Dietary Patterns Are Associated with Cardiovascular and Cancer Mortality among Swiss Adults in a Census-Linked Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Dietary Assessment
2.3. Identification of Dietary Patterns
2.4. Association between Dietary Patterns and Demographics and Lifestyle Data
2.5. Association between Dietary Patterns and Mortality
3. Results
3.1. Population Description
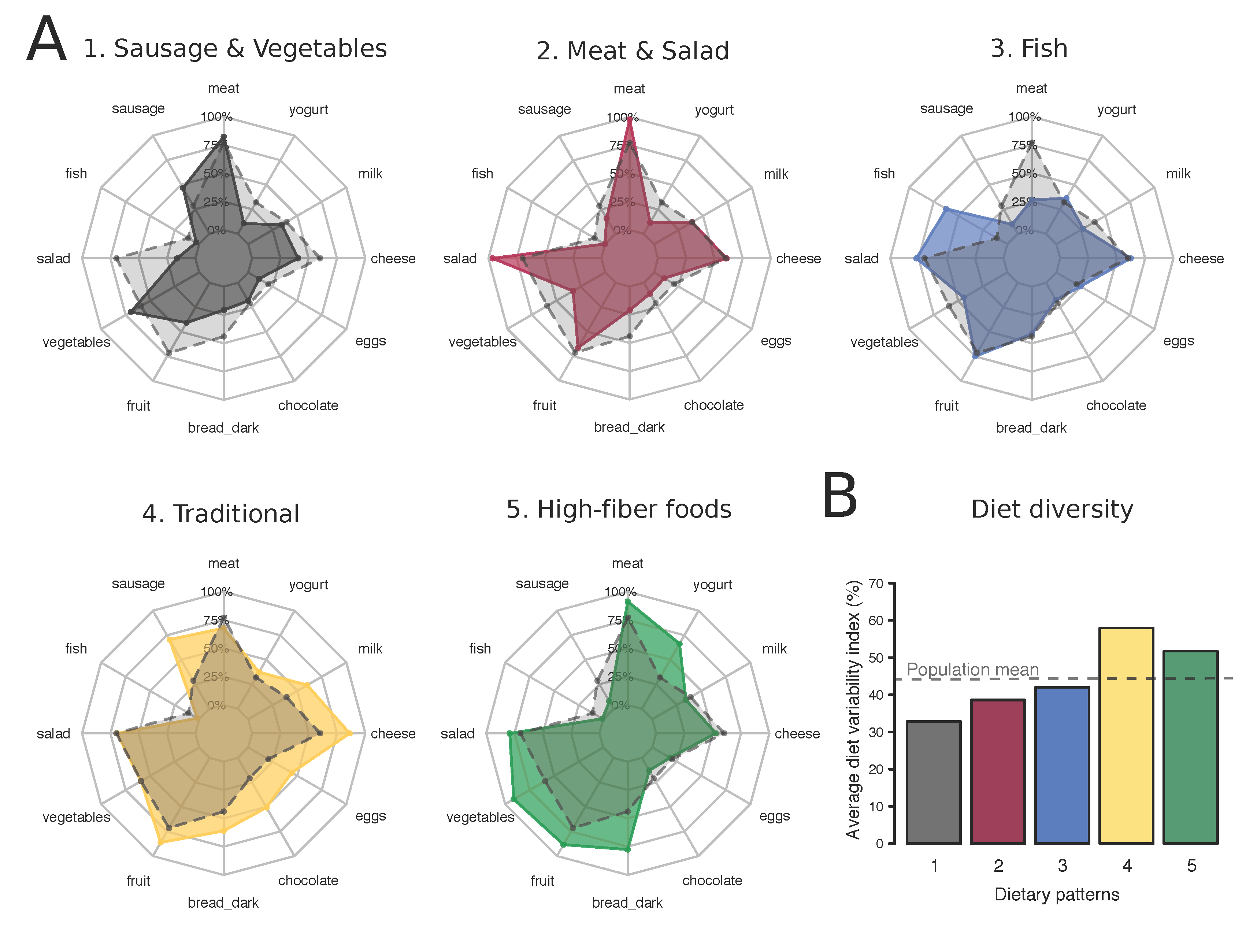
3.2. Identification of Dietary Patterns
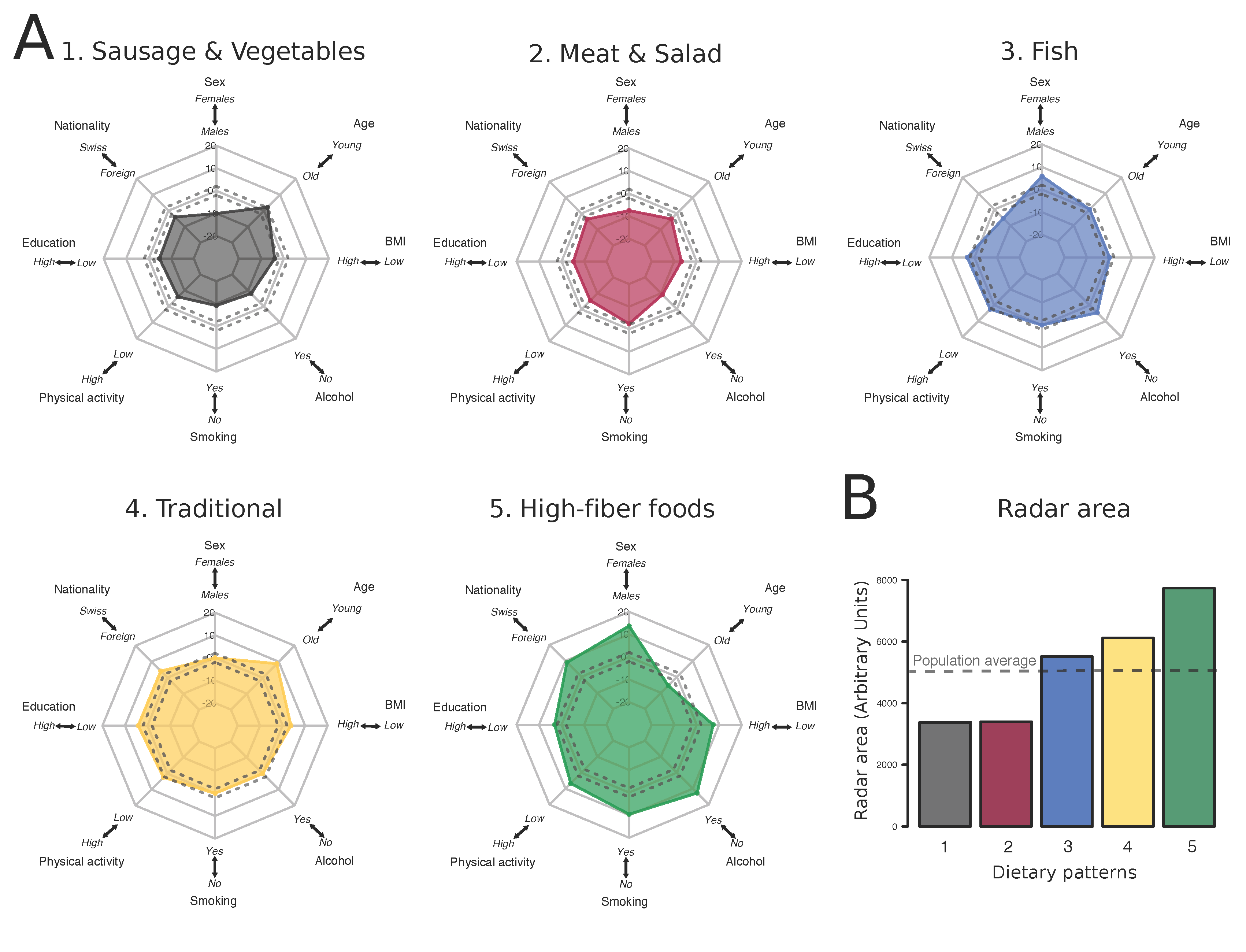
3.3. Characterization of the Population Associated to Each Dietary Pattern
3.4. Association between Dietary Patterns and Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Moeller, S.M.; Reedy, J.; Millen, A.E.; Dixon, L.B.; Newby, P.K.; Tucker, K.L.; Krebs-Smith, S.M.; Guenther, P.M. Dietary Patterns: Challenges and Opportunities in Dietary Patterns Research. J. Am. Diet. Assoc. 2007, 107, 1233–1239. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef] [PubMed]
- Vormund, K.; Braun, J.; Rohrmann, S.; Bopp, M.; Ballmer, P.; Faeh, D. Mediterranean diet and mortality in Switzerland: An alpine paradox? Eur. J. Nutr. 2015, 54, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Ocké, M.C. Evaluation of methodologies for assessing the overall diet: Dietary quality scores and dietary pattern analysis. Proc. Nutr. Soc. 2013, 72, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.L.; Whincup, P.H.; Morris, R.W.; Lennon, L.T.; Papacosta, O.; Wannamethee, S.G. Dietary patterns and the risk of CVD and all-cause mortality in older British men. Br. J. Nutr. 2016, 116, 1246–1255. [Google Scholar] [CrossRef] [PubMed]
- Nanri, A.; Mizoue, T.; Shimazu, T.; Ishihara, J.; Takachi, R.; Noda, M.; Iso, H.; Sasazuki, S.; Sawada, N.; Tsugane, S.; Japan Public Health Center-Based Prospective Study Group. Dietary patterns and all-cause, cancer, and cardiovascular disease mortality in Japanese men and women: The Japan public health center-based prospective study. PLoS ONE 2017, 12, e0174848. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Zazpe, I.; Razquin, C.; Sanchez-Tainta, A.; Corella, D.; Salas-Salvado, J.; Toledo, E.; Ros, E.; Muñoz, M.Á.; Recondo, J.; et al. Empirically-derived food patterns and the risk of total mortality and cardiovascular events in the PREDIMED study. Clin. Nutr. 2015, 34, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Böthig, S. WHO MONICA Project: Objectives and design. Int. J. Epidemiol. 1989, 18, S29–S37. [Google Scholar] [CrossRef] [PubMed]
- Gutzwiller, F.; Nater, B.; Martin, J. Community-based primary prevention of cardiovascular disease in Switzerland: Methods and results of the National Research Program (NRP 1A). Prev. Med. 1985, 14, 482–491. [Google Scholar] [CrossRef]
- Bopp, M.; Spoerri, A.; Zwahlen, M.; Gutzwiller, F.; Paccaud, F.; Braun-Fahrländer, C.; Rougemont, A.; Egger, M. Cohort Profile: The Swiss National Cohort-a longitudinal study of 6.8 million people. Int. J. Epidemol. 2009, 38, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Bochud, M.; Chatelan, A.; Blanco, J.-M.; Beer-Borst, S.; Federal Office of Public Health and the Food Safety and Veterinary Office. Anthropometric Characteristics and Indicators of Eating and Physical Activity Behaviors in the Swiss Adult Population. Available online: https://www.blv.admin.ch/blv/de/home/lebensmittel-und-ernaehrung/ernaehrung/menuch/menu-ch-ergebnisse-essverhalten.html (accessed on 27 July 2017).
- Bopp, M.; Braun, J.; Faeh, D.; Gutzwiller, F. Establishing a follow-up of the Swiss MONICA participants (1984–1993): Record linkage with census and mortality data. BMC Public Health 2010, 10, 562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bopp, M.; Braun, J.; Gutzwiller, F.; Faeh, D.; Swiss National Cohort Study Group. Health Risk or Resource? Gradual and Independent Association between Self-Rated Health and Mortality Persists Over 30 Years. PLoS ONE 2012, 7, e30795. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenacre, M.; Blasius, J. Multiple Correspondence Analysis and Related Methods, 1st ed.; Chapman & Hall/CRC Statistics in the Social and Behavioral Sciences; CRC Press: Boca Raton, FL, USA, 2006; ISBN 9781584886280. [Google Scholar]
- Tenenhaus, M.; Young, F.W. An analysis and synthesis of multiple correspondence analysis, optimal scaling, dual scaling, homogeneity analysis and other methods for quantifying categorical multivariate data. Psychometrika 1985, 50, 91–119. [Google Scholar] [CrossRef]
- Greenacre, M.J. Interpreting multiple correspondence analysis. Appl. Stoch. Models Data Anal. 1991, 7, 195–210. [Google Scholar] [CrossRef]
- Ward, J.H. Hierarchical Grouping to Optimize an Objective Function. J. Am. Stat. Assoc. 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Fransen, H.P.; May, A.M.; Stricker, M.D.; Boer, J.M.A.; Hennig, C.; Rosseel, Y.; Ocké, M.C.; Peeters, P.H.M.; Beulens, J.W.J. A posteriori dietary patterns: How many patterns to retain? J. Nutr. 2014, 144, 1274–1282. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: Design and Applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Husson, F.; Lê, S.; Pagès, J. Exploratory Multivariate Analysis by Example Using R, 2nd ed.; Chapman & Hall/CRC Computer Science & Data Analysis; CRC Press: Boca Raton, FL, USA, 2017; ISBN 9781138196346. [Google Scholar]
- Brenner, H.; Gefeller, O.; Greenland, S. Risk and rate advancement periods as measures of exposure impact on the occurrence of chronic diseases. Epidemiology 1993, 4, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Lê, S.; Josse, J.; Husson, F. FactoMineR: An R Package for Multivariate Analysis. J. Stat. Softw. 2008, 25. [Google Scholar] [CrossRef]
- Greenwood, D.C.; Cade, J.E.; Draper, A. Seven unique food consumption patterns identifed among women in the UK Women’s Cohort Study. Eur. J. Clin. Nutr. 2000, 54, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Slattery, M.L.; Boucher, K.M.; Caan, B.J.; Potter, J.D.; Ma, K.N. Eating patterns and risk of colon cancer. Am. J. Epidemiol. 1998, 148, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.; Hu, F.B.; Fuchs, C.; Giovannucci, E.; Hunter, D.J.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C. Major dietary patterns and the risk of colorectal cancer in women. Arch. Intern. Med. 2003, 163, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Pryer, J.A.; Nichols, R.; Elliott, P.; Thakrar, B.; Brunner, E.; Marmot, M. Dietary patterns among a national random sample of British adults. J. Epidemiol. Community Health 2001, 55, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Terry, P.; Hu, F.B.; Hansen, H.; Wolk, A. Prospective study of major dietary patterns and colorectal cancer risk in women. Am. J. Epidemiol. 2001, 154, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Engeset, D.; Alsaker, E.; Ciampi, A.; Lund, E. Dietary patterns and lifestyle factors in the Norwegian EPIC cohort: The Norwegian Women and Cancer (NOWAC) study. Eur. J. Clin. Nutr. 2005, 59, 675–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, F.B.; Rimm, E.; Smith-Warner, S.A.; Feskanich, D.; Stampfer, M.J.; Ascherio, A.; Sampson, L.; Willett, W.C. Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am. J. Clin. Nutr. 1999, 69, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Bronner, L.; Willett, W.C.; Stampfer, M.J.; Rexrode, K.M.; Albert, C.M.; Hunter, D.; Manson, J.E. Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA 2002, 287, 1815–1821. [Google Scholar] [CrossRef] [PubMed]
- Oomen, C.M.; Feskens, E.J.; Räsänen, L.; Fidanza, F.; Nissinen, A.M.; Menotti, A.; Kok, F.J.; Kromhout, D. Fish consumption and coronary heart disease mortality in Finland, Italy, and The Netherlands. Am. J. Epidemiol. 2000, 151, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Lippke, S.; Nigg, C.R.; Maddock, J.E. Health-promoting and health-risk behaviors: Theory-driven analyses of multiple health behavior change in three international samples. Int J. Behav. Med. 2012, 19, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Hou, L.N.; Chen, W.; Chen, P.L.; Lei, C.Y.; Wei, Q.; Tan, W.L.; Zheng, S.B. Associations of dietary patterns with the risk of all-cause, CVD and stroke mortality: A meta-analysis of prospective cohort studies. Br. J. Nutr. 2015, 113, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Couto, E.; Boffetta, P.; Lagiou, P.; Ferrari, P.; Buckland, G.; Overvad, K.; Dahm, C.C.; Tjønneland, A.; Olsen, A.; Clavel-Chapelon, F.; et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer 2011, 104, 1493–1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zazpe, I.; Sanchez-Tainta, A.; Toledo, E.; Sanchez-Villegas, A.; Martinez-Gonzalez, M.A. Dietary patterns and total mortality in a Mediterranean cohort: The SUN project. J. Acad. Nutr. Diet. 2014, 114, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; Foote, J.A.; Wilkens, L.R.; Basiotis, P.P.; Carlson, A.; White, K.K.L.; Yonemori, K.M. Simple measures of dietary variety are associated with improved dietary quality. J. Am. Diet. Assoc. 2006, 106, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Krebs-Smith, S.M.; Smiciklas-Wright, H.; Guthrie, H.A.; Krebs-Smith, J. The effects of variety in food choices on dietary quality. J. Am. Diet. Assoc. 1987, 87, 897–903. [Google Scholar] [PubMed]
- Foote, J.A.; Murphy, S.P.; Wilkens, L.R.; Basiotis, P.P.; Carlson, A. Dietary variety increases the probability of nutrient adequacy among adults. J. Nutr. 2004, 134, 1779–1785. [Google Scholar] [CrossRef] [PubMed]
- Psota, T.L.; Gebauer, S.K.; Kris-Etherton, P. Dietary omega-3 fatty acid intake and cardiovascular risk. Am. J. Cardiol. 2006, 98, 3i–18i. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M. Omega-3 fatty acids and cancers: A systematic update review of epidemiological studies. Br. J. Nutr. 2012, 107, S228–S239. [Google Scholar] [CrossRef] [PubMed]
- World Cancer Research Fund International: Continuous Update Project Matrix. Available online: http://www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports (accessed on 20 September 2017).
- Parkin, D.M.; Boyd, L.; Walker, L.C. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br. J. Cancer 2011, 105, S2–S5. [Google Scholar] [CrossRef] [PubMed]
- Borges, C.A.; Rinaldi, A.E.; Conde, W.L.; Mainardi, G.M.; Behar, D.; Slater, B. Dietary patterns: A literature review of the methodological characteristics of the main step of the multivariate analyzes. Rev. Bras. Epidemiol. 2015, 18, 837–857. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.D.; Emmett, P.M.; Newby, P.K.; Northstone, K. Dietary patterns obtained through principal components analysis: The effect of input variable quantification. Br. J. Nutr. 2013, 109, 1881–1891. [Google Scholar] [CrossRef] [PubMed]
- Millen, B.E.; Quatromoni, P.A.; Gagnon, D.R.; Cupples, L.A.; Franz, M.M.; D'Agostino, R.B. Dietary patterns of men and women suggest targets for health promotion: The Framingham Nutrition Studies. Am. J. Health Promot. 1996, 11, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Gorst-Rasmussen, A.; Dahm, C.C.; Dethlefsen, C.; Scheike, T.; Overvad, K. Exploring dietary patterns by using the treelet transform. Am. J. Epidemiol. 2011, 173, 1097–1104. [Google Scholar] [CrossRef] [PubMed]
- Jacques, P.F.; Tucker, K.L. Are dietary patterns useful for understanding the role of diet in chronic disease? Am. J. Clin. Nutr. 2001, 73, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Panaretos, D.; Tzavelas, G.; Vamvakari, M.; Panagiotakos, D. Repeatability of dietary patterns extracted through multivariate statistical methods: A literature review in methodological issues. Int. J. Food Sci. Nutr. 2017, 68, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Nanri, A.; Shimazu, T.; Ishihara, J.; Takachi, R.; Mizoue, T.; Inoue, M.; Tsugane, S. Reproducibility and validity of dietary patterns assessed by a food frequency questionnaire used in the 5-year follow-up survey of the Japan Public Health Center-Based Prospective Study. J. Epidemiol. 2012, 22, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Khani, B.R.; Ye, W.; Terry, P.; Wolk, A. Reproducibility and validity of major dietary patterns among Swedish women assessed with a food-frequency questionnaire. J. Nutr. 2004, 134, 1541–1545. [Google Scholar] [CrossRef] [PubMed]
- Sauvageot, N.; Schritz, A.; Leite, S.; Alkerwi, A.; Stranges, S.; Zannad, F.; Streel, S.; Hoge, A.; Donneau, A.-F.; Albert, A.; Guillaume, M. Stability-based validation of dietary patterns obtained by cluster analysis. Nutr. J. 2017, 16, 4. [Google Scholar] [CrossRef] [PubMed]
| Overall | Females | Males | Missing | |
|---|---|---|---|---|
| Total | 15,936 (100) | 8143 (51.1) | 7793 (48.9) | |
| Number of deaths | 4630 (29.1) | 2077 (25.5) | 2553 (32.8) | |
| Age, year | 45.0 ± 13.5 | 45.2 ± 13.8 | 44.8 ± 13.1 | |
| Survival time, year | 25.5 ± 9.1 | 26.3 ± 8.6 | 24.6 ± 9.4 | |
| BMI | 15 (0.1) | |||
| <25 kg/m2 | 8845 (55.5) | 5317 (65.3) | 3528 (45.3) | |
| 25–30 kg/m2 | 5503 (34.5) | 2069 (25.4) | 3434 (44.1) | |
| ≤30 kg/m2 | 1573 (9.9) | 752 (9.2) | 821 (10.5) | |
| Nationality | 0 (0) | |||
| Swiss | 12,949 (81.3) | 6829 (83.9) | 6120 (78.5) | |
| Foreign | 2987 (18.7) | 1314 (16.1) | 1673 (21.5) | |
| Education | 20 (0.1) | |||
| Mandatory | 5504 (34.5) | 3339 (41.0) | 2165 (27.8) | |
| Upper secondary | 7567 (47.5) | 3649 (44.8) | 3918 (50.3) | |
| Tertiary | 2845 (17.9) | 1143 (14.0) | 1702 (21.8) | |
| Physical activity | 253 (1.6) | |||
| <1×/week | 8722 (54.7) | 4534 (55.7) | 4188 (53.7) | |
| 1×/week | 3497 (21.9) | 1891 (23.2) | 1606 (20.6) | |
| >1×/week | 3464 (21.7) | 1568 (19.3) | 1896 (24.3) | |
| Smoking | 25 (0.2) | |||
| Never | 7533 (47.3) | 4945 (60.7) | 2588 (33.2) | |
| Former | 2699 (16.9) | 822 (10.1) | 1877 (24.1) | |
| Light | 3232 (20.3) | 1601 (19.7) | 1631 (20.9) | |
| Heavy | 2447 (15.4) | 758 (9.3) | 1689 (21.7) | |
| Alcohol | 93 (0.6) | |||
| No | 7087 (44.5) | 4896 (60.1) | 2191 (28.1) | |
| Moderate | 5971 (37.5) | 2571 (31.6) | 3400 (43.6) | |
| High | 2785 (17.5) | 622 (7.6) | 2163 (27.8) |
| Overall | Women | Men | ||||
|---|---|---|---|---|---|---|
| Basic | Multivariable | Basic | Multivariable | Basic | Multivariable | |
| ALL CAUSE | ||||||
| Number of deaths | n = 4264 | n = 1947 | n = 2317 | |||
| “Sausage and Vegetables” | 1 | 1 | 1 | 1 | 1 | 1 |
| “Meat and Salad” | 0.92 (0.84–1.00) | 0.94 (0.86–1.03) | 0.90 (0.77–1.04) | 0.93 (0.80–1.08) | 0.93 (0.82–1.04) | 0.95 (0.85–1.07) |
| “Fish” | 0.79 (0.71–0.88) | 0.87 (0.78–0.97) | 0.93 (0.79–1.09) | 0.98 (0.83–1.15) | 0.77 (0.67–0.90) | 0.82 (0.71–0.96) |
| “Traditional” | 0.81 (0.73–0.90) | 0.89 (0.80–0.98) | 0.84 (0.80–1.10) | 1.02(0.87–1.19) | 0.75 (0.65–0.85) | 0.81 (0.71–0.93) |
| “High-fiber foods” | 0.76 (0.69–0.83) | 0.92 (0.84–1.02) | 0.82 (0.72–0.95) | 0.91 (0.79–1.05) | 0.84 (0.74–0.95) | 0.94 (0.83–1.08) |
| CARDIOVASCULAR DISEASE | ||||||
| Number of deaths | n = 1432 | n = 662 | n = 770 | |||
| “Sausage and Vegetables” | 1 | 1 | 1 | 1 | 1 | 1 |
| “Meat and Salad” | 1.01 (0.86–1.19) | 1.02 (0.87–1.20) | 1.05 (0.81–1.37) | 1.07 (0.82–1.39) | 0.97 (0.78–1.19) | 0.98 (0.50–1.21) |
| “Fish” | 0.85 (0.70–1.03) | 0.91 (0.75–1.11) | 1.22 (0.92–1.63) | 1.24 (0.93–1.65) | 0.69 (0.52–0.91) | 0.73 (0.55–0.97) |
| “Traditional” | 0.83 (0.69–1.00) | 0.87 (0.73–1.04) | 1.00 (0.75–1.32) | 1.06 (0.79–1.41) | 0.73 (0.57–0.93) | 0.76 (0.59–0.98) |
| “High-fiber foods” | 0.84 (0.71–0.99) | 0.99 (0.85–1.18) | 0.92 (0.72–1.18) | 0.98 (0.76–1.26) | 0.94 (0.75–1.17) | 1.02 (0.81–1.28) |
| CANCER | ||||||
| Number of deaths | n = 1460 | n = 634 | n = 826 | |||
| “Sausage and Vegetables” | 1 | 1 | 1 | 1 | 1 | 1 |
| “Meat and Salad” | 0.91 (0.78–1.06) | 0.95 (0.82–1.11) | 0.83 (0.65–1.07) | 0.88 (0.68–1.12) | 0.96 (0.80–1.17) | 0.95 (0.82–1.20) |
| “Fish” | 0.72 (0.60–0.86) | 0.82 (0.68–0.99) | 0.71 (0.54–0.94) | 0.77 (0.58–1.02) | 0.80 (0.63–1.03) | 0.87 (0.68–1.12) |
| “Traditional” | 0.83 (0.70–0.98) | 0.93 (0.79–1.10) | 0.95 (0.74–1.23) | 1.04 (0.81–1.35) | 0.77 (0.62–0.97) | 0.86 (0.69–1.08) |
| “High-fiber foods” | 0.68 (0.58–0.80) | 0.85 (0.72–1.00) | 0.69 (0.54–0.88) | 0.77 (0.60–0.99) | 0.79 (0.63–0.98) | 0.92 (0.74–1.16) |
| OTHER CAUSES | ||||||
| Number of deaths | n = 1372 | n = 651 | n = 721 | |||
| “Sausage and Vegetables” | 1 | 1 | 1 | 1 | 1 | 1 |
| “Meat and Salad” | 0.83 (0.71–0.98) | 0.86 (0.73–1.01) | 0.83 (0.64–1.09) | 0.86 (0.66–1.13) | 0.96 (0.80–1.17) | 0.99 (0.82–1.20) |
| “Fish” | 0.81 (0.67–0.97) | 0.89 (0.73–1.08) | 0.94 (0.71–1.26) | 0.99 (0.74–1.32) | 0.80 (0.63–1.08) | 0.87 (0.68–1.12) |
| “Traditional” | 0.79 (0.66–0.94) | 0.86 (0.72–1.03) | 0.87 (0.67–1.15) | 0.95 (0.72–1.25) | 0.77 (0.62–0.97) | 0.86 (0.69–1.08) |
| “High-fiber foods” | 0.77 (0.65–0.90) | 0.93 (0.79–1.10) | 0.88 (0.69–1.12) | 0.99 (0.77–1.26) | 0.79 (0.63–0.98) | 0.92 (0.74–1.16) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krieger, J.-P.; Cabaset, S.; Pestoni, G.; Rohrmann, S.; Faeh, D.; Swiss National Cohort Study Group. Dietary Patterns Are Associated with Cardiovascular and Cancer Mortality among Swiss Adults in a Census-Linked Cohort. Nutrients 2018, 10, 313. https://doi.org/10.3390/nu10030313
Krieger J-P, Cabaset S, Pestoni G, Rohrmann S, Faeh D, Swiss National Cohort Study Group. Dietary Patterns Are Associated with Cardiovascular and Cancer Mortality among Swiss Adults in a Census-Linked Cohort. Nutrients. 2018; 10(3):313. https://doi.org/10.3390/nu10030313
Chicago/Turabian StyleKrieger, Jean-Philippe, Sophie Cabaset, Giulia Pestoni, Sabine Rohrmann, David Faeh, and Swiss National Cohort Study Group. 2018. "Dietary Patterns Are Associated with Cardiovascular and Cancer Mortality among Swiss Adults in a Census-Linked Cohort" Nutrients 10, no. 3: 313. https://doi.org/10.3390/nu10030313





