Concentrations of Plasma Free Palmitoleic and Dihomo-Gamma Linoleic Fatty Acids Are Higher in Children with Abdominal Obesity
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Smith, U. Abdominal obesity: A marker of ectopic fat accumulation. J. Clin. Investig. 2015, 125, 1790–1792. [Google Scholar] [CrossRef] [PubMed]
- Rosique-Esteban, N.; Diaz-Lopez, A.; Martinez-Gonzalez, M.A.; Corella, D.; Goday, A.; Martinez, J.A.; Romaguera, D.; Vioque, J.; Aros, F.; Garcia-Rios, A.; et al. Leisure-time physical activity, sedentary behaviors, sleep, and cardiometabolic risk factors at baseline in the predimed-plus intervention trial: A cross-sectional analysis. PLoS ONE 2017, 12, e0172253. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; McNaughton, S.A.; Owen, N.; Dunstan, D.W. Independent and joint associations of tv viewing time and snack food consumption with the metabolic syndrome and its components; a cross-sectional study in australian adults. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 96. [Google Scholar] [CrossRef] [PubMed]
- Bays, H.E.; Toth, P.P.; Kris-Etherton, P.M.; Abate, N.; Aronne, L.J.; Brown, W.V.; Gonzalez-Campoy, J.M.; Jones, S.R.; Kumar, R.; La Forge, R.; et al. Obesity, adiposity, and dyslipidemia: A consensus statement from the national lipid association. J. Clin. Lipidol. 2013, 7, 304–383. [Google Scholar] [CrossRef] [PubMed]
- Bays, H. Central obesity as a clinical marker of adiposopathy; increased visceral adiposity as a surrogate marker for global fat dysfunction. Curr. Opin. Endocrinol. Diabetes Obes. 2014, 21, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Sears, B.; Perry, M. The role of fatty acids in insulin resistance. Lipids Health Dis. 2015, 14, 121. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Adipose tissue and metabolic syndrome: Too much, too little or neither. Eur. J. Clin. Investig. 2015, 45, 1209–1217. [Google Scholar] [CrossRef] [PubMed]
- Cooke, A.A.; Connaughton, R.M.; Lyons, C.L.; McMorrow, A.M.; Roche, H.M. Fatty acids and chronic low grade inflammation associated with obesity and the metabolic syndrome. Eur. J. Pharmacol. 2016, 785, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Warensjö, E.; Rosell, M.; Hellenius, M.L.; Vessby, B.; De Faire, U.; Risérus, U. Associations between estimated fatty acid desaturase activities in serum lipids and adipose tissue in humans: Links to obesity and insulin resistance. Lipids Health Dis. 2009, 8, 37. [Google Scholar] [CrossRef] [PubMed]
- Stefan, N.; Stumvoll, M.; Bogardus, C.; Tataranni, P.A. Elevated plasma nonesterified fatty acids are associated with deterioration of acute insulin response in igt but not ngt. Am. J. Physiol. Endocrinol. Metab. 2003, 284, E1156–E1161. [Google Scholar] [CrossRef] [PubMed]
- Paillard, F.; Catheline, D.; Duff, F.L.; Bouriel, M.; Deugnier, Y.; Pouchard, M.; Daubert, J.C.; Legrand, P. Plasma palmitoleic acid, a product of stearoyl-coa desaturase activity, is an independent marker of triglyceridemia and abdominal adiposity. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Boden, G. Obesity and free fatty acids. Endocrinol. Metab. Clin. N. Am. 2008, 37, 635–646. [Google Scholar] [CrossRef] [PubMed]
- Juonala, M.; Viikari, J.S.; Raitakari, O.T. Main findings from the prospective cardiovascular risk in young finns study. Curr. Opin. Lipidol. 2013, 24, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Juonala, M.; Magnussen, C.G.; Berenson, G.S.; Venn, A.; Burns, T.L.; Sabin, M.A.; Srinivasan, S.R.; Daniels, S.R.; Davis, P.H.; Chen, W.; et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N. Engl. J. Med. 2011, 365, 1876–1885. [Google Scholar] [CrossRef] [PubMed]
- Toledo-Corral, C.M.; Alderete, T.L.; Richey, J.; Sequeira, P.; Goran, M.I.; Weigensberg, M.J. Fasting, post-ogtt challenge, and nocturnal free fatty acids in prediabetic versus normal glucose tolerant overweight and obese latino adolescents. Acta Diabetol. 2015, 52, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.; Collins, C.E.; Garg, M.L. Omega-3 index, obesity and insulin resistance in children. Int. J. Pediatr. Obes. 2011, 6, e532–e539. [Google Scholar] [CrossRef] [PubMed]
- Sabin, M.A.; De Hora, M.; Holly, J.M.; Hunt, L.P.; Ford, A.L.; Williams, S.R.; Baker, J.S.; Retallick, C.J.; Crowne, E.C.; Shield, J.P. Fasting nonesterified fatty acid profiles in childhood and their relationship with adiposity, insulin sensitivity, and lipid levels. Pediatrics 2007, 120, e1426–e1433. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Kiess, W.; Andler, W. Insulin sensitivity indices of glucose and free fatty acid metabolism in obese children and adolescents in relation to serum lipids. Metabolism 2005, 54, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Chu, N.F.; Chang, J.B.; Shieh, S.M. Plasma leptin, fatty acids, and tumor necrosis factor-receptor and insulin resistance in children. Obes. Res. 2003, 11, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Bermúdez-Cardona, J.; Velásquez-Rodríguez, C. Profile of free fatty acids and fractions of phospholipids, cholesterol esters and triglycerides in serum of obese youth with and without metabolic syndrome. Nutrients 2016, 8, 54. [Google Scholar] [CrossRef] [PubMed]
- Gil-Campos, M.; del Carmen Ramírez-Tortosa, M.; Larqué, E.; Linde, J.; Aguilera, C.M.; Cañete, R.; Gil, A. Metabolic syndrome affects fatty acid composition of plasma lipids in obese prepubertal children. Lipids 2008, 43, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.S.; Wang, J.; Maynard, L.M.; Thornton, J.C.; Mei, Z.; Pierson, R.N.; Dietz, W.H.; Horlick, M. Relation of bmi to fat and fat-free mass among children and adolescents. Int. J. Obes. (Lond.) 2005, 29, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Maynard, L.M.; Wisemandle, W.; Roche, A.F.; Chumlea, W.C.; Guo, S.S.; Siervogel, R.M. Childhood body composition in relation to body mass index. Pediatrics 2001, 107, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P.; Kovacs, E.; Moreno, L.A.; Veidebaum, T.; Tornaritis, M.; Kourides, Y.; Siani, A.; Lauria, F.; Sioen, I.; Claessens, M.; et al. Percentile reference values for anthropometric body composition indices in european children from the idefics study. Int. J. Obes. (Lond.) 2014, 38 (Suppl. S2), S15–S25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcés, C.; Cano, B.; Granizo, J.J.; Benavente, M.; Viturro, E.; Gutiérrez-Guisado, J.; de Oya, I.; Lasunción, M.A.; de Oya, M. Insulin and homa in spanish prepubertal children: Relationship with lipid profile. Clin. Biochem. 2005, 38, 920–924. [Google Scholar] [CrossRef] [PubMed]
- Salgin, B.; Ong, K.K.; Thankamony, A.; Emmett, P.; Wareham, N.J.; Dunger, D.B. Higher fasting plasma free fatty acid levels are associated with lower insulin secretion in children and adults and a higher incidence of type 2 diabetes. J. Clin. Endocrinol. Metab. 2012, 97, 3302–3309. [Google Scholar] [CrossRef] [PubMed]
- Hershkop, K.; Besor, O.; Santoro, N.; Pierpont, B.; Caprio, S.; Weiss, R. Adipose insulin resistance in obese adolescents across the spectrum of glucose tolerance. J. Clin. Endocrinol. Metab. 2016, 101, 2423–2431. [Google Scholar] [CrossRef] [PubMed]
- Pagadala, M.; Kasumov, T.; McCullough, A.J.; Zein, N.N.; Kirwan, J.P. Role of ceramides in nonalcoholic fatty liver disease. Trends Endocrinol. Metab. 2012, 23, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, A.; Sugawara, S.; Okita, M.; Akahane, T.; Fukui, K.; Hashiuchi, M.; Kataoka, C.; Tsukamoto, I. Plasma fatty acid composition, estimated desaturase activities, and intakes of energy and nutrient in japanese men with abdominal obesity or metabolic syndrome. J. Nutr. Sci. Vitaminol. (Tokyo) 2009, 55, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Warensjö, E.; Risérus, U.; Vessby, B. Fatty acid composition of serum lipids predicts the development of the metabolic syndrome in men. Diabetologia 2005, 48, 1999–2005. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.E.; Egeland, G.M.; Meltzer, S.J.; Kubow, S. The association of desaturase 9 and plasma fatty acid composition with insulin resistance-associated factors in female adolescents. Metabolism 2009, 58, 158–166. [Google Scholar] [CrossRef] [PubMed]
- De Henauw, S.; Michels, N.; Vyncke, K.; Hebestreit, A.; Russo, P.; Intemann, T.; Peplies, J.; Fraterman, A.; Eiben, G.; de Lorgeril, M.; et al. Blood lipids among young children in europe: Results from the european idefics study. Int. J. Obes. (Lond.) 2014, 38 (Suppl. S2), S67–S75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peplies, J.; Jiménez-Pavón, D.; Savva, S.C.; Buck, C.; Günther, K.; Fraterman, A.; Russo, P.; Iacoviello, L.; Veidebaum, T.; Tornaritis, M.; et al. Percentiles of fasting serum insulin, glucose, hba1c and homa-ir in pre-pubertal normal weight european children from the idefics cohort. Int. J. Obes. (Lond.) 2014, 38 (Suppl. S2), S39–S47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, P.S.; Sharp, S.J.; Jansen, E.; Luben, R.N.; Khaw, K.T.; Wareham, N.J.; Forouhi, N.G. Fatty acids measured in plasma and erythrocyte-membrane phospholipids and derived by food-frequency questionnaire and the risk of new-onset type 2 diabetes: A pilot study in the european prospective investigation into cancer and nutrition (epic)-norfolk cohort. Am. J. Clin. Nutr. 2010, 92, 1214–1222. [Google Scholar] [PubMed]
- Bingham, S.A.; Gill, C.; Welch, A.; Cassidy, A.; Runswick, S.A.; Oakes, S.; Lubin, R.; Thurnham, D.I.; Key, T.J.; Roe, L.; et al. Validation of dietary assessment methods in the uk arm of epic using weighed records, and 24-hour urinary nitrogen and potassium and serum vitamin c and carotenoids as biomarkers. Int. J. Epidemiol. 1997, 26 (Suppl. S1), S137–S151. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.; Roche, A.; Martorell, R. Antropometric Standardization Reference Manual; Human Kinetics Publishers: Champaign, IL, USA, 1988; pp. 2–80. [Google Scholar]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horswill, C.A.; Stillman, R.J.; Van Loan, M.D.; Bemben, D.A. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar] [PubMed]
- Wallace, T.M.; Matthews, D.R. The assessment of insulin resistance in man. Diabet. Med. 2002, 19, 527–534. [Google Scholar] [CrossRef] [PubMed]
- Folch, J.; Lees, M.; Sloane Stanley, G.H. A simple method for the isolation and purification of total lipides from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar] [PubMed]
- Hodson, L.; Skeaff, C.M.; Fielding, B.A. Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog. Lipid Res. 2008, 47, 348–380. [Google Scholar] [CrossRef] [PubMed]
- Bjermo, H.; Risérus, U. Role of hepatic desaturases in obesity-related metabolic disorders. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Lönnroth, P.; Digirolamo, M.; Krotkiewski, M.; Smith, U. Insulin binding and responsiveness in fat cells from patients with reduced glucose tolerance and type ii diabetes. Diabetes 1983, 32, 748–754. [Google Scholar] [CrossRef] [PubMed]
- Arner, P.; Bolinder, J.; Engfeldt, P.; Hellmér, J.; Ostman, J. Influence of obesity on the antilipolytic effect of insulin in isolated human fat cells obtained before and after glucose ingestion. J. Clin. Investig. 1984, 73, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Paolisso, G.; Tataranni, P.A.; Foley, J.E.; Bogardus, C.; Howard, B.V.; Ravussin, E. A high concentration of fasting plasma non-esterified fatty acids is a risk factor for the development of niddm. Diabetologia 1995, 38, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Frigolet, M.E.; Gutierrez-Aguilar, R. The role of the novel lipokine palmitoleic acid in health and disease. Adv. Nutr. 2017, 8, 173s–181s. [Google Scholar] [CrossRef] [PubMed]
- Hodson, L.; Karpe, F. Is there something special about palmitoleate? Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Campos, H.; McGarvey, S.; Wu, Z.; Goldberg, R.; Baylin, A. Adipose tissue palmitoleic acid and obesity in humans: Does it behave as a lipokine? Am. J. Clin. Nutr. 2011, 93, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Scagliusi, F.B.; Ferriolli, E.; Pfrimer, K.; Laureano, C.; Cunha, C.S.; Gualano, B.; Lourenco, B.H.; Lancha, A.H., Jr. Underreporting of energy intake in brazilian women varies according to dietary assessment: A cross-sectional study using doubly labeled water. J. Am. Diet. Assoc. 2008, 108, 2031–2040. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Cao, H.; King, I.B.; Lemaitre, R.N.; Song, X.; Siscovick, D.S.; Hotamisligil, G.S. Circulating palmitoleic acid and risk of metabolic abnormalities and new-onset diabetes. Am. J. Clin. Nutr. 2010, 92, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Warensjö, E.; Ohrvall, M.; Vessby, B. Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Okada, T.; Furuhashi, N.; Kuromori, Y.; Miyashita, M.; Iwata, F.; Harada, K. Plasma palmitoleic acid content and obesity in children. Am. J. Clin. Nutr. 2005, 82, 747–750. [Google Scholar] [PubMed]
- Wang, X.; Lin, H.; Gu, Y. Multiple roles of dihomo-gamma-linolenic acid against proliferation diseases. Lipids Health Dis. 2012, 11, 25. [Google Scholar] [CrossRef] [PubMed]
- Aschner, P.; Buendía, R.; Brajkovich, I.; Gonzalez, A.; Figueredo, R.; Juarez, X.E.; Uriza, F.; Gomez, A.M.; Ponte, C.I. Determination of the cutoff point for waist circumference that establishes the presence of abdominal obesity in latin american men and women. Diabetes Res. Clin. Pract. 2011, 93, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Haffner, S.M.; Miettinen, H.; Stern, M.P. The homeostasis model in the san antonio heart study. Diabetes Care 1997, 20, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Hanley, A.J.; Williams, K.; Stern, M.P.; Haffner, S.M. Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: The san antonio heart study. Diabetes Care 2002, 25, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
| Children without Abdominal Obesity (n = 29) | Children with Abdominal Obesity (n = 29) | p-Value | |
|---|---|---|---|
| Age (years) | 7.1 ± 2.6 | 7.2 ± 2.7 | 0.876 |
| Energy intake (kcal/day) | 2453 ± 946 | 2358 ± 781 | 0.704 |
| Carbohydrate intake (g/day) | 307.8 ± 134.6 | 278.6 ± 92.4 | 0.374 |
| Protein intake (g/day) | 84.9 ± 30.7 | 92.4 ± 42.3 | 0.478 |
| Saturated fat intake (g/day) | 37.8 ± 15.1 | 37.5 ± 12.8 | 0.942 |
| Monounsaturated fat intake (g/day) | 40.1 ± 17.8 | 40.2 ± 14.5 | 0.975 |
| Polyunsaturated fat intake (g/day) | 15.5 ± 8.4 | 14.1 ± 5.6 | 0.488 |
| Body height (cm) | 118.8 ± 16.8 | 122.4 ± 16.7 | 0.424 |
| Body weight (kg) | 22.1 ± 6.0 | 30.9 ± 10.7 | 0.000 * |
| Body mass index (kg/m2) | 15.4 (1.5) | 19.7 (3.5) | 0.000 † |
| Body mass index for age (z-score) | −0.2 ± 0.7 | 1.9 ± 0.8 | 0.000* |
| Waist circumference (cm) | 53.7 (5.8) | 64.9 (16.5) | 0.000 † |
| Skinfolds Sum (mm) | 26.5 (9.8) | 60.5 (36.8) | 0.000 † |
| Fat Percentage (%) | 16.4 ± 5.5 | 26.1 ± 6.9 | 0.000 * |
| Systolic blood pressure (mmHg) | 93.5 ± 6.4 | 98.6 ± 6.4 | 0.004 * |
| Diastolic blood pressure (mmHg) | 58.5 ± 5.3 | 61.1 ± 6.5 | 0.096 |
| Fasting blood glucose (mmol/L) | 4.9 ± 0.3 | 4.8 ± 0.3 | 0.523 |
| Fasting blood insulin (pmol/L) | 42.4 (24.3) | 70.2 (54.7) | 0.032 † |
| HOMA-IR | 1.3 (0.7) | 2.2 (1.8) | 0.051 |
| Triglycerides (mmol/L) | 0.77 (0.53) | 0.87 (0.45) | 0.363 |
| Total cholesterol (mmol/L) | 4.12 (1.26) | 3.97 (1.15) | 0.363 |
| HDL-C (mmol/L) | 1.4 ± 0.3 | 1.3 ± 0.3 | 0.051 |
| LDL-C (mmol/L) | 2.3 ± 0.7 | 2.5 ± 0.7 | 0.246 |
| Total FFAs (mmol/L) | 1.02 (0.61) | 0.89 (0.37) | 0.258 |
| Hs-CRP (nmol/L) | 11.0 (7.8) | 16.6 (14.2) | 0.016 † |
| Children without Abdominal Obesity | Children with Abdominal Obesity | p-Value | |
|---|---|---|---|
| Saturated fatty acids | 42.77 ± 3.69 | 43.44 ± 3.63 | 0.485 |
| Myristic (14:0) ‡ | 0.65 ± 0.23 | 0.67 ± 0.20 | 0.865 |
| Palmitic (16:0) | 26.32 ± 3.06 | 27.09 ± 3.39 | 0.365 |
| Estearic (18:0) | 16.02 ± 1.24 | 15.96 ± 1.24 | 0.858 |
| Monounsaturated fatty acids | 25.88 ± 11.30 | 25.26 ± 8.95 | 0.819 |
| Palmitoleic (16:1 n-7) ‡ | 0.70 ± 0.29 | 0.94 ± 0.35 | 0.038 * |
| Oleic (18:1 n-9) | 25.47 ± 11.33 | 24.71 ± 8.90 | 0.778 |
| Polyunsaturated fatty acids | 31.34 ± 8.00 | 31.28 ± 5.94 | 0.974 |
| Linoleic (18:2 n-6) | 19.72 ± 4.04 | 19.23 ± 3.97 | 0.603 |
| DHGL (20:3 n-6) | 2.07 ± 0.98 | 2.76 ± 1.09 | 0.015 * |
| Arachidonic (20:4 n-6) | 6.75 ± 2.05 | 6.96 ± 2.35 | 0.729 |
| DHA (22:6 n-3) | 2.79 ± 1.80 | 2.34 ± 0.83 | 0.221 |
| Fatty acids ratios | |||
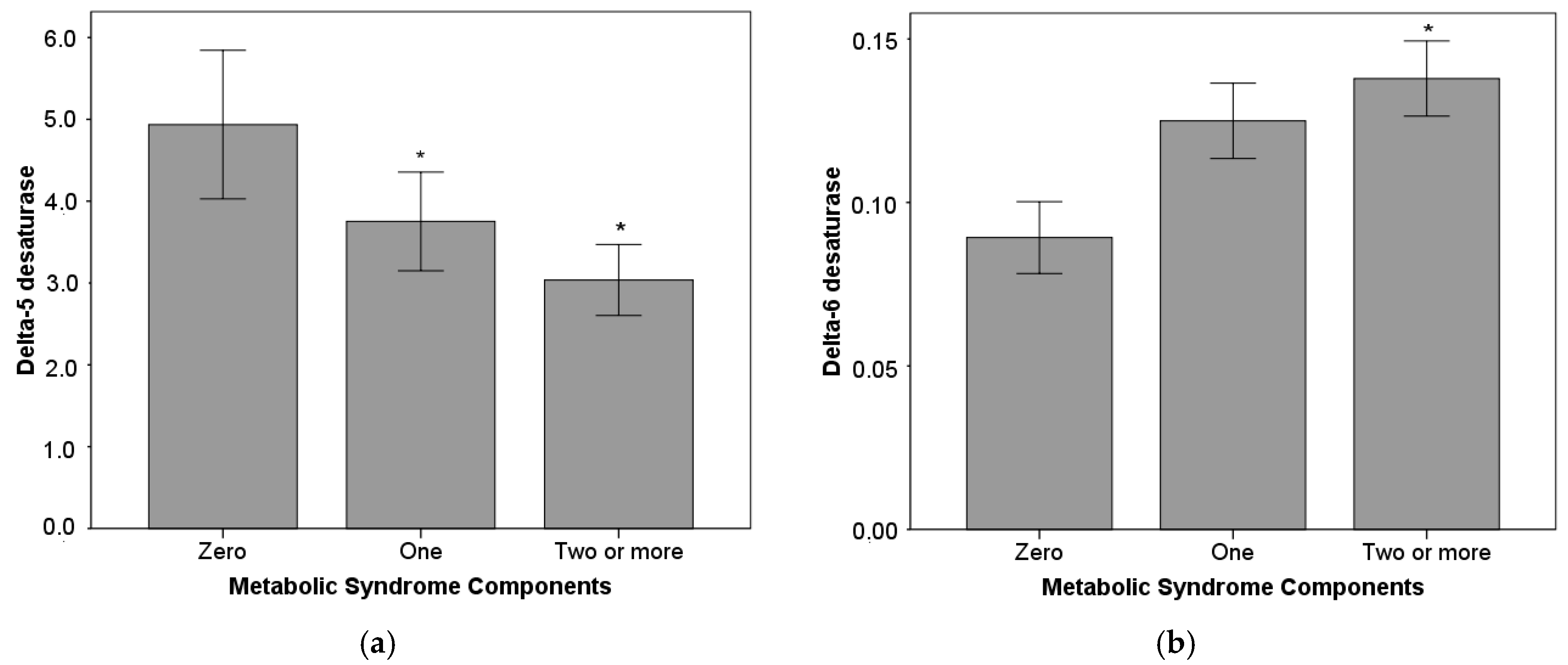
| 16:1 n-7/16:0 (D9) ‡ | 0.03 ± 0.01 | 0.04 ± 0.01 | 0.010 * |
| 20:3 n-6/18:2 n-6 (D6) | 0.10 ± 0.04 | 0.14 ± 0.06 | 0.002 * |
| 20:4 n-6/20:3 n-6 (D5) | 3.47 (1.69) | 2.53 (0.63) | 0.002 † |
| Omega-6/Omega-3 | 12.76 ± 4.55 | 13.64 ± 3.65 | 0.406 |
| Anthropometric and Cardiometabolic | Palmitic (16:0) | Palmitoleic (16:1 n-7) | DHGL (20:3 n-6) | 16:1 n-7/16:0 (D9) | 20:3 n-6/18:2 n-6 (D6) | 20:4 n-6/20:3 n-6 (D5) |
|---|---|---|---|---|---|---|
| Body mass index | 0.145 | 0.397 * | 0.296 * | 0.451 * | 0.342 * | −0.299 * |
| Waist circumference | 0.160 | 0.380 * | 0.276 * | 0.414 * | 0.332 * | −0.302 * |
| Fat mass percentage | 0.146 | 0.338 | 0.232 | 0.403 * | 0.289 * | −0.242 |
| Systolic blood pressure | 0.265 * | 0.386 * | 0.330 * | 0.368 * | 0.284 * | −0.314 * |
| Insulin | −0.014 | 0.272 | 0.132 | 0.306 | 0.142 | −0.281 * |
| HDL-C | −0.164 | −0.572 ** | −0.198 | −0.540 ** | −0.250 | 0.242 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aristizabal, J.C.; González-Zapata, L.I.; Estrada-Restrepo, A.; Monsalve-Alvarez, J.; Restrepo-Mesa, S.L.; Gaitán, D. Concentrations of Plasma Free Palmitoleic and Dihomo-Gamma Linoleic Fatty Acids Are Higher in Children with Abdominal Obesity. Nutrients 2018, 10, 31. https://doi.org/10.3390/nu10010031
Aristizabal JC, González-Zapata LI, Estrada-Restrepo A, Monsalve-Alvarez J, Restrepo-Mesa SL, Gaitán D. Concentrations of Plasma Free Palmitoleic and Dihomo-Gamma Linoleic Fatty Acids Are Higher in Children with Abdominal Obesity. Nutrients. 2018; 10(1):31. https://doi.org/10.3390/nu10010031
Chicago/Turabian StyleAristizabal, Juan C., Laura I. González-Zapata, Alejandro Estrada-Restrepo, Julia Monsalve-Alvarez, Sandra L. Restrepo-Mesa, and Diego Gaitán. 2018. "Concentrations of Plasma Free Palmitoleic and Dihomo-Gamma Linoleic Fatty Acids Are Higher in Children with Abdominal Obesity" Nutrients 10, no. 1: 31. https://doi.org/10.3390/nu10010031





