Government Intervention, Human Mobility, and COVID-19: A Causal Pathway Analysis from 121 Countries
Abstract
:1. Introduction
2. Literature Review
3. Model Specification and Data Sources
3.1. Model Specification
3.1.1. Causal Model and Its Structural Equation Form
- (1)
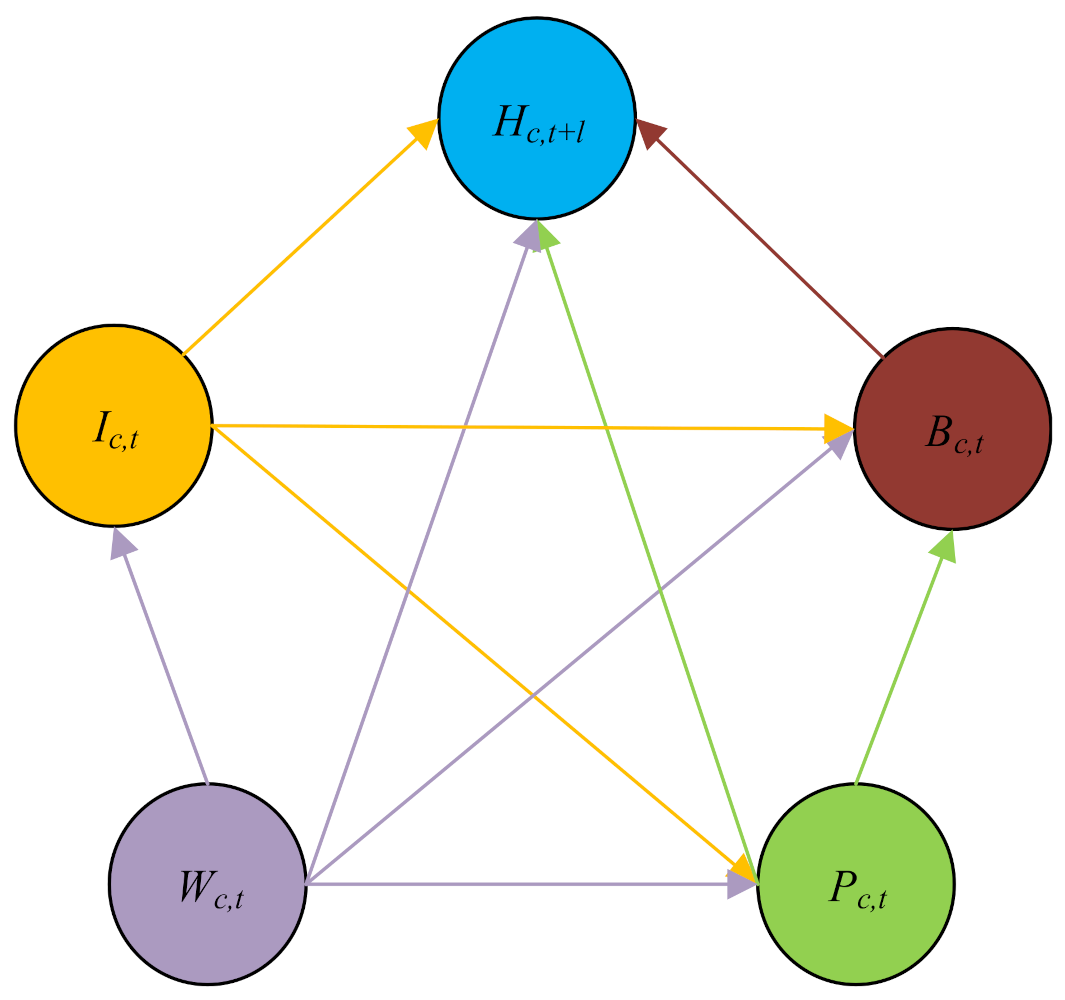
- Confounding factors Wc,t influence information variables Ic,t, government epidemic prevention policies Pc,t, human mobility behaviors Bc,t, and anti-epidemic outcomes Hc,t+l, as shown by the four purple directed lines in Figure 1.
- (2)
- Information variables Ic,t influence government epidemic prevention policies Pc,t, human mobility behaviors Bc,t, and anti-epidemic outcomes Hc,t+l, as shown by the three yellow directed lines in Figure 1.
- (3)
- As shown by the two green directed lines in Figure 1. Government epidemic prevention policies Pc,t not only directly affects human mobility behaviors Bc,t and anti-epidemic outcomes Hc,t+l, but also indirectly affects anti-epidemic outcomes through behavioral variables.
- (4)
- Human mobility behaviors Bc,t have a direct effect on the anti-epidemic outcomes Hc,t+l, as shown by the brown directed line in Figure 1.
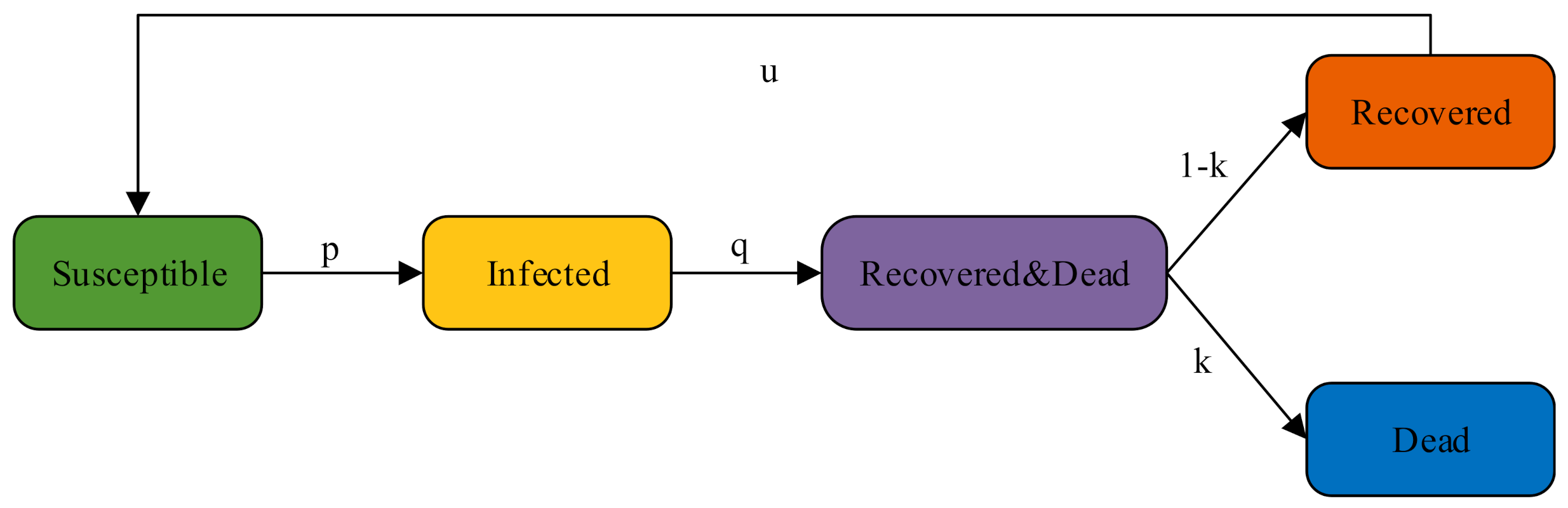
3.1.2. SIRDS Epidemic Model
3.1.3. Counterfactual Policy Analysis
3.2. Data Source
4. Empirical Analysis
4.1. The Effect of Policies and Information on Behaviors
4.2. The Direct Effect of Policies, Behaviors, and Information on Cases and Deaths Growth
4.3. The Total Effect of Policies and Information on Cases and Deaths Growth When Causal Pathways Are Not Considered
4.4. The Direct, Indirect, and Total Effects of Government Epidemic Prevention Policies and Information on Anti-Epidemic Outcomes
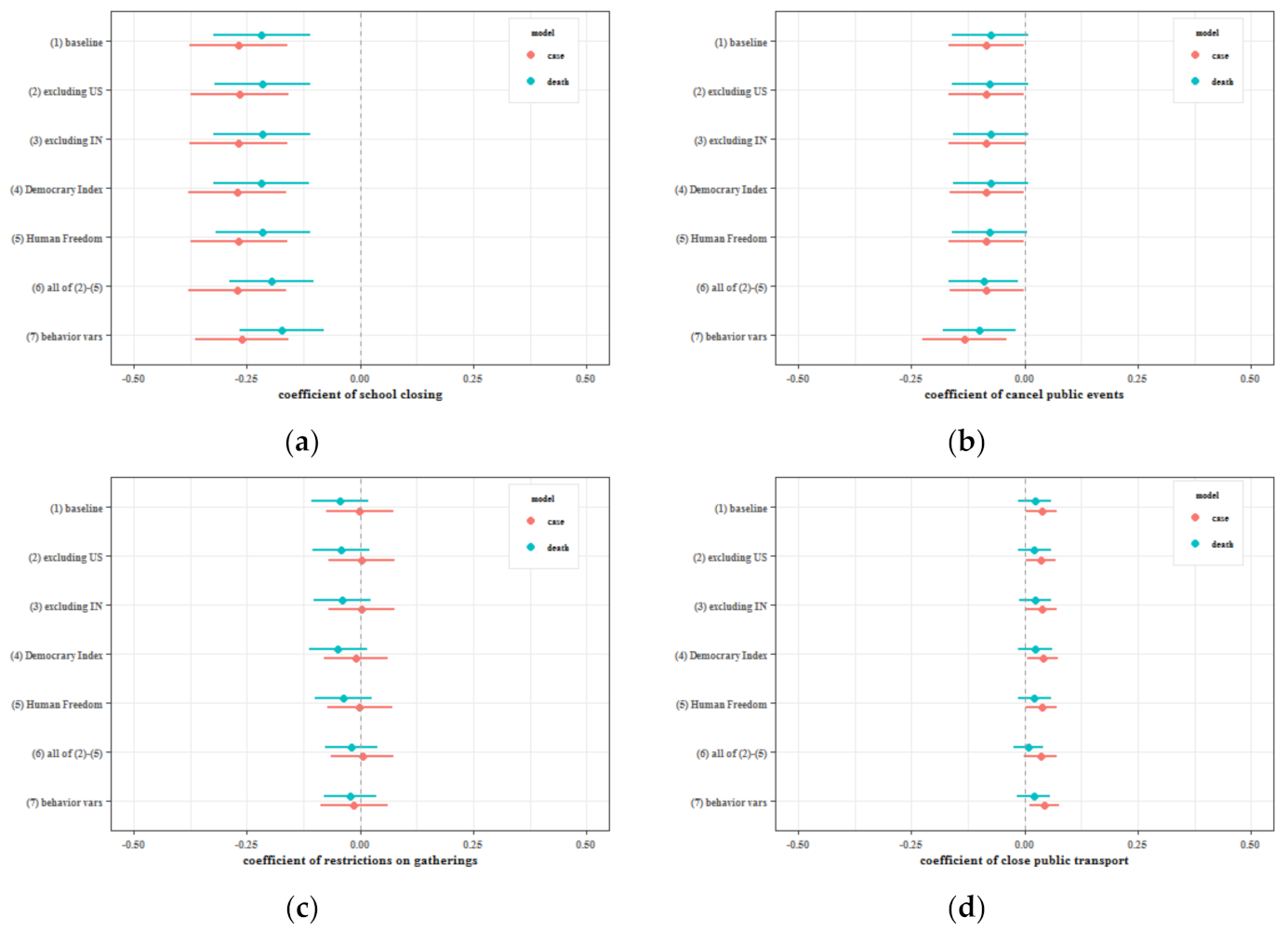
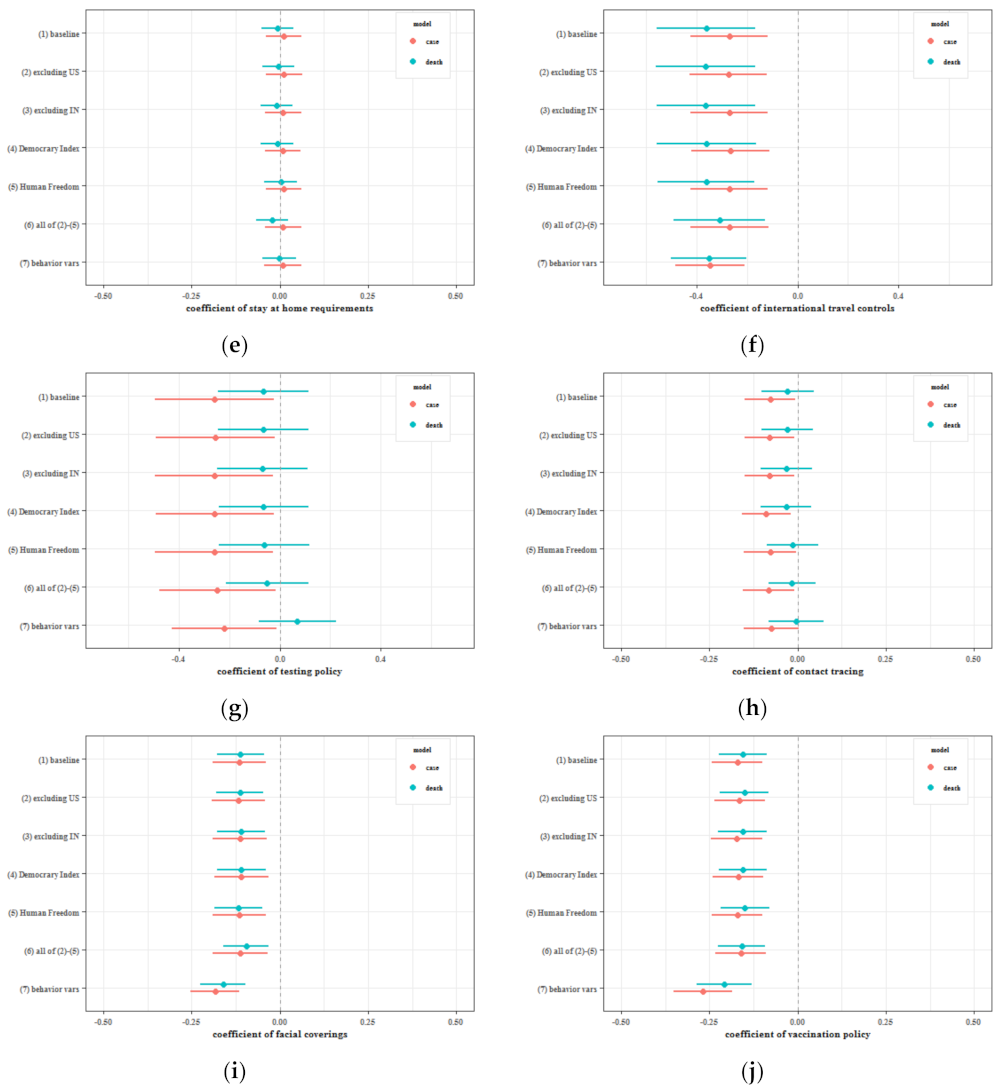
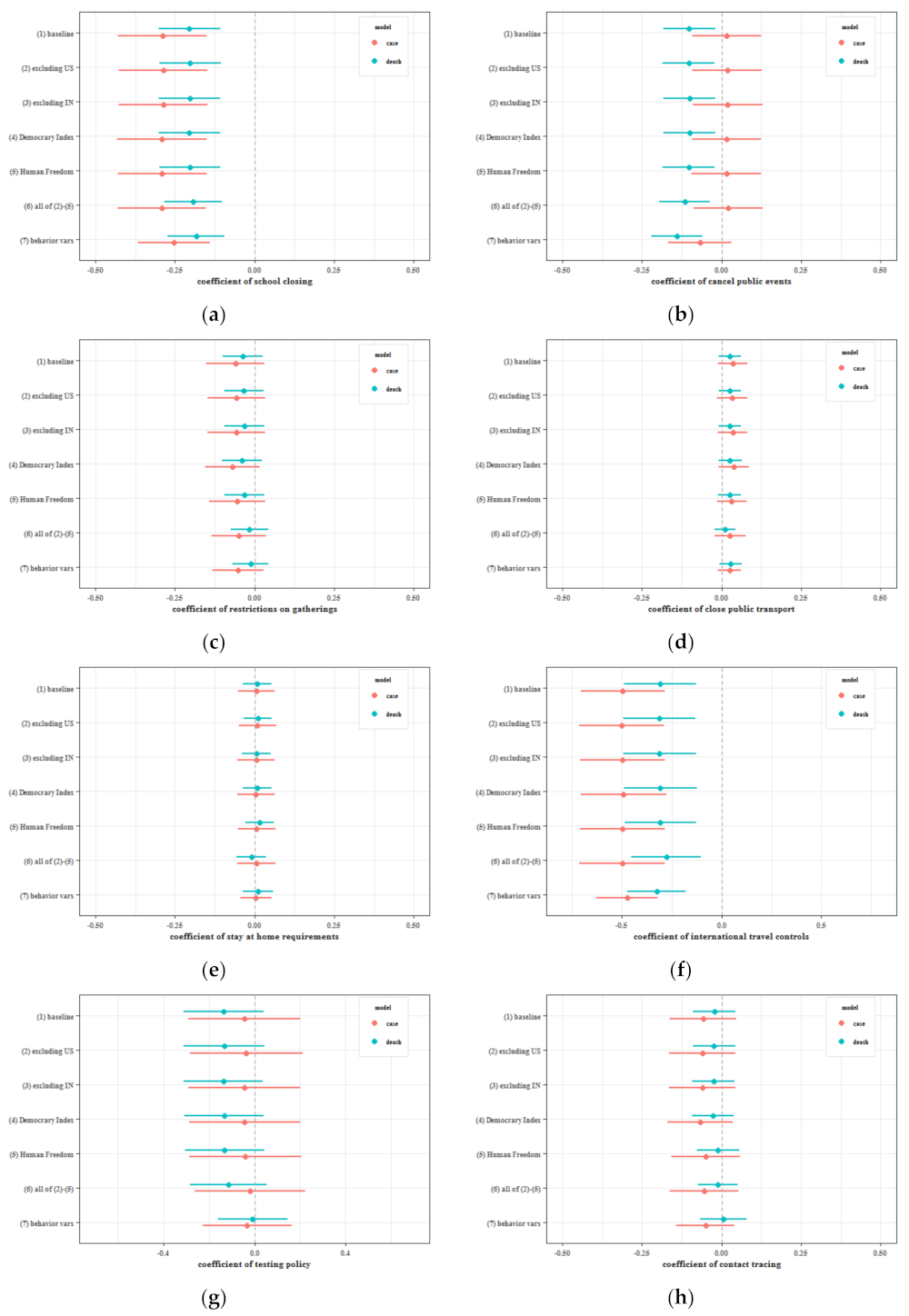
5. Sensitivity Analysis
5.1. Excluding Special Samples and Changing Variables
- (1)
- Baseline model.
- (2)
- Exclude the United States from the sample because it was the developed country with the highest cumulative number of confirmed cases.
- (3)
- Exclude India from the sample because it was the developing country with the highest cumulative number of confirmed cases.
- (4)
- Add the democracy index to the regression variables.
- (5)
- Add the human freedom index to the regression variables.
- (6)
- Include all additional controls in (2)–(5).
- (7)
- Use the lagged terms of human behavioral variables as informative variables.
5.2. Changing Time Lag
6. Counterfactual Policy Analysis
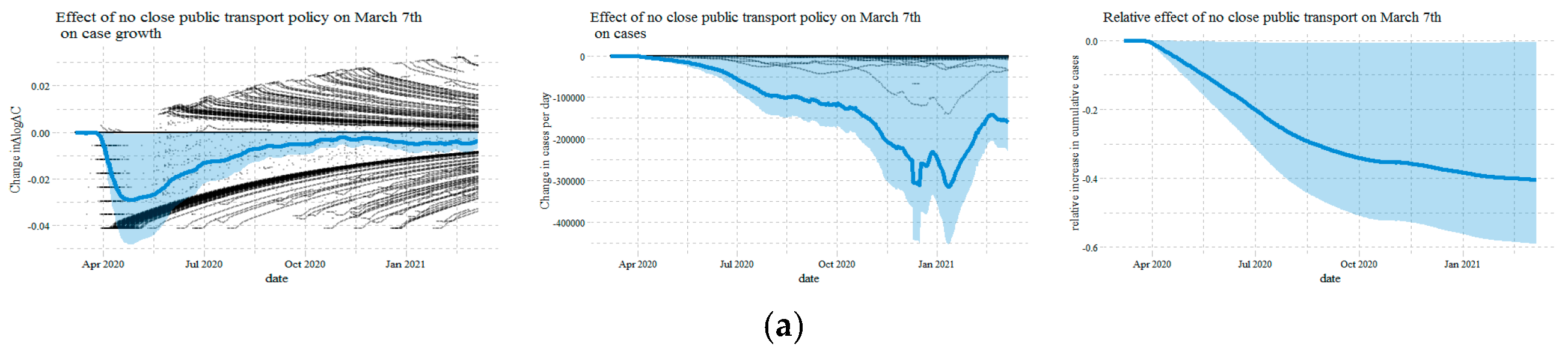
6.1. Mandating Facial Coverings
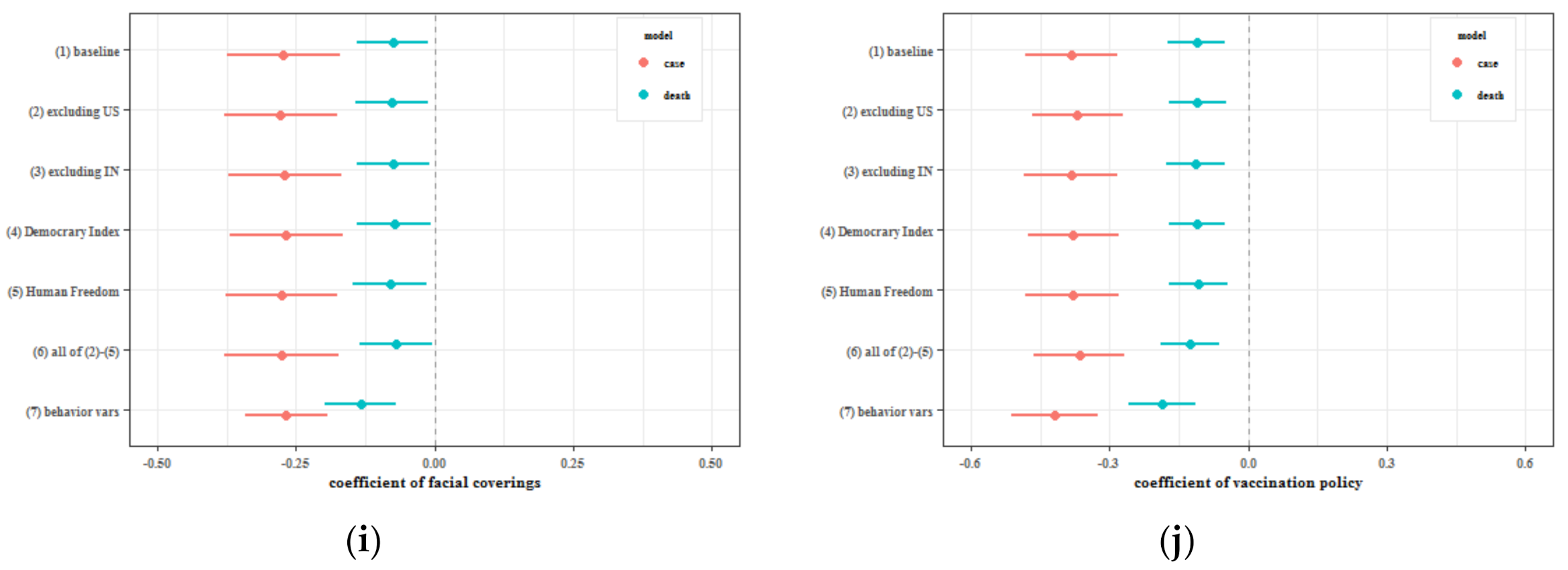
6.2. Mandating Vaccination Policy
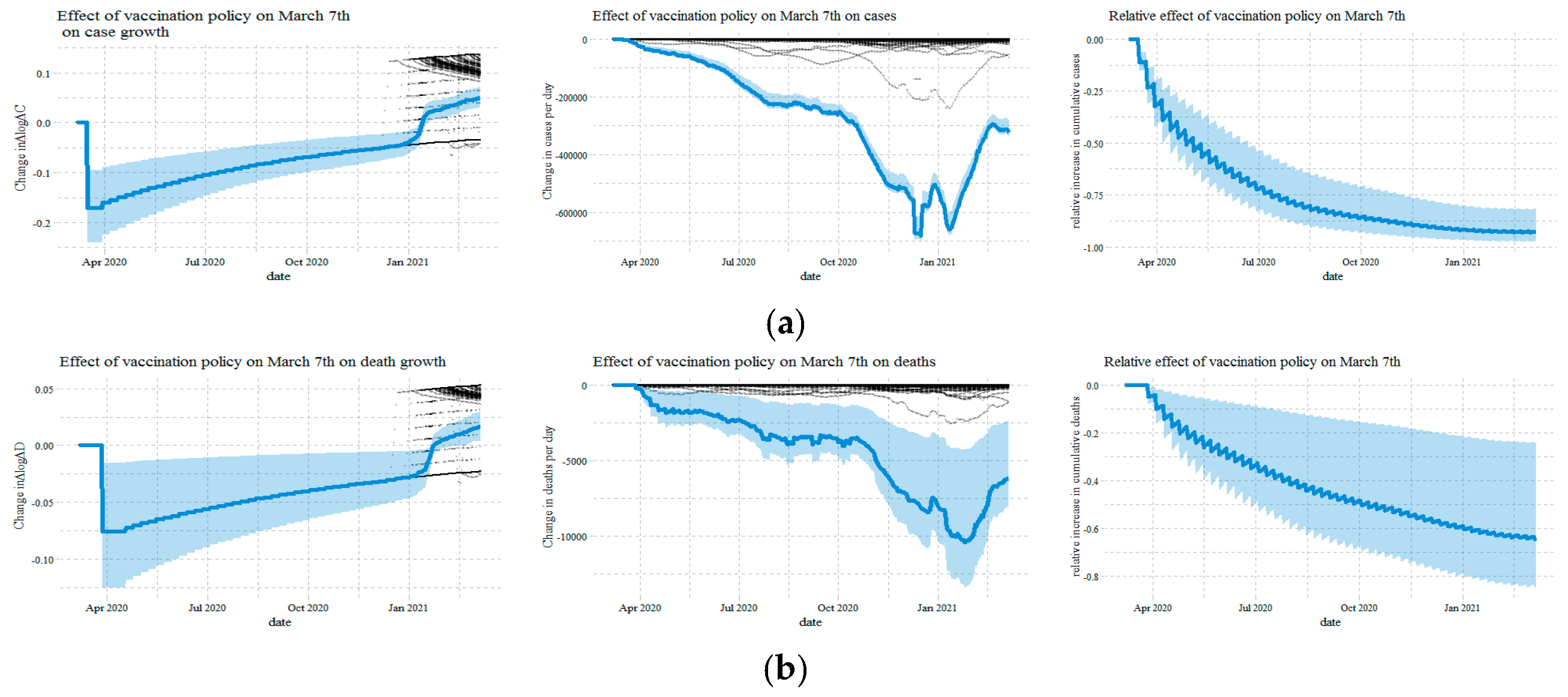
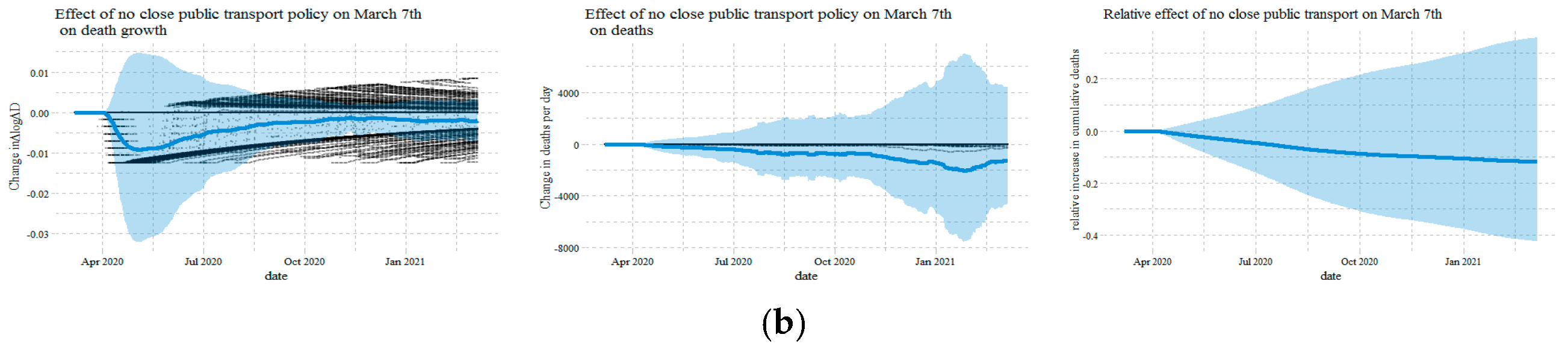
6.3. No Close Public Transport Policy
7. Discussion
8. Conclusions and Policy Implications
8.1. Conclusions
8.2. Policy Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chen, H.; Shi, L.; Zhang, Y.; Wang, X.; Jiao, J.; Yang, M.; Sun, G. Response to the COVID-19 Pandemic: Comparison of Strategies in Six Countries. Front. Public Health 2021, 9, 708496. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Y. Comparison between two types of control strategies for the coronavirus disease 2019 pandemic. J. Infect. Dev. Ctries. 2020, 14, 696–698. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Chen, X.; Shi, W. Impacts of social and economic factors on the transmission of coronavirus disease 2019 (COVID-19) in China. J. Popul. Econ. 2020, 33, 1127–1172. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Huang, J.; Gu, Q.; Du, P.; Liang, H.; Dong, Q. Optimal temperature zone for the dispersal of COVID-19. Sci. Total Environ. 2020, 736, 139487. [Google Scholar] [CrossRef]
- Chien, L.C.; Chen, L.W. Meteorological impacts on the incidence of COVID-19 in the US. Stoch. Environ. Res. Risk Assess. 2020, 34, 1675–1680. [Google Scholar] [CrossRef]
- Selcuk, M.; Gormus, S.; Guven, M. Impact of Weather Parameters and Population Density on the COVID-19 Transmission: Evidence from 81 Provinces of Turkey. Earth Syst. Environ. 2021, 5, 87–100. [Google Scholar] [CrossRef]
- Bolaño-Ortiz, T.R.; Camargo-Caicedo, Y.; Puliafito, S.E.; Ruggeri, M.F.; Bolaño-Diaz, S.; Pascual-Flores, R.; Saturno, J.; Ibarra-Espinosa, S.; Mayol-Bracero, O.L.; Torres-Delgado, E.; et al. Spread of SARS-CoV-2 through Latin America and the Caribbean region: A look from its economic conditions, climate and air pollution indicators. Environ. Res. 2020, 191, 109938. [Google Scholar] [CrossRef]
- Bretschger, L.; Grieg, E.; Welfens, P.J.J.; Xiong, T. COVID-19 infections and fatalities developments: Empirical evidence for OECD countries and newly industrialized economies. Int. Econ. Econ. Policy 2020, 17, 801–847. [Google Scholar] [CrossRef]
- Kozlovskyi, S.; Bilenko, D.; Dluhopolskyi, O.; Vitvitskyi, S.; Bondarenko, O.; Korniichuk, O. Determinants of COVID-19 Death Rate in Europe: Empirical Analysis. Probl. Ekorozw. 2021, 16, 17–28. [Google Scholar] [CrossRef]
- Chennakesavulu, K.; Reddy, G.R. The effect of latitude and PM2. 5 on spreading of SARS-CoV-2 in tropical and temperate zone countries. Environ. Pollut. 2020, 266, 115176. [Google Scholar] [CrossRef]
- Vera-Valdés, J.E. The political risk factors of COVID-19. Int. Rev. Appl. Econ. 2021, 35, 269–287. [Google Scholar] [CrossRef]
- Baniamin, H.M.; Rahman, M.; Hasan, M.T. The COVID-19 pandemic: Why are some countries coping more successfully than others? Asia Pac. J. Public Adm. 2020, 42, 153–169. [Google Scholar] [CrossRef]
- David, A.C.; Pienknagura, S. On the effectiveness of containment measures in controlling the COVID-19 pandemic: The role of labour market characteristics and governance. Appl. Econ. Lett. 2021, 28, 1641–1647. [Google Scholar] [CrossRef]
- Chernozhukov, V.; Kasahara, H.; Schrimpf, P. Causal impact of masks, policies, behavior on early COVID-19 pandemic in the U.S. J. Econ. 2021, 220, 23–62. [Google Scholar] [CrossRef]
- Perone, G. The determinants of COVID-19 case fatality rate (CFR) in the Italian regions and provinces: An analysis of environmental, demographic, and healthcare factors. Sci. Total Environ. 2021, 755, 142523. [Google Scholar] [CrossRef]
- Moosa, I.A.; Khatatbeh, I.N. Robust and fragile determinants of the infection and case fatality rates of Covid-19: International cross-sectional evidence. Appl. Econ. 2021, 53, 1225–1234. [Google Scholar] [CrossRef]
- Ecks, S. Multimorbidity, Polyiatrogenesis, and COVID-19. Med. Anthropol. Q. 2020, 34, 488–503. [Google Scholar] [CrossRef]
- Fang, H.; Wang, L.; Yang, Y. Human mobility restrictions and the spread of the novel coronavirus (2019-nCoV) in China. J. Popul. Econ. 2020, 191, 104272. [Google Scholar] [CrossRef]
- Coker, E.S.; Cavalli, L.; Fabrizi, E.; Guastella, G.; Lippo, E.; Parisi, M.L.; Pontarollo, N.; Rizzati, M.; Varacca, A.; Vergalli, S. The effects of air pollution on COVID-19 related mortality in northern Italy. Environ. Resour. Econ. 2020, 76, 611–634. [Google Scholar] [CrossRef]
- Ang, J.P.; Dong, F.; Patalinghug, J. COVID-19: Effectiveness of socioeconomic factors in containing the spread and mortality. Int. Rev. Appl. Econ. 2021, 35, 164–187. [Google Scholar] [CrossRef]
- Łuczak, A.; Kalinowski, S. Fuzzy Clustering Methods to Identify the Epidemiological Situation and Its Changes in European Countries during COVID-19. Entropy 2021, 24, 14. [Google Scholar] [CrossRef] [PubMed]
- Dudek, M.; Śpiewak, R. Effects of the COVID-19 Pandemic on Sustainable Food Systems: Lessons Learned for Public Policies? The Case of Poland. Agriculture 2022, 12, 61. [Google Scholar] [CrossRef]
- Kalinowski, S.; Łuczak, A.; Koziolek, A. The Social Dimension of Security: The Dichotomy of Respondents’ Perceptions during the COVID-19 Pandemic. Sustainability 2022, 14, 1363. [Google Scholar] [CrossRef]
- Churski, P.; Kroczak, H.; Łuczak, M.; Shelest-Szumilas, O.; Woźniak, M. Adaptation Strategies of Migrant Workers from Ukraine during the COVID-19 Pandemic. Sustainability 2021, 13, 8337. [Google Scholar] [CrossRef]
- Robinson, J.M.; Mzali, L.; Knudsen, D.; Farmer, J.; Spiewak, R.; Suttles, S.; Burris, M.; Shattuck, A.; Valliant, J.; Babb, A. Food after the COVID-19 Pandemic and the Case for Change Posed by Alternative Food: A Case Study of the American Midwest. Glob. Sustain. 2021, 4, e6. [Google Scholar] [CrossRef]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- Awaidy, S.A.; Mahomed, O. Impact of non-pharmaceutical interventions on the COVID-19 epidemic: A modelling study. SAGE Open Med. 2020, 8, 2050312120979462. [Google Scholar] [CrossRef]
- Chen, X.; Qiu, Z. Scenario analysis of non-pharmaceutical interventions on global COVID-19 transmissions. arXiv 2004, arXiv:2004.04529. [Google Scholar] [CrossRef]
- Lemaitre, J.C.; Perez-Saez, J.; Azman, A.S.; Rinaldo, A.; Fellay, J. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med. Wkly. 2020, 150, w20295. [Google Scholar] [CrossRef]
- Amuedo-Dorantes, C.; Borra, C.; Rivera-Garrido, N.; Sevilla, A. Early adoption of non-pharmaceutical interventions and COVID-19 mortality. Econ. Hum. Biol. 2021, 42. [Google Scholar] [CrossRef]
- Banholzer, N.; Van Weenen, E.; Lison, A.; Cenedese, A.; Seeliger, A.; Kratzwald, B.; Tschernutter, D.; Puig Salles, J.; Bottrighi, P.; Lehtinen, S.; et al. Estimating the effects of non-pharmaceutical interventions on the number of new infections with COVID-19 during the first epidemic wave. PLoS ONE 2021, 16, e0252827. [Google Scholar] [CrossRef] [PubMed]
- Jayaweera, M.; Dannangoda, C.; Dilshan, D.; Dissanayake, J.; Perera, H.; Manatunge, J.; Gunawardana, B. Grappling with COVID-19 by imposing and lifting non-pharmaceutical interventions in Sri Lanka: A modeling perspective. Infect. Dis. Model. 2021, 6, 820–831. [Google Scholar] [CrossRef] [PubMed]
- Amuedo-Dorantes, C.; Kaushal, N.; Muchow, A.N. Timing of social distancing policies and COVID-19 mortality: County-level evidence from the US. J. Popul. Econ. 2021, 34, 1445–1472. [Google Scholar] [CrossRef] [PubMed]
- Fritz, C.; Kauermann, G. On the interplay of regional mobility, social connectedness and the spread of COVID-19 in Germany. J. R. Stat. Soc. Ser. A Stat. Soc. 2021, 185, 400–424. [Google Scholar] [CrossRef]
- Zheng, Z.; Xie, Z.; Qin, Y.; Wang, K.; Yu, Y.; Fu, P. Exploring the influence of human mobility factors and spread prediction on early COVID-19 in the USA. BMC Public Health 2021, 21, 615. [Google Scholar] [CrossRef]
- Mamelund, S.E.; Dimka, J.; Bakkeli, N.Z. Social Disparities in Adopting Non-pharmaceutical Interventions During COVID-19 in Norway. J. Dev. Soc. 2021, 37, 302–328. [Google Scholar] [CrossRef]
- Turoń, K.; Kubik, A.; Chen, F. Electric Shared Mobility Services during the Pandemic: Modeling Aspects of Transportation. Energies 2021, 14, 2622. [Google Scholar] [CrossRef]
- Turoń, K.; Kubik, A. Business Innovations in the New Mobility Market during the COVID-19 with the Possibility of Open Business Model Innovation. J. Open Innov. Technol. Mark. Complex. 2021, 7, 195. [Google Scholar] [CrossRef]
- Marín-Hernández, D.; Nixon, D.F.; Hupert, N. Anticipated reduction in COVID-19 mortality due to population-wide BCG vaccination: Evidence from Germany. Hum. Vaccines Immunother. 2021, 17, 2451–2453. [Google Scholar] [CrossRef]
- Giordano, G.; Colaneri, M.; di Filippo, A.; Blanchini, F.; Bolzern, P.; de Nicolao, G.; Sacchi, P.; Colaneri, P.; Bruno, R. Modeling vaccination rollouts, SARS-CoV-2 variants and the requirement for non-pharmaceutical interventions in Italy. Nat. Med. 2021, 27, 993–998. [Google Scholar] [CrossRef]
- Linton, N.M.; Kobayashi, T.; Yang, Y.; Hayashi, K.; Akhmetzhanov, A.R.; Jung, S.; Yuan, B.; Kinoshita, R.; Nishiura, H. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: A statistical analysis of publicly available case data. J. Clin. Med. 2020, 9, 538. [Google Scholar] [CrossRef] [Green Version]
- Seres, G.; Balleyer, A.; Cerutti, N.; Friedrichsen, J.; Süer, M. Face Mask Use and Physical Distancing Before and After Mandatory Masking: Evidence from Public Waiting Lines; WZB Discussion Paper; Wissenschaftszentrum Berlin für Sozialforschung (WZB): Berlin, Germany, 2020; Available online: https://www.econstor.eu/handle/10419/222483 (accessed on 2 March 2022).


| Country | Country | Country | Country |
|---|---|---|---|
| Angola | Fiji | Mali | Serbia |
| Argentina | Finland | Malta | Singapore |
| Australia | France | Mexico | Slovakia |
| Austria | Gabon | Moldova | Slovenia |
| Bahrain | Georgia | Mongolia | South Africa |
| Bangladesh | Germany | Morocco | South Korea |
| Barbados | Ghana | Mozambique | Spain |
| Belarus | Greece | Myanmar | Sri Lanka |
| Belgium | Guatemala | Namibia | Sweden |
| Belize | Haiti | Nepal | Switzerland |
| Benin | Honduras | Netherlands | Tajikistan |
| Bolivia | Hungary | New Zealand | Tanzania |
| Bosnia and Herzegovina | India | Nicaragua | Thailand |
| Botswana | Indonesia | Niger | The Bahamas |
| Brazil | Iraq | Nigeria | Togo |
| Bulgaria | Ireland | Norway | Trinidad and Tobago |
| Burkina Faso | Israel | Oman | Turkey |
| Cambodia | Italy | Pakistan | Uganda |
| Cameroon | Jamaica | Panama | Ukraine |
| Canada | Japan | Papua New Guinea | United Arab Emirates |
| Cape Verde | Jordan | Paraguay | United Kingdom |
| Chile | Kazakhstan | Peru | United States |
| Colombia | Kenya | Philippines | Uruguay |
| Costa Rica | Kuwait | Poland | Venezuela |
| Croatia | Kyrgyzstan | Portugal | Vietnam |
| Czechia | Laos | Qatar | Yemen |
| Denmark | Latvia | Romania | Zambia |
| Ecuador | Lebanon | Russia | Zimbabwe |
| Egypt | Lithuania | Rwanda | |
| El Salvador | Luxembourg | Saudi Arabia | |
| Estonia | Malaysia | Senegal | |
| (a) Cases as Information | Workplaces | Retail | Transit | Grocery |
| school closing | −0.078 *** | −0.085 *** | −0.074 ** | −0.067 * |
| (0.022) | (0.028) | (0.029) | (0.036) | |
| cancel public events | 0.005 | −0.024 | −0.025 | −0.023 |
| (0.020) | (0.026) | (0.027) | (0.031) | |
| restrictions on gatherings | −0.056 *** | −0.045 | −0.051 | −0.040 |
| (0.021) | (0.032) | (0.035) | (0.035) | |
| close public transport | −0.033 *** | −0.068 *** | −0.053 *** | −0.042 *** |
| (0.013) | (0.016) | (0.020) | (0.015) | |
| stay at home requirements | −0.050 *** | −0.067 *** | −0.080 *** | −0.045 ** |
| (0.010) | (0.016) | (0.024) | (0.018) | |
| international travel controls | −0.023 | −0.017 | −0.052 ** | −0.0004 |
| (0.024) | (0.029) | (0.024) | (0.027) | |
| testing | −0.061 *** | −0.039 | −0.068 ** | −0.042 |
| (0.017) | (0.030) | (0.032) | (0.033) | |
| contact tracing | 0.031 * | 0.048 ** | −0.003 | 0.041 ** |
| (0.018) | (0.020) | (0.022) | (0.019) | |
| facial coverings | 0.077 *** | 0.100 *** | 0.095 *** | 0.088 *** |
| (0.015) | (0.024) | (0.021) | (0.019) | |
| vaccination | 0.011 | 0.002 | −0.016 | 0.020 |
| (0.017) | (0.023) | (0.029) | (0.021) | |
| dlogdc | 0.015 *** | 0.013 *** | 0.010 *** | 0.003 |
| (0.002) | (0.003) | (0.003) | (0.003) | |
| logdc | −0.009 *** | −0.014 *** | −0.003 | −0.002 |
| (0.003) | (0.003) | (0.004) | (0.003) | |
| country variables | YES | YES | YES | YES |
| quarter × country variables | YES | YES | YES | YES |
| observations | 44,891 | 44,891 | 44,891 | 44,891 |
| adjusted R2 | 0.4043 | 0.5179 | 0.4641 | 0.3676 |
| (b) Deaths as Information | Workplaces | Retail | Transit | Grocery |
| school closing | −0.082 *** | −0.090 *** | −0.074 ** | −0.067 * |
| (0.022) | (0.028) | (0.029) | (0.035) | |
| cancel public events | 0.003 | −0.025 | −0.021 | −0.022 |
| (0.021) | (0.026) | (0.027) | (0.030) | |
| restrictions on gatherings | −0.063 *** | −0.054 * | −0.053 | −0.041 |
| (0.021) | (0.032) | (0.035) | (0.035) | |
| close public transport | −0.033 ** | −0.065 *** | −0.050 ** | −0.042 *** |
| (0.013) | (0.016) | (0.020) | (0.015) | |
| stay at home requirements | −0.050 *** | −0.063 *** | −0.075 *** | −0.044 ** |
| (0.010) | (0.016) | (0.024) | (0.018) | |
| international travel controls | −0.033 | −0.028 | −0.058 ** | −0.003 |
| (0.025) | (0.030) | (0.025) | (0.027) | |
| testing | −0.075 *** | −0.061 ** | −0.071 ** | −0.045 |
| (0.017) | (0.028) | (0.031) | (0.032) | |
| contact tracing | 0.026 | 0.039 * | −0.005 | 0.039 ** |
| (0.018) | (0.020) | (0.021) | (0.019) | |
| facial coverings | 0.071 *** | 0.097 *** | 0.093 *** | 0.086 *** |
| (0.015) | (0.023) | (0.020) | (0.019) | |
| vaccination | 0.007 | 0.006 | −0.015 | 0.019 |
| (0.017) | (0.023) | (0.029) | (0.022) | |
| dlogdd | −0.0002 | −0.0005 | −0.003 | −0.003 * |
| (0.002) | (0.002) | (0.002) | (0.002) | |
| logdd | −0.009 *** | −0.015 *** | −0.006 | −0.003 |
| (0.002) | (0.003) | (0.004) | (0.003) | |
| country variables | YES | YES | YES | YES |
| quarter × country variables | YES | YES | YES | YES |
| observations | 44,891 | 44,891 | 44,891 | 44,891 |
| adjusted R2 | 0.4017 | 0.5247 | 0.4666 | 0.3689 |
| (a) Cases | dlogdc | (b) Deaths | dlogdd |
|---|---|---|---|
| lag(school closing, 14) | −0.233 *** | lag(school closing, 21) | −0.174 *** |
| (0.060) | (0.059) | ||
| lag(cancel public events, 14) | −0.093 * | lag(cancel public events, 21) | −0.079 * |
| (0.048) | (0.048) | ||
| lag(restrictions on gatherings, 14) | 0.023 | lag(restrictions on gatherings, 21) | −0.015 |
| (0.042) | (0.036) | ||
| lag(close public transport, 14) | 0.054 *** | lag(close public transport, 21) | 0.038 * |
| (0.019) | (0.021) | ||
| lag(stay at home requirements, 14) | 0.037 | lag(stay at home requirements, 21) | 0.023 |
| (0.032) | (0.029) | ||
| lag(international travel controls, 14) | −0.253 *** | lag(international travel controls, 21) | −0.336 *** |
| (0.087) | (0.113) | ||
| lag(testing, 14) | −0.235 * | lag(testing, 21) | −0.029 |
| (0.139) | (0.106) | ||
| lag(contact tracing, 14) | −0.082 * | lag(contact tracing, 21) | −0.027 |
| (0.044) | (0.043) | ||
| lag(facial coverings, 14) | −0.133 *** | lag(facial coverings, 21) | −0.126 *** |
| (0.044) | (0.039) | ||
| lag(vaccination, 14) | −0.158 *** | lag(vaccination, 21) | −0.144 *** |
| (0.045) | (0.041) | ||
| lag(workplaces, 14) | 0.474 *** | lag(workplaces, 21) | 0.399 *** |
| (0.140) | (0.125) | ||
| lag(retail, 14) | 0.168 | lag(retail, 21) | 0.079 |
| (0.152) | (0.123) | ||
| lag(transit, 14) | 0.148 | lag(transit, 21) | 0.246 ** |
| (0.106) | (0.102) | ||
| lag(grocery, 14) | −0.412 *** | lag(grocery, 21) | −0.323 *** |
| (0.116) | (0.103) | ||
| lag(dlogdc, 14) | 0.048 *** | lag(dlogdd, 21) | 0.050 *** |
| (0.017) | (0.012) | ||
| lag(logdc, 14) | −0.028 *** | lag(logdd, 21) | −0.021 *** |
| (0.006) | (0.004) | ||
| dlogtests | 0.019 ** | ||
| (0.009) | |||
| country variables | YES | country variables | YES |
| quarter × country variables | YES | quarter × country variables | YES |
| observations | 42,472 | observations | 42,350 |
| adjusted R2 | 0.1082 | adjusted R2 | 0.0455 |
| (a) Cases | dlogdc | (b) Deaths | dlogdd |
|---|---|---|---|
| lag(school closing, 14) | −0.268 *** | lag(school closing, 21) | −0.217 *** |
| (0.066) | (0.065) | ||
| lag(cancel public events, 14) | −0.084 * | lag(cancel public events, 21) | −0.075 |
| (0.051) | (0.051) | ||
| lag(restrictions on gatherings, 14) | −0.0005 | lag(restrictions on gatherings, 21) | −0.044 |
| (0.045) | (0.039) | ||
| lag(close public transport, 14) | 0.038 * | lag(close public transport, 21) | 0.023 |
| (0.020) | (0.022) | ||
| lag(stay at home requirements, 14) | 0.010 | lag(stay at home requirements, 21) | −0.007 |
| (0.031) | (0.028) | ||
| lag(international travel controls, 14) | −0.271 *** | lag(international travel controls, 21) | −0.362 *** |
| (0.093) | (0.119) | ||
| lag(testing, 14) | −0.261 * | lag(testing, 21) | −0.066 |
| (0.143) | (0.109) | ||
| lag(contact tracing, 14) | −0.078 * | lag(contact tracing, 21) | −0.028 |
| (0.043) | (0.045) | ||
| lag(facial coverings, 14) | −0.115 ** | lag(facial coverings, 21) | −0.111 *** |
| (0.046) | (0.040) | ||
| lag(vaccination, 14) | −0.171 *** | lag(vaccination, 21) | −0.155 *** |
| (0.044) | (0.042) | ||
| lag(dlogdc, 14) | 0.057 *** | lag(dlogdd, 21) | 0.052 *** |
| (0.017) | (0.012) | ||
| lag(logdc, 14) | −0.035 *** | lag(logdd, 21) | −0.026 *** |
| (0.006) | (0.004) | ||
| dlogtests | 0.019 ** | ||
| (0.009) | |||
| country variables | YES | country variables | YES |
| quarter × country variables | YES | quarter × country variables | YES |
| observations | 42,472 | observations | 42,350 |
| adjusted R2 | 0.1025 | adjusted R2 | 0.0417 |
| (a) Cases | Direct Effect | Indirect Effect | Total Effect | Average | Difference | |
| Considering Causal Pathways | Not Considering Causal Pathways | |||||
| school closing | −0.233 *** | −0.035 ** | −0.268 *** | −0.268 *** | −0.268 *** | 0.000 |
| (0.059) | (0.014) | (0.064) | (0.065) | (0.064) | (0.005) | |
| cancel public events | −0.093 * | 0.004 | −0.089 * | −0.084 * | −0.087 * | −0.005 |
| (0.048) | (0.012) | (0.051) | (0.051) | (0.051) | (0.005) | |
| restrictions on gatherings | 0.023 | −0.025 ** | −0.002 | −0.000 | −0.001 | −0.002 |
| (0.042) | (0.012) | (0.045) | (0.045) | (0.045) | (0.005) | |
| close public transport | 0.054 *** | −0.018 * | 0.036 * | 0.038 * | 0.037 * | −0.001 |
| (0.019) | (0.010) | (0.021) | (0.021) | (0.021) | (0.003) | |
| stay at home requirements | 0.037 | −0.028 *** | 0.009 | 0.010 | 0.009 | −0.002 |
| (0.032) | (0.009) | (0.030) | (0.030) | (0.030) | (0.003) | |
| international travel controls | −0.253 *** | −0.021 | −0.274 *** | −0.271 *** | −0.273 *** | −0.003 |
| (0.087) | (0.014) | (0.095) | (0.093) | (0.094) | (0.005) | |
| testing | −0.235 * | −0.028 ** | −0.263 * | −0.261 * | −0.262 * | −0.002 |
| (0.136) | (0.011) | (0.140) | (0.140) | (0.140) | (0.006) | |
| contact tracing | −0.082 * | 0.005 | −0.077 * | −0.078 * | −0.077 * | 0.001 |
| (0.043) | (0.011) | (0.043) | (0.042) | (0.042) | (0.004) | |
| facial coverings | −0.133 *** | 0.032 *** | −0.102 ** | −0.115 ** | −0.108 ** | 0.013 *** |
| (0.042) | (0.011) | (0.044) | (0.044) | (0.044) | (0.005) | |
| vaccination | −0.158 *** | −0.005 | −0.163 *** | −0.171 *** | −0.167 *** | 0.008 |
| (0.044) | (0.010) | (0.044) | (0.043) | (0.043) | (0.008) | |
| dlogdc | 0.048 *** | 0.010 *** | 0.057 *** | 0.057 *** | 0.057 *** | −0.000 |
| (0.016) | (0.002) | (0.017) | (0.017) | (0.017) | (0.001) | |
| logdc | −0.028 *** | −0.006 *** | −0.034 *** | −0.035 *** | −0.034 *** | 0.001 |
| (0.006) | (0.002) | (0.006) | (0.006) | (0.006) | (0.001) | |
| (b) Deaths | Direct Effect | Indirect Effect | Total Effect | Average | Difference | |
| Considering Causal Pathways | Not Considering Causal Pathways | |||||
| school closing | −0.174 *** | −0.036 *** | −0.210 *** | −0.217 *** | −0.214 *** | 0.007 |
| (0.059) | (0.013) | (0.063) | (0.064) | (0.064) | (0.006) | |
| cancel public events | −0.079 * | 0.001 | −0.078 | −0.075 | −0.077 | −0.003 |
| (0.045) | (0.012) | (0.048) | (0.049) | (0.048) | (0.005) | |
| restrictions on gatherings | −0.015 | −0.029 ** | −0.044 | −0.044 | −0.044 | 0.000 |
| (0.037) | (0.012) | (0.040) | (0.040) | (0.040) | (0.005) | |
| close public transport | 0.038 * | −0.017 * | 0.021 | 0.023 | 0.022 | −0.001 |
| (0.022) | (0.009) | (0.023) | (0.023) | (0.023) | (0.002) | |
| stay at home requirements | 0.023 | −0.029 *** | −0.007 | −0.007 | −0.007 | 0.000 |
| (0.029) | (0.009) | (0.028) | (0.028) | (0.028) | (0.003) | |
| international travel controls | −0.336 *** | −0.029 ** | −0.365 *** | −0.362 *** | −0.363 *** | −0.003 |
| (0.113) | (0.013) | (0.119) | (0.118) | (0.119) | (0.005) | |
| testing | −0.029 | −0.037 *** | −0.066 | −0.066 | −0.066 | −0.000 |
| (0.103) | (0.010) | (0.106) | (0.107) | (0.106) | (0.007) | |
| contact tracing | −0.027 | −0.001 | −0.028 | −0.028 | −0.028 | 0.001 |
| (0.042) | (0.009) | (0.043) | (0.043) | (0.043) | (0.004) | |
| facial coverings | −0.126 *** | 0.031 *** | −0.095 ** | −0.111 *** | −0.103 *** | 0.017 *** |
| (0.039) | (0.011) | (0.040) | (0.041) | (0.040) | (0.006) | |
| vaccination | −0.144 *** | −0.007 | −0.150 *** | −0.155 *** | −0.153 *** | 0.005 |
| (0.041) | (0.010) | (0.042) | (0.041) | (0.041) | (0.009) | |
| dlogdd | 0.050 *** | 0.0004 | 0.050 *** | 0.052 *** | 0.051 *** | −0.002 ** |
| (0.012) | (0.001) | (0.012) | (0.012) | (0.012) | (0.001) | |
| logdd | −0.021 *** | −0.005 *** | −0.026 *** | −0.026 *** | −0.026 *** | 0.001 |
| (0.004) | (0.002) | (0.004) | (0.004) | (0.004) | (0.001) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, F.; Ge, X.; Huang, D. Government Intervention, Human Mobility, and COVID-19: A Causal Pathway Analysis from 121 Countries. Sustainability 2022, 14, 3694. https://doi.org/10.3390/su14063694
Wang F, Ge X, Huang D. Government Intervention, Human Mobility, and COVID-19: A Causal Pathway Analysis from 121 Countries. Sustainability. 2022; 14(6):3694. https://doi.org/10.3390/su14063694
Chicago/Turabian StyleWang, Feng, Xing Ge, and Danwen Huang. 2022. "Government Intervention, Human Mobility, and COVID-19: A Causal Pathway Analysis from 121 Countries" Sustainability 14, no. 6: 3694. https://doi.org/10.3390/su14063694






