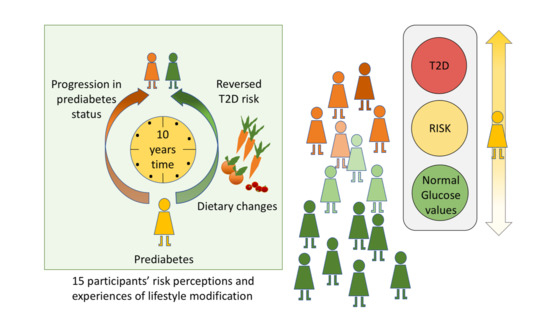
“I Did Not Believe You Could Get Better”—Reversal of Diabetes Risk Through Dietary Changes in Older Persons with Prediabetes in Region Stockholm
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Design and Participant Selection
- Impaired Glucose Tolerance (IGT) on OGTT (fasting plasma glucose < 7.0 mmol/L and 2 h plasma glucose > 7.8 and < 11.1 mmol/L) AND HbA1c > 42 mmol/mol
- Impaired Fasting Glucose (IFG) on OGTT [fasting plasma glucose > 6.1 and < 6.9 mmol/L and 2 h plasma glucose < 7.8 mmol/L, if measured] AND HbA1c > 42 mmol/mol
- Newly diagnosed diabetes (fasting plasma glucose > 7.0 mmol/L or 2 h plasma glucose > 11.1 mmol/L) without prior diagnosis of T2D or treatment with any anti-diabetic medication in the intervening period.
2.3. Data Collection and Analysis
3. Results
3.1. T2D Risk is Not Urgent Enough to Act Upon
- “I think I would worry if I felt symptoms, this with bad blood circulation and sensations in the feet… Impaired vision. Or something like that, but I don’t have these warning signs”. (ID: 6)
- “At first, I thought: Yes, but oh what a relief that I didn’t have it [diabetes] then. Then it wasn’t really a risk anyway. Because you don’t know. You can go and carry on something you don’t know about”. (ID: 1)
- “For me, it [the risk of diabetes] is not so bad. The fear is when they say that you have a tumor, malignant.” (ID: 2)
- “I was a little unsure of what I was told … I interpreted the answer of elevated values as it could mean normal, because it wasn’t a diagnosis. And it made me unsure about the answer. So, I did not dare to interpret it as anything else than that I remained at risk as before, because I didn’t believe you could get better. That you remain where you are. So that’s my interpretation.” (ID: 10)
- “Because if you have four values or five test results [different types of blood tests]. If one of them says that you have prediabetes, then I do not have it in my world, because there are the four other values.” (ID: 5)
3.2. Adaptations in Everyday Life as a Part of Aging
- … “We have changed diet. (…) Yes and then I’ve been to the hospital when my husband … and I demanded that we needed a nutritionist.” (ID: 7)
- “But then when I’m away, I don’t know what sort of eating monster that (laughing) that I am... but I’m trying to stay away from it.” (ID: 7)
- -
- “If you received information now that you are at risk, how do you think you would…?”
- -
- Then I would go to the doctor and let him decide.
- -
- But if he tells you: You are at risk?
- -
- Then he can tell me what to do.” (ID: 12)
3.3. Diagnosis as a Motive for Change
- “Yes, but it is when I have been diagnosed that I’m grasping it. That’s when I kind of have to put in the effort.” (ID: 8)
- “No, because I know that if I develop diabetes, it is possible to live a good life anyway. And at the same time when you come to that situation, perhaps you can think of keeping sugar values down more. To walk or move and then kind of eat up your own sugar, or not consume wrong foods.” (ID: 9)
- “Yes, prediabetes feels calmer, but diabetes is more regulated, more on track and with insulin and so, more control throughout the day. So, it’s more structured. More locked. So, you should avoid getting there.” (ID: 7)
- “Then I thought: Now I will change this totally. Now I will turn this and see if it helps. Then I started quite hard with a lot of vegetables and skipped all the grease. And after some time, I went for new tests, and they showed them to me, and there was nothing.” (ID: 8)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lupton, D. Risk as moral danger: The social and political functions of risk discourse in public health. Int. J. Health Serv. 1993, 23, 3425–3435. [Google Scholar] [CrossRef]
- Sachs, L.T.A.; Tischelman, C. Risk in numbers? difficulties in the transformation of genetic knowledge from research to people? The case of hereditary cancer. Acta Oncol. 2009, 40, 4445–4453. [Google Scholar] [CrossRef] [PubMed]
- Linell, P.; Adelswärd, V.; Sachs, L.; Bredmar, M.; Lindstedt, U. Expert talk in medical contexts: Explicit and implicit orientation to risks. Res. Lang. Soc. Interact. 2002, 35, 2195–2218. [Google Scholar] [CrossRef]
- Slovic, P.; Finucane, M.L.; Peters, E.; MacGregor, D.G. Risk as analysis and risk as feelings: Some thoughts about affect, reason, risk, and rationality. Risk Anal. Int. J. 2004, 24, 2311–2322. [Google Scholar] [CrossRef] [PubMed]
- Sachs, L. Att Leva Med Risk: Fem Kvinnor, Gentester Och Kunskapens Frukter; Gedin: Stockholm, Sweden, 1998. [Google Scholar]
- World Health Organisation. Global Status Report on Non Communical Diseases 2014. Available online: https://www.who.int/nmh/publications/ncd-status-report-2014/en/ (accessed on 1 February 2016).
- International Diabetes Federation. IDF Global Diabetes Plan 2011–2021. Available online: https://idf.org/our-activities/advocacy-awareness/resources-and-tools/129-global-diabetes-plan-2011-2021.html (accessed on 1 February 2016).
- International Diabetes Federation. IDF Clinical Practice Recommendations for Managing Type 2 Diabetes in Primary Care 2017. Available online: https://www.idf.org/e-library/guidelines/128-idf-clinical-practice-recommendations-for-managing-type-2-diabetes-in-primary-care.html (accessed on 1 October 2017).
- Ramos, L.R.; Malta, D.C.; Gomes, G.A.D.O.; Bracco, M.M.; Florindo, A.A.; Mielke, G.I.; Parra, D.C.; Lobelo, F.; Simoes, E.J.; Hallal, P.C. Prevalence of health promotion programs in primary health care units in Brazil. Revista De Saude Publica 2014, 48, 837–844. [Google Scholar] [CrossRef] [Green Version]
- Parker, W.-A.; Steyn, N.P.; Levitt, N.S.; Lombard, C.J. Health promotion services for patients having non-communicable diseases: Feedback from patients and health care providers in Cape Town, South Africa. BMC Public Health 2012, 12, 1503. [Google Scholar] [CrossRef]
- Schülein, S.; Taylor, K.J.; Schriefer, D.; Blettner, M.; Klug, S.J. Participation in preventive health check-ups among 19,351 women in Germany. Prev. Med. Rep. 2017, 6, 23–26. [Google Scholar] [CrossRef]
- Kohro, T.; Furui, Y.; Mitsutake, N.; Fujii, R.; Morita, H.; Oku, S.; Ohe, K.; Nagai, R. The Japanese national health screening and intervention program aimed at preventing worsening of the metabolic syndrome. Int. Heart J. 2008, 49, 2193–2203. [Google Scholar] [CrossRef]
- Hellenius, M.-L.; Faire, U.D.; Krakau, I.; Berglund, B. Prevention of cardiovascular disease within the primary health care system: Feasibility of a prevention programme within the Sollentuna primary health care catchment area. Scand. J. Prim. Health Care 1993, 11, 168–173. [Google Scholar] [CrossRef]
- Björkelund, C.; Bengtsson, C. Feasibility of a primary health care programme aiming at reducing cardiovascular and cerebrovascular risk factors among women in a swedish community, strömstad. Scand. J. Prim. Health Care 1991, 9, 289–295. [Google Scholar] [CrossRef]
- Lingfors, H.; Lindström, K.; Persson, L.-G.; Bengtsson, C.; Lissner, L. Lifestyle changes after a health dialogue results from the live for life health promotion programme. Scand. J. Prim. Health Care 2003, 21, 4248–4252. [Google Scholar] [CrossRef] [PubMed]
- Karolinska Institutet. SMART2D. Available online: http://ki.se/en/phs/smart2d (accessed on 15 January 2019).
- Karolinska Institutet. Program 4D. 2017. Updated 2018; Cited 2019. Available online: http://ki.se/medarbetare/program-4d (accessed on 15 January 2019).
- World Health Organisation. Global Report on Diabetes. Available online: https://apps.who.int/iris/bitstream/handle/10665/204874/WHO_NMH_NVI_16.3_eng.pdf?sequence=1 (accessed on 3 November 2016).
- Adriaanse, M.; Snoek, F.; Dekker, J.; Van der Ploeg, H.; Heine, R.J. Screening for type 2 diabetes: An exploration of subjects’ perceptions regarding diagnosis and procedure. Diabet. Med. 2002, 19, 5406–5411. [Google Scholar]
- Simmons, D.; Zgibor, J.C. Should we screen for type 2 diabetes among asymptomatic individuals? Yes. Diabetologia 2017, 60, 2148–2152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vähäsarja, K.; Kasila, K.; Kettunen, T.; Rintala, P.; Salmela, S.; Poskiparta, M. I saw what the future direction would be: Experiences of diabetes risk and physical activity after diabetes screening. Br. J. Health Psychol. 2015, 20, 1172–1193. [Google Scholar] [CrossRef]
- Eborall, H.; Davies, R.; Kinmonth, A.L.; Griffin, S.; Lawton, J. Patients’ experiences of screening for type 2 diabetes: Prospective qualitative study embedded in the ADDITION (Cambridge) randomised controlled trial. BMJ 2007, 335, 490. [Google Scholar] [CrossRef]
- Alvarsson, M.; Hilding, A.; Östenson, C.G. Factors determining normalization of glucose intolerance in middle-aged Swedish men and women: A 8–10-year follow-up. Diabet. Med. 2009, 26, 4345–4353. [Google Scholar] [CrossRef]
- Glechner, A.; Keuchel, L.; Affengruber, L.; Titscher, V.; Sommer, I.; Matyas, N.; Wagner, G.; Kien, C.; Klerings, I.; Gartlehner, G. Effects of lifestyle changes on adults with prediabetes: A systematic review and meta-analysis. Prim. Care Diabetes 2018, 12, 393–408. [Google Scholar] [CrossRef]
- Paxton, R.; Scott, S. Nonsmoking reinforced by improvements in lung function. Addict. Behav. 1981, 6, 4313–4315. [Google Scholar] [CrossRef]
- Furst, T.; Connors, M.; Bisogni, C.A.; Sobal, J.; Falk, L.W. Food choice: A conceptual model of the process. Appetite 1996, 26, 3247–3266. [Google Scholar] [CrossRef]
- Ouellette, J.A.; Wood, W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol. Bull. 1998, 124, 54. [Google Scholar] [CrossRef]
- Lauque, S.; Nourashemi, F.; Soleilhavoup, C.; Guyonnet, S.; Bertiere, M.; Sachet, P.; Vellas, B.; Albarede, J.L. A prospective study of changes on nutritional patterns 6 months before and 18 months after retirement. J. Nutr. Health Aging 1998, 2, 288–291. [Google Scholar]
- Zins, M.; Guéguen, A.; Kivimaki, M.; Singh-Manoux, A.; Leclerc, A.; Vahtera, J.; Westerlund, H.; Ferrie, J.E.; Goldberg, M. Effect of retirement on alcohol consumption: Longitudinal evidence from the French Gazel cohort study. PLoS ONE 2011, 6, 10e26531. [Google Scholar] [CrossRef] [PubMed]
- Helldán, A.; Lallukka, T.; Rahkonen, O.; Lahelma, E. Changes in healthy food habits after transition to old age retirement. Eur. J. Public Health 2011, 22, 4582–4586. [Google Scholar] [CrossRef] [PubMed]
- Young, K.; Bunn, F.; Trivedi, D.; Dickinson, A. Nutritional education for community dwelling older people: A systematic review of randomised controlled trials. Int. J. Nurs. Stud. 2011, 48, 6751–6780. [Google Scholar] [CrossRef] [PubMed]
- Group DPPR. Achieving weight and activity goals among diabetes prevention program lifestyle participants. Obes. Res. 2004, 12, 91426–91434. [Google Scholar]
- Pachucki, M.A.; Jacques, P.F.; Christakis, N.A. Social network concordance in food choice among spouses, friends, and siblings. Am. J. Public Health 2011, 101, 2170–2177. [Google Scholar] [CrossRef]
- Darlow, S.D.; Xu, X. The influence of close others’ exercise habits and perceived social support on exercise. Psychol. Sport Exerc. 2011, 12, 5575–5578. [Google Scholar] [CrossRef]
- Bahr, D.B.; Browning, R.C.; Wyatt, H.R.; Hill, J.O. Exploiting social networks to mitigate the obesity epidemic. Obesity 2009, 17, 4723–4728. [Google Scholar] [CrossRef]
- Adriaanse, M.A.; Kroese, F.M.; Gillebaart, M.; De Ridder, D.T. Effortless inhibition: Habit mediates the relation between self-control and unhealthy snack consumption. Front. Psychol. 2014, 5, 444. [Google Scholar] [CrossRef]
- Sachs, L. Is there a pathology of prevention? The implications of visualizing the invisible in screening programs. Cult. Med. Psychiatry 1995, 19, 4503–4525. [Google Scholar] [CrossRef]
- Smith-Morris, C. The chronicity of life, the acuteness of diagnosis. In Chronic Conditions, Fluid States: Chronicity and the Anthropology of Illness; Manderson, L., Smith-Morris, C., Eds.; Rutgers University Press: New Brunswik, NB, Canada, 2010; pp. 21–37. [Google Scholar]
- Andersen, J.H.; Whyte, S.R. Measuring risk, managing values: Health technology and subjectivity in Denmark. Anthropol. Med. 2014, 21, 3265–3276. [Google Scholar] [CrossRef] [PubMed]
- Brinkmann, S.; Petersen, A. Diagnoser: Perspektiver, Kritik Og Discussion; Klim: Aarhus, Denmark, 2016. [Google Scholar]
- Andersson, S.; Ekman, I.; Lindblad, U.; Friberg, F. It’s up to me! Experiences of living with pre-diabetes and the increased risk of developing type 2 diabetes mellitus. Prim. Care Diabetes 2008, 2, 4187–4193. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.J.; Moran, M.R.; Tang, J.W.; Vargas, M.C.; Talen, M.; Zimmermann, L.J.; Ackermann, R.T.; Kandula, N.R. Patient perceptions about prediabetes and preferences for diabetes prevention. Diabetes Educ. 2016, 42, 6667–6677. [Google Scholar] [CrossRef] [PubMed]
- Jallinoja, P.; Pajari, P.; Absetz, P. Repertoires of lifestyle change and self-responsibility among participants in an intervention to prevent type 2 diabetes. Scand. J. Caring Sci. 2008, 22, 3455–3462. [Google Scholar] [CrossRef] [PubMed]
- Troughton, J.; Jarvis, J.; Skinner, C.; Robertson, N.; Khunti, K.; Davies, M. Waiting for diabetes: Perceptions of people with pre-diabetes: A qualitative study. Patient Educ. Couns. 2008, 72, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Taloyan, M.; Fresk, M.; Seijbolt, K.; Risberg, D. Kartläggning Av Vården Vid Typ-2 Diabetes I Stockholms Läns Landsting. 2015. Available online: https://studylibsv.com/doc/590064/kartl%C3%A4ggning-av-v%C3%A5rden-vid-typ-2-diabetes-i-stockholms-l%C3%A4ns (accessed on 2 May 2016).
- Socialstyrelsen. Nationella Riktlinjer för Diabetesvård: Socialstyrelsen. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/nationella-riktlinjer/2018-10-25.pdf (accessed on 4 March 2019).
- Stockholms Läns Landsting. Viss 2015 Updated 2018; Cited 2019. Available online: http://www.viss.nu/Handlaggning/Vardprogram/Endokrina-organ/Prediabetes/ (accessed on 4 March 2019).
- Hälso och Sjukvårdsförvaltningen. Diabetes I Primärvården 2013. Available online: https://www.vardgivarguiden.se/globalassets/utbildning-och-utveckling/vardutveckling/fokusrapporter/diabetes-inom-primarvarden-2013.pdf?IsPdf=true (accessed on 4 March 2019).
- Andersson, C. Challenges of Studying Complex Community Health Promotion Programmes: Experiences from Stockholm Diabetes Prevention Programme; Karolinska Institutet: Stockholm, Sweden, 2006. [Google Scholar]
- Andersson, C.M.; Bjärås, G.E.; Östenson, C.-G. A stage model for assessing a community-based diabetes prevention program in Sweden. Health Promot. Int. 2002, 17, 4317–4327. [Google Scholar] [CrossRef]
- Bjärås, G.; Ahlbom, A.; Alvarsson, M.; Burström, B.; Diderichsen, F.; Efendic, S.; Grill, V.; Haglund, B.J.; Norman, A.; Persson, P.G.; et al. Strategies and methods for implementing a community-based diabetes primary prevention program in Sweden. Health Promot. Int. 1997, 12, 2151–2160. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 6349–6357. [Google Scholar] [CrossRef]
- World Health Organisation. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycemia; World Health Organisation: Geneva, Switzerland, 2006; Available online: https://apps.who.int/iris/bitstream/handle/10665/43588/9241594934_eng.pdf; jsessionid=C87B2553E38FAA0CDDCAFD8C1A82E25E?sequence=1 (accessed on 20 October 2019).
- World Health Organisation. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of DiabetesMellitus. Available online: https://www.who.int/diabetes/publications/report-hba1c_2011.pdf?ua=1 (accessed on 20 October 2019).
- Malterud, K.; Siersma, V.D.; Guassora, A.D. Sample size in qualitative interview studies: Guided by information power. Qual. Health Res. 2016, 26, 131753–131760. [Google Scholar] [CrossRef]
- Wildavsky, A.; Dake, K. Theories of risk perception: Who fears what and why? Daedalus 1990, 119, 41–60. [Google Scholar]
- Slovic, P.; Fischhoff, B.; Lichtenstein, S. Why study risk perception? Risk Anal. 1982, 2, 283–293. [Google Scholar] [CrossRef]
- Barter, C.R.E. The use of vignettes in qualitative research. Soc. Res. Update 1999, 25, 1–4. [Google Scholar]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Fainzang, S. Lying, secrecy and power within the doctor-patient relationship. Anthropol. Med. 2002, 9, 2117–2133. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; MacKison, D.; Swanson, V.; Donnan, P.; Emslie-Smith, A.; Lawton, J. Self-monitoring of blood glucose in type 2 diabetes: Patients’ perceptions of" high" readings. Diabetes Technol. Ther. 2015, 17, S6. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, B. Diagnosing overdiagnosis: Conceptual challenges and suggested solutions. Eur. J. Epidemiol. 2014, 29, 9599–9604. [Google Scholar] [CrossRef]
- van Dijk, W.; Faber, M.J.; Tanke, M.A.; Jeurissen, P.P.; Westert, G.P. Medicalisation and overdiagnosis: What society does to medicine. Int. J. Health Policy Manag. 2016, 5, 11619. [Google Scholar] [CrossRef]
- Illich, I. Medical nemesis. J. Epidemiol. Community Health 2003, 57, 12919–12922. [Google Scholar] [CrossRef]
- Walker, C.G.; Solis-Trapala, I.; Holzapfel, C.; Ambrosini, G.L.; Fuller, N.R.; Loos, R.J.; Hauner, H.; Caterson, I.D.; Jebb, S.A. Modelling the interplay between lifestyle factors and genetic predisposition on markers of type 2 diabetes mellitus risk. PLoS ONE 2015, 10, 7e0131681. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Cavanaugh, K.; Huizinga, M.M.; Wallston, K.A.; Gebretsadik, T.; Shintani, A.; Davis, D.; Gregory, R.P.; Fuchs, L.; Malone, R.; Cherrington, A.; et al. Association of numeracy and diabetes control. Ann. Intern. Med. 2008, 148, 737–746. [Google Scholar] [CrossRef]
- Rothman, R.L.; Montori, V.M.; Cherrington, A.; Pignone, M.P. Perspective: The role of numeracy in health care. J. Health Commun. 2008, 13, 6583–6595. [Google Scholar] [CrossRef]
- Schapira, M.M.; Nattinger, A.B.; McHorney, C.A. Frequency or probability? A qualitative study of risk communication formats used in health care. Med. Decis. Mak. 2001, 21, 6459–6467. [Google Scholar] [CrossRef]
- Anderson, R.M.; Funnell, M.M. Patient empowerment: Reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ. Couns. 2005, 57, 2153–2157. [Google Scholar] [CrossRef]
- Anderson, R.M.; Funnell, M.M. Patient empowerment: Myths and misconceptions. Patient Educ. Couns. 2010, 79, 3277–3282. [Google Scholar] [CrossRef]
- Swartz, D.L. The sociology of habit: The perspective of Pierre Bourdieu. OTJR Occup. Participa. Health 2002, 22, 61S–69S. [Google Scholar] [CrossRef]
- Schmier, J.K.; Halpern, M.T. Patient recall and recall bias of health state and health status. Expert Rev. Pharm. Outcomes Res. 2004, 4, 2159–2163. [Google Scholar] [CrossRef]
- Stull, D.E.; Leidy, N.K.; Parasuraman, B.; Chassany, O. Optimal recall periods for patient-reported outcomes: Challenges and potential solutions. Curr. Med. Res. Opin. 2009, 25, 4929–4942. [Google Scholar] [CrossRef]
- Levine, L.J.; Safer, M.A. Sources of bias in memory for emotions. Curr. Dir. Psychol. Sci. 2002, 11, 5169–5173. [Google Scholar] [CrossRef]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016, 9, 211. [Google Scholar] [CrossRef]
- Van de Mortel, T.F. Faking it: Social desirability response bias in self-report research. Aust. J. Adv. Nurs. 2008, 25, 440. [Google Scholar]
- Fisher, R.J. Social desirability bias and the validity of indirect questioning. J. Consum. Res. 1993, 20, 2303–2315. [Google Scholar] [CrossRef]


| Participant ID | Sex | Age | Education Level | Household Status | Medical Status Reported by SDPP in 2014–2017 |
|---|---|---|---|---|---|
| 1 | Female | 68 | Secondary/upper secondary school | Lives together with partner | Reversed T2D risk |
| 2 | Female | 70 | College/University | Lives alone | Reversed T2D risk |
| 3 | Male | 72 | Secondary/upper secondary school | Lives together with partner | Reversed T2D risk |
| 4 | Male | 70 | Secondary/upper secondary school | Lives alone | Progression of T2D risk |
| 5 | Male | 71 | College/University | Lives together with partner | Progression of T2D risk |
| 6 | Male | 71 | Secondary/upper secondary school | Lives together with partner | Progression of T2D risk |
| 7 | Female | 67 | College/University | Lives together with partner | Reversed T2D risk |
| 8 | Female | 71 | Secondary/upper secondary school | Lives together with partner | Progression of T2D risk |
| 9 | Female | 68 | Secondary/upper secondary school | Lives together with partner | Progression of T2D risk |
| 10 | Male | 58 | College/University | Lives together with partner | Reversed T2D risk |
| 11 | Male | 70 | Secondary/upper secondary school | Lives alone | Reversed T2D risk |
| 12 | Male | 72 | Secondary/upper secondary school | Lives together with partner | Reversed T2D risk |
| 13 | Female | 71 | Secondary/upper secondary school | Lives alone | Reversed T2D risk |
| 14 | Female | 73 | Secondary/upper secondary school | Lives together with partner | Reversed T2D risk |
| 15 | Male | 72 | College/University | Lives alone | Reversed T2D risk |
| Theme | T2D Risk is not Perceived as Concrete Enough to Motivate Lifestyle Modification without Other External Triggers | |||||||
|---|---|---|---|---|---|---|---|---|
| Category | T2D Risk is not Urgent Enough to Change Behavior | Adaptations in Everyday Life as a Part of Aging | Diagnosis as a Motive for Change | |||||
| Sub category | T2D is perceived as intangible | Difficult to understand what T2D risk means | Information is not enough to produce change | Common habits change together with others | Lifestyle modification trade offs | Responsibility of medical authority | T2D diagnosis as a reason to change habits | Other diagnosis than T2D as motive for change |
| Code | Risk is not concrete Prediabetes is not a real diagnosis Risk is invisible Absence of disease No fear of prediabetes | Uncertainty about what risk means Increased risk is normal Uncertainty about meaning of numbers Numbers as a tool for understanding risk information Risk is an abstract concept | Repetition is not useful Awareness of risk Obvious things Information is wanted but creates uncertainty Common sense | Eating as social activity Familiar preferences Shared responsibility Control for partner’s health Support each other | Weight reduction Aging Indulge oneself Pain Social events Willingness to replace diet Changes over time | Trust in healthcare Continuity in care Experts’ help Others positive experiences Believe in the doctors’ capacity Advice | Proof of having disease Medication Numbers make T2D visible Strict Fear of insulin injections Regulation | Disease is structured Diagnose Control Changes in diet is needed Changed level of physical activity because of diagnosis Partner’s diagnosis |
| Participant ID | Recruitment Status | Perception of Risk at the First Follow up 2004–2005 | Lifestyle Modifications between First and Second Follow up | Perception of Risk at the Second Follow up 2014–2017 |
|---|---|---|---|---|
| 1 | Reversed T2D risk | Yes, at risk | Active lifestyle changes because of T2D risk and weight reduction | Reversed T2D risk |
| 2 | Reversed T2D risk | Yes, at risk | Dietary changes because of stomach problems | Reversed T2D risk |
| 3 | Reversed T2D risk | No, not at risk “It was ok” | No active lifestyle changes | Do not know |
| 4 | Progression of T2D risk | No, not at risk “I interpreted it as it was good” | No active lifestyle changes | Increased T2D risk |
| 5 | Progression of T2D risk | No, not at risk “No, I haven’t received a response” | No active lifestyle changes because of T2D risk. Eats healthy and is physically active | No change |
| 6 | Progression of T2D risk | Yes, at risk | No active lifestyle changes | Increased T2D risk, but “Nothing alarming” |
| 7 | Reversed T2D risk | Yes, at risk | Active lifestyle changes because of T2D risk | Reversed T2D risk |
| 8 | Progression of T2D risk | Yes, at risk | No active lifestyle changes 10 years back, but active lifestyle changes after information from the last follow up | Increased T2D risk (interpreted as diabetic values) |
| 9 | Progression of T2D risk | Yes, at risk | No active lifestyle changes | Increased T2D risk |
| 10 | Reversed T2D risk | Yes, at risk | Dietary changes because of stomach problems | No change |
| 11 | Reversed T2D risk | No, not at risk “Not at a particular risk” | Dietary changes because partner’s change in choices of food | No change |
| 12 | Reversed T2D risk | No, not at risk | No active lifestyle changes | Reversed T2D risk |
| 13 | Reversed T2D risk | Yes, at risk | Dietary changes because of stomach problems | Reversed T2D risk |
| 14 | Reversed T2D risk | No, not at risk “But maybe I have always had a little risk” | Dietary changes to reduce weight | Increased T2D risk |
| 15 | Reversed T2D risk | Yes, at risk | Active lifestyle changes because of T2D risk | Reversed T2D risk |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Timm, L.; Daivadanam, M.; Lager, A.; Forsberg, B.; Östenson, C.-G.; Mölsted Alvesson, H. “I Did Not Believe You Could Get Better”—Reversal of Diabetes Risk Through Dietary Changes in Older Persons with Prediabetes in Region Stockholm. Nutrients 2019, 11, 2658. https://doi.org/10.3390/nu11112658
Timm L, Daivadanam M, Lager A, Forsberg B, Östenson C-G, Mölsted Alvesson H. “I Did Not Believe You Could Get Better”—Reversal of Diabetes Risk Through Dietary Changes in Older Persons with Prediabetes in Region Stockholm. Nutrients. 2019; 11(11):2658. https://doi.org/10.3390/nu11112658
Chicago/Turabian StyleTimm, Linda, Meena Daivadanam, Anton Lager, Birger Forsberg, Claes-Göran Östenson, and Helle Mölsted Alvesson. 2019. "“I Did Not Believe You Could Get Better”—Reversal of Diabetes Risk Through Dietary Changes in Older Persons with Prediabetes in Region Stockholm" Nutrients 11, no. 11: 2658. https://doi.org/10.3390/nu11112658