Geriatric Nutritional Risk Index Is Associated with Unique Health Conditions and Clinical Outcomes in Chronic Kidney Disease Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Body Composition Measurements
2.3. Laboratory Measurements
2.4. Geriatric Nutritional Risk Index
2.5. Outcomes
2.6. Statistical Analyses
3. Results
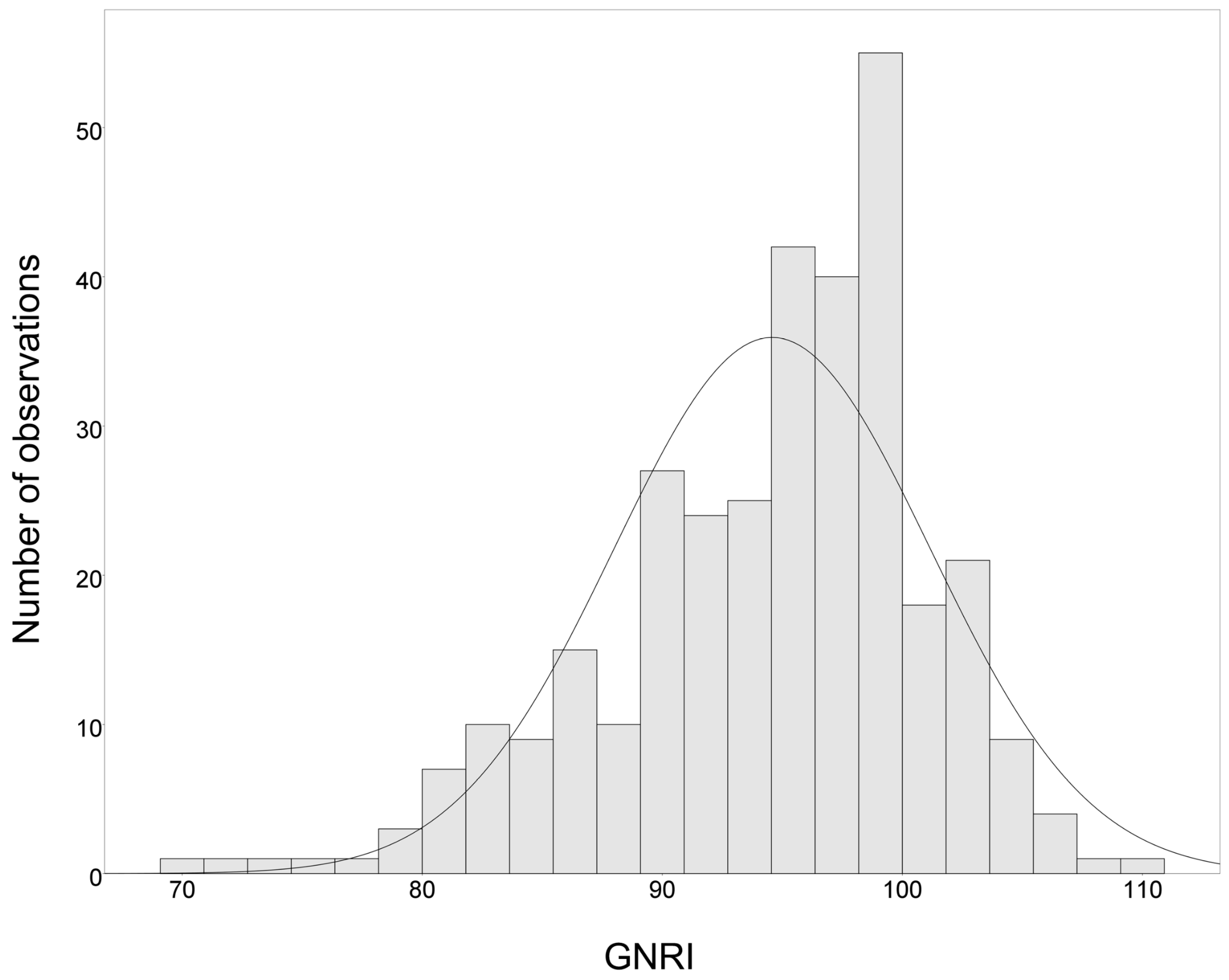
3.1. Patient Characteristics
3.2. Variables Associated with the GNRI
3.3. Association of the GNRI with Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Xie, Y.; Bowe, B.; Mokdad, A.H.; Xian, H.; Yan, Y.; Li, T.; Maddukuri, G.; Tsai, C.Y.; Floyd, T.; Al Aly, Z. Analysis of the Global Burden of Disease Study Highlights the Global, Regional, and National Trends of Chronic Kidney Disease Epidemiology From 1990 to 2016. Kidney Int. 2018, 94, 567–581. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J.; Thomas, F.; Nagy, K.; Nagy, K.; Arogundade, F.; Avesani, C.M.; Chan, M.; Chmielewski, M.; Cordeiro, A.C.; Espinosa Cuevas, A.; et al. Global Prevalence of Protein-Energy Wasting in Kidney Disease: A Meta-Analysis of Contemporary Observational Studies from the International Society of Renal Nutrition and Metabolism. J. Ren. Nutr. 2018, 28, 380–392. [Google Scholar] [CrossRef] [PubMed]
- Su, C.T.; Yabes, J.; Pike, F.; Weiner, D.E.; Beddhu, S.; Burrowes, J.D.; Rocco, M.V.; Unruh, M.L. Changes in Anthropometry and Mortality in Maintenance Hemodialysis Patients in the HEMO Study. Am. J. Kidney Dis. 2013, 62, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.L. The Mini Nutritional Assessment (MNA) and its Use in Grading the Nutritional State of Elderly Patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Ferguson, M.; Capra, S.; Bauer, J.; Banks, M. Development of a Valid and Reliable Malnutrition Screening Tool for Adult Acute Hospital Patients. Nutrition 1999, 15, 458–464. [Google Scholar] [CrossRef]
- Stratton, R.J.; Hackston, A.; Longmore, D.; Dixon, R.; Price, S.; Stroud, M.; King, C.; Elia, M. Malnutrition in Hospital Outpatients and Inpatients: Prevalence, Concurrent Validity and Ease of Use of the Malnutrition Universal Screening Tool (‘MUST’) for Adults. Br. J. Nutr. 2004, 92, 799–808. [Google Scholar] [CrossRef]
- Kondru, J.; Rasmussen, H.H.; Hamberg, O.; Stanga, Z.; Ad Hoc ESPEN Working Group. Nutritional risk Screening (NRS 2002): A New Method Based on an Analysis of Controlled Clinical Trials. Clin. Nutr. 2003, 22, 321–336. [Google Scholar] [CrossRef]
- Ikizler, T.A. A Patient with CKD and Poor Nutritional Status. Clin. J. Am. Soc. Nephrol. 2013, 8, 2174–2182. [Google Scholar] [CrossRef]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A New Index for Evaluating At-Risk Elderly Medical Patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef]
- Fouque, D.; Kalantar Zadeh, K.; Kopple, J.; Cano, N.; Chauveau, P.; Cuppari, L.; Franch, H.; Guarnieri, G.; Ikizler, T.A.; Kaysen, G.; et al. A Proposed Nomenclature and Diagnostic Criteria for Protein-Energy Wasting in Acute and Chronic Kidney Disease. Kidney Int. 2008, 73, 391–398. [Google Scholar] [CrossRef]
- Takahashi, H.; Inoue, K.; Shimizu, K.; Hiraga, K.; Takahashi, E.; Otaki, K.; Yoshikawa, T.; Furuta, K.; Tokunaga, C.; Sakakibara, T.; et al. Tokai Renal Nutrition Study Group. Comparison of Nutritional Risk Scores for Predicting Mortality in Japanese Chronic Hemodialysis Patients. J. Ren. Nutr. 2017, 27, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Furuya, R.; Takita, T.; Maruyama, Y.; Yamaguchi, Y.; Ohkawa, S.; Kumagai, H. Simplified Nutritional Screening Tools for Patients on Maintenance Hemodialysis. Am. J. Clin. Nutr. 2008, 87, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.; Kuo, K.L.; Peng, C.H.; Wu, C.H.; Lien, Y.C.; Wang, Y.C.; Tarng, D.C. Volume Overload Correlates with Cardiovascular Risk Factors in Patients with Chronic Kidney Disease. Kidney Int. 2014, 85, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Hung, S.C.; Lai, Y.S.; Kuo, K.L.; Tarng, D.C. Volume Overload and Adverse Outcomes in Chronic Kidney Disease: Clinical Observational and Animal Studies. J. Am. Heart Assoc. 2015, 4, e001918. [Google Scholar] [CrossRef]
- Chamney, P.W.; Wabel, P.; Moissl, U.M.; Muller, M.J.; Bosy Westphal, A.; Korth, O.; Fuller, N.J. A Whole-Body Model to Distinguish Excess Fluid from the Hydration of Major Body Tissues. Am. J. Clin. Nutr. 2007, 85, 80–89. [Google Scholar] [CrossRef]
- Yokoyama, H.; Kanno, S.; Takahashi, S.; Yamada, D.; Itoh, H.; Saito, K.; Sone, H.; Haneda, M. Determinants of Decline in Glomerular Filtration Rate in Nonproteinuric Subjects with or without Diabetes and Hypertension. Clin. J. Am. Soc. Nephrol. 2009, 4, 1432–1440. [Google Scholar] [CrossRef]
- Turin, T.C.; James, M.; Ravani, P.; Tonelli, M.; Manns, B.J.; Quinn, R.; Jun, M.; Klarenbach, S.; Hemmelgarn, B.R. Proteinuria and Rate of Change in Kidney Function in a Community-Based Population. J. Am. Soc. Nephrol. 2013, 24, 1661–1667. [Google Scholar] [CrossRef]
- Esmeray, K.; Dizdar, O.S.; Erdem, S.; Gunal, A.I. Effect of Strict Volume Control on Renal Progression and Mortality in Non-Dialysis-Dependent Chronic Kidney Disease Patients: A Prospective Interventional Study. Med. Princ. Pract. 2018, 27, 420–427. [Google Scholar] [CrossRef]
- Paisley, K.E.; Beaman, M.; Tooke, J.E.; Mohamed Ali, V.; Lowe, G.D.; Shore, A.C. Endothelial Dysfunction and Inflammation in Asymptomatic Proteinuria. Kidney Int. 2003, 63, 624–633. [Google Scholar] [CrossRef]
- Wang, A.Y.; Sanderson, J.; Sea, M.M.; Wang, M.; Lam, C.W.; Li, P.K.; Lui, S.F.; Woo, J. Important Factors Other than Dialysis Adequacy Associated with Inadequate Dietary Protein and Energy Intakes in Patients Receiving Maintenance Peritoneal Dialysis. Am. J. Clin. Nutr. 2003, 77, 834–841. [Google Scholar] [CrossRef]
- Anders, H.J.; Andersen, K.; Stecher, B. The Intestinal Microbiota, a Leaky Gut, and Abnormal Immunity in Kidney Disease. Kidney Int. 2013, 83, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Stenvinkel, P.; Heimburger, O.; Paultre, F.; Diczfalusy, U.; Wang, T.; Berglund, L.; Jogestrand, T. Strong Association Between Malnutrition, Inflammation, and Atherosclerosis in Chronic Renal Failure. Kidney Int. 1999, 55, 1899–1911. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J.; Stenvinkel, P.; Cuppari, L.; Ikizler, T.A.; Kalantar Zadeh, K.; Kaysen, G.; Mitch, W.E.; Price, S.R.; Wanner, C.; Wang, A.Y.; et al. Etiology of the Protein-Energy Wasting Syndrome in Chronic Kidney Disease: A Consensus Statement from the International Society of Renal Nutrition and Metabolism (ISRNM). J. Ren. Nutr. 2013, 23, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Menon, V.; Greene, T.; Wang, X.; Pereira, A.A.; Marcovina, S.M.; Beck, G.J.; Kusek, J.W.; Collins, A.J.; Levey, A.S.; Sarnak, M.J. C-Reactive Protein and Albumin as Predictors of All-Cause and Cardiovascular Mortality in Chronic Kidney Disease. Kidney Int. 2005, 68, 766–772. [Google Scholar] [CrossRef]
- Barreto, D.V.; Barreto, F.C.; Liabeuf, S.; Temmar, M.; Lemke, H.D.; Tribouilloy, C.; Choukroun, G.; Vanholder, R.; Massy, Z.A.; European Uremic Toxin Work Group (EUTox). Plasma Interleukin-6 is Independently Associated with Mortality in Both Hemodialysis and Pre-Dialysis Patients with Chronic Kidney Disease. Kidney Int. 2010, 77, 550–556. [Google Scholar] [CrossRef]
- Honda, H.; Qureshi, A.R.; Heimburger, O.; Barany, P.; Wang, K.; Pecoits Filho, R.; Stenvinkel, P.; Lindholm, B. Serum Albumin, C-Reactive Protein, Interleukin 6, and Fetuin a as Predictors of Malnutrition, Cardiovascular Disease, and Mortality in Patients with ESRD. Am. J. Kidney Dis. 2006, 47, 139–148. [Google Scholar] [CrossRef]
- Matsuo, Y.; Kumakura, H.; Kanai, H.; Iwasaki, T.; Ichikawa, S. The Geriatric Nutritional Risk Index Predicts Long-Term Survival and Cardiovascular or Limb Events in Peripheral Arterial Disease. J. Atheroscler. Thromb. 2019. [Google Scholar] [CrossRef]
- Minamisawa, M.; Seidelmann, S.B.; Claggett, B.; Hegde, S.M.; Shah, A.M.; Desai, A.S.; Lewis, E.F.; Shah, S.J.; Sweitzer, N.K.; Fang, J.C.; et al. Impact of Malnutrition Using Geriatric Nutritional Risk Index in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2019, 7, 664–675. [Google Scholar] [CrossRef]
- Kuo, I.C.; Huang, J.C.; Wu, P.Y.; Chen, S.C.; Chang, J.M.; Chen, H.C. A Low Geriatric Nutrition Risk Index is Associated with Progression to Dialysis in Patients with Chronic Kidney Disease. Nutrients 2017, 9, 1228. [Google Scholar] [CrossRef]
- Kiuchi, A.; Ohashi, Y.; Tai, R.; Aoki, T.; Mizuiri, S.; Ogura, T.; Aikawa, A.; Sakai, K. Association Between Low Dietary Protein Intake and Geriatric Nutrition Risk Index in Patients with Chronic Kidney Disease: A Retrospective Single-Center Cohort Study. Nutrients 2016, 8, 662. [Google Scholar] [CrossRef]
- Kalantar Zadeh, K.; Kopple, J.D.; Block, G.; Humphreys, M.H. A Malnutrition-Inflammation Score is Correlated with Morbidity and Mortality in Maintenance Hemodialysis Patients. Am. J. Kidney Dis. 2001, 38, 1251–1263. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Characteristics | GNRI Tertiles | p Value | ||
|---|---|---|---|---|
| T1 (n = 109) | T2 (n = 109) | T3 (n = 108) | ||
| Age (years) | 66.7 ± 14.2 | 66.4 ± 12.4 | 64.3 ± 13.3 | 0.375 |
| Male sex, n (%) | 69 (63.3%) | 66 (60.6%) | 89 (82.4%) b,c | 0.001 |
| Smoking history, n (%) | 25 (22.9%) | 21 (19.3%) | 21 (19.4%) | 0.752 |
| DM, n (%) | 65 (59.6%) | 45 (41.3%) a | 38 (35.2%) c | 0.001 |
| CVD, n (%) | 30 (27.5%) | 24 (22.0%) | 23 (21.3%) | 0.497 |
| CHF, n (%) | 12 (11%) | 9 (8.3%) | 6 (5.6%) | 0.346 |
| CAD, n (%) | 15 (13.8%) | 8 (7.3%) | 15 (13.9%) | 0.227 |
| CVA, n (%) | 12 (11%) | 9 (8.3%) | 4 (3.7%) | 0.124 |
| RAAS, n (%) | 66 (60.6%) | 63 (57.8%) | 67 (62.0%) | 0.811 |
| CCB, n (%) | 64 (58.7%) | 53 (48.6%) | 49 (45.4%) | 0.122 |
| Furosemide, n (%) | 36 (33.3%) | 19 (17.4%) | 12 (11.1%) | <0.001 |
| No. of antihypertensives | 2.32 ± 1.32 | 1.92 ± 1.36 | 1.84 ± 1.38 | 0.020 |
| Statin, n (%) | 31 (28.4%) | 26 (23.9%) | 29 (26.9%) | 0.738 |
| BMI (kg/m2) | 25.3 ± 4.6 | 26.0 ± 3.9 | 26.4 ± 3.7 | 0.160 |
| FTI (kg/m2) | 9.5 ± 4.4 | 10.2 ± 4.0 | 9.6 ± 4.5 | 0.403 |
| LTI (kg/m2) | 14.5 ± 3.2 | 15.0 ± 2.9 | 16.2 ± 3.3 b,c | <0.001 |
| Overhydration (%) | 13.2 ± 9.5 | 7.0 ± 7.2 a | 4.4 ± 6.4 b,c | <0.001 |
| Fat percentage (%) | 27.1 ± 9.9 | 28.4 ± 8.7 | 26.1 ± 9.7 | 0.201 |
| Systolic BP (mmHg) | 142.3 ± 17.6 | 136.8 ± 18.6 a | 133.7 ± 13.9 c | 0.001 |
| eGFR (ml/min/1.73 m2) | 25.7 ± 14.6 | 27.2 ± 14.3 | 33.7 ± 14.2 b,c | <0.001 |
| UPCR (g/g) | 2.40 (0.86–4.97) | 0.84 (0.40–1.68) a | 0.38 (0.15–0.94) b,c | <0.001 |
| Albumin (g/dL) | 3.1 ± 0.3 | 3.7 ± 0.1 a | 4.0 ± 0.2 b,c | <0.001 |
| Fasting glucose (mg/dL) | 127 ± 46 | 118 ± 39 | 117 ± 39 | 0.147 |
| Total cholesterol (mg/dL) | 183 ± 47 | 175 ± 39 | 167 ± 33 c | 0.020 |
| Triglycerides (mg/dL) | 152 ± 107 | 171 ± 126 | 167 ± 109 | 0.441 |
| hs-CRP (mg/L) | 5.5 (1.7–12.3) | 3.4 (1.1–9.1) | 3.4 (1.2–8.0) c | 0.033 |
| IL-6 (pg/mL) | 5.00 (3.14–8.94) | 3.17 (2.07–5.41) a | 2.93 (1.45–4.30) c | <0.001 |
| TNF-α (pg/mL) | 8.51 (6.48–11.03) | 6.15 (4.72–8.97) a | 5.48 (3.21–7.62) b,c | <0.001 |
| Characteristic | Univariate | Multivariate a | ||
|---|---|---|---|---|
| β Coefficient (95% CI) | p Value | β Coefficient (95% CI) | p Value | |
| Age | −0.035 (−0.089, 0.019) | 0.204 | - | - |
| Male sex | 2.142 (0.612, 3.673) | 0.006 | - | - |
| DM (Presence) | −3.217 (−4.615, −1.818) | <0.001 | - | - |
| Previous CVD (Presence) | −1.074 (−2.760, 0.613) | 0.211 | - | - |
| LTI (kg/m2) | 0.466 (0.247, 0.684) | <0.001 | - | - |
| Overhydration (%) | −0.373 (−0.446, −0.301) | <0.001 | −0.245 (−0.322, −0.169) | <0.001 |
| Systolic BP (mmHg) | −0.088 (−0.128, −0.047) | <0.001 | - | - |
| eGFR (ml/min/1.73 m2) | 0.068 (0.020, 0.117) | 0.006 | - | - |
| log UPCR (g/g) | −5.303 (−6.400, −4.207) | <0.001 | −3.424 (−4.532, −2.316) | <0.001 |
| log IL−6 (pg/mL) | −5.349 (−7.103, −3.596) | <0.001 | −3.002 (−4.551, −1.458) | <0.001 |
| ESRD | Composite Outcome | |||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Unadjusted | ||||
| T2 + T3 | Reference | Reference | ||
| T1 | 3.57 (2.40–5.30) | <0.001 | 3.43 (2.24–5.26) | <0.001 |
| Model 1 | ||||
| T2 + T3 | Reference | Reference | ||
| T1 | 3.54 (2.38–5.25) | <0.001 | 3.08 (2.01–4.72) | <0.001 |
| Model 2 | ||||
| T2 + T3 | Reference | Reference | ||
| T1 | 3.15 (1.95–5.07) | <0.001 | 1.79 (1.10–2.92) | 0.019 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, T.-Y.; Hung, S.-C. Geriatric Nutritional Risk Index Is Associated with Unique Health Conditions and Clinical Outcomes in Chronic Kidney Disease Patients. Nutrients 2019, 11, 2769. https://doi.org/10.3390/nu11112769
Lin T-Y, Hung S-C. Geriatric Nutritional Risk Index Is Associated with Unique Health Conditions and Clinical Outcomes in Chronic Kidney Disease Patients. Nutrients. 2019; 11(11):2769. https://doi.org/10.3390/nu11112769
Chicago/Turabian StyleLin, Ting-Yun, and Szu-Chun Hung. 2019. "Geriatric Nutritional Risk Index Is Associated with Unique Health Conditions and Clinical Outcomes in Chronic Kidney Disease Patients" Nutrients 11, no. 11: 2769. https://doi.org/10.3390/nu11112769




