Dietary Patterns in Primary School are of Prospective Relevance for the Development of Body Composition in Two German Pediatric Populations
Abstract
:1. Introduction
2. Methods
2.1. Study Populations
2.2. Nutritional Assessment
2.3. Anthropometric Measurements and Calculations
2.4. Statistical Methods
2.4.1. PCA
2.4.2. RRR
2.4.3. Logistic Regression Analyses
3. Results
3.1. Dietary Patterns
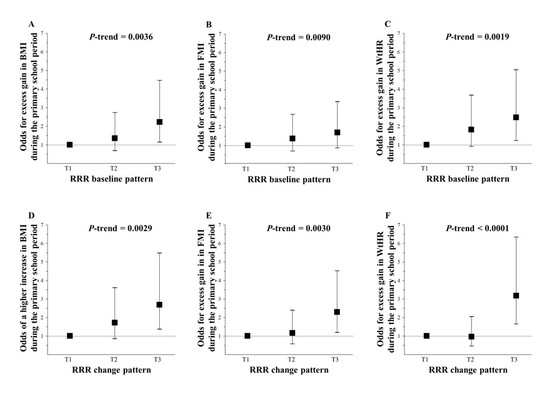
3.2. Logistic Regression Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kurth, B.M.; Schaffrath Rosario, A. [The prevalence of overweight and obese children and adolescents living in germany. Results of the german health interview and examination survey for children and adolescents (kiggs)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2007, 50, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the united states, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Von Kries, R.; Reulen, H.; Bayer, O.; Riedel, C.; Diethelm, K.; Buyken, A.E. Increase in prevalence of adiposity between the ages of 7 and 11 years reflects lower remission rates during this period. Pediatr. Obes. 2013, 8, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Hughes, A.R.; Sherriff, A.; Lawlor, D.A.; Ness, A.R.; Reilly, J.J. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev. Med. 2011, 52, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Pust, S.; Asbeck, I.; Czerwinski-Mast, M.; Langnase, K.; Fischer, C.; Bosy-Westphal, A.; Kriwy, P.; Muller, M.J. Four-year follow-up of school-based intervention on overweight children: The kops study. Obesity (Silver Spring) 2007, 15, 3159–3169. [Google Scholar] [CrossRef] [PubMed]
- Datar, A.; Shier, V.; Sturm, R. Changes in body mass during elementary and middle school in a national cohort of kindergarteners. Pediatrics 2011, 128, e1411–e1417. [Google Scholar] [CrossRef] [PubMed]
- Verrotti, A.; Penta, L.; Zenzeri, L.; Agostinelli, S.; De Feo, P. Childhood obesity: Prevention and strategies of intervention. A systematic review of school-based interventions in primary schools. J. Endocrinol. Invest. 2014, 37, 1155–1164. [Google Scholar] [CrossRef] [PubMed]
- Li, X.H.; Lin, S.; Guo, H.; Huang, Y.; Wu, L.; Zhang, Z.; Ma, J.; Wang, H.J. Effectiveness of a school-based physical activity intervention on obesity in school children: A nonrandomized controlled trial. BMC Public Health 2014, 14, 1282. [Google Scholar] [CrossRef] [PubMed]
- Diethelm, K.; Gunther, A.L.; Schulze, M.B.; Standl, M.; Heinrich, J.; Buyken, A.E. Prospective relevance of dietary patterns at the beginning and during the course of primary school to the development of body composition. Br. J. Nutr. 2014, 111, 1488–1498. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cutler, G.J.; Flood, A.; Hannan, P.J.; Slavin, J.L.; Neumark-Sztainer, D. Association between major patterns of dietary intake and weight status in adolescents. Br. J. Nutr. 2012, 108, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Oellingrath, I.M.; Svendsen, M.V.; Brantsaeter, A.L. Tracking of eating patterns and overweight—a follow-up study of norwegian schoolchildren from middle childhood to early adolescence. Nutr. J. 2011, 10, 106. [Google Scholar] [CrossRef] [PubMed]
- Pala, V.; Lissner, L.; Hebestreit, A.; Lanfer, A.; Sieri, S.; Siani, A.; Huybrechts, I.; Kambek, L.; Molnar, D.; Tornaritis, M.; et al. Dietary patterns and longitudinal change in body mass in european children: A follow-up study on the idefics multicenter cohort. Eur. J. Clin. Nutr. 2013, 67, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- Shroff, M.R.; Perng, W.; Baylin, A.; Mora-Plazas, M.; Marin, C.; Villamor, E. Adherence to a snacking dietary pattern and soda intake are related to the development of adiposity: A prospective study in school-age children. Public Health Nutr. 2014, 17, 1507–1513. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.; Mander, A.P.; Jones, L.R.; Emmett, P.M.; Jebb, S.A. Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. Am. J. Clin. Nutr. 2008, 87, 846–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emmett, P.M.; Jones, L.R.; Northstone, K. Dietary patterns in the avon longitudinal study of parents and children. Nutr. Rev. 2015, 73 Suppl 3, 207–230. [Google Scholar] [CrossRef]
- Danielzik, S.; Pust, S.; Landsberg, B.; Muller, M.J. First lessons from the kiel obesity prevention study (KOPS). Int. J. Obes. (Lond.) 2005, 29 Suppl 2, S78–S83. [Google Scholar] [CrossRef]
- Brambilla, P.; Bedogni, G.; Heo, M.; Pietrobelli, A. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int. J. Obes. (Lond.) 2013, 37, 943–946. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P.; Kovacs, E.; Moreno, L.A.; Veidebaum, T.; Tornaritis, M.; Kourides, Y.; Siani, A.; Lauria, F.; Sioen, I.; Claessens, M.; et al. Percentile reference values for anthropometric body composition indices in european children from the idefics study. Int. J. Obes. (Lond.) 2014, 38 Suppl 2, S15–S25. [Google Scholar] [CrossRef] [Green Version]
- Schroder, H.; Ribas, L.; Koebnick, C.; Funtikova, A.; Gomez, S.F.; Fito, M.; Perez-Rodrigo, C.; Serra-Majem, L. Prevalence of abdominal obesity in spanish children and adolescents. Do we need waist circumference measurements in pediatric practice? PLoS One 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.F.; Dodd, K.W.; Guenther, P.M.; Kipnis, V.; Midthune, D.; McDowell, M.; Tooze, J.A.; Freedman, L.S.; Krebs-Smith, S.M. The food propensity questionnaire: Concept, development, and validation for use as a covariate in a model to estimate usual food intake. J. Am. Diet. Assoc. 2006, 106, 1556–1563. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.J.; Asbeck, I.; Mast, M.; Langnase, K.; Grund, A. Prevention of obesity-more than an intention. Concept and first results of the kiel obesity prevention study (KOPS). Int. J. Obes. Relat. Metab. Disord. 2001, 25 (Suppl 1), S66–S74. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, W.; Bammann, K.; Siani, A.; Buchecker, K.; De Henauw, S.; Iacoviello, L.; Hebestreit, A.; Krogh, V.; Lissner, L.; Marild, S.; et al. The idefics cohort: Design, characteristics and participation in the baseline survey. Int. J. Obes. (Lond.) 2011, 35 Suppl 1, S3–S15. [Google Scholar] [CrossRef]
- von Kries, R.; Beyerlein, A.; Muller, M.J.; Heinrich, J.; Landsberg, B.; Bolte, G.; Chmitorz, A.; Plachta-Danielzik, S. Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int. J. Obes. (Lond.) 2012, 36, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Landsberg, B.; Seiberl, J.; Gehrke, M.I.; Gose, M.; Kehden, B.; Muller, M.J. Longitudinal data of the kiel obesity prevention study (KOPS). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2012, 55, 885–891. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Landsberg, B.; Lange, D.; Seiberl, J.; Muller, M.J. Eight-year follow-up of school-based intervention on childhood overweight--the kiel obesity prevention study. Obes Facts 2011, 4, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Mast, M.; Kortzinger, I.; Konig, E.; Muller, M.J. Gender differences in fat mass of 5–7-year old children. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 878–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pust, S. Evaluation eines Adipositas-Präventionsprogrammes für Kinder. Ergebnisse der Kieler Adipositas-Präventionsstudie (Kops); Der Andere Verlag: Tönning, Lübeck, Marburg, Germany, 2006. [Google Scholar]
- Lanfer, A.; Hebestreit, A.; Ahrens, W.; Krogh, V.; Sieri, S.; Lissner, L.; Eiben, G.; Siani, A.; Huybrechts, I.; Loit, H.M.; et al. Reproducibility of food consumption frequencies derived from the children’s eating habits questionnaire used in the idefics study. Int. J. Obes. (Lond.) 2011, 35 (Suppl 1), S61–S68. [Google Scholar] [CrossRef] [PubMed]
- Huybrechts, I.; Bornhorst, C.; Pala, V.; Moreno, L.A.; Barba, G.; Lissner, L.; Fraterman, A.; Veidebaum, T.; Hebestreit, A.; Sieri, S.; et al. Evaluation of the children’s eating habits questionnaire used in the idefics study by relating urinary calcium and potassium to milk consumption frequencies among european children. Int. J. Obes. (Lond.) 2011, 35 (Suppl 1), S69–S78. [Google Scholar] [CrossRef] [PubMed]
- Bel-Serrat, S.; Mouratidou, T.; Pala, V.; Huybrechts, I.; Bornhorst, C.; Fernandez-Alvira, J.M.; Hadjigeorgiou, C.; Eiben, G.; Hebestreit, A.; Lissner, L.; et al. Relative validity of the children’s eating habits questionnaire-food frequency section among young european children: The idefics study. Public Health Nutr. 2014, 17, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Plachta-Danielzik, S.; Gehrke, M.I.; Kehden, B.; Kromeyer-Hauschild, K.; Grillenberger, M.; Willhoft, C.; Bosy-Westphal, A.; Muller, M.J. Body fat percentiles for german children and adolescents. Obes Facts 2012, 5, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Tyrrell, V.J.; Richards, G.; Hofman, P.; Gillies, G.F.; Robinson, E.; Cutfield, W.S. Foot-to-foot bioelectrical impedance analysis: A valuable tool for the measurement of body composition in children. Int. J. Obes. Relat. Metab. Disord. 2001, 25, 273–278. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist circumference and waist–hip ratio: Report of a who expert consultation, 8–11 December 2008. Available online: http://whqlibdoc.who.int/publications/2011/9789241501491_eng.pdf (accessed on 9 November.2017).
- McCarthy, H.D.; Ashwell, M. A study of central fatness using waist-to-height ratios in uk children and adolescents over two decades supports the simple message-‘keep your waist circumference to less than half your height’. Int. J. Obes. (Lond.) 2006, 30, 988–992. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Faith, M.S.; Pietrobelli, A.; Heo, M. What is the best measure of adiposity change in growing children: Bmi, bmi %, bmi z-score or bmi centile? Eur. J. Clin. Nutr. 2005, 59, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Schulze, M.B.; Hoffmann, K.; Kroke, A.; Boeing, H. Dietary patterns and their association with food and nutrient intake in the european prospective investigation into cancer and nutrition (epic)-potsdam study. Br. J. Nutr. 2001, 85, 363–373. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, L. A Step-by-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling; SAS Institute: Cary, NC, USA, 2007; p. 588. [Google Scholar]
- Schulze, M.B.; Hoffmann, K.; Kroke, A.; Boeing, H. An approach to construct simplified measures of dietary patterns from exploratory factor analysis. Br. J. Nutr. 2003, 89, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, K.; Schulze, M.B.; Schienkiewitz, A.; Nothlings, U.; Boeing, H. Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am. J. Epidemiol. 2004, 159, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Willett, W. Nutritional Epidemiology, 2nd ed.; Oxford University Press: New York, NY, USA, 1998; p. 514. [Google Scholar]
- Haukoos, J.S.; Newgard, C.D. Advanced statistics: Missing data in clinical research-part 1: An introduction and conceptual framework. Acad. Emerg. Med. 2007, 14, 662–668. [Google Scholar] [PubMed]
- Rosenheck, R. Fast food consumption and increased caloric intake: A systematic review of a trajectory towards weight gain and obesity risk. Obes. Rev. 2008, 9, 535–547. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, I.; Stewart, A.W.; Hancox, R.J.; Beasley, R.; Murphy, R.; Mitchell, E.A. Fast-food consumption and body mass index in children and adolescents: An international cross-sectional study. BMJ Open 2014, 4. [Google Scholar] [CrossRef] [PubMed]
- Whitton, C.; Ma, Y.; Bastian, A.C.; Fen Chan, M.; Chew, L. Fast-food consumers in singapore: Demographic profile, diet quality and weight status. Public Health Nutr. 2014, 17, 1805–1813. [Google Scholar] [CrossRef] [PubMed]
- Shang, L.; O’Loughlin, J.; Tremblay, A.; Gray-Donald, K. The association between food patterns and adiposity among canadian children at risk of overweight. Appl. Physiol. Nutr. Metab. 2014, 39, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Poti, J.M.; Duffey, K.J.; Popkin, B.M. The association of fast food consumption with poor dietary outcomes and obesity among children: Is it the fast food or the remainder of the diet? Am. J. Clin. Nutr. 2014, 99, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Alexy, U.; Libuda, L.; Mersmann, S.; Kersting, M. Convenience foods in children’s diet and association with dietary quality and body weight status. Eur. J. Clin. Nutr. 2011, 65, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Tognon, G.; Moreno, L.A.; Mouratidou, T.; Veidebaum, T.; Molnar, D.; Russo, P.; Siani, A.; Akhandaf, Y.; Krogh, V.; Tornaritis, M.; et al. Adherence to a mediterranean-like dietary pattern in children from eight european countries. The idefics study. Int. J. Obes. (Lond.) 2014, 38 Suppl 2, S108–S114. [Google Scholar] [CrossRef] [Green Version]
- Lydakis, C.; Stefanaki, E.; Stefanaki, S.; Thalassinos, E.; Kavousanaki, M.; Lydaki, D. Correlation of blood pressure, obesity, and adherence to the mediterranean diet with indices of arterial stiffness in children. Eur. J. Pediatr. 2012, 171, 1373–1382. [Google Scholar] [CrossRef] [PubMed]
- Schroder, H.; Mendez, M.A.; Ribas-Barba, L.; Covas, M.I.; Serra-Majem, L. Mediterranean diet and waist circumference in a representative national sample of young spaniards. Int. J. Pediatr. Obes. 2010, 5, 516–519. [Google Scholar] [CrossRef] [PubMed]
- Martin-Calvo, N.; Chavarro, J.E.; Falbe, J.; Hu, F.B.; Field, A.E. Adherence to the mediterranean dietary pattern and bmi change among us adolescents. Int. J. Obes. (Lond.) 2016, 40, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Tognon, G.; Hebestreit, A.; Lanfer, A.; Moreno, L.A.; Pala, V.; Siani, A.; Tornaritis, M.; De Henauw, S.; Veidebaum, T.; Molnár, D.; et al. Mediterranean diet, overweight and body composition in children from eight european countries: Cross-sectional and prospective results from the idefics study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Farajian, P.; Risvas, G.; Karasouli, K.; Pounis, G.D.; Kastorini, C.M.; Panagiotakos, D.B.; Zampelas, A. Very high childhood obesity prevalence and low adherence rates to the mediterranean diet in greek children: The greco study. Atherosclerosis 2011, 217, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Jennings, A.; Welch, A.; van Sluijs, E.M.; Griffin, S.J.; Cassidy, A. Diet quality is independently associated with weight status in children aged 9–10 years. J. Nutr. 2011, 141, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Velazquez-Lopez, L.; Santiago-Diaz, G.; Nava-Hernandez, J.; Munoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014, 14, 175. [Google Scholar] [CrossRef] [PubMed]
- Romaguera, D.; Norat, T.; Vergnaud, A.C.; Mouw, T.; May, A.M.; Agudo, A.; Buckland, G.; Slimani, N.; Rinaldi, S.; Couto, E.; et al. Mediterranean dietary patterns and prospective weight change in participants of the epic-panacea project. Am. J. Clin. Nutr. 2010, 92, 912–921. [Google Scholar] [CrossRef] [PubMed]
- Buckland, G.; Bach, A.; Serra-Majem, L. Obesity and the mediterranean diet: A systematic review of observational and intervention studies. Obes. Rev. 2008, 9, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Shai, I.; Schwarzfuchs, D.; Henkin, Y.; Shahar, D.R.; Witkow, S.; Greenberg, I.; Golan, R.; Fraser, D.; Bolotin, A.; Vardi, H.; et al. Weight loss with a low-carbohydrate, mediterranean, or low-fat diet. N. Engl. J. Med. 2008, 359, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Bonaccio, M.; Di Castelnuovo, A.; Costanzo, S.; De Lucia, F.; Olivieri, M.; Donati, M.B.; de Gaetano, G.; Iacoviello, L.; Bonanni, A. Nutrition knowledge is associated with higher adherence to mediterranean diet and lower prevalence of obesity. Results from the moli-sani study. Appetite 2013, 68, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Michels, K.B.; Schulze, M.B. Can dietary patterns help us detect diet-disease associations? Nutr. Res. Rev. 2005, 18, 241–248. [Google Scholar] [CrossRef] [PubMed]
- McNaughton, S.A.; Ball, K.; Mishra, G.D.; Crawford, D.A. Dietary patterns of adolescents and risk of obesity and hypertension. J. Nutr. 2008, 138, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Northstone, K.; Emmett, P.M. Are dietary patterns stable throughout early and mid-childhood? A birth cohort study. Br. J. Nutr. 2008, 100, 1069–1076. [Google Scholar] [CrossRef] [PubMed]
- Craig, L.C.; McNeill, G.; Macdiarmid, J.I.; Masson, L.F.; Holmes, B.A. Dietary patterns of school-age children in scotland: Association with socio-economic indicators, physical activity and obesity. Br. J. Nutr. 2010, 103, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Richter, A.; Heidemann, C.; Schulze, M.B.; Roosen, J.; Thiele, S.; Mensink, G.B. Dietary patterns of adolescents in Germany—associations with nutrient intake and other health related lifestyle characteristics. BMC Pediatr. 2012, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Weikert, C.; Schulze, M.B. Evaluating dietary patterns: The role of reduced rank regression. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Simpson, S.J.; Raubenheimer, D. Perspective: Tricks of the trade. Nature 2014, 508, S66. [Google Scholar] [CrossRef] [PubMed]
- Gosby, A.K.; Conigrave, A.D.; Raubenheimer, D.; Simpson, S.J. Protein leverage and energy intake. Obes. Rev. 2014, 15, 183–191. [Google Scholar] [CrossRef] [PubMed]
- Solon-Biet, S.M.; McMahon, A.C.; Ballard, J.W.; Ruohonen, K.; Wu, L.E.; Cogger, V.C.; Warren, A.; Huang, X.; Pichaud, N.; Melvin, R.G.; et al. The ratio of macronutrients, not caloric intake, dictates cardiometabolic health, aging, and longevity in ad libitum-fed mice. Cell Metab. 2014, 19, 418–430. [Google Scholar] [CrossRef] [PubMed]
- Berryman, C.E.; Agarwal, S.; Lieberman, H.R.; Fulgoni, V.L., 3rd; Pasiakos, S.M. Diets higher in animal and plant protein are associated with lower adiposity and do not impair kidney function in us adults. Am. J. Clin. Nutr. 2016, 104, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Pasiakos, S.M.; Lieberman, H.R.; Fulgoni, V.L. , 3rd. Higher-protein diets are associated with higher hdl cholesterol and lower bmi and waist circumference in us adults. J. Nutr. 2015, 145, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Jen, V.; Karagounis, L.G.; Jaddoe, V.W.V.; Franco, O.H.; Voortman, T. Dietary protein intake in school-age children and detailed measures of body composition: The generation r study. Int. J. Obes. (Lond.) 2018. [Google Scholar] [CrossRef] [PubMed]
- Buyken, A.E.; Bolzenius, K.; Karaolis-Danckert, N.; Gunther, A.L.; Kroke, A. Body composition trajectories into adolescence according to age at pubertal growth spurt. Am. J. Hum. Biol. 2011, 23, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Johannsen, M. Übergewicht bei 5–7-jährigen Kindern. Analyse von Trends, Determinanten und gesundheitlichen Auswirkungen; eine Untersuchung im Rahmen der Kieler Adipositas-Präventionsstudie (KOPS). Der Andere Verlag: Tönning, Lübeck, Marburg, Germany, 2009. [Google Scholar]
- Gose, M.; Plachta-Danielzik, S.; Kehden, B.; Johannsen, M.; Landsberg, B.; Müller, M. Trends in incidence and determinants of overweight among 9–11-year-old children–kiel obesity prevention study (KOPS). Obesity Facts 2013, 6, 202. [Google Scholar]
- Costello, A.B.; Osborne, J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 2005, 10, 1–9. [Google Scholar]


| KOPS | IDEFICS-Germany | |||
|---|---|---|---|---|
| Median or n-Number | P25, P75 or Percentage | Median or n-Number | P25, P75 or Percentage | |
| n (% female) | 372 | 49.5 | 298 | 47.3 |
| Birth and infancy | ||||
| Birth year (min–max) | 1991–1996 | 2000–2003 | ||
| Gestational age (weeks) | 40 | 39, 40 | n/a | |
| Birth weight < 3500 g, n (%) | 184 | 49.5 | 113 | 37.9 |
| Appropriate for gestational age, n (%) | 276 | 74.2 | n/a | |
| Fully breast fed, n (%) a | 317 | 85.2 | 182 | 61.1 |
| Smoking during pregnancy, n (%) | 63 | 16.9 | 50 | 17.2 |
| Family | ||||
| Maternal overweight, n (%) b,c | 104 | 28.0 | 116 | 39.2 |
| Paternal overweight, n (%) b,c | 161 | 44.9 | 165 | 61.3 |
| Parental overweight, n (%) b,d | 209 | 56.2 | 205 | 68.8 |
| Parental education, n (%) e | 217 | 58.3 | 149 | 50.0 |
| Single parenting, n (%) c,f | 57 | 15.5 | 33 | 11.1 |
| Low income, n (%) c,g | 10 | 8.3 | 47 | 17.2 |
| Beginning of the Primary School Period | End of the Primary School Period | Mean Difference between End and Beginning of Primary School Period | ||||
|---|---|---|---|---|---|---|
| Median or n-Number | P25, P75, or Percentage | Median or n-Number | P25, P75, or Percentage | Median or n-Number | P25, P75, or Percentage | |
| KOPS | ||||||
| n (% female) | 372 | 49.5 | 372 | 49.5 | ||
| Age | 6.2 | 6.0, 6.5 | 9.8 | 9.6, 10.1 | 3.6 | 3.5, 3.7 |
| Anthropometry | ||||||
| BMI (kg/m2) | 15.41 | 14.63, 16.31 | 16.85 | 15.55, 18.35 | 1.32 | 0.58, 2.55 |
| Overweight, n (%)a | 37 | 10.0 | 58 | 15.6 | ||
| FMI (kg/m2) | 3.18 | 2.59, 3.91 | 3.17 | 2.28, 4.31 | −0.02 | −0.70, 1.00 |
| FFMI (kg/m2) | 12.31 | 11.68, 12.91 | 13.67 | 13.11, 14.40 | 1.46 | 0.92, 1.97 |
| Waist circumference (cm) | 54.5 | 52.3, 57.5 | 62.0 | 58.0, 66.0 | 7.0 | 4.0, 10.5 |
| Waist-to-height ratio | 0.46 | 0.44, 0.48 | 0.43 | 0.42, 0.46 | −0.02 | −0.04, 0.01 |
| WtHR >0.5b, n (%) | 46 | 12.4 | 36 | 9.7 | ||
| IDEFICS-Germany | ||||||
| n (% female) | 298 | 47.3 | 298 | 47.3 | ||
| Age | 6.5 | 5.6, 6.9 | 8.5 | 7.7, 9.0 | 2.0 | 2.0, 2.1 |
| Anthropometry | ||||||
| BMI (kg/m2) | 15.50 | 14.60, 16.60 | 16.15 | 14.90, 17.80 | 0.60 | 0.10, 1.30 |
| Overweight, n (%) a | 34 | 11.4 | 48 | 16.1 | ||
| FMI (kg/m2) | 4.33 | 3.68, 5.17 | 4.42 | 3.40, 5.68 | 0.07 | −0.44, 0.73 |
| FFMI (kg/m2) | 11.23 | 10.58, 11.79 | 11.85 | 11.22, 12.36 | 0.61 | 0.39, 0.82 |
| Waist circumference (cm) | 51.6 | 49.5, 54.1 | 56.5 | 53.3, 60.1 | 4.8 | 2.7, 6.9 |
| Waist-to-height ratio | 0.43 | 0.41, 0.45 | 0.42 | 0.40, 0.45 | −0.01 | −0.02, 0.01 |
| WtHR >0.5 b, n (%) | 12 | 4.0 | 16 | 5.4 | ||
| Included Food Groups | Factor Loading | Explained Variance in the Food Group Intake (%) | |
| PCA pattern a | |||
| PCA baseline pattern 1 (‘fast food pattern’) | + Fish sticks | 0.62 | 12.7 |
| + Curry-sausage | 0.62 | ||
| + Lasagna | 0.57 | ||
| + Pancakes | 0.55 | ||
| + Potato fritters | 0.52 | ||
| + Pizza | 0.51 | ||
| + Meat balls | 0.5 | ||
| PCA baseline pattern 2 (‘wholegrain, vegetables & fruits’) | + Whole-grain bread | 0.66 | 8.1 |
| + Vegetables, salad | 0.65 | ||
| + Fruits | 0.56 | ||
| + Cheese, curd, yogurt | 0.47 | ||
| + Muesli | 0.43 | ||
| PCA change pattern 1 (‘increase in the consumption of fast food’) | +Δ Meat balls | 0.61 | 9.4 |
| +Δ Fish sticks | 0.57 | ||
| +Δ Lasagna | 0.54 | ||
| +Δ Pizza | 0.52 | ||
| +Δ Pancakes | 0.48 | ||
| +Δ Curry-sausage | 0.44 | ||
| +Δ Potato fritters | 0.43 | ||
| PCA change pattern 2 (‘increase in the consumption of vegetables and fruits’) | +Δ Vegetables, salad | 0.61 | 6.8 |
| +Δ Fruits | 0.57 | ||
| +Δ Meat | 0.47 | ||
| +Δ Potatoes | 0.44 | ||
| PCA change pattern 3 (‘change towards unhealthy carbohydrates’) | +Δ White bread | 0.64 | 6.4 |
| +Δ Savory bakery goods | 0.49 | ||
| −Δ Whole-grain bread | −0.51 | ||
| Included Food Groups | Factor Loading | Explained Variance in Response Variables b (%) | |
| RRR pattern a | |||
| RRR baseline pattern (‘fast food pattern’) | − Whole-grain bread | −0.32 | Changes in BMI: 9.1 Changes in FMI: 5.5 Changes in WtHR: 7.9 Total variance: 7.5 |
| − Cheese, curd, yogurt | −0.32 | ||
| + Lemonade | 0.55 | ||
| + Children’s yogurt | 0.41 | ||
| + Potato fritters | 0.27 | ||
| + Meat balls | 0.24 | ||
| + Meat | 0.21 | ||
| RRR change pattern (‘increase in the consumption of fast foods and starchy carbohydrate foods’) | +Δ Fish sticks | 0.49 | Changes in BMI: 7.7 Changes in FMI: 5.9 Changes in WtHR: 8.6 Total variance: 7.4 |
| +Δ Whole-grain bread | 0.26 | ||
| +Δ Pizza | 0.21 | ||
| +Δ Potatoes | 0.2 | ||
| −Δ Vegetables | −0.44 | ||
| −Δ Lemonade | −0.33 | ||
| −Δ Sweets | −0.28 | ||
| −Δ Chocolate spread | −0.21 | ||
| −Δ Meat balls | −0.21 | ||
| Included Food Groups | Factor Loading | Explained Variance in Food Group Intake (%) | |
| PCA patterna | |||
| PCA baseline pattern 1 (‘snack pattern’) | + Sweet snacks (biscuits, packaged cakes, pastries, puddings) | 0.57 | 10.3 |
| + Potatoes (fried, croquettes) | 0.52 | ||
| + Ketchup and similar | 0.51 | ||
| + Savory snacks (Crisps, corn crisps, popcorn) | 0.51 | ||
| + Sweetened drinks | 0.45 | ||
| + Chocolate, candy bars | 0.44 | ||
| + Candies, loose candies, marshmallows | 0.44 | ||
| + Ice cream, milk, or fruit-based bars | 0.43 | ||
| PCA baseline pattern 2 (‘Mediterranean type pattern’) | + Plain unsweetened yogurt or kefir | 0.66 | 6.5 |
| + Dish of milled cereals | 0.57 | ||
| + Nuts, seeds, dried fruits | 0.56 | ||
| + Pizza as main dish | 0.45 | ||
| + Cheese (sliced and spreadable) | 0.44 | ||
| + Fresh meat, not fried | 0.44 | ||
| + Plain unsweetened milk | 0.42 | ||
| + Fresh fruits with added sugar | 0.41 | ||
| + Water | 0.41 | ||
| + Pasta, noodles, rice | 0.41 | ||
| PCA change pattern 1 (‘change towards a Mediterranean type pattern’) | +Δ Nuts, seeds, dried fruits | 0.6 | 8.9 |
| +Δ Pasta, noodles, rice | 0.56 | ||
| +Δ Fresh meat, not fried | 0.52 | ||
| +Δ Pizza as main dish | 0.49 | ||
| +Δ Dish of milled cereals | 0.48 | ||
| +Δ Sweet yogurt, fermented milk beverages | 0.43 | ||
| +Δ Fried meat | 0.41 | ||
| PCA change pattern 2 (‘change towards a traditional type pattern’) | +Δ Cooked vegetables, potatoes, beans, and legumes | 0.54 | 4.8 |
| +Δ Sweetened drinks | 0.49 | ||
| +Δ Butter, margarine on bread | 0.48 | ||
| +Δ Fresh fruits without added sugar | 0.47 | ||
| PCA change pattern 3 (‘change towards a snack pattern’) | +Δ Sweet snacks (biscuits, packaged cakes, pastries, puddings) | 0.65 | 4.5 |
| +Δ Candies, loose candies, marshmallows | 0.58 | ||
| +Δ Ice cream, milk, or fruit-based bars | 0.52 | ||
| +Δ Savory snacks (Crisps, corn crisps, popcorn) | 0.51 | ||
| +Δ Chocolate, candy bars | 0.46 | ||
| Included Food Groups | Factor Loading | Explained Variance in Response Variables b (%) | |
| RRR pattern a | |||
| RRR baseline pattern (‘Nuts, meat, and pizza pattern’) | + Nuts, seeds, dried fruits | 0.37 | Changes in BMI: 11.5 Changes in FMI: 11.9 Changes in WtHR: 12.3 Total variance: 11.9 |
| + Fresh meat, not fried | 0.36 | ||
| + Pizza as main dish | 0.3 | ||
| + Plain unsweetened yogurt or kefir | 0.23 | ||
| + Jam, honey | 0.22 | ||
| + Savory pastries, fritters | 0.23 | ||
| + Dish of milled cereals | 0.24 | ||
| − Cooked vegetables, potatoes, beans, and legumes | −0.29 | ||
| − Breakfast cereals, muesli, sweetened | −0.23 | ||
| RRR change pattern (‘decrease in the consumption of protein sources and snack carbohydrates’) | +Δ Reduced-fat products on bread | 0.24 | Changes in BMI: 14.0 Changes in FMI: 14.3 Changes in WtHR: 12.0 Total variance: 13.5 |
| −Δ Fresh meat, not fried | −0.36 | ||
| −Δ Savory pastries, fritters | −0.33 | ||
| −Δ Fried or scrambled eggs | −0.29 | ||
| −Δ Sweetened drinks | −0.27 | ||
| −Δ Nuts, seeds, dried fruits | −0.3 | ||
| −Δ Dish of milled cereals | −0.24 | ||
| PCA Baseline Pattern 1 (‘Fast Food Pattern’) | PCA Change Pattern 1 (‘Increase in the Consumption of Fast Food’) | |||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | T1 | T2 | T3 | Continuous b | ptrendc | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| BMI | ||||||||||||||||
| Model A | 1 | 0.89 | 0.50, 1.60 | 1.26 | 0.72, 2.21 | 1.03 | 0.98, 1.09 | 0.2768 | 1 | 0.91 | 0.50, 1.65 | 1.39 | 0.79, 2.46 | 1.04 | 0.99, 1.10 | 0.1478 |
| Model B | 0.81 | 0.44, 1.49 | 1.00 | 0.55, 1.80 | 1.01 | 0.95, 1.07 | 0.8457 | 1 | 0.95 | 0.51, 1.75 | 1.49 | 0.83, 2.68 | 1.05 | 0.99, 1.10 | 0.1133 | |
| FMI | ||||||||||||||||
| Model A | 1 | 0.79 | 0.44, 1.40 | 0.98 | 0.56, 1.73 | 1.02 | 0.97, 1.08 | 0.4590 | 1 | 1.10 | 0.60, 2.01 | 1.73 | 0.97, 3.07 | 1.05 | 1.00, 1.11 | 0.0538 |
| Model B | 1 | 0.67 | 0.37, 1.24 | 0.73 | 0.41, 1.33 | 0.99 | 0.94, 1.06 | 0.8556 | 1 | 1.19 | 0.64, 2.21 | 1.86 | 1.03, 3.38 | 1.06 | 1.00, 1.12 | 0.0411 |
| WtHR | ||||||||||||||||
| Model A | 1 | 0.59 | 0.32, 1.07 | 1.11 | 0.64, 1.93 | 1.03 | 0.97, 1.09 | 0.3318 | 1 | 0.76 | 0.42, 1.38 | 1.28 | 0.73, 2.23 | 1.02 | 0.97, 1.08 | 0.4498 |
| Model B | 1 | 0.54 | 0.29, 1.01 | 0.88 | 0.49, 1.57 | 1.00 | 0.95, 1.06 | 0.9329 | 1 | 0.79 | 0.43, 1.46 | 1.35 | 0.76, 2.40 | 1.02 | 0.97, 1.08 | 0.3665 |
| PCA Baseline Pattern 2 (‘Wholegrain, Vegetables & Fruits’) | PCA Change Pattern 2 (‘Increase in the Consumption of Vegetables and Fruits’) | |||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | T1 | T2 | T3 | Continuous b | ptrendc | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| BMI | ||||||||||||||||
| Model A | 1 | 0.94 | 0.54, 1.64 | 0.60 | 0.33, 1.09 | 0.95 | 0.88, 1.03 | 0.2316 | 1 | 1.01 | 0.57, 1.79 | 0.87 | 0.49, 1.55 | 1.00 | 0.92, 1.09 | 0.9687 |
| Model B | 1.10 | 0.62, 1.95 | 0.77 | 0.41, 1.43 | 1.00 | 0.91, 1.08 | 0.9079 | 1 | 1.03 | 0.57, 1.86 | 0.76 | 0.42, 1.39 | 0.98 | 0.90, 1.08 | 0.7236 | |
| FMI | ||||||||||||||||
| Model A | 1 | 1.20 | 0.69, 2.09 | 0.68 | 0.37, 1.25 | 0.96 | 0.89, 1.04 | 0.2859 | 1 | 0.85 | 0.47, 1.52 | 1.03 | 0.59, 1.82 | 1.02 | 0.93, 1.11 | 0.7210 |
| Model B | 1 | 1.42 | 0.80, 2.53 | 0.89 | 0.47, 1.67 | 1.00 | 0.92, 1.09 | 0.9971 | 1 | 0.86 | 0.47, 1.57 | 0.92 | 0.51, 1.65 | 1.00 | 0.91, 1.09 | 0.9852 |
| WtHR | ||||||||||||||||
| Model A | 1 | 0.87 | 0.50, 1.51 | 0.58 | 0.32, 1.05 | 0.96 | 0.89, 1.04 | 0.3049 | 1 | 0.65 | 0.36. 1.17 | 0.91 | 0.52, 1.59 | 0.98 | 0.90, 1.07 | 0.6387 |
| Model B | 1 | 0.97 | 0.55, 1.72 | 0.72 | 0.39, 1.34 | 1.00 | 0.92, 1.09 | 0.9676 | 1 | 0.61 | 0.33, 1.13 | 0.80 | 0.45, 1.43 | 0.96 | 0.88, 1.05 | 0.3628 |
| PCA Change Pattern 3 (‘Change towards Unhealthy Carbohydrates’) | ||||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | ||||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||||||||
| BMI | ||||||||||||||||
| Model A | 1 | 0.83 | 0.47, 1.46 | 0.80 | 0.45, 1.42 | 0.97 | 0.87, 1.08 | 0.5265 | ||||||||
| Model B | 1 | 0.89 | 0.50, 1.61 | 0.90 | 0.50, 1.63 | 0.99 | 0.88, 1.10 | 0.8046 | ||||||||
| FMI | ||||||||||||||||
| Model A | 1 | 0.69 | 0.39, 1.24 | 0.84 | 0.48, 1.47 | 0.95 | 0.85, 1.06 | 0.3516 | ||||||||
| Model B | 1 | 0.75 | 0.41, 1.35 | 0.96 | 0.53, 1.72 | 0.97 | 0.87, 1.09 | 0.6091 | ||||||||
| WtHR | ||||||||||||||||
| Model A | 1 | 0.87 | 0.49, 1.52 | 0.67 | 0.37, 1.20 | 0.91 | 0.81, 1.01 | 0.0836 | ||||||||
| Model B | 1 | 0.92 | 0.52, 1.64 | 0.71 | 0.39, 1.30 | 0.92 | 0.82, 1.03 | 0.1262 | ||||||||
| PCA Baseline Pattern 1 (‘Snack Pattern’) | PCA Change Pattern 1 (‘Increase in the Consumption of Fast Food’) | |||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | T1 | T2 | T3 | Continuous b | ptrendc | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| BMI | ||||||||||||||||
| Model A | 1 | 0.69 | 0.37, 1.29 | 0.52 | 0.27, 1.00 | 0.95 | 0.88, 1.02 | 0.1537 | 1 | 1.15 | 0.62, 2.15 | 0.67 | 0.34, 1.30 | 0.93 | 0.87, 1.00 | 0.0395 |
| Model B | 0.67 | 0.35, 1.26 | 0.47 | 0.23, 0.91 | 0.94 | 0.87, 1.01 | 0.0810 | 1 | 1.12 | 0.60, 2.11 | 0.65 | 0.33, 1.30 | 0.93 | 0.87, 0.99 | 0.0436 | |
| FMI | ||||||||||||||||
| Model A | 1 | 1.10 | 0.58, 2.07 | 0.85 | 0.44, 1.63 | 0.99 | 0.92, 1.06 | 0.8102 | 1 | 1.21 | 0.65, 2.27 | 0.75 | 0.38, 1.46 | 0.93 | 0.87, 0.99 | 0.0454 |
| Model B | 1 | 1.06 | 0.55, 2.03 | 0.78 | 0.39, 1.52 | 0.98 | 0.91, 1.05 | 0.6013 | 1 | 1.05 | 0.55, 1.99 | 0.79 | 0.40, 1.56 | 0.94 | 0.87, 0.99 | 0.0490 |
| WtHR | ||||||||||||||||
| Model A | 1 | 1.29 | 0.68, 2.45 | 1.00 | 0.52, 1.94 | 0.99 | 0.92, 1.06 | 0.8259 | 1 | 1.04 | 0.55, 1.95 | 0.76 | 0.39, 1.46 | 0.93 | 0.87, 0.99 | 0.0409 |
| Model B | 1 | 1.18 | 0.62, 2.28 | 0.95 | 0.48, 1.87 | 0.98 | 0.92, 1.05 | 0.6481 | 1 | 1.04 | 0.55, 1.99 | 0.79 | 0.40, 1.56 | 0.93 | 0.87, 0.99 | 0.0490 |
| PCA Baseline Pattern 2 (‘Mediterranean Type Pattern’) | PCA Change Pattern 2 (‘Change towards a Traditional Type Pattern’) | |||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | T1 | T2 | T3 | Continuous b | ptrendc | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||
| BMI | ||||||||||||||||
| Model A | 1 | 0.65 | 0.33, 1.25 | 0.92 | 0.49. 1.71 | 1.04 | 0.99, 1.09 | 0.1456 | 1 | 1.04 | 0.55, 1.99 | 1.06 | 0.55, 2.02 | 1.02 | 0.92, 1.13 | 0.7179 |
| Model B | 0.65 | 0.33, 1.27 | 0.92 | 0.47, 1.79 | 1.04 | 0.99, 1.11 | 0.1403 | 1 | 1.02 | 0.52, 1.98 | 1.06 | 0.54, 2.07 | 1.02 | 0.92, 1.14 | 0.6587 | |
| FMI | ||||||||||||||||
| Model A | 1 | 0.96 | 0.51, 1.82 | 0.86 | 0.45, 1.64 | 1.03 | 0.98, 1.09 | 0.1957 | 1 | 1.10 | 0.58, 2.07 | 0.85 | 0.44, 1.63 | 0.99 | 0.89, 1.10 | 0.8205 |
| Model B | 1 | 1.00 | 0.52, 1.92 | 0.91 | 0.46, 1.81 | 1.05 | 0.99, 1.12 | 0.1073 | 1 | 1.02 | 0.53, 1.96 | 0.83 | 0.42, 1.63 | 0.99) | 0.89, 1.10 | 0.8780 |
| WtHR | ||||||||||||||||
| Model A | 1 | 0.62 | 0.32, 1.19 | 0.83 | 0.44, 1.55 | 1.04 | 0.98, 1.10 | 0.2349 | 1 | 0.75 | 0.39, 1.44 | 0.90 | 0.48, 1.70 | 0.95 | 00.86, 1.05 | 0.3343 |
| Model B | 1 | 0.60 | 0.31, 1.17 | 0.86 | 0.44, 1.67 | 1.04 | 0.98, 1.11 | 0.1764 | 1 | 0.63 | 0.32, 1.24 | 0.77 | 0.40, 1.50 | 0.94 | 0.85, 1.04 | 0.2324 |
| PCA Change Pattern 3 (‘Change towards a Snack Pattern’) | ||||||||||||||||
| T1 | T2 | T3 | Continuous b | ptrendc | ||||||||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |||||||||||
| BMI | ||||||||||||||||
| Model A | 1 | 1.53 | 0.80, 2.99 | 1.41 | 0.73, 2.76 | 1.01 | 0.93, 1.10 | 0.7551 | ||||||||
| Model B | 1 | 1.60 | 0.83, 3.15 | 1.46 | 0.75, 2.87 | 1.02 | 0.94, 1.11 | 0.6363 | ||||||||
| FMI | ||||||||||||||||
| Model A | 1 | 1.24 | 0.64, 2.41 | 1.47 | 0.77, 2.83 | 0.98 | 0.90, 1.06 | 0.6550 | ||||||||
| Model B | 1 | 1.27 | 0.65, 2.50 | 1.49 | 0.78, 2.90 | 0.99 | 0.91, 1.08 | 0.8546 | ||||||||
| WtHR | ||||||||||||||||
| Model A | 1 | 1.11 | 0.57, 2.18 | 1.62 | 0.85, 3.11 | 1.03 | 0.95, 1.12 | 0.5336 | ||||||||
| Model B | 1 | 1.17 | 0.59, 2.33 | 1.64 | 0.86, 3.19 | 1.03 | 0.95, 1.12 | 0.4342 | ||||||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wolters, M.; Joslowski, G.; Plachta-Danielzik, S.; Standl, M.; Müller, M.J.; Ahrens, W.; Buyken, A.E. Dietary Patterns in Primary School are of Prospective Relevance for the Development of Body Composition in Two German Pediatric Populations. Nutrients 2018, 10, 1442. https://doi.org/10.3390/nu10101442
Wolters M, Joslowski G, Plachta-Danielzik S, Standl M, Müller MJ, Ahrens W, Buyken AE. Dietary Patterns in Primary School are of Prospective Relevance for the Development of Body Composition in Two German Pediatric Populations. Nutrients. 2018; 10(10):1442. https://doi.org/10.3390/nu10101442
Chicago/Turabian StyleWolters, Maike, Gesa Joslowski, Sandra Plachta-Danielzik, Marie Standl, Manfred J. Müller, Wolfgang Ahrens, and Anette E. Buyken. 2018. "Dietary Patterns in Primary School are of Prospective Relevance for the Development of Body Composition in Two German Pediatric Populations" Nutrients 10, no. 10: 1442. https://doi.org/10.3390/nu10101442
APA StyleWolters, M., Joslowski, G., Plachta-Danielzik, S., Standl, M., Müller, M. J., Ahrens, W., & Buyken, A. E. (2018). Dietary Patterns in Primary School are of Prospective Relevance for the Development of Body Composition in Two German Pediatric Populations. Nutrients, 10(10), 1442. https://doi.org/10.3390/nu10101442