COVID-19: Multiorgan Dissemination of SARS-CoV-2 Is Driven by Pulmonary Factors
Abstract
:1. Introduction
2. Materials and Methods
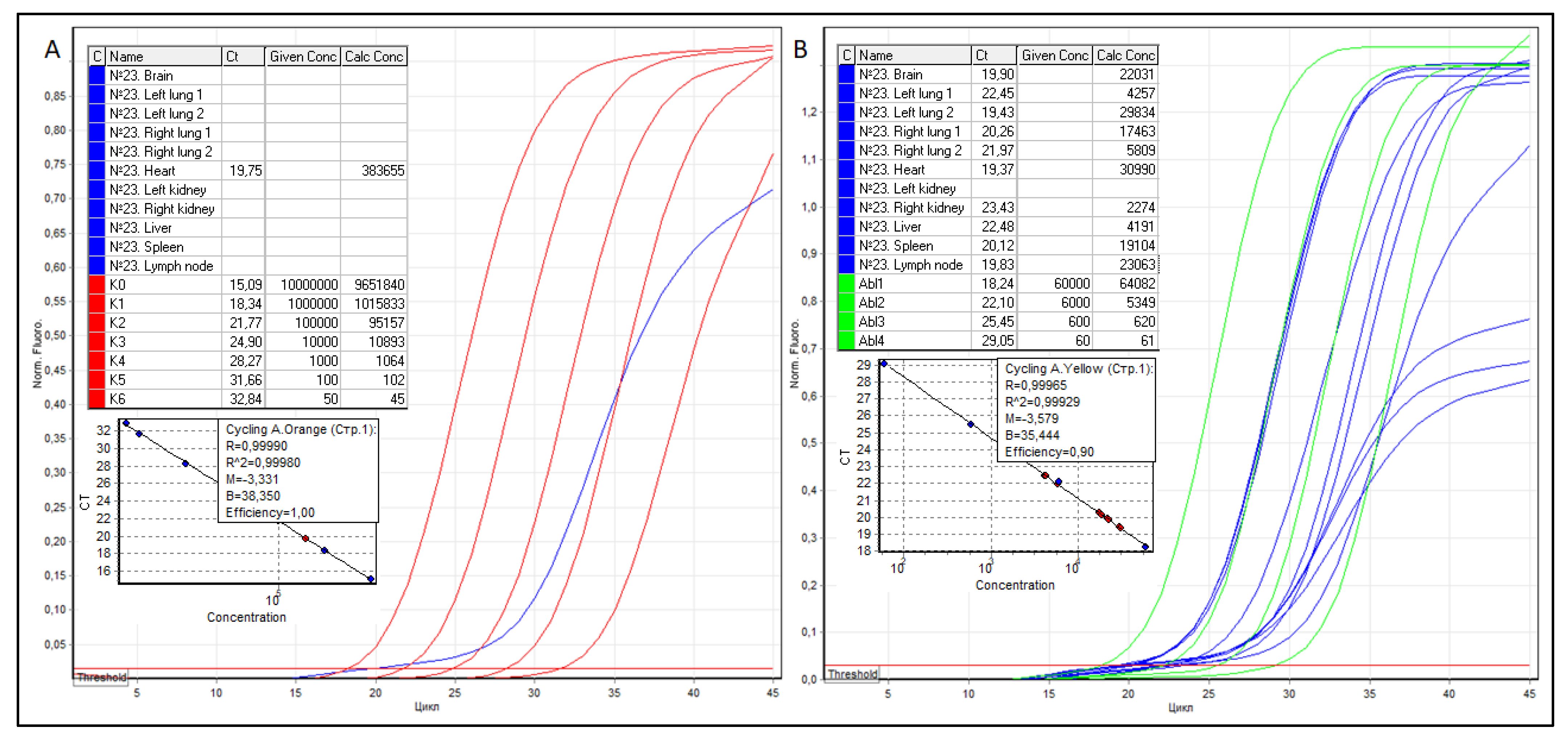
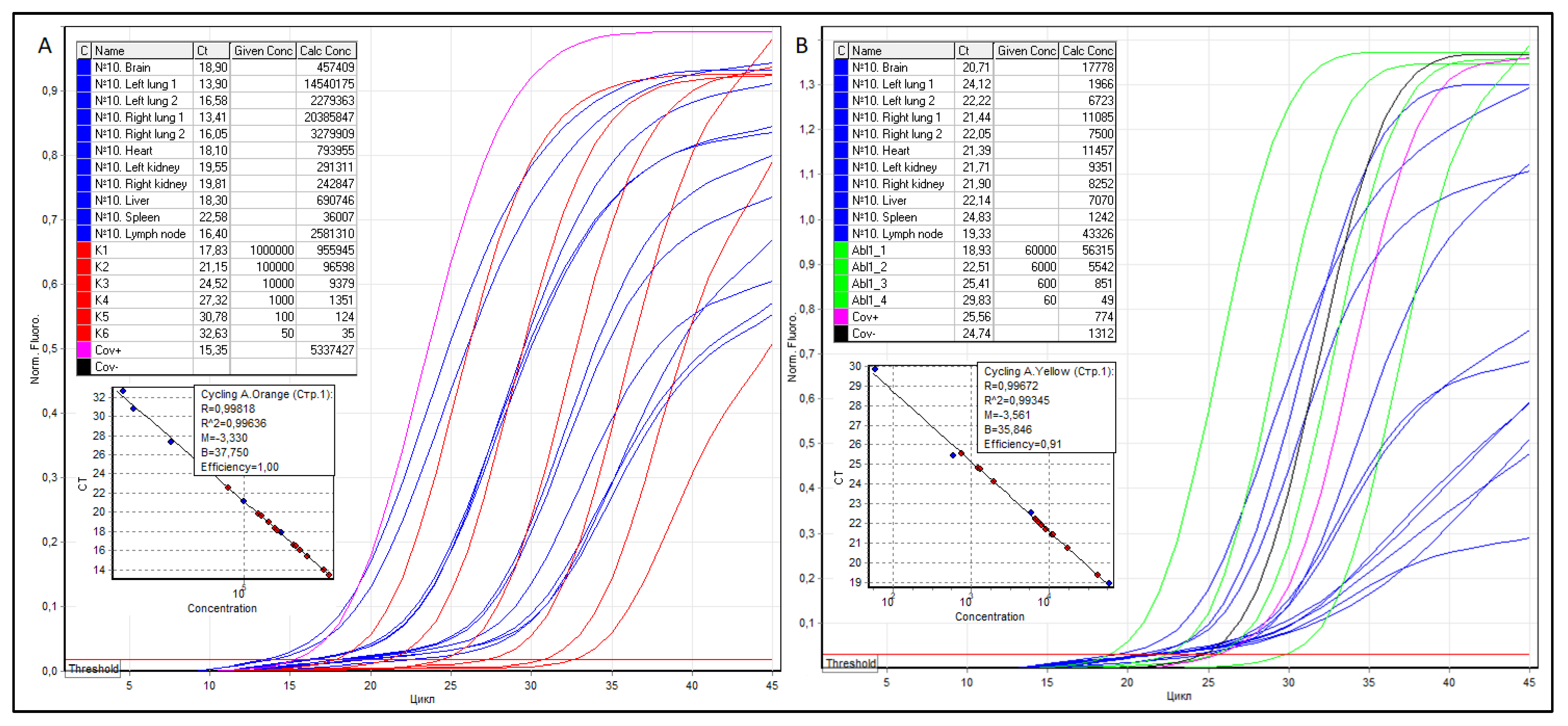
2.1. Quantitative RT PCR and SARS-CoV-2 VL Measuring Method in Tissues of Various Organs
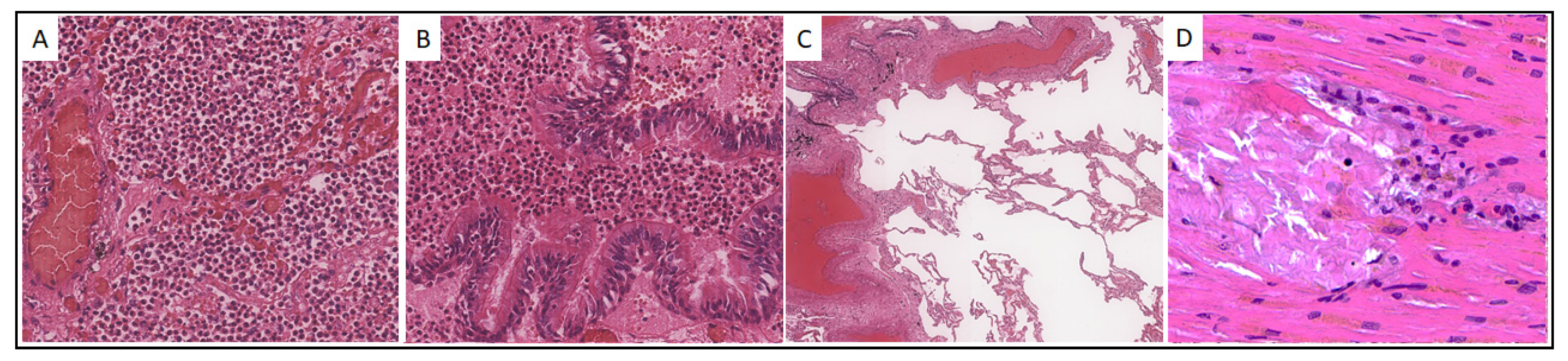
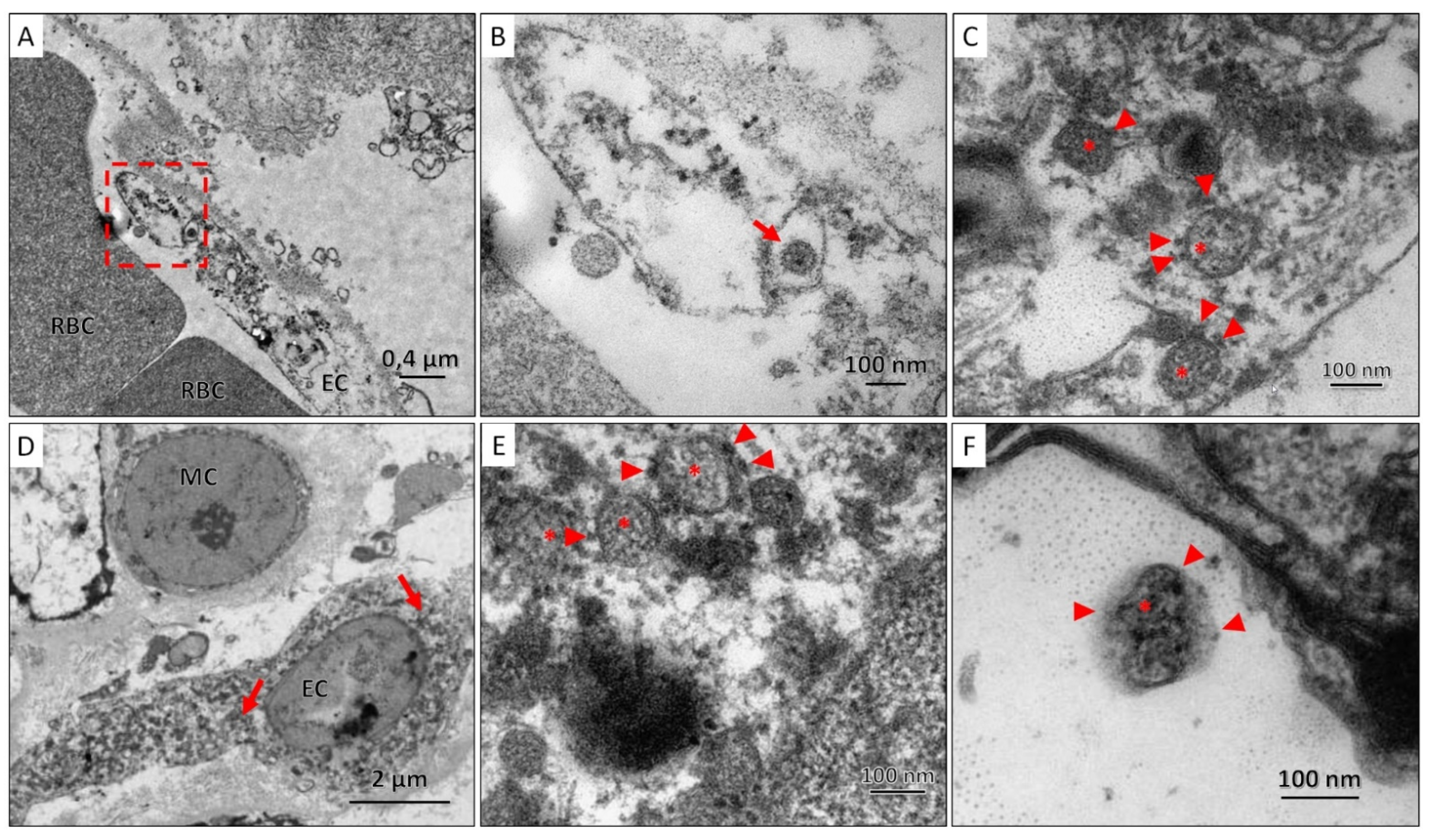
2.2. Immunohistochemical and Transmission Electron Microscopic Detection of SARS-CoV-2
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kgatle, M.M.; Lawal, I.O.; Mashabela, G.; Boshomane, T.M.G.; Koatale, P.C.; Mahasha, P.W.; Ndlovu, H.; Vorster, M.; Rodrigues, H.G.; Zeevaart, J.R.; et al. COVID-19 Is a Multi-Organ Aggressor: Epigenetic and Clinical Marks. Front. Immunol. 2021, 12, 752380. [Google Scholar] [CrossRef]
- Mokhtari, T.; Hassani, F.; Ghaffari, N.; Ebrahimi, B.; Yarahmadi, A.; Hassanzadeh, G. COVID-19 and multiorgan failure: A narrative review on potential mechanisms. J. Mol. Histol. 2020, 51, 613–628. [Google Scholar] [CrossRef] [PubMed]
- Gavriatopoulou, M.; Korompoki, E.; Fotiou, D.; Ntanasis-Stathopoulos, I.; Psaltopoulou, T.; Kastritis, E.; Terpos, E.; Dimopoulos, M.A. Organ-specific manifestations of COVID-19 infection. Clin. Exp. Med. 2020, 20, 493–506. [Google Scholar] [CrossRef]
- Loganathan, S.; Kuppusamy, M.; Wankhar, W.; Gurugubelli, K.R.; Mahadevappa, V.H.; Lepcha, L.; Choudhary, A.K. Angiotensin-converting enzyme 2 (ACE2): COVID 19 gate way to multiple organ failure syndromes. Respir. Physiol. Neurobiol. 2020, 283, 103548. [Google Scholar] [CrossRef] [PubMed]
- Sarkesh, A.; Sorkhabi, A.D.; Sheykhsaran, E.; Alinezhad, F.; Mohammadzadeh, N.; Hemmat, N.; Baghi, H.B. Extrapulmonary Clinical Manifestations in COVID-19 Patients. Am. J. Trop. Med. Hyg. 2020, 103, 1783–1796. [Google Scholar] [CrossRef]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA 2020, 323, 1612–1614. [Google Scholar] [CrossRef] [Green Version]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [Green Version]
- Varatharaj, A.; Thomas, N.; Ellul, M.; Davies, N.W.S.; Pollak, T.; Tenorio, E.L.; Sultan, M.; Easton, A.; Breen, G.; Zandi, M.; et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: A UK-wide surveillance study. Lancet Psychiatry 2020, 7, 875–882. [Google Scholar] [CrossRef]
- Helms, J.; Kremer, S.; Merdji, H.; Clere-Jehl, R.; Schenck, M.; Kummerlen, C.; Collange, O.; Boulay, C.; Fafi-Kremer, S.; Ohana, M.; et al. Neurologic Features in Severe SARS-CoV-2 Infection. N. Engl. J. Med. 2020, 382, 2268–2270. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, M.S.L.; Lima, C.F.C.; Pimentel, A.C.F.; Júnior, J.C.G.C.; Holanda, J.L.B. Multisystemic Infarctions in COVID-19: Focus on the Spleen. Eur. J. Case Rep. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Sztajnbok, J.; Brasil, L.M.C.D.R.; Romero, L.A.; Ribeiro, A.F.; Vidal, J.E.; Figueiredo-Mello, C.; Malaque, C.M.S.A. Splenic Infarction with Aortic Thrombosis in COVID-19. Am. J. Med. Sci. 2021, 362, 418–423. [Google Scholar] [CrossRef]
- Arjmand, B.; Alavi-Moghadam, S.; Roudsari, P.P.; Rezaei-Tavirani, M.; Rahim, F.; Gilany, K.; Mohamadi-Jahani, F.; Adibi, H.; Larijani, B. COVID-19 Pathology on Various Organs and Regenerative Medicine and Stem Cell-Based Interventions. Front. Cell Dev. Biol. 2021, 9, 675310. [Google Scholar] [CrossRef]
- Thakur, V.; Ratho, R.; Kumar, P.; Bhatia, S.; Bora, I.; Mohi, G.; Saxena, S.; Devi, M.; Yadav, D.; Mehariya, S. Multi-Organ Involvement in COVID-19: Beyond Pulmonary Manifestations. J. Clin. Med. 2021, 10, 446. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, N.R.; Phatak, S.; Sharma, V.R.; Agarwal, S.K. COVID-19 and thrombotic microangiopathies. Thromb. Res. 2021, 202, 191–198. [Google Scholar] [CrossRef]
- Colantuoni, A.; Martini, R.; Caprari, P.; Ballestri, M.; Capecchi, P.L.; Gnasso, A.; Presti, R.L.; Marcoccia, A.; Rossi, M.; Caimi, G. COVID-19 Sepsis and Microcirculation Dysfunction. Front. Physiol. 2020, 11, 747. [Google Scholar] [CrossRef] [PubMed]
- Puelles, V.G.; Lütgehetmann, M.; Lindenmeyer, M.T.; Sperhake, J.P.; Wong, M.N.; Allweiss, L.; Chilla, S.; Heinemann, A.; Wanner, N.; Liu, S.; et al. Multiorgan and Renal Tropism of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 590–592. [Google Scholar] [CrossRef]
- Wong, D.; Klinkhammer, B.; Djudjaj, S.; Villwock, S.; Timm, M.; Buhl, E.; Wucherpfennig, S.; Cacchi, C.; Braunschweig, T.; Knüchel-Clarke, R.; et al. Multisystemic Cellular Tropism of SARS-CoV-2 in Autopsies of COVID-19 Patients. Cells 2021, 10, 1900. [Google Scholar] [CrossRef]
- Malik, P.; Patel, U.; Mehta, D.; Patel, N.; Kelkar, R.; Akrmah, M.; Gabrilove, J.L.; Sacks, H. Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis. BMJ Evid.-Based Med. 2020, 26, 107–108. [Google Scholar] [CrossRef] [PubMed]
- Hudowenz, O.; Klemm, P.; Lange, U.; Rolf, A.; Schultheiss, H.-P.; Hamm, C.; Müller-Ladner, U.; Wegner, F. Case report of severe PCR-confirmed COVID-19 myocarditis in a European patient manifesting in mid-January 2020. Eur. Heart J. Case Rep. 2020, 4, 1–6. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, S.; Liu, H.; Li, W.; Lin, F.; Jiang, L.; Li, X.; Xu, P.; Zhang, L.; Zhao, L.; et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J. Hepatol. 2020, 73, 807–816. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Xiong, H.; Chen, H.; Li, Q.; Ruan, X.Z. Renal Injury by SARS-CoV-2 Infection: A Systematic Review. Kidney Dis. 2020, 7, 1–11. [Google Scholar] [CrossRef]
- Henry, B.M.; Aggarwal, G.; Wong, J.; Benoit, S.; Vikse, J.; Plebani, M.; Lippi, G. Lactate dehydrogenase levels predict coronavirus disease 2019 (COVID-19) severity and mortality: A pooled analysis. Am. J. Emerg. Med. 2020, 38, 1722–1726. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Xiong, Y.; Liu, H.; Niu, L.; Guo, J.; Liao, M.; Xiao, S.-Y. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020, 33, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Lindner, D.; Fitzek, A.; Bräuninger, H.; Aleshcheva, G.; Edler, C.; Meissner, K.; Scherschel, K.; Kirchhof, P.; Escher, F.; Schultheiss, H.-P.; et al. Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases. JAMA Cardiol. 2020, 5, 1281–1285. [Google Scholar] [CrossRef] [PubMed]
- Remmelink, M.; De Mendonça, R.; D’Haene, N.; De Clercq, S.; Verocq, C.; Lebrun, L.; Lavis, P.; Racu, M.-L.; Trépant, A.-L.; Maris, C.; et al. Unspecific post-mortem findings despite multiorgan viral spread in COVID-19 patients. Crit. Care 2020, 24, 495. [Google Scholar] [CrossRef]
- Lagana, S.M.; Kudose, S.; Iuga, A.C.; Lee, M.J.; Fazlollahi, L.; Remotti, H.E.; Del Portillo, A.; De Michele, S.; De Gonzalez, A.K.; Saqi, A.; et al. Hepatic pathology in patients dying of COVID-19: A series of 40 cases including clinical, histologic, and virologic data. Mod. Pathol. 2020, 33, 2147–2155. [Google Scholar] [CrossRef]
- Sekulic, M.; Harper, H.; Nezami, B.G.; Shen, D.L.; Sekulic, S.P.; Koeth, A.T.; Harding, C.V.; Gilmore, H.; Sadri, N. Molecular Detection of SARS-CoV-2 Infection in FFPE Samples and Histopathologic Findings in Fatal SARS-CoV-2 Cases. Am. J. Clin. Pathol. 2020, 154, 190–200. [Google Scholar] [CrossRef]
- Matschke, J.; Lütgehetmann, M.; Hagel, C.; Sperhake, J.P.; Schröder, A.S.; Edler, C.; Mushumba, H.; Fitzek, A.; Allweiss, L.; Dandri, M.; et al. Neuropathology of patients with COVID-19 in Germany: A post-mortem case series. Lancet Neurol. 2020, 19, 919–929. [Google Scholar] [CrossRef]
- Casagrande, M.; Fitzek, A.; Püschel, K.; Aleshcheva, G.; Schultheiss, H.-P.; Berneking, L.; Spitzer, M.S.; Schultheiss, M. Detection of SARS-CoV-2 in Human Retinal Biopsies of Deceased COVID-19 Patients. Ocul. Immunol. Inflamm. 2020, 28, 721–725. [Google Scholar] [CrossRef] [PubMed]
- Guerini-Rocco, E.; Taormina, S.V.; Vacirca, D.; Ranghiero, A.; Rappa, A.; Fumagalli, C.; Maffini, F.; Rampinelli, C.; Galetta, D.; Tagliabue, M.; et al. SARS-CoV-2 detection in formalin-fixed paraffin-embedded tissue specimens from surgical resection of tongue squamous cell carcinoma. J. Clin. Pathol. 2020, 73, 754–757. [Google Scholar] [CrossRef]
- Bradley, B.T.; Maioli, H.; Johnston, R.; Chaudhry, I.; Fink, S.L.; Xu, H.; Najafian, B.; Deutsch, G.; Lacy, J.M.; Williams, T.; et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: A case series. Lancet 2020, 396, 320–332. [Google Scholar] [CrossRef]
- Adachi, T.; Chong, J.-M.; Nakajima, N.; Sano, M.; Yamazaki, J.; Miyamoto, I.; Nishioka, H.; Akita, H.; Sato, Y.; Kataoka, M.; et al. Clinicopathologic and Immunohistochemical Findings from Autopsy of Patient with COVID-19, Japan. Emerg. Infect. Dis. 2020, 26, 2157–2161. [Google Scholar] [CrossRef]
- Martines, R.B.; Ritter, J.M.; Matkovic, E.; Gary, J.; Bollweg, B.C.; Bullock, H.; Goldsmith, C.S.; Silva-Flannery, L.; Seixas, J.N.; Reagan-Steiner, S.; et al. Pathology and Pathogenesis of SARS-CoV-2 Associated with Fatal Coronavirus Disease, United States. Emerg. Infect. Dis. 2020, 26, 2005–2015. [Google Scholar] [CrossRef] [PubMed]
- Massoth, L.R.; Desai, N.; Szabolcs, A.; Harris, C.K.; Neyaz, A.; Crotty, R.; Chebib, I.; Rivera, M.N.; Sholl, L.M.; Stone, J.R.; et al. Comparison of RNA In Situ Hybridization and Immunohistochemistry Techniques for the Detection and Localization of SARS-CoV-2 in Human Tissues. Am. J. Surg. Pathol. 2020, 45, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Schurink, B.; Roos, E.; Radonic, T.; Barbe, E.; Bouman, C.S.C.; de Boer, H.H.; de Bree, G.J.; Bulle, E.B.; Aronica, E.M.; Florquin, S.; et al. Viral presence and immunopathology in patients with lethal COVID-19: A prospective autopsy cohort study. Lancet Microbe 2020, 1, e290–e299. [Google Scholar] [CrossRef]
- Zhao, C.L.; Rapkiewicz, A.; Maghsoodi-Deerwester, M.; Gupta, M.; Cao, W.; Palaia, T.; Zhou, J.; Ram, B.; Vo, D.; Rafiee, B.; et al. Pathological findings in the postmortem liver of patients with coronavirus disease 2019 (COVID-19). Hum. Pathol. 2020, 109, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef]
- Xiang, Q.; Feng, Z.; Diao, B.; Tu, C.; Qiao, Q.; Yang, H.; Zhang, Y.; Wang, G.; Wang, H.; Wang, C.; et al. SARS-CoV-2 Induces Lymphocytopenia by Promoting Inflammation and Decimates Secondary Lymphoid Organs. Front. Immunol. 2021, 12, 661052. [Google Scholar] [CrossRef]
- Wang, C.; Xie, J.; Zhao, L.; Fei, X.; Zhang, H.; Tan, Y.; Nie, X.; Zhou, L.; Liu, Z.; Ren, Y.; et al. Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients. EBioMedicine 2020, 57, 102833. [Google Scholar] [CrossRef]
- Haslbauer, J.D.; Matter, M.S.; Stalder, A.K.; Tzankov, A. Histomorphological patterns of regional lymph nodes in COVID-19 lungs. Der Pathol. 2021, 42, 89–97. [Google Scholar] [CrossRef]
- Grimes, Z.; Bryce, C.; Sordillo, E.M.; Gordon, R.E.; Reidy, J.; Mondolfi, A.E.P.; Fowkes, M. Fatal Pulmonary Thromboembolism in SARS-CoV-2-Infection. Cardiovasc. Pathol. 2020, 48, 107227. [Google Scholar] [CrossRef]
- Carsana, L.; Sonzogni, A.; Nasr, A.; Rossi, R.S.; Pellegrinelli, A.; Zerbi, P.; Rech, R.; Colombo, R.; Antinori, S.; Corbellino, M.; et al. Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: A two-centre descriptive study. Lancet Infect. Dis. 2020, 20, 1135–1140. [Google Scholar] [CrossRef]
- Wu, M.A.; Fossali, T.; Pandolfi, L.; Carsana, L.; Ottolina, D.; Frangipane, V.; Rech, R.; Tosoni, A.; Lopez, G.; Agarossi, A.; et al. Hypoalbuminemia in COVID-19: Assessing the hypothesis for underlying pulmonary capillary leakage. J. Intern. Med. 2021, 289, 861–872. [Google Scholar] [CrossRef] [PubMed]
- Dolhnikoff, M.; Ferranti, J.F.; Monteiro, R.; Duarte-Neto, A.N.; Gomes-Gouvêa, M.S.; Degaspare, N.V.; Delgado, A.F.; Fiorita, C.M.; Leal, G.N.; Rodrigues, R.M.; et al. SARS-CoV-2 in cardiac tissue of a child with COVID-19-related multisystem inflammatory syndrome. Lancet Child Adolesc. Health 2020, 4, 790–794. [Google Scholar] [CrossRef]
- Tavazzi, G.; Pellegrini, C.; Maurelli, M.; Belliato, M.; Sciutti, F.; Bottazzi, A.; Sepe, P.A.; Resasco, T.; Camporotondo, R.; Bruno, R.; et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur. J. Heart Fail. 2020, 22, 911–915. [Google Scholar] [CrossRef] [Green Version]
- Farkash, E.A.; Wilson, A.M.; Jentzen, J.M. Ultrastructural Evidence for Direct Renal Infection with SARS-CoV-2. J. Am. Soc. Nephrol. 2020, 31, 1683–1687. [Google Scholar] [CrossRef] [PubMed]
- Dahdouh, E.; Lázaro-Perona, F.; Romero-Gómez, M.P.; Mingorance, J.; García-Rodriguez, J. Ct values from SARS-CoV-2 diagnostic PCR assays should not be used as direct estimates of viral load. J. Infect. 2020, 82, 414–451. [Google Scholar] [CrossRef] [PubMed]
- Schnuriger, A.; Perrier, M.; Marinho, V.; Michel, Y.; Saloum, K.; Boukli, N.; Lambert-Niclot, S.; Amiel, C.; Fofana, D.B.; Gozlan, J.; et al. Caution in interpretation of SARS-CoV-2 quantification based on RT-PCR cycle threshold value. Diagn. Microbiol. Infect. Dis. 2021, 100, 115366. [Google Scholar] [CrossRef]
- Rhoads, D.; Peaper, D.R.; She, R.C.; Nolte, F.S.; Wojewoda, C.M.; Anderson, N.W.; Pritt, B.S. College of American Pathologists (CAP) Microbiology Committee Perspective: Caution Must Be Used in Interpreting the Cycle Threshold (Ct) Value. Clin. Infect. Dis. 2020, 72, e685–e686. [Google Scholar] [CrossRef]
- Abdullaev, A.; Odilov, A.; Ershler, M.; Volkov, A.; Lipina, T.; Gasanova, T.; Lebedin, Y.; Babichenko, I.; Sudarikov, A. Viral Load and Patterns of SARS-CoV-2 Dissemination to the Lungs, Mediastinal Lymph Nodes, and Spleen of Patients with COVID-19 Associated Lymphopenia. Viruses 2021, 13, 1410. [Google Scholar] [CrossRef]
- Hanley, B.; Naresh, K.; Roufosse, C.; Nicholson, A.G.; Weir, J.; Cooke, G.S.; Thursz, M.; Manousou, P.; Corbett, R.; Goldin, R.; et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe 2020, 1, e245–e253. [Google Scholar] [CrossRef]
- Schaefer, I.-M.; Padera, R.F.; Solomon, I.H.; Kanjilal, S.; Hammer, M.M.; Hornick, J.L.; Sholl, L.M. In situ detection of SARS-CoV-2 in lungs and airways of patients with COVID-19. Mod. Pathol. 2020, 33, 2104. [Google Scholar] [CrossRef]
- Deinhardt-Emmer, S.; Wittschieber, D.; Sanft, J.; Kleemann, S.; Elschner, S.; Haupt, K.F.; Vau, V.; Häring, C.; Rödel, J.; Henke, A.; et al. Early postmortem mapping of SARS-CoV-2 RNA in patients with COVID-19 and the correlation with tissue damage. eLife 2021, 10, e60361. [Google Scholar] [CrossRef] [PubMed]
- Sauter, J.L.; Baine, M.K.; Butnor, K.J.; Buonocore, D.J.; Chang, J.C.; Jungbluth, A.A.; Szabolcs, M.J.; Morjaria, S.; Mount, S.L.; Rekhtman, N.; et al. Insights into pathogenesis of fatal COVID-19 pneumonia from histopathology with immunohistochemical and viral RNA studies. Histopathology 2020, 77, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Schaller, T.; Hirschbühl, K.; Burkhardt, K.; Braun, G.; Trepel, M.; Märkl, B.; Claus, R. Postmortem Examination of Patients With COVID-19. JAMA 2020, 323, 2518–2520. [Google Scholar] [CrossRef]
- Magleby, R.; Westblade, L.F.; Trzebucki, A.; Simon, M.S.; Rajan, M.; Park, J.; Goyal, P.; Safford, M.M.; Satlin, M.J. Impact of SARS-CoV-2 Viral Load on Risk of Intubation and Mortality Among Hospitalized Patients with Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 73, e4197–e4205. [Google Scholar] [CrossRef]
- Pujadas, E.; Chaudhry, F.; McBride, R.; Richter, F.; Zhao, S.; Wajnberg, A.; Nadkarni, G.; Glicksberg, B.S.; Houldsworth, J.; Cordon-Cardo, C. SARS-CoV-2 viral load predicts COVID-19 mortality. Lancet Respir. Med. 2020, 8, e70. [Google Scholar] [CrossRef]
- Rao, S.N.; Manissero, D.; Steele, V.R.; Pareja, J. A Systematic Review of the Clinical Utility of Cycle Threshold Values in the Context of COVID-19. Infect. Dis. Ther. 2020, 9, 573–586. [Google Scholar] [CrossRef] [PubMed]
- Gauchotte, G.; Venard, V.; Segondy, M.; Cadoz, C.; Esposito-Fava, A.; Barraud, D.; Louis, G. SARS-Cov-2 fulminant myocarditis: An autopsy and histopathological case study. Int. J. Leg. Med. 2021, 135, 577–581. [Google Scholar] [CrossRef]
- Chau, V.Q.; Giustino, G.; Mahmood, K.; Oliveros, E.; Neibart, E.; Oloomi, M.; Moss, N.; Mitter, S.S.; Contreras, J.P.; Croft, L.; et al. Cardiogenic Shock and Hyperinflammatory Syndrome in Young Males With COVID-19. Circ. Hear. Fail. 2020, 13, e007485. [Google Scholar] [CrossRef]
- Pérez, A.; Torregrosa, I.; D’Marco, L.; Juan, I.; Terradez, L.; Solís, M.; Moncho, F.; Carda-Batalla, C.; Forner, M.; Gorriz, J. IgA-Dominant Infection-Associated Glomerulonephritis Following SARS-CoV-2 Infection. Viruses 2021, 13, 587. [Google Scholar] [CrossRef] [PubMed]
- Diao, B.; Wang, C.; Wang, R.; Feng, Z.; Zhang, J.; Yang, H.; Tan, Y.; Wang, H.; Wang, C.; Liu, L.; et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection. Nat. Commun. 2021, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Stahl, K.; Bräsen, J.H.; Hoeper, M.M.; David, S. Direct evidence of SARS-CoV-2 in gut endothelium. Intensiv. Care Med. 2020, 46, 2081–2082. [Google Scholar] [CrossRef]
- Martin-Cardona, A.; Trull, J.L.; Albero-González, R.; Beser, M.P.; Andújar, X.; Ruiz-Ramirez, P.; Tur-Martínez, J.; Ferrer, C.; Izquierdo, J.A.D.M.; Pérez-Madrigal, A.; et al. SARS-CoV-2 identified by transmission electron microscopy in lymphoproliferative and ischaemic intestinal lesions of COVID-19 patients with acute abdominal pain: Two case reports. BMC Gastroenterol. 2021, 21, 334. [Google Scholar] [CrossRef]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- Fox, S.E.; Li, G.; Akmatbekov, A.; Harbert, J.L.; Lameira, F.S.; Brown, J.Q.; Heide, R.S.V. Unexpected Features of Cardiac Pathology in COVID-19 Infection. Circulation 2020, 142, 1123–1125. [Google Scholar] [CrossRef] [PubMed]
- Colmenero, I.; Santonja, C.; Alonso-Riaño, M.; Noguera-Morel, L.; Hernández-Martín, A.; Andina, D.; Wiesner, T.; Rodríguez-Peralto, J.; Requena, L.; Torrelo, A. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: Histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br. J. Dermatol. 2020, 183, 729–737. [Google Scholar] [CrossRef]
- Zhang, L.; Zhou, L.; Bao, L.; Liu, J.; Zhu, H.; Lv, Q.; Liu, R.; Chen, W.; Tong, W.; Wei, Q.; et al. SARS-CoV-2 crosses the blood–brain barrier accompanied with basement membrane disruption without tight junctions alteration. Signal Transduct. Target. Ther. 2021, 6, 337. [Google Scholar] [CrossRef]
- Pirisi, M.; Rigamonti, C.; D’Alfonso, S.; Nebuloni, M.; Fanni, D.; Gerosa, C.; Orrù, G.; Venanzi Rullo, E.; Pavone, P.; Faa, G.; et al. Liver Infection and COVID-19: The Electron Microscopy Proof and Revision of the Literature. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2146–2151. [Google Scholar] [CrossRef]
- Qadir, M.M.F.; Bhondeley, M.; Beatty, W.; Gaupp, D.D.; Doyle-Meyers, L.A.; Fischer, T.; Bandyopadhyay, I.; Blair, R.V.; Bohm, R.; Rappaport, J.; et al. SARS-CoV-2 infection of the pancreas promotes thrombofibrosis and is associated with new-onset diabetes. JCI Insight 2021, 6. [Google Scholar] [CrossRef] [PubMed]
- Fodor, A.; Tiperciuc, B.; Login, C.; Orasan, O.H.; Lazar, A.L.; Buchman, C.; Hanghicel, P.; Sitar-Taut, A.; Suharoschi, R.; Vulturar, R.; et al. Endothelial Dysfunction, Inflammation, and Oxidative Stress in COVID-19—Mechanisms and Therapeutic Targets. Oxidative Med. Cell. Longev. 2021, 2021, 8671713. [Google Scholar] [CrossRef] [PubMed]
- Noris, M.; Benigni, A.; Remuzzi, G. The case of complement activation in COVID-19 multiorgan impact. Kidney Int. 2020, 98, 314–322. [Google Scholar] [CrossRef]
- Chornenkyy, Y.; Mejia-Bautista, M.; Brucal, M.; Blanke, T.; Dittmann, D.; Yeldandi, A.; Boike, J.R.; Lomasney, J.W.; Nayar, R.; Jennings, L.J.; et al. Liver Pathology and SARS-CoV-2 Detection in Formalin-Fixed Tissue of Patients With COVID-19. Am. J. Clin. Pathol. 2021, 155, 802–814. [Google Scholar] [CrossRef] [PubMed]
- El Jamal, S.M.; Pujadas, E.; Ramos, I.; Bryce, C.; Grimes, Z.M.; Amanat, F.; Tsankova, N.M.; Mussa, Z.; Olson, S.; Salem, F.; et al. Tissue-based SARS-CoV-2 detection in fatal COVID-19 infections: Sustained direct viral-induced damage is not necessary to drive disease progression. Hum. Pathol. 2021, 114, 110–119. [Google Scholar] [CrossRef]


| # | Sex | Age | Time 1 | Phase of DAD 2/Other Pulmonary Findings | SARS-CoV-2 VL Level by Organs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lungs 3 | LN 4 | Heart | Spleen | Liver | Kidneys 5 | Brain | |||||
| Group 1: (n = 2) SARS-CoV-2 has not been detected | |||||||||||
| 7 | M | 62 | 2 | Proliferative | 0 | 0 | 0 | 0 | 0 | - | 0 |
| 17 | F | 77 | 15 | Proliferative/emphysema | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Group 2: (n = 11) SARS-CoV-2 mono-organ dissemination | |||||||||||
| 23 | M | 90 | 9 | Bronchopneumonia with fibrosis | 0 | 0 | 1238 | 0 | 0 | 0 | 0 |
| 34 | F | 73 | 23 | Bronchopneumonia | 27 | 0 | 0 | 0 | 0 | 0 | 0 |
| 29 | F | 79 | 24 | Bronchopneumonia | 38 | 0 | 0 | 0 | 0 | 0 | 0 |
| 22 | M | 90 | 10 | Proliferative | 63 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15 | M | 68 | 19 | Bronchopneumonia | 190 | 0 | 0 | 0 | 0 | 0 | 0 |
| 31 | F | 78 | 10 | Proliferative | 208 | 0 | 0 | 0 | 0 | 0 | 0 |
| 20 | F | 85 | 23 | Bronchopneumonia | 270 | 0 | 0 | 0 | 0 | 0 | 0 |
| 8 | M | 64 | 19 | Proliferative | 677 | 0 | 0 | 0 | 0 | - | 0 |
| 32 | M | 85 | 10 | Proliferative | 694 | 0 | 0 | 0 | 0 | 0 | 0 |
| 11 | M | 84 | 17 | Proliferative | 706 | - | 0 | n/a | 0 | - | 0 |
| 14 | M | 80 | 10 | Proliferative | 1952 | 0 | - | 0 | - | - | 0 |
| Group 3: (n = 23) SARS-CoV-2 multi-organ dissemination | |||||||||||
| 5 | F | 73 | 18 | Proliferative/bronchopneumonia with hemorrhages | 18 | 0 | 0 | 0 | 70 | 0 | 0 |
| 6 | M | 66 | 27 | Hemorrhages and fibrosis | 313 | 0 | 0 | 0 | 7 | 0 | 0 |
| 33 | F | 86 | 3 | Proliferative | 810 | 96 | 0 | 0 | 0 | 0 | 0 |
| 13 | F | 71 | 1 | Exudative | 834 | 1318 | 974 | 629 | 602 | - | 718 |
| 35 | F | 73 | 2 | Proliferative | 910 | 215 | 197 | 0 | 0 | 0 | 0 |
| 21 | M | 67 | 13 | Proliferative | 982 | 180 | 0 | 0 | 0 | 0 | 0 |
| 30 | M | 61 | 5 | Proliferative/bronchopneumonia | 1002 | 237 | 0 | 0 | 0 | 0 | 0 |
| 1 | M | 52 | 1 | Proliferative/emphysema | 1016 | 112 | 0 | 0 | 0 | 0 | 0 |
| 25 | M | 74 | 22 | Proliferative | 1032 | 825 | 0 | 0 | 0 | 0 | n/a |
| 16 | M | 67 | 9 | Proliferative/bronchopneumonia with hemorrhages | 2657 | 1110 | 0 | 0 | 0 | 0 | 0 |
| 4 | M | 76 | 5 | Exudative and early proliferative/hemorrhages | 4909 | 195 | 1267 | 71 | 47 | 52 | 0 |
| 19 | M | 84 | 24 | Exudative | 7476 | 1807 | 0 | 0 | 0 | 0 | 0 |
| 9 | F | 72 | 12 | Exudative/bronchopneumonia | 12,116 | 3801 | 2223 | - | 0 | 0 | 0 |
| 28 | F | 95 | 7 | Exudative | 14,522 | 839 | 392 | 34 | 425 | 0 | 0 |
| 3 | M | 84 | 11 | Exudative/bronchopneumonia with necrosis | 14,937 | 162 | 3733 | 9 | 160 | 0 | 0 |
| 27 | M | 84 | 16 | Exudative | 16,867 | 1180 | 0 | 1320 | 522 | 0 | n/a |
| 18 | M | 85 | 16 | Exudative | 17,817 | n/a | 270 | 218 | 0 | - | 0 |
| 36 | M | 73 | 2 | Exudative | 18,219 | 2691 | 409 | 181 | 0 | 83 | 0 |
| 26 | F | 93 | 7 | Exudative | 27,349 | 1629 | 1222 | 213 | 256 | 878 | 0 |
| 2 | F | 86 | 25 | Exudative | 73,214 | 789 | 761 | 72 | 40 | 126 | 782 |
| 12 | F | 85 | 7 | Exudative | 151,183 | 513 | 538 | 1891 | 980 | - | 0 |
| 24 | F | 76 | 11 | Exudative | 159,217 | 11,586 | 2418 | 551 | 0 | 1291 | n/a |
| 10 | M | 61 | 6 | Exudative | 250,281 | 5958 | 6930 | 2899 | 9770 | 3029 | 2573 |
| # | VL Heart | CPK, IU/L | VL Liver | AST, IU/L | ALT, IU/L | LDH, U/L | ALP, IU/L | VL Kidney | Cr, μmoles/L |
|---|---|---|---|---|---|---|---|---|---|
| NR | 20–200 | 8–33 | 4–36 | 40–280 | 44–147 | 61.9–114.9 | |||
| Group 1. SARS-CoV-2 has not been detected | |||||||||
| 7 | 0 | 485 | 0 | 149 | 121 | 490 | 307 | - | 415 |
| 17 | 0 | 71.3 | 0 | 31.2 | 17.1 | 207.4 | - | 0 | 114.7 |
| Group 2. SARS-CoV-2 mono-organ dissemination | |||||||||
| 23 | 1238 | 154 | 0 | 46 | 33 | 323 | 192 | 0 | 194 |
| 22 | 0 | - | 0 | 25 | 11 | 395 | 189 | 0 | 309 |
| 15 | 0 | - | 0 | 26 | 26 | 555 | 162 | 0 | 103 |
| 20 | 0 | - | 0 | 62.2 | 42.5 | - | - | 0 | 185.3 |
| 8 | 0 | 775 | 0 | 72.5 | 87.35 | 836 | - | 0 | 96.41 |
| 11 | 0 | 83 | 0 | 978 | 503 | 2058 | 239 | 0 | 82 |
| 14 | 0 | - | - | 58 | 41 | 564 | - | 0 | 109 |
| Group 3. SARS-CoV-2 multi-organ dissemination | |||||||||
| 5 | 0 | 1007 | 70 | 93 | 35 | - | 337 | 0 | 228 |
| 6 | 0 | 656.6 | 7 | 33.2 | 42.6 | 396.7 | - | 0 | 98.7 |
| 13 | 974 | 290.8 | 0 | 47.1 | 20.5 | 358.2 | - | - | 83.6 |
| 21 | 0 | 197 | 0 | 73.9 | 58.7 | 637.9 | - | 0 | 129.7 |
| 1 | 0 | - | 0 | 813 | 390 | - | - | 0 | 296.1 |
| 25 | 0 | 145.4 | 0 | 31 | 31.7 | 649.5 | - | 0 | 156.2 |
| 16 | 0 | - | 0 | 170.5 | 56.1 | - | - | 0 | 104.6 |
| 4 | 1267 | 722 | 47 | 73 | 73 | 626 | - | 52 | 194 |
| 19 | 0 | 641.4 | 0 | 140.8 | 81.7 | 493.3 | - | 0 | 283 |
| 9 | 2223 | 29 | 0 | 18 | 14 | - | - | 0 | 75.2 |
| 3 | 3733 | - | 160 | 75 | - | - | - | 0 | 122 |
| 27 | 0 | - | 522 | 35 | 22 | - | - | 0 | 216 |
| 18 | 270 | 260 | 0 | 23 | 21 | 289 | 48 | - | 89.6 |
| 26 | 1222 | 495 | 256 | 43 | 18 | 428 | 206 | 878 | 353 |
| 2 | 761 | 1327 | 40 | 54 | 13 | - | - | 126 | 364.4 |
| 12 | 538 | 735.4 | 980 | 594.6 | 786.6 | 902.7 | - | - | 193.6 |
| 24 | 2418 | - | 0 | 16,3 | 8.6 | - | - | 1291 | 137.4 |
| 10 | 6930 | 609 | 9770 | 71 | 62 | 767 | - | 3029 | 199 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Odilov, A.; Volkov, A.; Abdullaev, A.; Gasanova, T.; Lipina, T.; Babichenko, I. COVID-19: Multiorgan Dissemination of SARS-CoV-2 Is Driven by Pulmonary Factors. Viruses 2022, 14, 39. https://doi.org/10.3390/v14010039
Odilov A, Volkov A, Abdullaev A, Gasanova T, Lipina T, Babichenko I. COVID-19: Multiorgan Dissemination of SARS-CoV-2 Is Driven by Pulmonary Factors. Viruses. 2022; 14(1):39. https://doi.org/10.3390/v14010039
Chicago/Turabian StyleOdilov, Akmaljon, Alexey Volkov, Adhamjon Abdullaev, Tatiana Gasanova, Tatiana Lipina, and Igor Babichenko. 2022. "COVID-19: Multiorgan Dissemination of SARS-CoV-2 Is Driven by Pulmonary Factors" Viruses 14, no. 1: 39. https://doi.org/10.3390/v14010039
APA StyleOdilov, A., Volkov, A., Abdullaev, A., Gasanova, T., Lipina, T., & Babichenko, I. (2022). COVID-19: Multiorgan Dissemination of SARS-CoV-2 Is Driven by Pulmonary Factors. Viruses, 14(1), 39. https://doi.org/10.3390/v14010039






