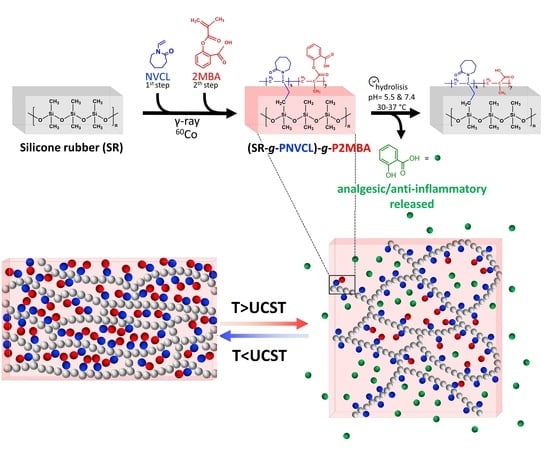
Poly(N-vinylcaprolactam) and Salicylic Acid Polymeric Prodrug Grafted onto Medical Silicone to Obtain a Novel Thermo- and pH-Responsive Drug Delivery System for Potential Medical Devices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
Synthesis of 2MBA
2.2. Grafting Process
2.2.1. Synthesis of SR-g-PNVCL (First Functionalization)
2.2.2. Synthesis of (SR-g-PNVCL)-g-P2MBA (Second Functionalization)
2.3. Characterization of (SR-g-PNVCL)-g-(P2MBA) Films
2.3.1. ATR-FTIR Analysis
2.3.2. TGA Analysis
2.3.3. SEM-EDX Analysis
2.3.4. Contact Angle, Swelling, and Temperature-Responsive Analysis
2.4. Drug Release and Characterization Analysis (HPLC and GC–MS)
2.5. Cytocompatibility Analysis
3. Results
3.1. Grafting Process
3.1.1. Synthesis of SR-g-PNVCL
3.1.2. Synthesis of (SR-g-PNVCL)-g-P2MBA
3.2. Characterization of (SR-g-PNVCL)-g-P2MBA Films
3.2.1. ATR-FTIR Analysis
3.2.2. TGA Analysis
3.2.3. SEM-EDX Analysis
3.2.4. Contact Angle, Swelling, and Temperature Responsiveness Analysis
3.3. Drug Release and Characterization Analysis (HPLC and GC–MS)
3.4. Cytocompatibility Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Song, W.; Li, J.; Li, H.; Ming, X. Human factors risk assessment: An integrated method for improving safety in clinical use of medical devices. Appl. Soft Comput. 2020, 86, 105918. [Google Scholar] [CrossRef]
- Grennan, M.; Town, R.J. Regulating Innovation with Uncertain Quality: Information, Risk, and Access in Medical Devices. Am. Econ. Rev. 2020, 110, 120–161. [Google Scholar] [CrossRef] [Green Version]
- Aronson, J.K.; Ferner, R.E. Clarification of Terminology in Drug Safety. Drug Saf. 2005, 28, 851–870. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.K.; Heneghan, C.; Ferner, R.E. Medical Devices: Definition, Classification, and Regulatory Implications. Drug Saf. 2019, 43, 83–93. [Google Scholar] [CrossRef]
- Vajapey, S.P.; Li, M. Medical Device Recalls in Orthopedics: Recent Trends and Areas for Improvement. J. Arthroplast. 2020, 35, 2259–2266. [Google Scholar] [CrossRef] [PubMed]
- McKittrick, C.M.; Cardona, M.J.; Black, R.A.; McCormick, C. Development of a Bioactive Polymeric Drug Eluting Coronary Stent Coating Using Electrospraying. Ann. Biomed. Eng. 2020, 48, 271–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, B.; Moriarty, T.F.; Webster, T.; Xing, M. Racing for the Surface: Antimicrobial and Interface Tissue Engineering; Springer: Morgantown, WV, USA, 2020; ISBN 9783030344719. [Google Scholar]
- Benito-Ruiz, J.; Redondo, A. Breast Augmentation Surgery: How Do We Do It? Results of a Joint Survey from European Association of Societies of Aesthetic Plastic Surgery. Aesthetic Plast. Surg. 2020, 44, 1957–1964. [Google Scholar] [CrossRef] [PubMed]
- Geyao, L.; Yang, D.; Wanglin, C.; Chengyong, W. Development and application of physical vapor deposited coatings for medical devices: A review. Procedia CIRP 2020, 89, 250–262. [Google Scholar] [CrossRef]
- Almouse, R.; Wen, X.; Na, S.; Anderson, G.; Xie, D. Polyvinylchloride surface with enhanced cell/bacterial adhesion-resistant and antibacterial functions. J. Biomater. Appl. 2019, 33, 1415–1426. [Google Scholar] [CrossRef]
- Zanocco, M.; Marin, E.; Boschetto, F.; Adachi, T.; Yamamoto, T.; Kanamura, N.; Zhu, W.; McEntire, B.J.; Bal, B.S.; Ashida, R.; et al. Surface Functionalization of Polyethylene by Silicon Nitride Laser Cladding. Appl. Sci. 2020, 10, 2612. [Google Scholar] [CrossRef] [Green Version]
- Asadinezhad, A.; Lehocký, M.; Sáha, P.; Mozetič, M. Recent Progress in Surface Modification of Polyvinyl Chloride. Materials 2012, 5, 2937–2959. [Google Scholar] [CrossRef] [Green Version]
- Slettengren, M.; Mohanty, S.; Kamolvit, W.; Van Der Linden, J.; Brauner, A. Making medical devices safer: Impact of plastic and silicone oil on microbial biofilm formation. J. Hosp. Infect. 2020, 106, 155–162. [Google Scholar] [CrossRef]
- Bernard, M.; Jubeli, E.; Pungente, M.D.; Yagoubi, N. Biocompatibility of polymer-based biomaterials and medical devices—Regulations, in vitroscreening and risk-management. Biomater. Sci. 2018, 6, 2025–2053. [Google Scholar] [CrossRef]
- Teo, A.J.; Mishra, A.; Park, I.; Kim, Y.-J.; Park, W.-T.; Yoon, Y.-J. Polymeric Biomaterials for Medical Implants and Devices. ACS Biomater. Sci. Eng. 2016, 2, 454–472. [Google Scholar] [CrossRef]
- Bracaglia, L.G.; Smith, B.T.; Watson, E.; Arumugasaamy, N.; Mikos, A.G.; Fisher, J.P. 3D printing for the design and fabrication of polymer-based gradient scaffolds. Acta Biomater. 2017, 56, 3–13. [Google Scholar] [CrossRef]
- Arrabito, G.; Ferrara, V.; Bonasera, A.; Pignataro, B. Artificial Biosystems by Printing Biology. Small 2020, 16, e1907691. [Google Scholar] [CrossRef] [PubMed]
- Mu, X.; Fitzpatrick, V.; Kaplan, D.L. From Silk Spinning to 3D Printing: Polymer Manufacturing using Directed Hierarchical Molecular Assembly. Adv. Health Mater. 2020, 9, e1901552. [Google Scholar] [CrossRef] [PubMed]
- Daniels, A.U. Silicone breast implant materials. Swiss Med. Wkly. 2012, 142, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Bengtson, B.P.; Heo, C.Y. Various Properties of Silicone Breast Implant Surfaces and Multimodal Techniques for the Functional Surface Modification. Clin. Plast. Surg. 2021, 48, 87–99. [Google Scholar] [CrossRef]
- Mujagic, E.; Zeindler, J.; Coslovsky, M.; Hoffmann, H.; Soysal, S.D.; Mechera, R.; Von Strauss, M.; Delko, T.; Saxer, F.; Glaab, R.; et al. The association of surgical drains with surgical site infections—A prospective observational study. Am. J. Surg. 2019, 217, 17–23. [Google Scholar] [CrossRef]
- Hallab, N.J.; Samelko, L.; Hammond, D. The Inflammatory Effects of Breast Implant Particulate Shedding: Comparison With Orthopedic Implants. Aesthetic Surg. J. 2019, 39, S36–S48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, A.R.; Forster, S.P.; White, D.; Terife, G.; Lowinger, M.; Teller, R.S.; Barrett, S.E. Drug eluting implants in pharmaceutical development and clinical practice. Expert Opin. Drug Deliv. 2021, 1–17. [Google Scholar] [CrossRef]
- Ratner, B.D.; Hoffman, A.S.; McArthur, S.L. Physicochemical Surface Modification of Materials Used in Medicine, 4th ed.; Elsevier: Pittsburgh, PA, USA, 2020; ISBN 978-0-12-816137-1. [Google Scholar]
- Pino-Ramos, V.H.; Meléndez-Ortiz, H.I.; Ramos-Ballesteros, A.; Bucio, E. Radiation Grafting of Biopolymers and Synthetic Polymers; Elsevier Inc.: Amsterdam, The Netherlands, 2018; ISBN 9780128104620. [Google Scholar]
- Vázquez, E.; Muro, C.; Illescas, J.; Burillo, G.; Hernández, O.; Rivera, E. Obtainment and Characterization of Hydrophilic Polysulfone Membranes by N-Vinylimidazole Grafting Induced by Gamma Irradiation. Polymer 2020, 12, 1284. [Google Scholar] [CrossRef]
- Meléndez-Ortiz, H.I.; Alvarez-Lorenzo, C.; Burillo, G.; Magariños, B.; Concheiro, A.; Bucio, E. Radiation-grafting of N-vinylimidazole onto silicone rubber for antimicrobial properties. Radiat. Phys. Chem. 2015, 110, 59–66. [Google Scholar] [CrossRef]
- Cabana, S.; Lecona-Vargas, C.S.; Meléndez-Ortiz, H.I.; Contreras-García, A.; Barbosa, S.; Taboada, P.; Magariños, B.; Bucio, E.; Concheiro, A.; Alvarez-Lorenzo, C. Silicone rubber films functionalized with poly(acrylic acid) nanobrushes for immobilization of gold nanoparticles and photothermal therapy. J. Drug Deliv. Sci. Technol. 2017, 42, 245–254. [Google Scholar] [CrossRef]
- Fuke, C.A.; Mahanwar, P.A.; Chowdhury, S.R. Modified ethylene-propylene-diene elastomer (EPDM)-contained silicone rubber/ethylene-propylene-diene elastomer (EPDM) blends: Effect of composition and electron beam crosslinking on mechanical, heat shrinkability, electrical, and morphological properties. J. Appl. Polym. Sci. 2019, 136, 1–8. [Google Scholar] [CrossRef]
- Chapiro, A. Radiation induced grafting. Radiat. Phys. Chem. 1977, 9, 55–67. [Google Scholar] [CrossRef]
- Pérez-Calixto, M.; González-Pérez, G.; Dionisio, N.; Bucio, E.; Burillo, G.; García-Uriostegui, L. Surface functionalization of polypropylene and polyethylene films with allylamine by γ radiation. MRS Commun. 2019, 9, 264–269. [Google Scholar] [CrossRef]
- Pino-Ramos, V.H.; Ramos-Ballesteros, A.; López-Saucedo, F.; López-Barriguete, J.E.; Varca, G.H.C.; Bucio, E. Radiation Grafting for the Functionalization and Development of Smart Polymeric Materials. Top. Curr. Chem. 2016, 374, 63. [Google Scholar] [CrossRef]
- Ramos-Ballesteros, A.; Pino-Ramos, V.H.; López-Saucedo, F.; Flores-Rojas, G.G.; Bucio, E. γ-Rays and Ions Irradiation. Surf. Modif. Polym. 2019, 185–209. [Google Scholar] [CrossRef]
- Flores-Rojas, G.G.; López-Saucedo, F.; Vázquez, E.; Hernández-Mecinas, E.; Huerta, L.; Cedillo, G.; Concheiro, A.; Alvarez-Lorenzo, C.; Bucio, E. Synthesis of polyamide-6@cellulose microfilms grafted with N-vinylcaprolactam using gamma-rays and loading of antimicrobial drugs. Cellulose 2020, 27, 2785–2801. [Google Scholar] [CrossRef]
- Kavaklı, P.A.; Kavaklı, C.; Seko, N.; Tamada, M.; Güven, O. Radiation induced emulsion graft polymerization of 4-vinylpyridine onto PE/PP nonwoven fabric for As(V) adsorption. Radiat. Phys. Chem. 2016, 127, 13–20. [Google Scholar] [CrossRef]
- Hidzir, N.M.; Kępa, K.; Hill, D.J.T.; Jorgensen, L.; Grøndahl, L. Protein adsorption to poly(tetrafluoroethylene) membranes modified with grafted poly(acrylic acid) chains. Biointerphases 2020, 15, 031011. [Google Scholar] [CrossRef] [PubMed]
- Zuñiga-Zamorano, I.; Meléndez-Ortiz, H.I.; Costoya, A.; Alvarez-Lorenzo, C.; Concheiro, A.; Bucio, E. Poly(vinyl chloride) catheters modified with pH-responsive poly(methacrylic acid) with affinity for antimicrobial agents. Radiat. Phys. Chem. 2018, 142, 107–114. [Google Scholar] [CrossRef]
- Das, S.S.; Bharadwaj, P.; Bilal, M.; Barani, M.; Rahdar, A.; Taboada, P.; Bungau, S.; Kyzas, G.Z. Stimuli-Responsive Polymeric Nanocarriers for Drug Delivery, Imaging, and Theragnosis. Polymer 2020, 12, 1397. [Google Scholar] [CrossRef]
- Bedoya, D.A.; Figueroa, F.N.; Macchione, M.A.; Strumia, M.C. Stimuli-Responsive Polymeric Systems for Smart Drug Delivery; Springer International Publishing: Amman, Jordan, 2020; ISBN 9783030469238. [Google Scholar]
- Pasparakis, G.; Tsitsilianis, C. LCST polymers: Thermoresponsive nanostructured assemblies towards bioapplications. Polymer 2020, 211, 123146. [Google Scholar] [CrossRef]
- Sponchioni, M.; Palmiero, U.C.; Moscatelli, D. Thermo-responsive polymers: Applications of smart materials in drug delivery and tissue engineering. Mater. Sci. Eng. C 2019, 102, 589–605. [Google Scholar] [CrossRef]
- Gandhi, A.; Paul, A.; Sen, S.O.; Sen, K.K. Studies on thermoresponsive polymers: Phase behaviour, drug delivery and biomedical applications. Asian J. Pharm. Sci. 2015, 10, 99–107. [Google Scholar] [CrossRef] [Green Version]
- Meléndez-Ortiz, H.I.; Alvarez-Lorenzo, C.; Concheiro, A.; Bucio, E. Grafting of N-vinyl caprolactam and methacrylic acid onto silicone rubber films for drug-eluting products. J. Appl. Polym. Sci. 2015, 132, 1–11. [Google Scholar] [CrossRef]
- Pino-Ramos, V.H.; Flores-Rojas, G.G.; Alvarez-Lorenzo, C.; Concheiro, A.; Bucio, E. Graft copolymerization by ionization radiation, characterization, and enzymatic activity of temperature-responsive SR-g-PNVCL loaded with lysozyme. React. Funct. Polym. 2018, 126, 74–82. [Google Scholar] [CrossRef]
- Magaña, H.; Palomino, K.; Cornejo-Bravo, J.M.; Díaz-Gómez, L.; Concheiro, A.; Zavala-Lagunes, E.; Alvarez-Lorenzo, C.; Bucio, E. Polymeric prodrug⿿functionalized polypropylene films for sustained release of salicylic acid. Int. J. Pharm. 2016, 511, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Magaña, H.; Becerra, C.D.; Serrano-Medina, A.; Palomino, K.; Palomino-Vizcaíno, G.; Olivas-Sarabia, A.; Bucio, E.; Cornejo-Bravo, J.M. Radiation Grafting of a Polymeric Prodrug onto Silicone Rubber for Potential Medical/Surgical Procedures. Polymer 2020, 12, 1297. [Google Scholar] [CrossRef]
- Uddin, S. Development of Biopharmaceutical Drug-Device Products; Springer: Glasgow, UK, 2020; Volume 35, ISBN 978-3-030-31414-9. [Google Scholar]
- Paradise, J. Regulating Nanomedicine at the Food and Drug Administration. AMA J. Ethic 2019, 21, E347–E355. [Google Scholar] [CrossRef] [Green Version]
- Wu, P.; Grainger, D.W. Drug/device combinations for local drug therapies and infection prophylaxis. Biomaterials 2006, 27, 2450–2467. [Google Scholar] [CrossRef]
- Quarterman, J.C.; Geary, S.M.; Salem, A.K. Evolution of drug-eluting biomedical implants for sustained drug delivery. Eur. J. Pharm. Biopharm. 2021, 159, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Lorenzo, C.; Garcia-Gonzalez, C.A.; Bucio, E.; Concheiro, A. Stimuli-responsive polymers for antimicrobial therapy: Drug targeting, contact-killing surfaces and competitive release. Expert Opin. Drug Deliv. 2016, 13, 1109–1119. [Google Scholar] [CrossRef] [PubMed]
- Licea-Claverie, A.; Rogel-Hernández, E.; Lopez-Sanchez, J.A.; Castillo-Arámbula, L.A.; Cornejo-Bravo, J.M.; Arndt, K.F. A facile synthesis route for carboxyaryl-methacrylates: A way to obtain aromatic polyelectrolytes. Des. Monomers Polym. 2003, 6, 67–80. [Google Scholar] [CrossRef]
- Valencia-Mora, R.A.; Zavala-Lagunes, E.; Bucio, E. Grafting of thermo-sensitive N-vinylcaprolactam onto silicone rubber through the direct radiation method. Radiat. Phys. Chem. 2016, 124, 155–158. [Google Scholar] [CrossRef]
- Statgraphics Centurion XVIII. Available online: https://statgraphics.net/ (accessed on 30 December 2019).
- Shit, S.C.; Shah, P.M. A Review on Silicone Rubber. Natl. Acad. Sci. Lett. 2013, 36, 355–365. [Google Scholar] [CrossRef]
- Ashfaq, A.; Clochard, M.-C.; Coqueret, X.; Dispenza, C.; Driscoll, M.S.; Ulański, P.; Al-Sheikhly, M. Polymerization Reactions and Modifications of Polymers by Ionizing Radiation. Polymer 2020, 12, 2877. [Google Scholar] [CrossRef] [PubMed]
- Menhofer, H.; Zluticky, J.; Heusinger, H. The influence of irradiation temperature and oxygen on crosslink formation and segment mobility in gamma-irradiated polydimethylsiloxanes. Int. J. Radiat. Appl. Instrum. C 1989, 33, 561–566. [Google Scholar] [CrossRef]
- Shaik, M.G.; Karuppaiyan, V. Effect of Ageing on the Tracking Characteristics of High-Temperature Vulcanized Silicone Rubber Hybrid Composites for High Voltage Insulation. Materials 2020, 13, 2242. [Google Scholar] [CrossRef]
- Kozanoǧlu, S.; Özdemir, T.; Usanmaz, A. Polymerization of N-Vinylcaprolactam and Characterization of Poly(N-Vinylcaprolactam). J. Macromol. Sci. Part A 2011, 48, 467–477. [Google Scholar] [CrossRef]
- Sobhi, H.; Matthews, M.E.; Grandy, B.; Masnovi, J.; Riga, A.T. Selecting polymers for medical devices based on thermal analytical methods. J. Therm. Anal. Calorim. 2008, 93, 535–539. [Google Scholar] [CrossRef]
- Xiong, Y.; Rowland, S.; Robertson, J.; Day, R. Surface analysis of asymmetrically aged 400 kV silicone rubber composite insulators. IEEE Trans. Dielectr. Electr. Insul. 2008, 15, 763–770. [Google Scholar] [CrossRef]
- Qin, G.; Shen, Z.; Yu, Y.; Fan, L.; Cao, H.; Yin, C. Effect of Silicone Rubber of a Waste Composite Insulator on Cement Mortar Properties. Materials 2019, 12, 2796. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fang, S.; Hu, Y.; Song, L.; Zhan, J.; He, Q. Mechanical properties, fire performance and thermal stability of magnesium hydroxide sulfate hydrate whiskers flame retardant silicone rubber. J. Mater. Sci. 2007, 43, 1057–1062. [Google Scholar] [CrossRef]
- Xuguang, L.; Yougong, W.; FuYi, L. Study on improving the tracking and erosion resistance of silicone rubber. In Proceedings of the 6th International Conference on Properties and Applications of Dielectric Materials (Cat. No.00CH36347), Xián, China, 21–26 June 2000; pp. 342–345. [Google Scholar] [CrossRef]
- Magaña, H.; Palomino, K.; Cornejo-Bravo, J.M.; Alvarez-Lorenzo, C.; Concheiro, A.; Bucio, E. Radiation-grafting of acrylamide onto silicone rubber films for diclofenac delivery. Radiat. Phys. Chem. 2015, 107, 164–170. [Google Scholar] [CrossRef]
- Vázquez-González, B.; Meléndez-Ortiz, H.I.; Díaz-Gómez, L.; Alvarez-Lorenzo, C.; Concheiro, A.; Bucio, E. Silicone Rubber Modified with Methacrylic Acid to Host Antiseptic Drugs. Macromol. Mater. Eng. 2014, 299, 1240–1250. [Google Scholar] [CrossRef]
- Syakur, A.; Berahim, H. Hydrophobic Contact Angle and Surface Degradation of Epoxy Resin Compound with Silicon Rubber and Silica. Electr. Electron. Eng. 2012, 2, 284–291. [Google Scholar] [CrossRef]
- Ali, M.; Hackam, R. Recovery of Hydrophobicity of HTV Silicone Rubber after Accelerated Aging in Saline Solutions. IEEE Trans. Dielectr. Electr. Insul. 2009, 16, 842–852. [Google Scholar] [CrossRef]
- Bennett, A.J. The absorption of globular proteins. Biopolymers 1973, 12, 1671–1676. [Google Scholar] [CrossRef] [PubMed]
- Hameed, N.; Guo, Q.; Hanley, T.; Mai, Y.-W. Hydrogen bonding interactions, crystallization, and surface hydrophobicity in nanostructured epoxy/block copolymer blends. J. Polym. Sci. Part B Polym. Phys. 2010, 48, 790–800. [Google Scholar] [CrossRef]
- Meeussen, F.; Nies, E.; Berghmans, H.; Verbrugghe, S.; Goethals, E.; Du Prez, F. Phase behaviour of poly(N-vinyl caprolactam) in water. Polymer 2000, 41, 8597–8602. [Google Scholar] [CrossRef]
- Ferraz, C.C.; Varca, G.H.; Ruiz, J.-C.; Lopes, P.S.; Mathor, M.B.; Lugao, A.B.; Bucio, E. Radiation-grafting of thermo- and pH-responsive poly(N-vinylcaprolactam-co-acrylic acid) onto silicone rubber and polypropylene films for biomedical purposes. Radiat. Phys. Chem. 2014, 97, 298–303. [Google Scholar] [CrossRef]
- Pietsch, C.; Hoogenboom, R.; Schubert, U.S. PMMA based soluble polymeric temperature sensors based on UCST transition and solvatochromic dyes. Polym. Chem. 2010, 1, 1005–1008. [Google Scholar] [CrossRef]
- Zhang, Q.; Hoogenboom, R. Polymers with upper critical solution temperature behavior in alcohol/water solvent mixtures. Prog. Polym. Sci. 2015, 48, 122–142. [Google Scholar] [CrossRef]
- Marcus, F.; Colaizzi, J.L.; Barry, H. pH Effects on Salicylate Absorption from Hydrophilic Ointment. J. Pharm. Sci. 1970, 59, 1616–1620. [Google Scholar] [CrossRef]
- Chandorkar, Y.; Bhagat, R.K.; Madras, G.; Basu, B. Cross-Linked, Biodegradable, Cytocompatible Salicylic Acid Based Polyesters for Localized, Sustained Delivery of Salicylic Acid: An In Vitro Study. Biomacromolecules 2014, 15, 863–875. [Google Scholar] [CrossRef]
- Swietach, P.; Vaughan-Jones, R.D.; Harris, A.L.; Hulikova, A. The chemistry, physiology and pathology of pH in cancer. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130099. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dujić, T.; Causević, A.; Malenica, M. The Effects of Different Concentrations of Acetylsalicylic Acid on Proliferation and Viability of Lymphocytes in Cell Culture. Bosn. J. Basic Med. Sci. 2008, 8, 210–213. [Google Scholar] [CrossRef] [Green Version]
- Ponce, A.M.; Vujaskovic, Z.; Yuan, F.; Needham, D.; Dewhirst, M.W. Hyperthermia mediated liposomal drug delivery. Int. J. Hyperth. 2006, 22, 205–213. [Google Scholar] [CrossRef] [PubMed]










| P2MBA Graft (%) | Release Medium pH | Temperature (°C) | Model | Rate Constants | R2 |
|---|---|---|---|---|---|
| 7.6 | 5.5 | 30 | First order | 0.015 h−1 | 0.991 |
| 33.5 | 5.5 | 30 | Zero order | 0.170 mg/g h | 0.9696 |
| 7.6 | 5.5 | 37 | Zero order | 0.569 mg/g h | 0.994 |
| 33.5 | 5.5 | 37 | Zero order | 0.401 mg/g h | 0.978 |
| 7.6 | 7.4 | 30 | First order | 0.026 h−1 | 0.966 |
| 33.5 | 7.4 | 30 | Zero order | 0.469 mg/g h | 0.985 |
| 7.6 | 7.4 | 37 | First order | 0.037 h−1 | 0.967 |
| 33.5 | 7.4 | 37 | Zero order | 1.867 mg/g h | 0.9792 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cornejo-Bravo, J.M.; Palomino, K.; Palomino-Vizcaino, G.; Pérez-Landeros, O.M.; Curiel-Alvarez, M.; Valdez-Salas, B.; Bucio, E.; Magaña, H. Poly(N-vinylcaprolactam) and Salicylic Acid Polymeric Prodrug Grafted onto Medical Silicone to Obtain a Novel Thermo- and pH-Responsive Drug Delivery System for Potential Medical Devices. Materials 2021, 14, 1065. https://doi.org/10.3390/ma14051065
Cornejo-Bravo JM, Palomino K, Palomino-Vizcaino G, Pérez-Landeros OM, Curiel-Alvarez M, Valdez-Salas B, Bucio E, Magaña H. Poly(N-vinylcaprolactam) and Salicylic Acid Polymeric Prodrug Grafted onto Medical Silicone to Obtain a Novel Thermo- and pH-Responsive Drug Delivery System for Potential Medical Devices. Materials. 2021; 14(5):1065. https://doi.org/10.3390/ma14051065
Chicago/Turabian StyleCornejo-Bravo, José M., Kenia Palomino, Giovanni Palomino-Vizcaino, Oscar M. Pérez-Landeros, Mario Curiel-Alvarez, Benjamín Valdez-Salas, Emilio Bucio, and Héctor Magaña. 2021. "Poly(N-vinylcaprolactam) and Salicylic Acid Polymeric Prodrug Grafted onto Medical Silicone to Obtain a Novel Thermo- and pH-Responsive Drug Delivery System for Potential Medical Devices" Materials 14, no. 5: 1065. https://doi.org/10.3390/ma14051065