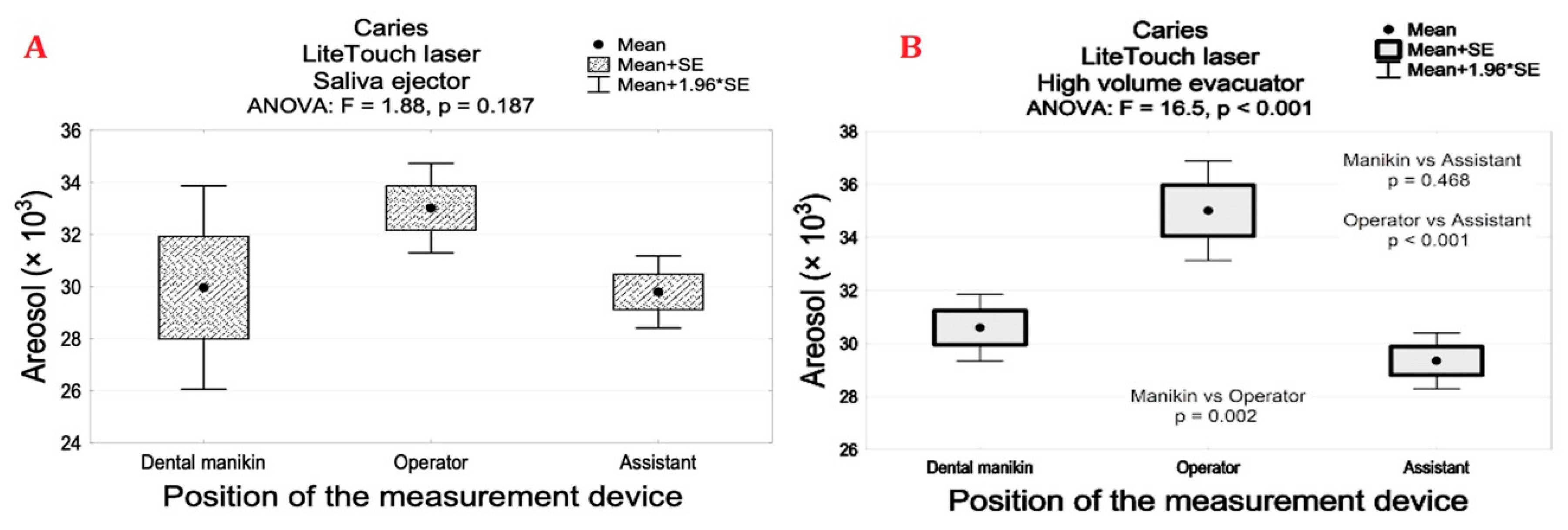
3.1. Erbium Lasers Reduced the Number of Aerosol Particles during Caries’ Treatment
3.2. Erbium Lasers Reduces the Number of Aerosol Particles during Ceramic Crown Debonding
3.3. Erbium Lasers Generated a Minimal Quantity of Aerosols during Orthodontic Bracket Debonding
3.4. Erbium Lasers-Assisted Endodontic Irrigation Generating Minimal Amount of Aerosols
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matys, J.; Grzech-Leśniak, K.; Dominiak, M. Disinfectants and devices for surface and air disinfection in dental offices. J. Stomatol. 2020, 73, 200–205. [Google Scholar] [CrossRef]
- Arnabat-Dominguez, J.; Del Vecchio, A.; Todea, C.; Grzech-Leśniak, K.; Vescovi, P.; Romeo, U.; Nammour, S. Laser dentistry in daily practice during the COVID-19 pandemic: Benefits, risks and recommendations for safe treatments. Adv. Clin. Exp. Med. 2021, 30, 119–125. [Google Scholar] [CrossRef]
- Dominiak, M.; Różyło-Kalinowska, I.; Gedrange, T.; Konopka, T.; Hadzik, J.; Bednarz, W.; Matys, J.; Lella, A.; Rayad, S.; Maksymowicz, R.; et al. COVID-19 and professional dental practice. The Polish Dental Association Working Group recommendations for procedures in dental office during an increased epidemiological risk. J. Stomatol. 2020, 73, 1–10. [Google Scholar] [CrossRef]
- Micik, R.E.; Miller, R.L.; Mazzarella, M.A.; Ryge, G. Studies on Dental Aerobiology: I. Bacterial Aerosols Generated during Dental Procedures. J. Dent. Res. 1969, 48, 49–56. [Google Scholar] [CrossRef]
- Miller, R.L. Characteristics of Blood-Containing Aerosols Generated by Common Powered Dental Instruments. Am. Ind. Hyg. Assoc. J. 1995, 56, 670–676. [Google Scholar] [CrossRef]
- Harrel, S.K.; Molinari, J. Aerosols and splatter in dentistry. J. Am. Dent. Assoc. 2004, 135, 429–437. [Google Scholar] [CrossRef]
- Bentley, C.D.; Burkhart, N.W.; Crawford, J.J. Evaluating Spatter and Aerosol Contamination During Dental Procedures. J. Am. Dent. Assoc. 1994, 125, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, A.B.; De Lima, C.J.; Villaverde, A.G.B.; Pereira, P.C.; Carvalho, H.C.; Zângaro, R.A. Photobiomodulation: Shining Light on COVID-19. Photobiomod. Photomed. Laser Surg. 2020, 38, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.-H.; Chen, C.-T.; Chuang, L.-C.; Lin, W.-M.; Wan, G.-H. Removal efficiency of central vacuum system and protective masks to suspended particles from dental treatment. PLoS ONE 2019, 14, e0225644. [Google Scholar] [CrossRef]
- Services CD. Services CD. The COVID-19 Dental Services Evidence Review Working Group. Recommendations for the Re-Opening of Dental Services: A Rapid Review of International Sources. Cochrane Oral Health. 2020. Available online: https://oralhealth.cochrane.org/sites/oralhealth.cochrane.org/files/public/uploads/covid19_dental_reopening_rapid_review_13052020.pdf (accessed on 16 April 2021).
- Coulthard, P. Dentistry and coronavirus (COVID-19)—Moral decision-making. Br. Dent. J. 2020, 228, 503–505. [Google Scholar] [CrossRef] [PubMed]
- Jacks, M.E. A laboratory comparison of evacuation devices on aerosol reduction. J. Dent. Hyg. JDH 2002, 76, 202–206. [Google Scholar]
- Flieger, R.; Gedrange, T.; Grzech-Leśniak, K.; Dominiak, M.; Matys, J. Low-Level Laser Therapy with a 635 nm Diode Laser Affects Orthodontic Mini-Implants Stability: A Randomized Clinical Split-Mouth Trial. J. Clin. Med. 2019, 9, 112. [Google Scholar] [CrossRef] [Green Version]
- Grzech-Leśniak, K.; Gaspirc, B.; Sculean, A. Clinical and microbiological effects of multiple applications of antibacterial photodynamic therapy in periodontal maintenance patients. A randomized controlled clinical study. Photodiagnosis Photodyn. Ther. 2019, 27, 44–50. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Nowicka, J.; Pajączkowska, M.; Matys, J.; Szymonowicz, M.; Kuropka, P.; Rybak, Z.; Dobrzyński, M.; Dominiak, M. Effects of Nd:YAG laser irradiation on the growth of Candida albicans and Streptococcus mutans: In vitro study. Lasers Med. Sci. 2018, 34, 129–137. [Google Scholar] [CrossRef]
- Matys, J.; Hadzik, J.; Dominiak, M. Schneiderian Membrane Perforation Rate and Increase in Bone Temperature During Maxillary Sinus Floor Elevation by Means of Er. Implant. Dent. 2017, 26, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Świder, K.; Flieger, R. Laser instant implant impression method: A case presentation. Dent. Med. Probl. 2017, 54, 101–106. [Google Scholar] [CrossRef] [Green Version]
- Zakrzewski, W.; Dobrzynski, M.; Kuropka, P.; Matys, J.; Malecka, M.; Kiryk, J.; Rybak, Z.; Dominiak, M.; Grzech-Lesniak, K.; Wiglusz, K.; et al. Removal of Composite Restoration from the Root Surface in the Cervical Region Using Er: YAG Laser and Drill—In Vitro Study. Materials 2020, 13, 3027. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Jurczyszyn, K.; Ziółkowski, P.; Dominiak, M.; Junior, A.B.; Romeo, U. Histological and Thermometric Examination of Soft Tissue De-Epithelialization Using Digitally Controlled Er:YAG Laser Handpiece: An Ex Vivo Study. Photomed. Laser Surg. 2018, 36, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Świder, K.; Dominiak, M.; Grzech-Leśniak, K.; Matys, J. Effect of Different Laser Wavelengths on Periodontopathogens in Peri-Implantitis: A Review of In Vivo Studies. Microorganisms 2019, 7, 189. [Google Scholar] [CrossRef] [Green Version]
- Grzech-Leśniak, K.; Bencharit, S.; Bs, N.D.; Mroczka, K.; Deeb, J.G. In Vitro Examination of the Use of Er:YAG Laser to Retrieve Lithium Disilicate Crowns from Titanium Implant Abutments. J. Prosthodont. 2019, 28, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Grzech-Leśniak, K.; Matys, J.; Żmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Junior, A.B.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Matys, J.; Grzech-Leśniak, K.; Flieger, R.; Dominiak, M. Assessment of an Impact of a Diode Laser Mode with Wavelength of 980 nm on a Temperature Rise Measured by Means of k-02 Thermocouple: Preliminary Results. Dent. Med. Probl. 2016, 53, 345–351. [Google Scholar] [CrossRef] [Green Version]
- Kenyon, B.J.; Van Zyl, I.; Louie, K.G. Comparison of cavity preparation quality using an electric motor handpiece and an air turbine dental handpiece. J. Am. Dent. Assoc. 2005, 136, 1101–1105. [Google Scholar] [CrossRef]
- Olivi, M.; Olivi, G. Physics of Laser. In Lasers in Restorative Dentistry; Springer: Berlin/Heidelberg, Germany, 2015; pp. 39–50. [Google Scholar]
- Rizcalla, N.; Bader, C.; Bortolotto, T.; Krejci, I. Improving the efficiency of an Er:YAG laser on enamel and dentin. Quintessence Int. 2012, 43, 22257878. [Google Scholar]
- Zhu, X.; Yin, X.; Chang, J.W.; Wang, Y.; Cheung, G.S.; Zhang, C. Comparison of the Antibacterial Effect and Smear Layer Removal Using Photon-Initiated Photoacoustic Streaming Aided Irrigation Versus a Conventional Irrigation in Single-Rooted Canals: An In Vitro Study. Photomed. Laser Surg. 2013, 31, 371–377. [Google Scholar] [CrossRef] [Green Version]
- Rupf, S.; Berger, H.; Buchter, A.; Harth, V.; Ong, M.F.; Hannig, M. Exposure of patient and dental staff to fine and ultrafine particles from scanning spray. Clin. Oral Investig. 2015, 19, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Nulty, A.; Lefkaditis, C.; Zachrisson, P.; Van Tonder, Q.; Yar, R. A clinical study measuring dental aerosols with and without a high-volume extraction device. Br. Dent. J. 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Szymańska, J. Dental bioaerosol as an occupational hazard in a dentist’s workplace. Ann. Agric. Environ. Med. 2007, 14, 203–207. [Google Scholar] [PubMed]
- Sotiriou, M.; Ferguson, S.F.; Davey, M.; Wolfson, J.M.; Demokritou, P.; Lawrence, J.; Sax, S.N.; Koutrakis, P. Measurement of particle concentrations in a dental office. Environ. Monit. Assess. 2007, 137, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Elkharashi, A.; Grzech-Leśniak, K.; Deeb, J.G.; Abdulmajeed, A.A.; Bencharit, S. Exploring the use of pulsed erbium lasers to retrieve a zirconia crown from a zirconia implant abutment. PLoS ONE 2020, 15, e0233536. [Google Scholar] [CrossRef] [PubMed]
- Deeb, J.G.; Bencharit, S.; Dalal, N.; Abdulmajeed, A.; Grzech-Leśniak, K. Using Er:YAG laser to remove lithium disilicate crowns from zirconia implant abutments: An in vitro study. PLoS ONE 2019, 14, e0223924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grzech-Leśniak, K.; Bencharit, S.; Skrjanc, L.; Kanduti, D.; Matys, J.; Deeb, J.G. Utilization of Er:YAG Laser in Retrieving and Reusing of Lithium Disilicate and Zirconia Monolithic Crowns in Natural Teeth: An In Vitro Study. Appl. Sci. 2020, 10, 4357. [Google Scholar] [CrossRef]
- Grzech-Leśniak, K.; Matys, J.; Dominiak, M. Comparison of the clinical and microbiological effects ofantibiotic therapy in periodontal pockets following laser treatment: An in vivo study. Adv. Clin. Exp. Med. 2018, 27, 1263–1270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [Green Version]
- Enwemeka, C.S.; Bumah, V.V.; Masson-Meyers, D.S. Light as a potential treatment for pandemic coronavirus infections: A perspective. J. Photochem. Photobiol. B Biol. 2020, 207, 111891. [Google Scholar] [CrossRef] [PubMed]


| – | AdvErL Evo Laser | LiteTouch Laser | LightWalker Laser |
|---|---|---|---|
| Laser class | class 4 | class 4 | class 4 |
| Mode | pulsed | pulsed | pulsed |
| Wavelength | 2940 nm | 2940 nm | 2940 nm |
| Transmission system | flexible waveguide | reduced articulated arm | articulated arm |
| Air compression system | built in | external | built in |
| Types of coolant supply | modified laser tip with water and air supply lines built in the tip | conventional laser handpiece with water supply lines in the handpiece and with the lines’ exits in the head of the handpiece | conventional laser handpiece with water supply lines in the handpiece and with the lines’ exits in the head of the handpiece |
| Coolant | saline solution | distillated water | distillated water |
| Procedure | Tools | Exhaustion | Place of Measurement | ANOVA p | ||
|---|---|---|---|---|---|---|
| Manikin (A) Mean (SD) | Operator (B) Mean (SD) | Assistant (C) Mean (SD) | p Values | |||
| Caries | High-speed handpiece | Saliva ejector | 235.2 (18.80) | 112.2 (18.6) | 101.5 (10.6) | A vs. BC p < 0.001 |
| High volume evacuator | 64.1 (4.6) | 42.3 (4.5) | 33.5 (3.1) | A vs. BC p < 0.001 B vs. C p < 0.001 | ||
| Low-speed handpiece | Saliva ejector | 183.0 (8.1) | 89.1 (7.6) | 44.3 (4.9) | A vs. BC p < 0.001 B vs. C p < 0.001 | |
| High volume evacuator | 55.1 (3.3) | 37.1 (4.2) | 34.1 (4.5) | A vs. BC p < 0.001 | ||
| Morita laser | Saliva ejector | 30.1 (0.7) | 30.0 (0.8) | 29.6 (0.5) | 0.447 | |
| High volume evacuator | 29.5 (0.6) | 29.7 (0.9) | 29.2 (0.4) | 0.542 | ||
| Fotona laser | Saliva ejector | 29.9 (1.3) | 32.5 (3.8) | 32.1 (1.5) | 0.368 | |
| High volume evacuator | 29.4 (1.4) | 33.8 (2.8) | 31.3 (1.5) | 0.248 | ||
| LiteTouch laser | Saliva ejector | 29.9 (4.9) | 33.0 (2.1) | 29.8 (1.7) | 0.187 | |
| High volume evacuator | 30.6 (1.6) | 35.0 (2.3) | 29.3 (1.3) | B vs. AC p < 0.05 | ||
| – | – | ANOVA | p < 0.001 | p < 0.001 | p < 0.001 | — |
| Exhaustion | Place of Measurement | Crown Debonding—Tools | ANOVA p | |||
|---|---|---|---|---|---|---|
| Morita Laser (A) Mean (SD) | Fotona Laser (B) Mean (SD) | LiteTouch Laser (C) Mean (SD) | High-Speed Turbine (D) | p Values | ||
| Saliva ejector | Manikin | 41.8 (2.7) | 43.6 (2.2) | 54.3 (4.7) | 284.8 (26.5) | D vs. ABC p < 0.001 C vs. AB p < 0.001 |
| Operator | 33.1 (2.7) | 44.1 (2.6) | 47.4 (3.9) | 154.4 (22.3) | D vs. ABC p < 0.001 B, C vs. A p < 0.001 | |
| Assistant | 30.7 (1.4) | 43.2 (2.1) | 43.7 (3.1) | 112.5 (14.2) | D vs. ABC p < 0.001 B, C vs. A p < 0.001 | |
| High volume evacuator | Manikin | 40.5 (1.9) | 43.2 (0.6) | 44.1 (4.0) | 67.5 (8.3) | D vs. ABC p < 0.001 |
| Operator | 30.6 (0.6) | 43.9 (1.8) | 44.3 (3.1) | 58.3 (7.4) | D vs. ABC p < 0.001 B, C vs. A p < 0.001 | |
| Assistant | 29.4 (1.2) | 43.6 (2.4) | 43.1 (2.9) | 47.5 (4.3) | D vs. ABC p < 0.001 B, C vs. A p < 0.001 | |
| Exhaustion | Place of Measurement | Debonding Ortho—Tools | ANOVA | ||
|---|---|---|---|---|---|
| Morita Laser (A) Mean (SD) | Fotona Laser (B) Mean (SD) | LiteTouch Laser (C) Mean (SD) | p Values | ||
| Saliva ejector | Manikin | 29.5 (3.3) | 30.5 (1.6) a | 31.4 (1.5) c | 0.374 |
| Operator | 25.8 (8.5) | 30.7 (1.2) b | 30.5 (3.0) | A vs. BC p < 0.001 | |
| Assistant | 26.8 (1.0) | 29.4 (1.1) | 30.6 (1.9) | A vs. BC p < 0.001 | |
| High volume evacuator | Manikin | 28.4 (3.8) | 28.6 (1.3) a | 29.6 (2.0) c | 0.365 |
| Operator | 26.2 (3.2) | 29.2 (0.8) b | 30.4 (0.5) | A vs. BC p < 0.001 | |
| Assistant | 26.5 (1.3) | 29.0 (1.1) | 29.6 (1.7) | A vs. BC p < 0.001 | |
| — | — | p > 0.05 | p < 0.05 | p < 0.05 | — |
| Exhaustion | Place of Measurement | Endo Irrigation—Tools | ANOVA p | |||
|---|---|---|---|---|---|---|
| Morita Laser (A) Mean (SD) | Fotona Laser (B) Mean (SD) | LiteTouch Laser (C) Mean (SD) | Endodontic Needle (D) Mean (SD) | p Values | ||
| Saliva ejector | Manikin | 30.1 (1.3) | 30.3 (1.8) | 30.8 (1.6) | 31.2 (1.5) | p > 0.05 |
| Operator | 30.7 (1.8) | 32.0 (1.9) | 31.7 (2.1) | 31.8 (1.6) | p > 0.05 | |
| Assistant | 30.3 (1.5) | 30.8 (1.7) | 31.3 (1.9) | 30.7 (1.6) | p > 0.05 | |
| High volume evacuator | Manikin | 29.9 (1.4) | 30.8 (0.9) | 30.9 (1.7) | 30.6 (1.1) | p > 0.05 |
| Operator | 30.7 (2.2) | 30.7 (2.4) | 31.7 (2.1) | 31.7 (2.8) | p > 0.05 | |
| Assistant | 30.1 (1.7) | 31.9 (1.4) | 30.7 (1.7) | 30.9 (1.1) | p > 0.05 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzech-Leśniak, K.; Matys, J. The Effect of Er:YAG Lasers on the Reduction of Aerosol Formation for Dental Workers. Materials 2021, 14, 2857. https://doi.org/10.3390/ma14112857
Grzech-Leśniak K, Matys J. The Effect of Er:YAG Lasers on the Reduction of Aerosol Formation for Dental Workers. Materials. 2021; 14(11):2857. https://doi.org/10.3390/ma14112857
Chicago/Turabian StyleGrzech-Leśniak, Kinga, and Jacek Matys. 2021. "The Effect of Er:YAG Lasers on the Reduction of Aerosol Formation for Dental Workers" Materials 14, no. 11: 2857. https://doi.org/10.3390/ma14112857