Transiently Transfected Mammalian Cell Cultures: An Adaptable and Effective Platform for Virus-like Particle-Based Vaccines against Foot-and-Mouth Disease Virus
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plasmid Constructions
2.2. Mammalian Cell Culture Transfections
2.3. Transmission Electron Microscopy
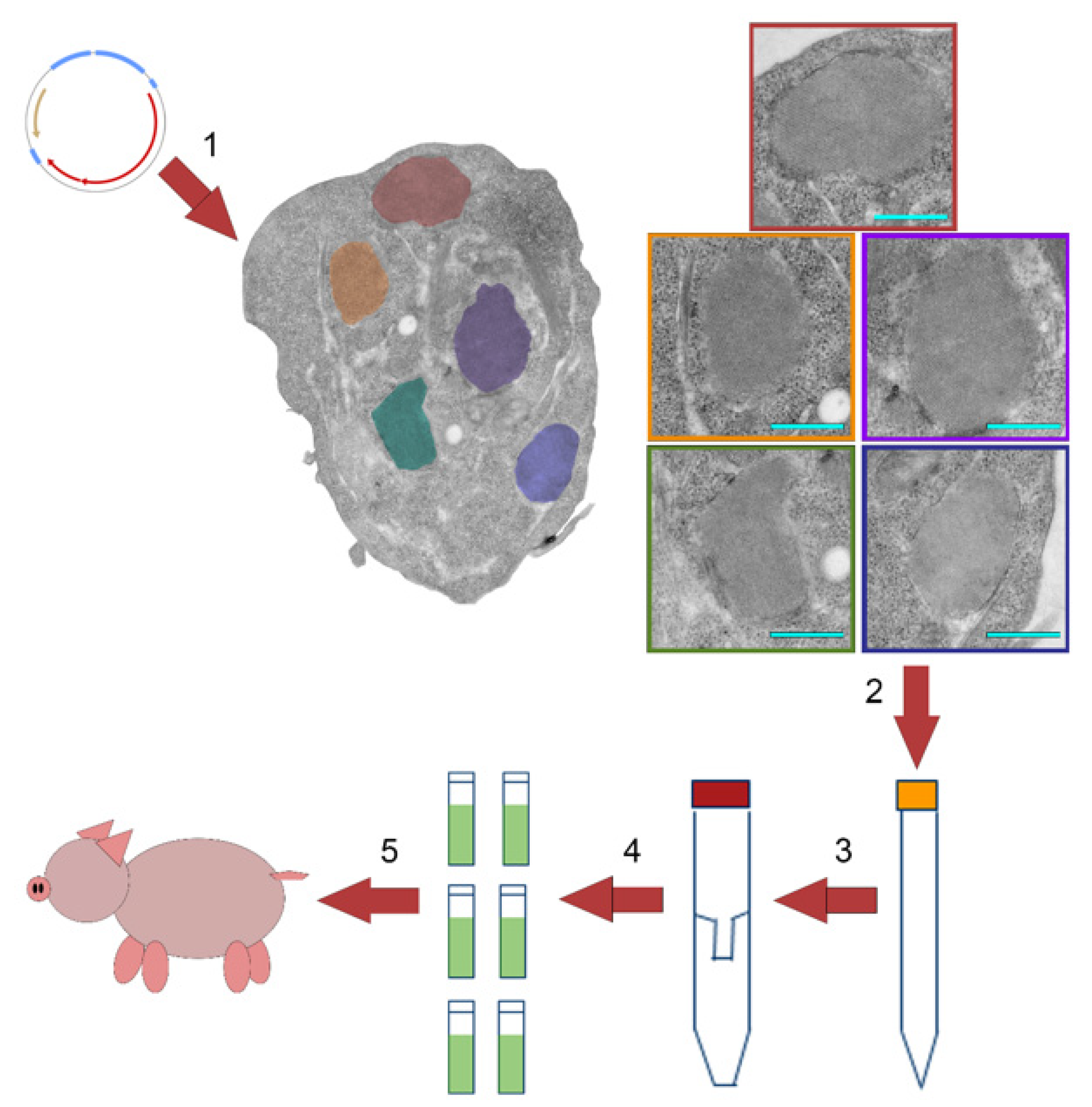
2.4. Preparation of mamVLP Vaccine
2.5. Cesium Chloride Gradients
2.6. Swine Studies
2.7. Cattle Study
2.8. Virus-Neutralizing Test Antibody Titer Assay
2.9. Viremia Detection
2.10. FMDV Nonstructural Protein ELISA
3. Results
3.1. Production Using Transiently Transfected Mammalian Cell Culture
3.2. Vaccination and Challenge of Swine and Cattle
3.3. Platform Adaptability
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mayr, G.A.; Chinsangaram, J.; Grubman, M.J. Development of replication-defective adenovirus serotype 5 containing the capsid and 3C protease coding regions of foot-and-mouth disease virus as a vaccine candidate. Virology 1999, 263, 496–506. [Google Scholar] [CrossRef] [Green Version]
- Gullberg, M.; Muszynski, B.; Organtini, L.J.; Ashley, R.E.; Hafenstein, S.L.; Belsham, G.J.; Polacek, C. Assembly and characterization of foot-and-mouth disease virus empty capsid particles expressed within mammalian cells. J. Gen. Virol. 2013, 94, 1769–1779. [Google Scholar] [CrossRef]
- Knight-Jones, T.J.; Robinson, L.; Charleston, B.; Rodriguez, L.L.; Gay, C.G.; Sumption, K.J.; Vosloo, W. Global Foot-and-Mouth Disease Research Update and Gap Analysis: 1—Overview of Global Status and Research Needs. Transbound. Emerg. Dis. 2016, 63 (Suppl. 1), 3–13. [Google Scholar] [CrossRef]
- Jamal, S.M.; Belsham, G.J. Foot-and-mouth disease: Past, present and future. Vet. Res. 2013, 44, 116. [Google Scholar] [CrossRef] [Green Version]
- Anderson, I. Foot and Mouth Disease 2007: A Review and Lessons Learned; Report to the Prime Minister and the Secretary of State for Environment Food and Rural Affairs; The Stationery Office: London, UK, 2008. [Google Scholar]
- Domingo, E.; Escarmis, C.; Baranowski, E.; Ruiz-Jarabo, C.M.; Carrillo, E.; Nunez, J.I.; Sobrino, F. Evolution of foot-and-mouth disease virus. Virus Res. 2003, 91, 47–63. [Google Scholar] [CrossRef]
- Mahapatra, M.; Parida, S. Foot and mouth disease vaccine strain selection: Current approaches and future perspectives. Expert Rev. Vaccines 2018, 17, 577–591. [Google Scholar] [CrossRef]
- Medina, G.N.; Montiel, N.; Diaz-San Segundo, F.; Sturza, D.; Ramirez-Medina, E.; Grubman, M.J.; de los Santos, T. Evaluation of a Fiber-Modified Adenovirus Vector Vaccine against Foot-and-Mouth Disease in Cattle. Clin. Vaccine Immunol. 2015, 23, 125–136. [Google Scholar] [CrossRef] [Green Version]
- Schutta, C.; Barrera, J.; Pisano, M.; Zsak, L.; Grubman, M.J.; Mayr, G.A.; Moraes, M.P.; Kamicker, B.J.; Brake, D.A.; Ettyreddy, D.; et al. Multiple efficacy studies of an adenovirus-vectored foot-and-mouth disease virus serotype A24 subunit vaccine in cattle using homologous challenge. Vaccine 2016, 34, 3214–3220. [Google Scholar] [CrossRef] [Green Version]
- Barrera, J.; Brake, D.A.; Schutta, C.; Ettyreddy, D.; Kamicker, B.J.; Rasmussen, M.V.; Bravo de Rueda, C.; Zurita, M.; Pisano, M.; Hurtle, W.; et al. Versatility of the adenovirus-vectored foot-and-mouth disease vaccine platform across multiple foot-and-mouth disease virus serotypes and topotypes using a vaccine dose representative of the AdtA24 conditionally licensed vaccine. Vaccine 2018, 36, 7345–7352. [Google Scholar] [CrossRef]
- Porta, C.; Xu, X.; Loureiro, S.; Paramasivam, S.; Ren, J.; Al-Khalil, T.; Burman, A.; Jackson, T.; Belsham, G.J.; Curry, S.; et al. Efficient production of foot-and-mouth disease virus empty capsids in insect cells following down regulation of 3C protease activity. J. Virol. Methods 2013, 187, 406–412. [Google Scholar] [CrossRef] [Green Version]
- Mignaqui, A.C.; Ferella, A.; Cass, B.; Mukankurayija, L.; L’Abbe, D.; Bisson, L.; Sanchez, C.; Scian, R.; Cardillo, S.B.; Durocher, Y.; et al. Foot-and-Mouth Disease: Optimization, Reproducibility, and Scalability of High-Yield Production of Virus-Like Particles for a Next-Generation Vaccine. Front. Vet. Sci. 2020, 7, 601. [Google Scholar] [CrossRef]
- Terhuja, M.; Saravanan, P.; Tamilselvan, R.P. Comparative efficacy of virus like particle (VLP) vaccine of foot-and-mouth-disease virus (FMDV) type O adjuvanted with poly I:C or CpG in guinea pigs. Biologicals 2015, 43, 437–443. [Google Scholar] [CrossRef]
- Li, H.; Li, Z.; Xie, Y.; Qin, X.; Qi, X.; Sun, P.; Bai, X.; Ma, Y.; Zhang, Z. Novel chimeric foot-and-mouth disease virus-like particles harboring serotype O VP1 protect guinea pigs against challenge. Vet. Microbiol. 2016, 183, 92–96. [Google Scholar] [CrossRef]
- Veerapen, V.P.; van Zyl, A.R.; Wigdorovitz, A.; Rybicki, E.P.; Meyers, A.E. Novel expression of immunogenic foot-and-mouth disease virus-like particles in Nicotiana benthamiana. Virus Res. 2018, 244, 213–217. [Google Scholar] [CrossRef]
- Bhat, S.A.; Saravanan, P.; Hosamani, M.; Basagoudanavar, S.H.; Sreenivasa, B.P.; Tamilselvan, R.P.; Venkataramanan, R. Novel immunogenic baculovirus expressed virus-like particles of foot-and-mouth disease (FMD) virus protect guinea pigs against challenge. Res. Vet. Sci. 2013, 95, 1217–1223. [Google Scholar] [CrossRef]
- Almeida, M.R.; Rieder, E.; Chinsangaram, J.; Ward, G.; Beard, C.; Grubman, M.J.; Mason, P.W. Construction and evaluation of an attenuated vaccine for foot-and-mouth disease: Difficulty adapting the leader proteinase-deleted strategy to the serotype O1 virus. Virus Res. 1998, 55, 49–60. [Google Scholar] [CrossRef]
- Wu, Q.; Moraes, M.P.; Grubman, M.J. Recombinant adenovirus co-expressing capsid proteins of two serotypes of foot-and-mouth disease virus (FMDV): In vitro characterization and induction of neutralizing antibodies against FMDV in swine. Virus Res. 2003, 93, 211–219. [Google Scholar] [CrossRef]
- Bidart, J.; Mignaqui, A.; Kornuta, C.; Lupi, G.; Gammella, M.; Soria, I.; Galarza, R.; Ferella, A.; Cardillo, S.; Langellotti, C.; et al. FMD empty capsids combined with the Immunostant Particle Adjuvant -ISPA or ISA206 induce protective immunity against foot and mouth disease virus. Virus Res. 2021, 297, 198339. [Google Scholar] [CrossRef]
- Mignaqui, A.C.; Ruiz, V.; Perret, S.; St-Laurent, G.; Singh Chahal, P.; Transfiguracion, J.; Sammarruco, A.; Gnazzo, V.; Durocher, Y.; Wigdorovitz, A. Transient gene expression in serum-free suspension-growing mammalian cells for the production of foot-and-mouth disease virus empty capsids. PLoS ONE 2013, 8, e72800. [Google Scholar] [CrossRef] [Green Version]
- Mignaqui, A.C.; Ruiz, V.; Durocher, Y.; Wigdorovitz, A. Advances in novel vaccines for foot and mouth disease: Focus on recombinant empty capsids. Crit. Rev. Biotechnol. 2019, 39, 306–320. [Google Scholar] [CrossRef]
- Puckette, M.; Clark, B.A.; Smith, J.D.; Turecek, T.; Martel, E.; Gabbert, L.; Pisano, M.; Hurtle, W.; Pacheco, J.M.; Barrera, J.; et al. Foot-and-Mouth Disease (FMD) Virus 3C Protease Mutant L127P: Implications for FMD Vaccine Development. J. Virol. 2017, 91, e00924-17. [Google Scholar] [CrossRef] [Green Version]
- Martel, E.; Forzono, E.; Kurker, R.; Clark, B.A.; Neilan, J.G.; Puckette, M. Effect of foot-and-mouth disease virus 3C protease B2 beta-strand proline mutagenesis on expression and processing of the P1 polypeptide using a plasmid expression vector. J. Gen. Virol. 2019, 100, 446–456. [Google Scholar] [CrossRef]
- OIE. Foot and mouth disease. OIE Terrestrial Manual Chapter 3.1.8. Paris, France: World Organisation for Animal Health. Available online: https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.01.08_FMD.pdf (accessed on 11 October 2019).
- Puckette, M.; Burrage, T.; Neilan, J.G.; Rasmussen, M. Evaluation of Gaussia luciferase and foot-and-mouth disease virus 2A translational interrupter chimeras as polycistronic reporters for transgene expression. BMC Biotechnol. 2017, 17, 52. [Google Scholar] [CrossRef] [Green Version]
- Breese, S.S., Jr.; Graves, J.H. Electron microscopic observation of crystalline arrays of foot-and-mouth disease virus. J. Bacteriol. 1966, 92, 1835–1837. [Google Scholar] [CrossRef] [Green Version]
- Chung, C.J.; Clavijo, A.; Bounpheng, M.A.; Uddowla, S.; Sayed, A.; Dancho, B.; Olesen, I.C.; Pacheco, J.; Kamicker, B.J.; Brake, D.A.; et al. An improved, rapid competitive ELISA using a novel conserved 3B epitope for the detection of serum antibodies to foot-and-mouth disease virus. J. Vet. Diagn. Investig. 2018, 30, 699–707. [Google Scholar] [CrossRef]
- Gelkop, S.; Sobarzo, A.; Brangel, P.; Vincke, C.; Romao, E.; Fedida-Metula, S.; Strom, N.; Ataliba, I.; Mwiine, F.N.; Ochwo, S.; et al. The Development and Validation of a Novel Nanobody-Based Competitive ELISA for the Detection of Foot and Mouth Disease 3ABC Antibodies in Cattle. Front. Vet. Sci. 2018, 5, 250. [Google Scholar] [CrossRef]
- Porta, C.; Kotecha, A.; Burman, A.; Jackson, T.; Ren, J.; Loureiro, S.; Jones, I.M.; Fry, E.E.; Stuart, D.I.; Charleston, B. Rational engineering of recombinant picornavirus capsids to produce safe, protective vaccine antigen. PLoS Pathog. 2013, 9, e1003255. [Google Scholar] [CrossRef]
- Mohana Subramanian, B.; Madhanmohan, M.; Sriraman, R.; Chandrasekhar Reddy, R.V.; Yuvaraj, S.; Manikumar, K.; Rajalakshmi, S.; Nagendrakumar, S.B.; Rana, S.K.; Srinivasan, V.A. Development of foot-and-mouth disease virus (FMDV) serotype O virus-like-particles (VLPs) vaccine and evaluation of its potency. Antiviral Res. 2012, 96, 288–295. [Google Scholar] [CrossRef]
- Grubman, M.J.; Lewis, S.A.; Morgan, D.O. Protection of swine against foot-and-mouth disease with viral capsid proteins expressed in heterologous systems. Vaccine 1993, 11, 825–829. [Google Scholar] [CrossRef]
- Liang, T.; Yang, D.; Liu, M.; Sun, C.; Wang, F.; Wang, J.; Wang, H.; Song, S.; Zhou, G.; Yu, L. Selection and characterization of an acid-resistant mutant of serotype O foot-and-mouth disease virus. Arch. Virol. 2014, 159, 657–667. [Google Scholar] [CrossRef]
- Rai, D.K.; Segundo, F.D.; Schafer, E.; Burrage, T.G.; Rodriguez, L.L.; de Los Santos, T.; Hoeprich, P.D.; Rieder, E. Novel 6xHis tagged foot-and-mouth disease virus vaccine bound to nanolipoprotein adjuvant via metal ions provides antigenic distinction and effective protective immunity. Virology 2016, 495, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, P.; Pacheco, J.M.; Uddowla, S.; Hollister, J.; Kotecha, A.; Fry, E.; Rieder, E. Foot-and-mouth disease virus (FMDV) with a stable FLAG epitope in the VP1 G-H loop as a new tool for studying FMDV pathogenesis. Virology 2013, 436, 150–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Protection From | ||||||
|---|---|---|---|---|---|---|
| Species | Dose (μg) | Regimen | Doc Avg VNT(SD) (Log10) | Clinical Disease | Fever | Viremia |
| Cattle | 16 | 1-dose | 1.08 (0.34) | 5 of 5 | 4 of 5 | 5 of 5 |
| Cattle | 0 | Control | 0.60 (0.00) | 0 of 2 | 0 of 2 | N/A |
| Swine | 20 | 1-dose | 0.96 (0.39) | 0 of 5 | 0 of 5 | 0 of 5 |
| Swine | 12 | 2-dose | 2.64 (0.25) | 5 of 5 | 5 of 5 | 5 of 5 |
| Swine | 16 | 2-dose | 1.50 (0.56) | 5 of 5 | 2 of 5 | 5 of 5 |
| Swine | 0 | Control | 0.60 (0.00) | 0 of 10 | 0 of 8 * | N/A |
| Animal ID | Days Post-Challenge % Inhibition | ||
|---|---|---|---|
| 0 | 14 | 21 | |
| D21-03 | 7 | 13 | 13 |
| D21-05 | 13 | 23 | 14 |
| D21-06 | 4 | 72 | 68 |
| D21-07 | 13 | 21 | 24 |
| D21-10 | 17 | 21 | 14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puckette, M.; Primavera, V.; Martel, E.; Barrera, J.; Hurtle, W.; Clark, B.; Kamicker, B.; Zurita, M.; Brake, D.; Neilan, J. Transiently Transfected Mammalian Cell Cultures: An Adaptable and Effective Platform for Virus-like Particle-Based Vaccines against Foot-and-Mouth Disease Virus. Viruses 2022, 14, 989. https://doi.org/10.3390/v14050989
Puckette M, Primavera V, Martel E, Barrera J, Hurtle W, Clark B, Kamicker B, Zurita M, Brake D, Neilan J. Transiently Transfected Mammalian Cell Cultures: An Adaptable and Effective Platform for Virus-like Particle-Based Vaccines against Foot-and-Mouth Disease Virus. Viruses. 2022; 14(5):989. https://doi.org/10.3390/v14050989
Chicago/Turabian StylePuckette, Michael, Victoria Primavera, Erica Martel, Jose Barrera, William Hurtle, Benjamin Clark, Barbara Kamicker, Mariceny Zurita, David Brake, and John Neilan. 2022. "Transiently Transfected Mammalian Cell Cultures: An Adaptable and Effective Platform for Virus-like Particle-Based Vaccines against Foot-and-Mouth Disease Virus" Viruses 14, no. 5: 989. https://doi.org/10.3390/v14050989






