Concentration and Variability of Urinary Phthalate Metabolites, Bisphenol A, Triclosan, and Parabens in Korean Mother–Infant Pairs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Sample Collection
2.2. Analysis of Chemicals
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Concentration of the Chemicals in the Mothers and Infants
3.3. Correlations between the Mothers and Infants for the Chemical Concentrations
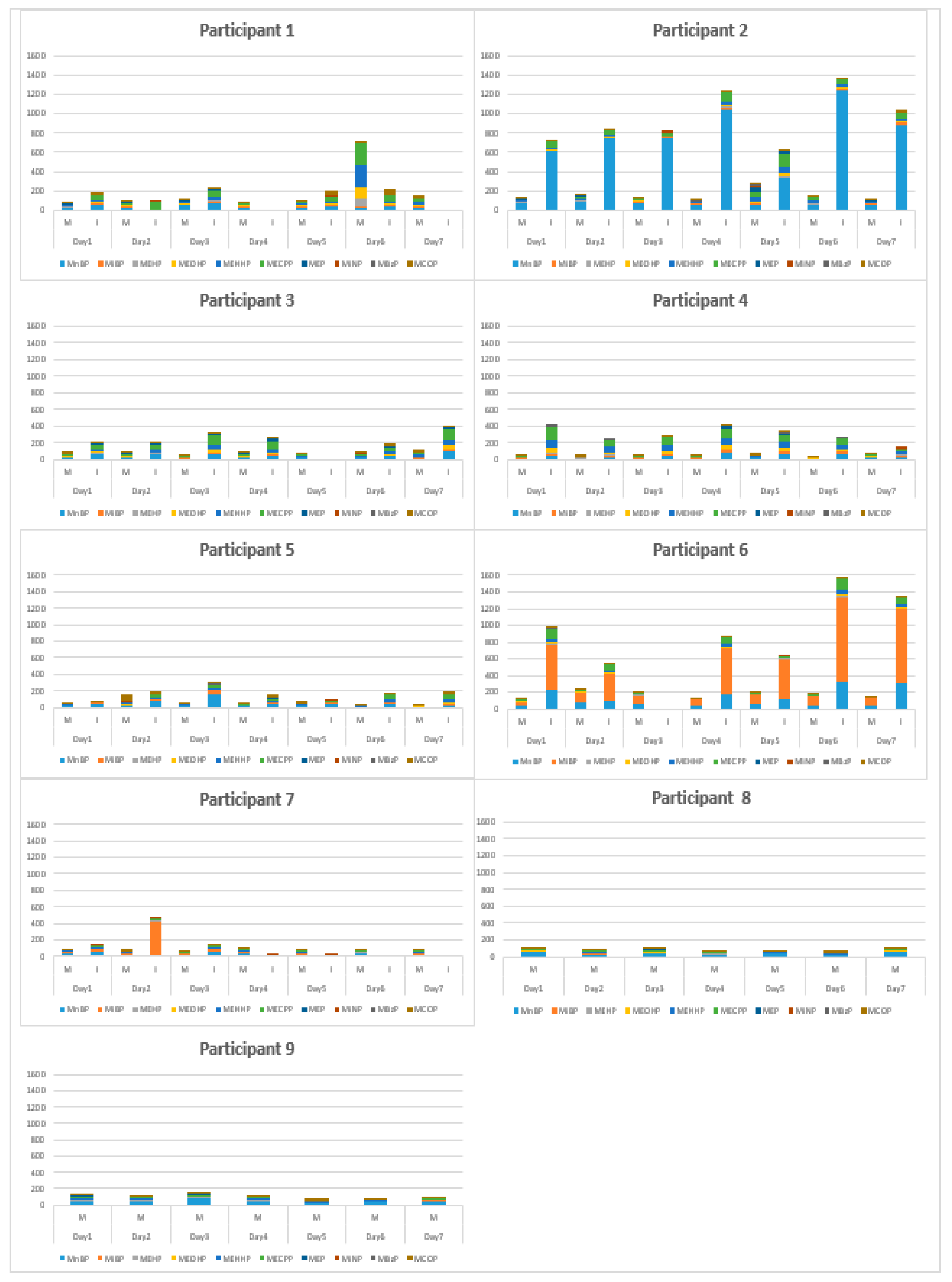
3.4. Variability in Chemicals in Mothers and Infants
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kavlock, R.; Barr, D.; Boekelheide, K.; Breslin, W.; Breysse, P.; Chpin, R.; Gaido, K.; Hodgson, E.; Marcus, M.; Shea, K.; et al. NTP-CERHR Expert Panel Update on the Reproductive and Developmental Toxicity of di (2-ethylhexyl) phthalate. Reprod Toxicol. 2006, 22, 291–399. [Google Scholar] [CrossRef]
- Haines, D.A.; Saravanabhavan, G.; Werry, K.; Khoury, C. An overview of human biomonitoring of environmental chemicals in the Canadian Health Measures Survey: 2007–2019. Int. J. Hyg. Environ. Health 2017, 220, 13–28. [Google Scholar] [CrossRef] [PubMed]
- Lakind, J.S.; Idri, F.; Naiman, D.Q.; Verner, M.A. Biomonitoring and nonpersistent chemicals—Understanding and addressing variability and exposure misclassification. Curr. Environ. Health Rep. 2019, 6, 16–21. [Google Scholar] [CrossRef] [PubMed]
- US Environment Protection Agency. Environmental Justice-Related Terms as Defined Across the PSC Agencies. Available online: https://www.epa.gov/sites/production/files/2015-02/documents/team-ej-lexicon.pdf (accessed on 27 March 2020).
- Birnbaum, L.S. Endocrine effects of prenatal exposure to PCBs, dioxins, and other xenobiotics: Implications for policy and future research. Environ. Health Perspect. 1994, 102, 676–679. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, D.; Moon, S.M.; Yang, E.J. Associations of lifestyle factors with phthalate metabolites, bisphenol A, parabens, and triclosan concentrations in breast milk of Korean mothers. Chemosphere 2020, 249, 126149. [Google Scholar] [CrossRef] [PubMed]
- Dennedy, M.C.; Dunne, F. The maternal and fetal impacts of obesity and gestational diabetes on pregnancy outcome. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 573–589. [Google Scholar] [CrossRef]
- Tratnik, J.S.; Kosjeka, T.; Heath, E.; Mazeja, E.; Ćehića, S.; Karakitsios, S.P.; Sarigiannis, D.A.; Horvat, M. Urinary bisphenol A in children, mothers and fathers from Slovenia: Overallresults and determinants of exposure. Environ. Res. 2019, 168, 32–40. [Google Scholar] [CrossRef]
- Bamai, Y.A.; Arak, A.; Kawai, T.; Tsuboi, T.; Yoshioka, E.; Kanazawa, A.; Cong, S.; Kish, R. Comparisons of urinary phthalate metabolites and daily phthalateintakes among Japanese families. Int. J. Hyg. Environ. Health 2015, 218, 461–470. [Google Scholar] [CrossRef]
- Casas, L.; Fernández, M.F.; Llop, S.; Guxens, M.; Ballester, F.; Olea, N.; Irurzun, M.B.; Rodríguez, L.S.M.; Riaño, I.; Tardón, A.; et al. Urinary concentrations of phthalates and phenols in a population of Spanish pregnant women and children. Environ. Int. 2011, 37, 858–866. [Google Scholar] [CrossRef]
- Covaci, A.; Hond, E.D.; Geens, T.; Govarts, E.; Koppen, G.; Frederiksen, H.; Knudsen, L.E.; Mørck, T.A.; Gutleb, A.C.; Guignard, C.; et al. Urinary BPA measurements in children and mothers from six European member states: Overall results and determinants of exposure. Environ. Res. 2015, 141, 77–85. [Google Scholar] [CrossRef]
- Cullen, E.; Evans, D.; Griffin, C.; Burke, P.; Mannion, R.; Burns, D.; Flanagan, A.; Kellegher, A.; Schoeters, G.; Govarts, E.; et al. Urinary phthalate concentrations in mothers and their children in Ireland: Results of the DEMOCOPHES human biomonitoring study. Int. J. Environ. Res. Public Health 2017, 14, 1456. [Google Scholar] [CrossRef] [PubMed]
- Cutandaa, F.; Koch, H.M.; Estebana, M.; Sáncheza, J.; Angerer, J.; Castaño, A. Urinary levels of eight phthalate metabolites and bisphenol A inmother–child pairs from two Spanish locations. Int. J. Hyg. Environ. Health 2015, 218, 47–57. [Google Scholar] [CrossRef] [PubMed]
- Enke, U.; Schleussner, E.; Palmke, C.; Seyfarth, L.; Koch, H.M. Phthalate exposure in pregnant women and newborns—The urinary metabolite excretion pattern differs distinctly. Int. J. Hyg. Environ. Health 2013, 216, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Frederiksen, H.; Søgaard Nielsen, J.K.; Aarøe Mørck, T.; Hansen, P.W.; Jensen, J.F.; Nielsen, O.; Andersson, A.M.; Knudsen, L.E. Urinary excretion of phthalate metabolites, phenols and parabens in rural and urban Danish mother–child pairs. Int. J. Hyg. Environ. Health 2013, 216, 772–783. [Google Scholar] [CrossRef] [PubMed]
- Hlisníková, H.; Šidlovská, M.; Kolena, B.; Petrovičová, I. Association between Consumer Practices and Phthalate Exposure in Children and their Parents from Slovakia. Pol. J. Environ. Stud. 2018, 28, 1195–1202. [Google Scholar] [CrossRef]
- Kasper-Sonnenberg, M.K.; Koch, H.M.; Wittsiepe, J.; Fromme, H.; Wilhelma, M. Determination of bisphenol a in urine from mother–child-pairs–results from the Duisburg birth cohort study, Germany. J. Toxicol. Environ. Health A 2012, 75, 429–437. [Google Scholar] [CrossRef]
- Larsson, K.; Björklund, K.L.; Palm, B.; Wennberg, M.; Kaj, L.; Lindh, C.H.; Jönsson, B.A.G.; Berglund, M. Exposure determinants of phthalates, parabens, bisphenol A and triclosan in Swedish mothers and their children. Environ. Int. 2014, 73, 323–333. [Google Scholar] [CrossRef]
- Lin, S.; Ku, H.Y.; Su, P.H.; Chen, J.W.; Huang, P.C.; Angerer, J.; Wang, S.L. Phthalate exposure in pregnant women and their children in central Taiwan. Chemosphere 2011, 82, 947–955. [Google Scholar] [CrossRef]
- Myridakis, A.; Fthenou, E.; Balaska, E.; Vakinti, M.; Kogevinas, M.; Stephanou, E.G. Phthalate esters, parabens and bisphenol-A exposure among mothers and their children in Greece (Rhea cohort). Environ. Int. 2015, 83, 1–10. [Google Scholar] [CrossRef]
- Polinski, K.J.; Dabeleaa, D.; Hammana, R.F.; Adgateb, J.L.; Calafatc, A.M.; Ye, X.; Starlinga, A.P. Distribution and predictors of urinary concentrations of phthalate metabolites and phenols among pregnant women in the Healthy Start Study. Environ. Res. 2018, 162, 308–317. [Google Scholar] [CrossRef]
- Song, N.R.; On, J.W.; Lee, J.G.; Park, J.D.; Kwon, H.J.; Yoon, H.J.; Pyo, H.S. Biomonitoring of urinary di(2-ethylhexyl) phthalate metabolites of mother and child pairs in South Korea. Environ. Int. 2013, 54, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Skarha, J.; Messerlian, C.; Bellinger, D.; Minguez-Alarcon, L.; Romano, M.E.; Ford, J.P.; Williams, P.L.; Calafat, A.M.; Hauser, R.; Braun, J.M. Parental preconception and prenatal urinary bisphenol A and paraben concentrations and child behabior. Environ. Epid. 2020, 4, e082. [Google Scholar] [CrossRef]
- Hornung, R.W.; Reed, L.D. Estimation of average concentration in the presence of nondetectable values. J. Occup. Environ. Hyg. 1990, 5, 46–51. [Google Scholar] [CrossRef]
- Koch, H.M.; Bolt, H.M.; Angerer, J. Di (2- ethylhexyl) phthalate (DEHP) metabolites in human urine and serum after a single oral dose of deuterium-labelled DEHP. Arch. Toxicol. 2004, 78, 123–130. [Google Scholar] [CrossRef]
- Koch, H.M.; Bolt, H.M.; Preuss, R.; Angerer, J. New metabolites of di (2- ethylhexyl) phthalate (DEHP) in human urine and serum after single oral doses of deuterium-labelled DEHP. Arch. Toxicol. 2005, 79, 367–376. [Google Scholar] [CrossRef]
- Morgan, M.K.; Barr, D.B.; Starr, J.M.; Clifton, M.S.; Sobus, J.R. Distribution, variability, and predictors of urinary bisphenol A levels in 50 North Carolina adults over a six-week monitoring period. Environ. Int. 2018, 112, 85–99. [Google Scholar] [CrossRef]
- Völkel, W.; Colnot, T.; Csanády, G.A.; Johannes, G.; Filser, J.G.; Dekant, W. Metabolism and kinetics of bisphenol A in humans at low doses following oral administration. Chem. Res. Toxicol. 2002, 15, 1281–1287. [Google Scholar] [CrossRef]
- Ye, X.; Wong, L.Y.; Bishop, A.M.; Calafat, A.M. Variability of Urinary Concentrations of Bisphenol A in Spot Samples, First Morning Voids, and 24-Hour Collections. Environ. Health Perspect. 2011, 119, 983–988. [Google Scholar] [CrossRef]
- Scientific Committee on Consumer safety. Opinion on Triclosan; European Unions: Brussels, Belgium, 2011; Available online: https://ec.europa.eu/health/scientific_committees/consumer_safety/docs/sccs_o_054.pdf (accessed on 15 July 2000).
- Koch, H.M.; Aylward, L.L.; Hays, S.M.; Smolders, R.; Moos, R.K.; Cocker, J.; Jones, K.; Warren, N.; Levy, L.; Bevan, R. Inter- and intra-individual variation in urinary biomarker concentrations over a 6-day sampling period. Part 2: Personal care product ingredients. Toxicol. Lett. 2014, 231, 261–269. [Google Scholar] [CrossRef]
- Braun, J.M.; Kalkbrenner, A.E.; Calafat, A.M.; Bernert, J.T.; Ye, X.; Silva, M.J.; Barr, D.B.; Sathyanarayana, S.; Lanphear, B.P. Variability and predictors of urinary bisphenol A concentrations during pregnancy. Environ. Health Perspect. 2011, 119, 131–137. [Google Scholar] [CrossRef]
- Fisher, M.; Arbuckie, T.E.; Mallick, R.; LeBlanc, A.; Hauser, R.; Feeley, M.; Koniecki, D.; Ramsay, T.; Provencher, G.; Bérubé, R.; et al. Bisphenol A and phthalate metabolite urinary concentrations: Daily and across pregnancy variability. J. Expo. Sci. Env. Epid. 2015, 25, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Meeker, J.D.; Cantonwine, D.E.; Rivera-González, L.O.; Ferguson, K.K.; Mukherjee, M.; Calafat, A.M.; Ye, X.; Anzalota Del Toro, L.V.; Crespo-Hernández, N.; Jiménez-Vélez, B.; et al. Distribution, variability, and predictors of urinary concentrations of phenols and parabens among pregnant women in Puerto Rico. Environ. Sci. Technol. 2013, 47, 3439–3447. [Google Scholar] [CrossRef] [PubMed]
- Preau Jr, J.L.; Wong, L.Y.; Silva, M.J.; Needham, L.L.; Calafat, A.M. Variability over 1 week in the urinary concentrations of metabolites of diethyl phthalate and di(2-ethylhexyl) phthalate among eight adults: An observational study. Environ. Health Perspect. 2010, 118, 1748–1754. [Google Scholar] [CrossRef]
- Vernet, C.V.; Philippat, C.; Calafat, A.M.; Ye, X.; Caen, S.L.; Siroux, V.; Schisterman, E.F.; Slama, R. Within-day, between-day, and between-week variability of urinary concentrations of phenol biomarkers in pregnant women. Environ. Health Perspect. 2018, 126, 37705. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Laboratory Procedure Manual—Bisphenol A and Other Environmental Phenols and Parabens in Urine, Method no. 6301.01. NHANES 2009–2010; CDC: Atlanta, GA, USA, 2011; pp. 27–35. Available online: https://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/EPH_F_met_phenols_parabens.pdf (accessed on 25 July 2020).
- National Institute of Environmental Research (NIER). A Manual for Analysis of Environmental Pollutants in the Human Specimen, NIER GOVP1200717001; NIER: Incheon, Korea, 2006; p. 302. [Google Scholar]
- WHO. Biological Monitoring of Chemical Exposure in Workplace; World Health Organization: Geneva, Switzerland, 1996. [Google Scholar]
- LaKind, J.S.; Goodman, M.; Mattison, D.R. Bisphenol A and indicators of obesity, glucose metabolism/type 2 diabetes and cardiovascular disease: A systematic review of epidemiologic research. Crit. Rev. Toxicol. 2014, 44, 121–150. [Google Scholar] [CrossRef]
- Goodman, M.; Naiman, D.Q.; LaKind, J.S. Systematic review of the literature on triclosan and health outcomes in humans. Crit. Rev. Toxicol. 2018, 48, 1–51. [Google Scholar] [CrossRef]
- Rosner, B. Fundamentals of biostatistics, 5th ed.; Cengage: Pacific Grove, CA, USA, 2000; pp. 511–576. [Google Scholar]
- Kim, S.; Lee, S.; Shin, C.; Jangwoo Lee, J.; Kim, S.; Lee, A.; Park, J.; Kho, Y.; Moose, R.K.; Koche, H.M.; et al. Urinary parabens and triclosan concentrations and associated exposure characteristics in a Korean population-A comparison between night-time and first-morning urine. Int. J. Hyg. Environ. Health 2018, 221, 632–641. [Google Scholar] [CrossRef]
- Philippat, C.; Wolff, M.S.; Calafat, A.M.; Ye, X.; Bausell, R.; Meadows, M.; Stone, J.; Slama, R.; Engel, S.M. Prenatal exposure to environmental phenols: Concentrations in amniotic fluid and variability in urinary concentrations during pregnancy. Environ. Health Perspec. 2013, 121, 1125–1131. [Google Scholar] [CrossRef]
- Pollack, A.Z.; Perkins, N.J.; Sjaarda, L.; Mumford, S.M.; Kannan, K.; Philippat, C.; Wactawski-Wende, J.; Schisterman, E.F. Variability and exposure classification of urinary phenol and paraben metabolite concentrations in reproductive-aged women. Environ. Res. 2016, 151, 513–520. [Google Scholar] [CrossRef]
- Townsend, M.K.; Franke, A.A.; Li, X.; Hu, F.B.; Eliassen, A.H. Within-person reproducibility of urinary bisphenol A and phthalate metabolites over a 1 to 3 years period among women in the Nurses’ Health Studies: A prospective cohort study. Environ. Health 2013, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, S.; Park, J.; Kim, H.J.; Lee, J.; Choi, G.; Choi, S.; Kim, S.; Kim, S.Y.; Moon, H.B.; et al. Urinary paraben concentrations among pregnant women and their matching newborn infants of Korea, and the association with oxidative stress biomarkers. Sci. Total Environ. 2013, 461, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.S.; Kyung, M.S.; Ko, A.; Park, J.H.; Hwang, M.S.; Kwon, J.E.; Suh, J.H.; Lee, H.S.; Moon, G.I.; Hwang, I.G.; et al. Urinary concentrations of parabens and their association with demographic factors: A population-based cross-sectional study. Environ. Res. 2016, 146, 245–251. [Google Scholar] [CrossRef]
- Korean Environmental Biostatics. Available online: http://stat.me.go.kr/nesis/mesp2/webStatistics/stat_main.jsp?tblID=DT_106N_99_1100051&inq_gubun=1&lang=kor&list_id=106H_01_008004004&l_interval=2 (accessed on 26 March 2020).
- Jo, A.; Kim, H.S.; Chung, H.W.; Chang, N.S. Association between beverage intake with urinary bisphenol A levels in Korean women of reproductive age. Int. J. Environ. Res. Public Health 2016, 13, 680. [Google Scholar] [CrossRef]
- Park, C.; Hwang, M.; Baek, Y.; Jung, S.; Lee, Y.; Paek, D.; Choi, K. Urinary phthalate metabolite and bisphenol A levels in the Korean adult population in association with sociodemographic and behavioral characteristics: Korean National Environmental Health Survey (KoNEHS) 2012–2014. Int. J. Hyg. Environ. Health 2019, 222, 903–910. [Google Scholar] [CrossRef]
- Serra, H.; Beausoleil, C.; Habert, R.; Christophe Minier, C.; Picard-Hagen, N.; Michel, C. Evidence for bisphenol B endocrine properties: Scientific and regulatory perspectives. Environ. Health Perspect. 2019, 127, 106001. [Google Scholar] [CrossRef]
- Barroso, J. Commission Directive 2011/8/EU of 28 January 2011 amending Directive 2002/72/EC as regards the restriction of use of bisphenol a in plastic infant feeding bottles. Off. J. EU 2011, 26, 11–14. Available online: http://extwprlegs1.fao.org/docs/pdf/eur100741.pdf (accessed on 25 July 2020).
- European Commission. Commission Regulation (EU) 2016/2235 of 12 December 2016 amending Annex XVLL to Regulation (EC) NO 1907/2006 OG the European Parliament and of the Council concerning the Regulation, Evalution, Authorisation and Restriction of Chemicals (REACH) as regards bisphenol A. Off. J. EU 2016, 337, 3–5. [Google Scholar]
- European Commission. Commission Regulation (EU) 2018/213 of 12 February 2018 on the use of bisphenol A in varnishes and coatings intended to come into contact with food and amending Regulation (EU) NO 10/2011 as regards the use of that substance in plastic food contact materials. Off. J. EU 2018, 41, 6–12. [Google Scholar]
- European Chemical Agency. Agreement of the Member State Committee on the Identification of 4,4′-Isopropylidenediphnol (bisphenol A) as a Substance of Very High Concern. Available online: https://echa.europa.eu/documents/1062/ac9efb97-c06b-d1a7-2823-5dc69208a238/ (accessed on 12 March 2020).
- European Chemical Agency. Agreement of the Member State Committee on the Identification of 4,4-Isopropylidenediphnol (bisphenol A) as a Substance of very High Concern for the Environment. Available online: https://echa.europa.eu/documents/10162/81862f4e-92bc-6f64-9a01-42565b526022 (accessed on 12 March 2020).
- US Food and Drug Administration. FDA Issues Final Rule on Safety and Effectiveness of Antibacterial Soaps; US DHHS; FDA: White Oak, MD, USA, 2016. Available online: https://www.fda.gov/news-events/press-announcements/fda-issues-final-rule-safety-and-effectiveness-antibacterial-soaps (accessed on 25 July 2020).
- US Food and Drug Administration. Safety and Effectiveness for Health Care Antiseptics: Topical Antimicrobial Drug Products for Over-the-counter Human Use; DHHS; FDA: White Oak, MD, USA, 2017. Available online: https://www.fda.gov/media/92294/download (accessed on 25 July 2020).
- Edginton, A.N.; Ritter, L. Predicting plasma concentrations of bisphenol A in children younger than 2 years of age after typical feeding schedules, using a physiologically based toxicokinetic model. Environ. Health Perspect. 2009, 117, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Jaghbir, M.; Salam, M.; Al-Kadamany, G.; Damsees, R.; Al-Rawashdeh, N. Testing baby bottles for the presence of residual and migrated bisphenol A. Environ. Monit. Assess. 2019, 191, 7. [Google Scholar] [CrossRef]
- Becker, K.; Güen, T.; Seiwert, M.; Conrad, A.; Pick-Fuß, H.; Müller, J.; Wittassek, M.; Schulz, C.; Kolossa-Gehring, M. GerES IV: Phthalate metabolites and bisphenol-A in urine of German children. Int. J. Hyg. Environ. Health 2009, 212, 685–692. [Google Scholar] [CrossRef]
- Park, J.H.; Hwang, M.S.; Ko, A.; Jung, H.J.; Guiim, M.L.; Soo, M.K.; Ho, L.Y.; Ki, K.M.; Seok, S.H.; Seung, L.H.; et al. Risk assessment based on urinary bisphenol A levels in the general Korean population. Environ. Res. 2016, 150, 606–615. [Google Scholar] [CrossRef] [PubMed]


| Characteristic | Category | N (%)/Mean (SD) | Median (range) |
|---|---|---|---|
| Maternal age (years) | 30.9 (2.8) | 31 (25–37) | |
| Maternal BMI (m2/kg) | 21.4 (2.7) | 20.8 (17.5–29.7) | |
| Residence area | Metropolitan | 19 (42.2) | |
| Non-Metropolitan | 26 (57.8) | ||
| Maternal education | <College | 3 (6.7) | |
| ≧College | 42 (93.3) | ||
| Household income (USD/month) | <5000 | 26 (57.8) | |
| ≧5000 | 19(42.2) | ||
| Employment status | Yes | 35 (77.8) | |
| No | 10 (22.2) | ||
| Infant sex | Male | 6 (13.3) | |
| Female | 39 (86.7) | ||
| Infant age (month) | 11.4 (1.5) | 12.0 (6–14) | |
| Infant weight (kg) | 9.8 (1.2) | 9.6 (7.6–12.5) | |
| Infant birth weight (kg) | 2.8 (0.3) | 3.1 (2.2–3.4) | |
| Breastfeeding period (months) | 7.5 (3.9) | 8 (1–13) |
| Parent Compound | Measured Biomarker | LOD | Mother (n = 45), Samples (n = 225) | Infant (n = 36), Samples (n = 71) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % > LOD | GM | Percentile | % > LOD | GM | Percentile | |||||||||||||
| SD | Min | 25th | 50th | 75th | Max | SD | Min | 25th | 50th | 75th | Max | |||||||
| Creatinine-adjusted data (μg/L) | ||||||||||||||||||
| DEP | MEP | 0.13 | 65 | 3.94 | 7.19 | < LOD | < LOD | 3.68 | 4.71 | 3693 | 42 | 9.81 | 15.75 | < LOD | < LOD | < LOD | 24.7 | 199 |
| DnBP | MnBP | 0.28 | 100 | 25.5 | 2.03 | 4.23 | 14.6 | 26.2 | 41.8 | 138 | 91 | 64.4 | 5.20 | < LOD | 34.6 | 61.8 | 100 | 1241 |
| DIBP | MiBP | 0.19 | 100 | 6.59 | 3.24 | 0.21 | 2.92 | 5.68 | 11 | 145 | 90 | 19.7 | 6.34 | < LOD | 7.91 | 16.4 | 38.1 | 1009 |
| BBzP | MBzP | 0.08 | 60 | 0.66 | 4.38 | < LOD | < LOD | 0.63 | 1.36 | 43.3 | 44 | 1.89 | 6.79 | < LOD | < LOD | < LOD | 4.75 | 15.6 |
| DINP | MiNP | 0.04 | 100 | 1.02 | 2.45 | 0.07 | 0.28 | 0.53 | 0.99 | 57.6 | 91 | 0.85 | 2.40 | < LOD | 0.49 | 0.81 | 1.3 | 6.08 |
| DEHP | MEHP | 0.14 | 100 | 2.68 | 2.24 | 0.29 | 1.66 | 2.79 | 4.63 | 259 | 89 | 3.63 | 3.29 | < LOD | 2.14 | 3.62 | 5.98 | 40.5 |
| MEOHP | 0.15 | 94 | 4.25 | 3.38 | < LOD | 2.68 | 4.88 | 6.62 | 302 | 84 | 11.8 | 7.20 | < LOD | 9.62 | 14.3 | 20.6 | 81 | |
| MEHHP | 0.14 | 97 | 7.9 | 2.89 | < LOD | 6.25 | 9.7 | 13 | 557 | 87 | 14.76 | 6.25 | < LOD | 11.56 | 26.12 | 42.1 | 104.62 | |
| MECPP | 0.11 | 97 | 10.1 | 3.26 | < LOD | 6.87 | 11.2 | 15.8 | 533 | 91 | 40.8 | 3.52 | < LOD | 27.4 | 41.4 | 67.8 | 300 | |
| MCOP | 0.09 | 97 | 2.3 | 2.88 | < LOD | 1.31 | 2.18 | 3.71 | 121 | 81 | 6.85 | 7.85 | < LOD | 4.84 | 7.68 | 12.9 | 58.2 | |
| BPA | 0.02 | 66 | 1.54 | 11.58 | < LOD | < LOD | 1.57 | 3.6 | 29.2 | 87 | 6.39 | 9.12 | < LOD | 3.42 | 6.8 | 13.2 | 59.5 | |
| TCS | 0.04 | 75 | 0.32 | 5.18 | < LOD | 0.09 | 0.24 | 1.15 | 5.44 | 82 | 2.19 | 6.81 | < LOD | 0.92 | 2.06 | 4.67 | 78.7 | |
| MP | 0.17 | 100 | 6.16 | 2.90 | 0.94 | 2.92 | 4.85 | 9.97 | 464 | 93 | 27.9 | 9.17 | < LOD | 7.08 | 12.5 | 51.8 | 9192 | |
| EP | 0.11 | 99 | 65.6 | 6.45 | < LOD | 22.1 | 76.3 | 208 | 4692 | 44 | 19.6 | 8.58 | < LOD | < LOD | < LOD | 79.4 | 807 | |
| PP | 0.12 | 59 | 0.84 | 6.12 | < LOD | < LOD | 0.51 | 2.7 | 65.8 | 84 | 3.84 | 8.97 | < LOD | 0.82 | 2.08 | 11.9 | 2431 | |
| Unadjusted data (μg/L) | ||||||||||||||||||
| DEP | MEP | 0.13 | 65 | 5.02 | 8.96 | < LOD | < LOD | 4.68 | 8.37 | 1499 | 44 | 6.22 | 20.04 | < LOD | < LOD | < LOD | 19.2 | 95.9 |
| DnBP | MnBP | 0.28 | 100 | 32.1 | 3.25 | 2.72 | 17 | 32.1 | 59.4 | 315 | 95 | 27.8 | 6.98 | < LOD | 12.2 | 32.4 | 71.3 | 824 |
| DIBP | MiBP | 0.19 | 100 | 8.31 | 3.15 | 0.24 | 3.47 | 7.65 | 18.3 | 302 | 95 | 9.11 | 7.30 | < LOD | 3.92 | 8.57 | 20.7 | 281 |
| BBzP | MBzP | 0.08 | 60 | 0.93 | 5.08 | < LOD | < LOD | 0.91 | 1.76 | 104 | 47 | 1.11 | 6.43 | < LOD | < LOD | < LOD | 2.32 | 9.86 |
| DINP | MiNP | 0.04 | 100 | 0.69 | 2.73 | 0.07 | 0.37 | 0.66 | 1.2 | 73 | 98 | 0.38 | 3.26 | < LOD | 0.17 | 0.29 | 0.85 | 6.65 |
| DEHP | MEHP | 0.14 | 100 | 3.38 | 2.69 | 0.18 | 1.98 | 3.55 | 6.29 | 264 | 94 | 1.66 | 3.11 | < LOD | 0.78 | 1.7 | 2.98 | 33.6 |
| MEOHP | 0.15 | 94 | 9.33 | 3.22 | < LOD | 3.31 | 6.51 | 10 | 309 | 88 | 5.56 | 7.78 | < LOD | 2.75 | 7.56 | 13.8 | 45 | |
| MEHHP | 0.14 | 97 | 18.6 | 4.62 | < LOD | 6.51 | 12.8 | 19.6 | 569 | 91 | 9.66 | 8.04 | < LOD | 4.96 | 12.2 | 22.5 | 72.7 | |
| MECPP | 0.11 | 97 | 13.1 | 3.82 | < LOD | 7.13 | 15.7 | 23.5 | 545 | 96 | 17.6 | 4.63 | < LOD | 8.47 | 21.4 | 38.3 | 129 | |
| MCOP | 0.09 | 97 | 2.96 | 3.50 | < LOD | 1.61 | 2.82 | 5.28 | 154 | 85 | 3.49 | 7.94 | < LOD | 1.34 | 4.39 | 9.29 | 27.3 | |
| BPA | 0.02 | 66 | 2.17 | 14.50 | < LOD | < LOD | 2.27 | 5.49 | 76.2 | 92 | 2.88 | 10.66 | < LOD | 1.63 | 3.69 | 5.57 | 52.3 | |
| TCS | 0.04 | 75 | 0.49 | 5.25 | < LOD | 0.14 | 0.4 | 1.78 | 10.1 | 87 | 0.92 | 7.04 | < LOD | 0.45 | 0.96 | 2.15 | 17.7 | |
| MP | 0.17 | 100 | 21.2 | 4.81 | 0.77 | 3.82 | 6.68 | 12 | 1537 | 98 | 11.9 | 9.22 | < LOD | 1.81 | 6.86 | 30.5 | 4915 | |
| EP | 0.11 | 99 | 83.2 | 8.81 | < LOD | 26.2 | 103 | 288 | 3447 | 45 | 72.1 | 9.38 | < LOD | < LOD | < LOD | 84.7 | 807 | |
| PP | 0.12 | 59 | 1.09 | 7.73 | < LOD | < LOD | 0.61 | 3.37 | 218 | 89 | 35 | 7.55 | < LOD | 0.39 | 0.66 | 4.34 | 639 | |
| (μg/L) | I-MEP | I-MnBP | I-MiBP | I-MBzP | I-MiNP | I-MEHP | I-MEOHP | I-MEHHP | I-MECPP | I-MCOP | I-BPA | I-TCS | I-MP | I-EP | I-PP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M-MEP | 0.45 * | 0.03 | 0.05 | 0.01 | 0.01 | 0.03 | 0.04 | 0.01 | 0.11 | 0.23 | 0.09 | 0.05 | 0.10 | 0.01 | 0.07 |
| M-MnBP | 0.02 | 0.62 ** | 0.25 | 0.19 | 0.17 | 0.15 | 0.10 | 0.11 | 0.18 | 0.09 | 0.31 | 0.08 | 0.25 | 0.01 | 0.01 |
| M-MiBP | 0.26 | 0.38 * | 0.89 ** | 0.20 | 0.10 | 0.25 | 0.30 | 0.37 * | 0.35 | 0.08 | 0.02 | 0.03 | 0.03 | 0.07 | 0.02 |
| M-MBzP | 0.03 | 0.10 | 0.06 | 0.05 | 0.30 | 0.31 | 0.09 | 0.04 | 0.31 | 0.22 | 0.25 | 0.01 | 0.19 | 0.39 * | 0.31 |
| M-MiNP | 0.04 | 0.13 | 0.26 | 0.16 | 0.09 | 0.13 | 0.21 | 0.29 | 0.22 | 0.07 | 0.18 | 0.18 | 0.44 * | 0.15 | 0.01 |
| M-MEHP | 0.01 | 0.17 | 0.03 | 0.12 | 0.05 | 0.04 | 0.04 | 0.02 | 0.12 | 0.01 | 0.30 | 0.08 | 0.27 | 0.10 | 0.10 |
| M-MEOHP | 0.06 | 0.07 | 0.03 | 0.26 | 0.04 | 0.14 | 0.01 | 0.02 | 0.07 | 0.28 | 0.41 * | 0.01 | 0.50 * | 0.04 | 0.06 |
| M-MEHHP | 0.01 | 0.12 | 0.02 | 0.26 | 0.10 | 0.19 | 0.06 | 0.03 | 0.01 | 0.21 | 0.33 | 0.02 | 0.50 * | 0.07 | 0.02 |
| M-MECPP | 0.06 | 0.03 | 0.03 | 0.30 | 0.01 | 0.05 | 0.03 | 0.03 | 0.10 | 0.19 | 0.41 * | 0.02 | 0.55 ** | 0.02 | 0.11 |
| M-MCOP | 0.02 | 0.11 | 0.17 | 0.02 | 0.09 | 0.11 | 0.13 | 0.18 | 0.17 | 0.05 | 0.22 | 0.03 | 0.53 * | 0.07 | 0.04 |
| M-BPA | 0.20 | 0.29 | 0.22 | 0.08 | 0.04 | 0.18 | 0.25 | 0.26 | 0.32 | 0.08 | 0.39 * | 0.24 | 0.19 | 0.25 | 0.15 |
| M-TCS | 0.10 | 0.16 | 0.11 | 0.07 | 0.48 * | 0.52 * | 0.24 | 0.25 | 0.22 | 0.05 | 0.51 * | 0.27 | 0.02 | 0.09 | 0.08 |
| M-MP | 0.07 | 0.25 | 0.07 | 0.03 | 0.17 | 0.01 | 0.21 | 0.19 | 0.11 | 0.13 | 0.05 | 0.09 | 0.01 | 0.16 | 0.15 |
| M-EP | 0.15 | 0.13 | 0.08 | 0.21 | 0.09 | 0.23 | 0.35 | 0.38 * | 0.24 | 0.11 | 0.17 | 0.16 | 0.10 | 0.17 | 0.12 |
| M-PP | 0.29 | 0.16 | 0.17 | 0.36 * | 0.14 | 0.08 | 0.17 | 0.19 | 0.14 | 0.14 | 0.01 | 0.04 | 0.12 | 0.32 | 0.32 |
| Within-Individual ICC (95% CI) | |||||
|---|---|---|---|---|---|
| Creatinine Adjusted Data (μg/L) | M-FMV (n = 63) | M-LV (n = 63) | M-BV (n = 63) | M-SPOT (n = 189) | I-SPOT (n = 35) |
| MEP | 0.82 (0.55 to 0.95) | 0.12 (0.08 to 0.77) | 0.80 (0.51 to 0.95) | 0.17 (0.02 to 0.57) | 0.57 (0.29 to 0.92) |
| MnBP | 0.94 (0.86 to 0.99) | 0.92 (0.80 to 0.98) | 0.85 (0.64 to 0.96) | 0.90 (0.84 to 0.95) | 0.96 (0.87 to 0.99) |
| MiBP | 0.99 (0.98 to 0.99) | 0.97 (0.93 to 0.99) | 0.98 (0.94 to 0.99) | 0.98 (0.97 to 0.99) | 0.93 (0.80 to 0.99) |
| MBzP | 0.34 (0.13 to 0.83) | 0.41 (0.15 to 0.85) | 0.49 (0.05 to 0.87) | 0.38 (0.06 to 0.68) | 0.83 (0.48 to 0.97) |
| MiNP | 0.72 (0.31 to 0.93) | NA | 0.39 (0.05 to 0.84) | NA | 0.68 (0.05 to 0.94) |
| MEHP | 0.85 (0.64 to 0.96) | 0.13 (0.05 to 0.77) | 0.77 (0.44 to 0.94) | 0.15 (0.06 to 0.56) | 0.91 (0.73 to 0.98) |
| MEOHP | 0.86 (0.65 to 0.96) | 0.14 (0.03 to 0.77) | 0.18 (0.03 to 0.78) | 0.14 (0.07 to 0.56) | 0.90 (0.70 to 0.98) |
| MEHHP | 0.77 (0.44 to 0.94) | 0.13 (0.05 to 0.77) | 0.09 (0.05 to 0.76) | 0.13 (0.09 to 0.55) | 0.93 (0.78 to 0.99) |
| MECPP | 0.72 (0.32 to 0.93) | 0.16 (0.07 to 0.78) | 0.02 (0.01 to 0.74) | 0.16 (0.04 to 0.56) | 0.83 (0.48 to 0.97) |
| MCOP | 0.38 (0.02 to 0.84) | 0.26 (0.03 to 0.81) | 0.34 (0.03 to 0.83) | 0.27 (0.05 to 0.62) | 0.83 (0.48 to 0.97) |
| BPA | 0.40 (0.09 to 0.84) | 0.29 (0.06 to 0.81) | NA | 0.26 (0.05 to 0.62) | 0.70 (0.12 to 0.94) |
| TCS | 0.94 (0.86 to 0.99) | 0.94 (0.84 to 0.98) | 0.93 (0.84 to 0.98) | 0.94 (0.89 to 0.97) | NA |
| MP | 0.78 (0.45 to 0.94) | 0.46 (0.14 to 0.86) | 0.64 (0.11 to 0.90) | 0.55 (0.24 to 0.77) | 0.38 (0.16 to 0.88) |
| EP | 0.72 (0.30 to 0.93) | 0.62 (0.06 to 0.90) | 0.74 (0.37 to 0.93) | 0.67 (0.44 to 0.83) | 0.86 (0.74 to 0.82) |
| PP | 0.91 (0.79 to 0.98) | 0.85 (0.63 to 0.96) | 0.65 (0.14 to 0.90) | 0.76 (0.58 to 0.87) | NA |
| Authors (Publication Year) | Country (n) | Mother (n)/Infant (n) | MEP | MnBP | MiBP | MBzP | MiNP | MEHP | MEOHP | MEHHP | MECPP | MCOP | BPA | TCS | MP | EP | PP |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| This study (2020) | South Korea (n = 159) | Mother (225) | 3.68 | 26.2 | 5.68 | 0.63 | 0.53 | 2.79 | 4.88 | 9.7 | 11.2 | 2.18 | 1.6 | 0.2 | 4.9 | 76 | 1 |
| Infants (71) | 12.2 | 61.8 | 16.4 | 3.26 | 0.81 | 3.62 | 14.3 | 22.7 | 41.4 | 7.68 | 6.8 | 2.1 | 13 | 22 | 2 | ||
| Hlisníková et al. (2019) [16] | Slovakia (n = 78) | Parents (n = 21) | 24.1 | 32.82 | 17.1 | 3.26 | 7.63 | 10.03 | 5.6 | ||||||||
| Children (n = 57) | 23.7 | 54.11 | 32.1 | 2.32 | 14.5 | 17.52 | 11.73 | ||||||||||
| Tratnik et al. (2019) [8] | Slovenia (n = 381) | Mother (n = 155) | 1.1 | ||||||||||||||
| Children (n = 155) | 1.9 | ||||||||||||||||
| Father (n = 71) | 0.2 | ||||||||||||||||
| Cullen et al. (2017) [12] | Ireland (n = 240) | Mother (n = 120) | 50.2 ** | 18.5 ** | 23.8 ** | 3.1 ** | 2.8 ** | 8.8 ** | 17 | ||||||||
| Children (n = 120) | 38.7 ** | 26.1 ** | 41.4 ** | 5.4 ** | 3.5 ** | 17.7 ** | 32.8 | ||||||||||
| Covaci et al. (2015) [11] | Six European states | Mother (n = 639) | 1.94 * | ||||||||||||||
| Children (n = 653) | 1.96 * | ||||||||||||||||
| Cutanda et al. (2015) [13] | Spain (n = 240) | Mother (n = 120) | 150.8 ** | 30.59 ** | 35.03 ** | 7.99 ** | 9.52 ** | 6.65 ** | 12.96 ** | 20.07 ** | 1.97 ** | ||||||
| Children (n = 120) | 198.9 ** | 50.95 ** | 61.38 ** | 13.9 ** | 15.13 ** | 6.85 ** | 24.28 ** | 38.36 ** | 2.01 ** | ||||||||
| Bamai et al. (2015) [9] | Japan (n = 303) | Mother (n = 125) | <LOD | 47.3 * | 11.6 * | 28.6 * | 47.3 * | 7.5 * | |||||||||
| School-age (n = 178) | <LOD | 47 * | 16.3 * | 19.7 * | 51.5 * | 34.9 * | |||||||||||
| Myridakis et al. (2015) [20] | Greece (n = 478) | Mothers (n = 239) | 134 | 36.1 | 39.2 | 6 | 7.6 | 17.6 | 25.7 | 1.2 | 98 | 3 | |||||
| Children (n = 239) | 34.4 | 23.9 | 34.4 | 6.5 | 2.8 | 20 | 30.5 | 2.1 | 17 | 93 | |||||||
| Larsson et al. (2014) [18] | Sweden (n = 196) | Mothers (n = 98) | 37 | 58.49 | 10.83 | 2.4 | 7.34 | 13.17 | 10.04 | 1.2 | <LOD | 40 | 2 | 14 | |||
| Children (n = 98) | 27.4 | 83.24 | 22.37 | 3.19 | 17.74 | 26.69 | 23.12 | 1.5 | <LOD | 5.5 | 1 | 2.1 | |||||
| Polinski et al. (2014) [21] | Poland (n = 313) | 3rd Preg (n = 165) | 22.7 | 4.6 | 11.1 | 0.2 | 1.6 | 2.73 | |||||||||
| Children (n = 148) | 9.8 * | 4 * | 2.5 * | 0.2 * | 1.2 * | 2.1 * | |||||||||||
| Enke et al. (2013) [14] | Germany (n = 18) | Mothers (n = 9) | 61.4 * | 14.3 * | 15.3 * | 3.3 * | 4.8 * | 5.6 * | 10.4 * | ||||||||
| Newborn (n = 9) | 11.4 * | 22.5 * | 6.5 * | 0.9 * | 1.3 * | 1.7 * | 11.9 * | ||||||||||
| Frederiksen et al. (2013) [15] | Denmark (n = 288) | Mothers (n = 145) | 29 | 21 | 37 | 1.7 | 6.2 | 13 | 8.7 | 2.1 | 0.7 | 16 | 1 | ||||
| Children (n = 143) | 19 | 33 | 58 | 2.2 | 11 | 22 | 16 | 1.9 | 0.5 | 2.9 | 0 | <LOD | |||||
| Song et al. (2013) [22] | South Korea (n = 657) | Mothers (n = 265) | 10.9 | 25.9 | 29.6 | ||||||||||||
| Children (n = 392) | 20.9 | 116.6 | 115.2 | ||||||||||||||
| Kasper-Sonnenberg et al. (2012) [17] | Germany (n = 208) | Mothers (n = 104) | 53.8 * | 30.9 * | 43 * | 6.3 * | 4.6 * | 12.9 * | 17.3 * | 20.5 * | |||||||
| Children (n = 104) | 33.6 * | 54.2 * | 68.7 * | 11.7 * | 4 * | 26.4 * | 31 * | 42.1 * | |||||||||
| Casas et al. (2011) [10] | Spain (n = 150) | Preg (n = 120) | 324 | 27.5 | 29.9 | 10.5 | 4.4 | 15.7 | 17.3 | 32.20 | 4 | 2.2 | 6.1 | 191 | 9 | 30 | |
| Children (n = 30) | 755 | 30.2 | 41.9 | 33 | 6.2 | 44.6 | 57.4 | 115 | 7.5 | 4.2 | 1.2 | 150 | 8 | 22 | |||
| Lin et al. (2011) [19] | Taiwan (n = 189) | Preg (n = 100) | 87.49 | 15.2 | 2.07 | 16.37 | 29.5 | 33.2 | 44.69 | ||||||||
| 5 yrs old (n = 59) | 154.53 | 54 | 7.64 | 21.38 | 58.71 | 60.05 | 131.86 | ||||||||||
| 2 yrs old (n = 30) | 314 | 51 | 11.25 | 21.04 | 114.33 | 150.85 | 202.62 | ||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.H.; Kang, D.R.; Kwak, J.M.; Lee, J.K. Concentration and Variability of Urinary Phthalate Metabolites, Bisphenol A, Triclosan, and Parabens in Korean Mother–Infant Pairs. Sustainability 2020, 12, 8516. https://doi.org/10.3390/su12208516
Kim JH, Kang DR, Kwak JM, Lee JK. Concentration and Variability of Urinary Phthalate Metabolites, Bisphenol A, Triclosan, and Parabens in Korean Mother–Infant Pairs. Sustainability. 2020; 12(20):8516. https://doi.org/10.3390/su12208516
Chicago/Turabian StyleKim, Ju Hee, Dae Ryong Kang, Jung Min Kwak, and Jung Kuk Lee. 2020. "Concentration and Variability of Urinary Phthalate Metabolites, Bisphenol A, Triclosan, and Parabens in Korean Mother–Infant Pairs" Sustainability 12, no. 20: 8516. https://doi.org/10.3390/su12208516
APA StyleKim, J. H., Kang, D. R., Kwak, J. M., & Lee, J. K. (2020). Concentration and Variability of Urinary Phthalate Metabolites, Bisphenol A, Triclosan, and Parabens in Korean Mother–Infant Pairs. Sustainability, 12(20), 8516. https://doi.org/10.3390/su12208516





