A Personalised Dietary Approach—A Way Forward to Manage Nutrient Deficiency, Effects of the Western Diet, and Food Intolerances in Inflammatory Bowel Disease
Abstract
:1. Introduction
2. Nutrient Deficiencies Associated with IBD
2.1. Nutritional Status of People with Inflammatory Bowel Disease
2.2. Nutrient Absorption Impacted by Genotype
3. The Western Diet
3.1. Lower Intakes of Dietary Fibre
3.2. Increased Consumption of Saturated Fatty Acids
3.3. Fructose and Sugar Consumption
3.4. Other Western Diet Factors
4. Food Intolerances
4.1. FODMAPs
4.2. Gluten
4.3. Dairy Products and Lactose
4.4. Brassica
4.5. Mustard, Wasabi, Raw and Cooked Tomatoes and Sweet Potatoes
4.6. Mushrooms
4.7. Sulphur Dioxide, Sulphites and Sulphur Compounds
5. Ethical Issues
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Zeevi, D.; Korem, T.; Zmora, N.; Israeli, D.; Rothschild, D.; Weinberger, A.; Ben-Yacov, O.; Lador, D.; Avnit-Sagi, T.; Lotan-Pompan, M. Personalized nutrition by prediction of glycemic responses. Cell 2015, 163, 1079–1094. [Google Scholar] [CrossRef]
- Ercolini, D.; Fogliano, V. Food design to feed the human gut microbiota. J. Agric. Food Chem. 2018, 66, 3754–3758. [Google Scholar] [CrossRef] [PubMed]
- Grissinger, M. The five rights: A destination without a map. Pharm. Ther. 2010, 35, 542. [Google Scholar]
- Halawi, H.; Camilleri, M. Pharmacogenetics and the treatment of functional gastrointestinal disorders. Pharmacogenomics 2017, 18, 1085–1094. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Shen, J.; Seifer, B.J.; Jiang, S.; Wang, J.; Xiong, H.; Xie, L.; Wang, L.; Sui, X. Approaches and genetic determinants in predicting response to neoadjuvant chemotherapy in locally advanced gastric cancer. Oncotarget 2017, 8, 30477–30494. [Google Scholar] [CrossRef] [PubMed]
- Racine, A.; Carbonnel, F.; Chan, S.S.; Hart, A.R.; Bueno-de-Mesquita, H.B.; Oldenburg, B.; van Schaik, F.D.; Tjonneland, A.; Olsen, A.; Dahm, C.C.; et al. Dietary patterns and risk of inflammatory bowel disease in europe: Results from the EPIC Study. Inflamm. Bowel Dis. 2016, 22, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Frazier-Wood, A.C. Dietary patterns, genes, and health: Challenges and obstacles to be overcome. Curr. Nutr. Rep. 2015, 4, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, L.R. Nutrigenetics, nutrigenomics and inflammatory bowel diseases. Expert Rev. Clin. Immunol. 2013, 9, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Vagianos, K.; Bector, S.; McConnell, J.; Bernstein, C.N. Nutrition assessment of patients with inflammatory bowel disease. J. Parenter. Enter. Nutr. 2007, 31, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Stein, J.; Bott, C. Diet and Nutrition in Crohn’s Disease and Ulcerative Colitis 20 Questions 20 Answers; Falk Foundation e.V.: Freiburg, Germany, 2008. [Google Scholar]
- Basson, A. Nutrition management in the adult patient with Crohn’s disease. S. Afr. J. Clin. Nutr. 2012, 25, 164–172. [Google Scholar] [CrossRef]
- Harries, A.; Rhodes, J. Undernutrition in Crohn’s disease: An anthropometric assessment. Clin. Nutr. 1985, 4, 87–89. [Google Scholar] [CrossRef]
- Gassull, M.A.; Cabré, E. Nutrition in inflammatory Bowel disease. Curr. Opin. Clin. Nutr. Metab. Care 2001, 4, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Lomer, M.C.; Kodjabashia, K.; Hutchinson, C.; Greenfield, S.M.; Thompson, R.P.; Powell, J.J. Intake of dietary iron is low in patients with Crohn’s disease: A case–control study. Br. J. Nutr. 2004, 91, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Hartman, C.; Marderfeld, L.; Davidson, K.; Mozer-Glassberg, Y.; Poraz, I.; Silbermintz, A.; Zevit, N.; Shamir, R. Food intake adequacy in children and adolescents with inflammatory Bowel disease. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Lourenço, S.; Hussein, T.; Bologna, S.; Sipahi, A.; Nico, M. Oral manifestations of inflammatory Bowel Disease: A review based on the observation of six cases. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 204–207. [Google Scholar] [CrossRef]
- Malins, T.; Wilson, A.; Ward-Booth, R. Recurrent buccal space abscesses: A complication of Crohn’s disease. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 19–21. [Google Scholar] [CrossRef]
- Plauth, M.; Jenss, H.; Meyle, J. Oral manifestations of Crohn’s Disease: An analysis of 79 cases. J. Clin. Gastroenterol. 1991, 13, 29–37. [Google Scholar] [CrossRef]
- Schlosser, B.J.; Pirigyi, M.; Mirowski, G.W. Oral manifestations of hematologic and nutritional diseases. Otolaryngol. Clin. N. Am. 2011, 44, 183–203. [Google Scholar] [CrossRef]
- Thomas, D.M.; Mirowski, G.W. Nutrition and oral mucosal diseases. Clin. Dermatol. 2010, 28, 426–431. [Google Scholar] [CrossRef]
- Rebhan, M.; Chalifa-Caspi, V.; Prilusky, J.; Lancet, D. GeneCards: A novel functional genomics compendium with automated data mining and query reformulation support. Bioinformatics 1998, 14, 656–664. [Google Scholar] [CrossRef]
- D’Ambrosio, D.N.; Clugston, R.D.; Blaner, W.S. Vitamin A metabolism: An update. Nutrients 2011, 3, 63–103. [Google Scholar] [CrossRef] [PubMed]
- Leung, W.; Hessel, S.; Meplan, C.; Flint, J.; Oberhauser, V.; Tourniaire, F.; Hesketh, J.; Von Lintig, J.; Lietz, G. Two common single nucleotide polymorphisms in the gene encoding Β-Carotene 15, 15′-monoxygenase alter Β-carotene metabolism in female volunteers. FASEB J. 2009, 23, 1041–1053. [Google Scholar] [CrossRef] [PubMed]
- Su, H.Y.; Gupta, V.; Day, A.S.; Gearry, R.B. Rising incidence of inflammatory Bowel Disease in Canterbury, New Zealand. Inflamm. Bowel Dis. 2016, 22, 2238–2244. [Google Scholar] [CrossRef] [PubMed]
- University of Otago; Ministry of health New Zealand. A Focus on Nutrition: Key Findings of the 2008/09 New Zealand Adult Nutrition Survey; Ministry of Health: Wellington, New Zealand, 2011.
- Anand, P.K.; Kaul, D. Downregulation of TACO gene transcription restricts mycobacterial entry/survival within human macrophages. FEMS Microbiol. Lett. 2005, 250, 137–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stephensen, C.B. Vitamin A, infection, and immune function. Annu. Rev. Nutr. 2001, 21, 167–192. [Google Scholar] [CrossRef] [PubMed]
- Sommer, A. Vitamin A Deficiency; Wiley Online Library: Hoboken, NJ, USA, 2001. [Google Scholar]
- Thia, K.T.; Loftus, E.V.; Sandborn, W.J.; Yang, S. An update on the epidemiology of inflammatory Bowel Disease in Asia. Am. J. Gastroenterol. 2008, 103, 3167–3182. [Google Scholar] [CrossRef] [PubMed]
- Baumgart, D.C.; Bernstein, C.N.; Abbas, Z.; Colombel, J.F.; Day, A.S.; D’Haens, G.; Dotan, I.; Goh, K.L.; Hibi, T.; Kozarek, R.A. IBD around the world: Comparing the epidemiology, diagnosis, and treatment: Proceedings of the World Digestive Health Day 2010–Inflammatory bowel disease task force meeting. Inflamm. Bowel Dis. 2011, 17, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Gismera, C.S.; Aladren, B.S. Inflammatory Bowel diseases: A disease (s) of modern times? is incidence still increasing? World J. Gastroenterol. 2008, 14, 5491–5498. [Google Scholar] [CrossRef] [PubMed]
- Logan, I.; Bowlus, C.L. The geoepidemiology of autoimmune intestinal diseases. Autoimmun. Rev. 2010, 9, A372–A378. [Google Scholar] [CrossRef] [PubMed]
- Lomer, M.C.; Thompson, R.P.; Powell, J.J. Fine and ultrafine particles of the diet: Influence on the mucosal immune response and association with Crohn’s disease. In Proceedings-Nutrition Society of London; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Persson, P.; Ahlbom, A.; Hellers, G. Diet and inflammatory bowel disease: A case-control study. Epidemiology 1992, 3, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.K.; Abraham, B.; El-Serag, H. Dietary intake and risk of developing inflammatory bowel disease: A systematic review of the literature. Am. J. Gastroenterol. 2011, 106, 563–573. [Google Scholar] [CrossRef]
- Chapman-Kiddell, C.A.; Davies, P.S.; Gillen, L.; Radford-Smith, G.L. Role of diet in the development of inflammatory bowel disease. Inflamm. Bowel Dis. 2010, 16, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Sartor, R.B. Mechanisms of disease: Pathogenesis of Crohn’s disease and ulcerative colitis. Nat. Rev. Gastroenterol. Hepatol. 2006, 3, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Conterno, L.; Fava, F.; Viola, R.; Tuohy, K.M. Obesity and the gut microbiota: Does up-regulating colonic fermentation protect against obesity and metabolic disease? Genes Nutr. 2011, 6, 241–260. [Google Scholar] [CrossRef] [PubMed]
- Myles, I.A. Fast food fever: Reviewing the impacts of the western diet on immunity. Nutr. J. 2014, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Cordain, L.; Eaton, S.B.; Sebastian, A.; Mann, N.; Lindeberg, S.; Watkins, B.A.; O’Keefe, J.H.; Brand-Miller, J. Origins and evolution of the Western diet: Health implications for the 21st century. Am. J. Clin. Nutr. 2005, 81, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Tsironi, E.; Feakins, R.M.; Roberts, C.S.; Rampton, D.S. Incidence of inflammatory bowel disease is rising and abdominal tuberculosis is falling in bangladeshis in East London, United Kingdom. Am. J. Gastroenterol. 2004, 99, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- Dankers, W.; Colin, E.M.; Van Hamburg, J.P.; Lubberts, E. Vitamin D in autoimmunity: Molecular mechanisms and therapeutic potential. Front. Immunol. 2017, 7, 697. [Google Scholar] [CrossRef] [PubMed]
- M’koma, A.E. Inflammatory bowel disease: An expanding global health problem. Clin. Med. Insights Gastroenterol. 2013, 6, S12731. [Google Scholar] [CrossRef] [PubMed]
- Segata, N. Gut microbiome: Westernization and the disappearance of intestinal diversity. Curr. Biolog. 2015, 25, R611–R613. [Google Scholar] [CrossRef] [PubMed]
- Broussard, J.L.; Devkota, S. The changing microbial landscape of Western society: Diet, dwellings and discordance. Mol. Metab. 2016, 5, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Tuohy, K.M.; Conterno, L.; Gasperotti, M.; Viola, R. Up-regulating the human intestinal microbiome using whole plant foods, polyphenols, and/or fiber. J. Agric. Food Chem. 2012, 60, 8776–8782. [Google Scholar] [CrossRef] [PubMed]
- Amre, D.K.; D’Souza, S.; Morgan, K.; Seidman, G.; Lambrette, P.; Grimard, G.; Israel, D.; Mack, D.; Ghadirian, P.; Deslandres, C. Imbalances in dietary consumption of fatty acids, vegetables, and fruits are associated with risk for Crohn’s Disease in children. Am. J. Gastroenterol. 2007, 102, 2016–2025. [Google Scholar] [CrossRef] [PubMed]
- Hou, J.K.; Lee, D.; Lewis, J. Diet and inflammatory bowel disease: Review of patient-targeted recommendations. Clin. Gastroenterol. Hepatol. 2014, 12, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.G.; Fleming, C.R. Nutritional considerations in inflammatory bowel diseases. Gastroenterol. Clin. N. Am. 1995, 24, 597–611. [Google Scholar]
- Reif, S.; Klein, I.; Lubin, F.; Farbstein, M.; Hallak, A.; Gilat, T. Pre-illness dietary factors in inflammatory bowel disease. Gut 1997, 40, 754–760. [Google Scholar] [CrossRef] [PubMed]
- DeVries, J.W. On defining dietary fibre. Proc. Nutr. Soc. 2003, 62, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Jones, J.M. CODEX-aligned dietary fiber definitions help to bridge the ‘fiber gap’. Nutr. J. 2014, 13, 34. [Google Scholar] [CrossRef]
- ACCC International Cereals & Grains association. Dietary Fiber. 2019. Available online: https://www.aaccnet.org/initiatives/definitions/Pages/DietaryFiber.aspx (accessed on 16 March 2019).
- Ashwar, B.A.; Gani, A.; Shah, A.; Wani, I.A.; Masoodi, F.A. Preparation, health benefits and applications of resistant starch—A review. Starch-Stärke 2016, 68, 287–301. [Google Scholar] [CrossRef]
- Higgins, J.A.; Brown, I.L. Resistant starch: A promising dietary agent for the prevention/treatment of inflammatory bowel disease and bowel cancer. Curr. Opin. Gastroenterol. 2013, 29, 190–194. [Google Scholar] [CrossRef]
- Bassaganya-Riera, J.; DiGuardo, M.; Viladomiu, M.; De Horna, A.; Sanchez, S.; Einerhand, A.W.; Sanders, L.; Hontecillas, R. Soluble fibers and resistant starch ameliorate disease activity in interleukin-10–deficient mice with inflammatory bowel disease. J. Nutr. 2011, 141, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Pituch-Zdanowska, A.; Banaszkiewicz, A.; Albrecht, P. The role of dietary fibre in inflammatory bowel disease. Prz Gastroenterol. 2015, 10, 135–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crohn’s & Colitis Foundation of America. Diet, Nutrition, and Inflammatory Bowel Diseases; Crohn’s & Colitis Foundation of America: New York, NY, USA, 2013. [Google Scholar]
- The role of vegetables in the cause remission and regression of Crohn’s disease in an Auckland cohort. Available online: https://researchspace.auckland.ac.nz/handle/2292/19961 (accessed on 17 September 2018).
- Roberts, C.L.; Keita, Å.V.; Duncan, S.H.; O’Kennedy, N.; Söderholm, J.D.; Rhodes, J.M.; Campbell, B.J. Translocation of Crohn’s disease Escherichia coli across M-cells: Contrasting effects of soluble plant fibres and emulsifiers. Gut 2010, 59, 1331–1339. [Google Scholar] [CrossRef] [PubMed]
- Miller, H.; Zhang, J.; Kuolee, R.; Patel, G.B.; Chen, W. Intestinal M cells: The fallible sentinels? World J. Gastroenterol. 2007, 13, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Siebers, A.; Finlay, B.B. M cells and the pathogenesis of mucosal and systemic infections. Trends Microbiol. 1996, 4, 22–29. [Google Scholar] [CrossRef]
- Staudacher, H.M.; Kurien, M.; Whelan, K. Nutritional implications of dietary interventions for managing gastrointestinal disorders. Curr. Opin. Gastroenterol. 2018, 34, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Bockaert, J.; Pin, J.P. Molecular tinkering of G protein-coupled receptors: An evolutionary success. EMBO J. 1999, 18, 1723–1729. [Google Scholar] [CrossRef]
- Stoddart, L.A.; Smith, N.J.; Milligan, G. International union of pharmacology. LXXI. free fatty acid receptors FFA1,-2, and-3: pharmacology and pathophysiological functions. Pharmacol. Rev. 2008, 60, 405–417. [Google Scholar] [CrossRef]
- Senga, T.; Iwamoto, S.; Yoshida, T.; Yokota, T.; Adachi, K.; Azuma, E.; Hamaguchi, M.; Iwamoto, T. LSSIG is a novel murine leukocyte-specific GPCR that is induced by the activation of STAT3. Blood 2003, 101, 1185–1187. [Google Scholar] [CrossRef] [Green Version]
- Fournier, B.; Parkos, C. The role of neutrophils during intestinal inflammation. Mucosal Immunol. 2012, 5, 354–366. [Google Scholar] [CrossRef]
- Le Poul, E.; Loison, C.; Struyf, S.; Springael, J.; Lannoy, V.; Decobecq, M.; Brezillon, S.; Dupriez, V.; Vassart, G.; Van Damme, J. Functional characterization of human receptors for short chain fatty acids and their Role in polymorphonuclear cell activation. J. Biol. Chem. 2003, 278, 25481–25489. [Google Scholar] [CrossRef] [PubMed]
- Bindels, L.B.; Dewulf, E.M.; Delzenne, N.M. GPR43/FFA2: physiopathological relevance and therapeutic prospects. Trends. Pharmacol. Sci. 2013. [Google Scholar] [CrossRef] [PubMed]
- Maslowski, K.M.; Vieira, A.T.; Ng, A.; Kranich, J.; Sierro, F.; Yu, D.; Schilter, H.C.; Rolph, M.S.; Mackay, F.; Artis, D. Regulation of inflammatory responses by gut microbiota and chemoattractant receptor. GPR Nat. 2009, 461, 1282–1286. [Google Scholar] [CrossRef] [PubMed]
- Sivaprakasam, S.; Gurav, A.; Paschall, A.; Coe, G.; Chaudhary, K.; Cai, Y.; Kolhe, R.; Martin, P.; Browning, D.; Huang, L. An essential role of Ffar2 (Gpr43) in dietary fibre-mediated promotion of healthy composition of gut microbiota and suppression of intestinal carcinogenesis. Oncogenesis 2016, 5, e238. [Google Scholar] [CrossRef] [PubMed]
- Bordonaro, M.; Mariadason, J.M.; Aslam, F.; Heerdt, B.G.; Augenlicht, L.H. Butyrate-induced apoptotic cascade in colonic carcinoma cells: modulation of the beta-catenin-Tcf pathway and concordance with effects of sulindac and trichostatin A but not curcumin. Cell Growth Differ. 1999, 10, 713–720. [Google Scholar] [PubMed]
- Evans, W. Pharmacogenomics: Marshalling the human genome to individualise drug therapy. Gut 2003, 52, ii10–ii18. [Google Scholar] [CrossRef] [PubMed]
- Eastwood, M.; Kritchevsky, D. Dietary fiber: How did we get where we are? Annu. Rev. Nutr. 2005, 25, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Maslowski, K.M.; Mackay, C.R. Diet, gut microbiota and immune responses. Nat. Immunol. 2010, 12, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Schneeman, B.O.; Gallaher, D. Effects of dietary fiber on digestive enzyme activity and bile acids in the small intestine. In Proceedings of the Society for Experimental Biology and Medicine; Society for Experimental Biology and Medicine: New York, NY, USA, 1985; pp. 409–414. [Google Scholar]
- Lupton, J.R. Microbial degradation products influence colon cancer risk: The butyrate controversy. J. Nutr. 2004, 134, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Blaut, M.; Clavel, T. Metabolic diversity of the intestinal microbiota: Implications for health and disease. J. Nutr. 2007, 137, 751S–755S. [Google Scholar] [CrossRef]
- National Academy Press. Dietary, Functional and Total Fibre. Available online: https://www.nap.edu/read/10490/chapter/9Accessed (accessed on 9 August 2018).
- Silva, A.F.D.; Schieferdecker, M.E.M.; Amarante, H.M.B.d.S. Food intake in patients with inflammatory bowel disease. ABCD Arq. Bras. Cir. Dig. 2011, 24, 204–209. [Google Scholar] [CrossRef]
- Staudacher, H.M.; Irving, P.M.; Lomer, M.C.; Whelan, K. Mechanisms and efficacy of dietary FODMAP Restriction in IBS. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 256. [Google Scholar] [CrossRef] [PubMed]
- Halmos, E.P.; Christophersen, C.T.; Bird, A.R.; Shepherd, S.J.; Gibson, P.R.; Muir, J.G. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut 2015, 64, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Simopoulos, A.P. Omega-3 fatty acids in health and disease and in growth and development. Am. J. Clin. Nutr. 1991, 54, 438–463. [Google Scholar] [CrossRef] [PubMed]
- Razack, R.; Seidner, D.L. Nutrition in inflammatory bowel disease. Curr. Opin. Gastroenterol. 2007, 23, 400–405. [Google Scholar] [CrossRef]
- Patterson, E.; Wall, R.; Fitzgerald, G.; Ross, R.; Stanton, C. Health implications of high dietary omega-6 polyunsaturated fatty acids. J. Nutr. Metab. 2012, 2012, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kwon, S.; Han, Y.; Hahm, K.; Kim, E. Omega-3 polyunsaturated fatty acids as potential chemopreventive agent for gastrointestinal cancer. J. Cancer. Prev. 2013, 18, 201. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J.; Thomas, C.; Radcliffe, J.; Itsiopoulos, C. Omega-3 fatty acids in early prevention of inflammatory neurodegenerative disease: A focus on Alzheimer’s disease. BioMed Res. Int. 2015, 2015, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pascual, C.Y.; Reche, M.; Fiandor, A.; Valbuena, T.; Cuevas, T.; Esteban, M.M. Fish allergy in childhood. Pediatr. Allergy. Immunol. 2008, 19, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Vitoria, J.C.; Camarero, C.; Sojo, A.; Ruiz, A.; Rodriguez-Soriano, J. Enteropathy related to fish, rice, and chicken. Arch. Dis. Child. 1982, 57, 44–48. [Google Scholar] [PubMed]
- Dannaeus, A.; Johansson, S.; Foucard, T.; Öhman, S. Clinical and immunological aspects of food allergy in childhood I. Estimation of IgG, IgA and IgE antibodies to food antigens in children with food allergy and atopic dermatitis. Acta Paediatrica 1977, 66, 31–37. [Google Scholar] [CrossRef]
- Untersmayr, E.; Schöll, I.; Swoboda, I.; Beil, W.J.; Förster-Waldl, E.; Walter, F.; Riemer, A.; Kraml, G.; Kinaciyan, T.; Spitzauer, S. Antacid medication inhibits digestion of dietary proteins and causes food allergy: A fish allergy model in BALB/C mice. J. Allergy Clin. Immunol. 2003, 112, 616–623. [Google Scholar] [CrossRef]
- Leaf, A.; Weber, P.C. A new era for science in nutrition. Am. J. Clin. Nutr. 1987. [Google Scholar] [CrossRef] [PubMed]
- Eaton, S.B.; Konner, M. Paleolithic nutrition: A consideration of its nature and current implications. N. Engl. J. Med. 1985, 312, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Schaeffer, L.; Gohlke, H.; Muller, M.; Heid, I.M.; Palmer, L.J.; Kompauer, I.; Demmelmair, H.; Illig, T.; Koletzko, B.; Heinrich, J. Common genetic variants of the FADS1 FADS2 gene cluster and their reconstructed haplotypes are associated with the fatty acid composition in phospholipids. Hum. Mol. Genet. 2006, 15, 1745–1756. [Google Scholar] [CrossRef] [PubMed]
- Fajas, L.; Auboeuf, D.; Raspé, E.; Schoonjans, K.; Lefebvre, A.; Saladin, R.; Najib, J.; Laville, M.; Fruchart, J.; Deeb, S. The organization, promoter analysis, and expression of the human PPARγ gene. J. Biol. Chem. 1997, 272, 18779–18789. [Google Scholar] [CrossRef]
- Tai, E.S.; Corella, D.; Demissie, S.; Cupples, L.A.; Coltell, O.; Schaefer, E.J.; Tucker, K.L.; Ordovas, J.M. Polyunsaturated fatty acids interact with the PPARA-L162V polymorphism to affect plasma triglyceride and apolipoprotein C-III concentrations in the Framingham Heart Study. J. Nutr. 2005, 135, 397–403. [Google Scholar] [CrossRef]
- De Keyser, C.E.; Becker, M.L.; Uitterlinden, A.G.; Hofman, A.; Lous, J.J.; Elens, L.; Visser, L.E.; Van Schaik, R.H.; Stricker, B.H. Genetic variation in the PPARA gene is associated with simvastatin-mediated cholesterol reduction in the Rotterdam Study. Pharmacogenomics 2013, 14, 1295–1304. [Google Scholar] [CrossRef]
- Chen, M.; Wang, Y.; Zhang, W.; Han, X. Abstract PR428: Association of PparA Rs4253728 G> A gene polymorphisms with Cyp3A4 enzyme activity and fentanyl post-operative intravenous analgesic effect. Anesth. Analg. 2016, 123, 109–110. [Google Scholar] [CrossRef]
- Ferreira, P.; Cravo, M.; Guerreiro, C.S.; Tavares, L.; Santos, P.M.; Brito, M. Fat intake interacts with polymorphisms of Caspase9, FasLigand and PPARgamma apoptotic genes in modulating Crohn’s Disease activity. Clin. Nutr. 2010, 29, 819–823. [Google Scholar] [CrossRef]
- Jiang, Z.; Li, C.; Xu, Y.; Cai, S. A meta-analysis on XRCC1 and XRCC3 polymorphisms and colorectal cancer risk. Int. J. Colorectal Dis. 2010, 25, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Stern, M.C.; Butler, L.M.; Corral, R.; Joshi, A.D.; Yuan, J.M.; Koh, W.P.; Yu, M.C. Polyunsaturated fatty acids, DNA repair single nucleotide polymorphisms and colorectal cancer in the Singapore Chinese Health Study. J. Nutrigenet. Nutrigenomics 2009, 2, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Stryjecki, C.; Roke, K.; Clarke, S.; Nielsen, D.; Badawi, A.; El-Sohemy, A.; Ma, D.W.; Mutch, D.M. Enzymatic activity and genetic variation in SCD1 modulate the relationship between fatty acids and inflammation. Mol. Genet. Metab. 2012, 105, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Kumlin, M.; Ingelman-Sundberg, M.; Wolk, A. dietary long-chain N-3 fatty acids for the prevention of cancer: A review of potential mechanisms. Am. J. Clin. Nutr. 2004, 79, 935–945. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, M.L.; Neoptolemos, J.P.; Clayton, H.A.; Talbot, I.C.; Bell, P.R. Inhibition of experimental colorectal carcinogenesis by dietary N-6 polyunsaturated fats. Carcinogenesis 1990, 11, 2191–2197. [Google Scholar] [CrossRef]
- Bray, G.; Popkin, B.M. Calorie-sweetened beverages and fructose: What have we learned 10 years later. Pediatr. Obes. 2013, 8, 242–248. [Google Scholar] [CrossRef]
- Elliott, S.S.; Keim, N.L.; Stern, J.S.; Teff, K.; Havel, P.J. Fructose, weight gain, and the insulin resistance syndrome1—3. Am. J. Clin. Nutr. 2002, 76, 911–922. [Google Scholar] [CrossRef]
- Basu, S.; Yoffe, P.; Hills, N.; Lustig, R.H. The relationship of sugar to population-level diabetes prevalence: An econometric analysis of repeated cross-sectional data. PloS ONE 2013, 8, e57873. [Google Scholar] [CrossRef]
- Goran, M.I.; Ulijaszek, S.J.; Ventura, E.E. High fructose corn syrup and diabetes prevalence: A global perspective. Glob. Public Health 2013, 8, 55–64. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J.H.; Lucan, S.C. Added fructose: A principal driver of type 2 diabetes mellitus and its consequences. Mayo Clin. Proc. 2015, 90, 372–381. [Google Scholar] [CrossRef]
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, S.J.; Gibson, P.R. Fructose malabsorption and symptoms of irritable bowel syndrome: Guidelines for effective dietary management. J. Am. Diet. Assoc. 2006, 106, 1631–1639. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.; Shepherd, S. Personal view: Food for thought–western lifestyle and susceptibility to Crohn’s Disease. the FODMAP hypothesis. Aliment. Pharmacol. Ther. 2005, 21, 1399–1409. [Google Scholar] [CrossRef] [PubMed]
- Rumessen, J.J. Fructose and related food carbohydrates: Sources, intake, absorption, and clinical implications. Scand. J. Gastroenterol. 1992, 27, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, S.; Choi, H.K.; Lustig, R.H.; Hsu, C. Sugar-sweetened beverages, serum uric acid, and blood pressure in adolescents. J. Pediatr. 2009, 154, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Rippe, J.M.; Angelopoulos, T.J. Fructose-containing sugars and cardiovascular disease. Adv. Nutr. 2015, 6, 430–439. [Google Scholar] [CrossRef] [PubMed]
- DiNicolantonio, J.J.; Berger, A. Added sugars drive nutrient and energy deficit in obesity: A new paradigm. Open Heart 2016, 3, e000469. [Google Scholar] [CrossRef] [PubMed]
- Brinton, E.A. The time has come to flag and reduce excess fructose intake. Atherosclerosis 2016, 253, 262–264. [Google Scholar] [CrossRef] [PubMed]
- Schroeder, V.A.; Mattioli, L.F.; Kilkenny, T.A.; Belmont, J.M. Effects of lactose-containing vs lactose-free infant formula on postprandial superior mesenteric artery flow in term infants. JPEN J. Parenter. Enteral Nutr. 2014, 38, 236–242. [Google Scholar] [CrossRef] [PubMed]
- USDA ERS. Table High Fructose Corn Syrup: Estimated Number of Per Capita Calories Consumed Daily by Calendar Year; USDA ERS: Washington, DC, USA, 2016.
- Russell, D.; Parnell, W.; Wilson, N.; Faed, J.; Ferguson, E.; Herbison, P.; Horwath, C.; Nye, T.; Reid, P.; Walker, R. NZ Food: NZ People. Key Results of the 1997 National Nutrition Survey; Ministry of Health: Wellington, New Zealand, 1999; p. 71.
- Spencer, R.; Gearry, R.; Pearson, J.; Skidmore, P. Relationship between fructose and lactose intakes and functional gastrointestinal symptoms in a sample of 50-year-old cantabrians in New Zealand. NZ Med. J. 2014, 127, 39. [Google Scholar]
- Gould, G.W.; Thomas, H.M.; Jess, T.J.; Bell, G.I. Expression of human glucose transporters in xenopus oocytes: Kinetic characterization and substrate specificities of the erythrocyte, liver, and brain isoforms. Biochemistry 1991, 30, 5139–5145. [Google Scholar] [CrossRef] [PubMed]
- Burant, C.F.; Takeda, J.; Brot-Laroche, E.; Bell, G.I.; Davidson, N.O. Fructose transporter in human spermatozoa and small intestine is GLUT5. J. Biol. Chem. 1992, 267, 14523–14526. [Google Scholar] [PubMed]
- Douard, V.; Ferraris, R.P. Regulation of the Fructose Transporter GLUT5 in Health and Disease. Am. J. Physiol. Endocrinol. Metab. 2008, 295, E227–E237. [Google Scholar] [CrossRef] [PubMed]
- Berni Canani, R.; Pezzella, V.; Amoroso, A.; Cozzolino, T.; Di Scala, C.; Passariello, A. Diagnosing and treating intolerance to carbohydrates in children. Nutrients 2016, 8, 157. [Google Scholar] [CrossRef] [PubMed]
- Kolderup, A.; Svihus, B. Fructose metabolism and relation to atherosclerosis, type 2 diabetes, and obesity. J. Nutr. Metab. 2015, 2015, 823081. [Google Scholar] [CrossRef] [PubMed]
- Stanhope, K.L.; Schwarz, J.M.; Keim, N.L.; Griffen, S.C.; Bremer, A.A.; Graham, J.L.; Hatcher, B.; Cox, C.L.; Dyachenko, A.; Zhang, W.; et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J. Clin. Invest. 2009, 119, 1322–1334. [Google Scholar] [CrossRef] [Green Version]
- Dotimas, J.R.; Lee, A.W.; Schmider, A.B.; Carroll, S.H.; Shah, A.; Bilen, J.; Elliott, K.R.; Myers, R.B.; Soberman, R.J.; Yoshioka, J. Diabetes Regulates Fructose Absorption through Thioredoxin-Interacting Protein. eLife 2016, 5, e18313. [Google Scholar] [CrossRef]
- Wang, X.Q.; Nigro, P.; World, C.; Fujiwara, K.; Yan, C.; Berk, B.C. Thioredoxin Interacting Protein Promotes Endothelial Cell Inflammation in Response to Disturbed Flow by Increasing Leukocyte Adhesion and Repressing Kruppel-Like Factor. Circ. Res. 2012, 110, 560–568. [Google Scholar] [CrossRef]
- Liu, Y.; Lian, K.; Zhang, L.; Wang, R.; Yi, F.; Gao, C.; Xin, C.; Zhu, D.; Li, Y.; Yan, W. TXNIP Mediates NLRP3 Inflammasome Activation in Cardiac Microvascular Endothelial Cells as a Novel Mechanism in Myocardial Ischemia/Reperfusion Injury. Basic Res. Cardiol. 2014, 109, 1–14. [Google Scholar] [CrossRef]
- Park, M.; Kim, D.; Lim, S.; Choi, J.; Kim, J.; Yoon, K.; Lee, J.; Lee, J.; Han, H.; Choi, I. Thioredoxin-Interacting Protein Mediates Hepatic Lipogenesis and Inflammation Via PRMT1 and PGC-1α Regulation in Vitro and in Vivo. J. Hepatol. 2014, 61, 1151–1157. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, J.; Chen, X.; Hu, Q.; Wang, M.; Jin, R.; Zhang, Q.; Wang, W.; Wang, R.; Kang, L. Reactive Oxygen Species-Induced TXNIP Drives Fructose-Mediated Hepatic Inflammation and Lipid Accumulation through NLRP3 Inflammasome Activation. Antioxid. Redox Signal 2015, 22, 848–870. [Google Scholar] [CrossRef] [PubMed]
- Kelleher, Z.T.; Sha, Y.; Foster, M.W.; Foster, W.M.; Forrester, M.T.; Marshall, H.E. Thioredoxin-Mediated Denitrosylation Regulates Cytokine-Induced Nuclear Factor kappaB (NF-kappaB) Activation. J. Biol. Chem. 2014, 289, 3066–3072. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Ishii, Y.; Murata, A.; Nagata, T.; Asai, S. Localization of Thioredoxin-Interacting Protein (TXNIP) mRNA in Epithelium of Human Gastrointestinal Tract. J. Histochem. Cytochem. 2003, 51, 973–976. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Masuda, H.; Ishii, Y.; Nishida, Y.; Kobayashi, M.; Asai, S. Decreased Expression of Thioredoxin Interacting Protein mRNA in Inflamed Colonic Mucosa in Patients with Ulcerative Colitis. Oncol. Rep. 2007, 18, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Billiet, L.; Furman, C.; Cuaz-Pérolin, C.; Paumelle, R.; Raymondjean, M.; Simmet, T.; Rouis, M. Thioredoxin-1 and its Natural Inhibitor, Vitamin D 3 Up-Regulated Protein 1, are Differentially Regulated by PPARα in Human Macrophages. J. Mol. Biol. 2008, 384, 564–576. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.W.; JEON, J.; YOON, S.; Choi, I. Vitamin D3 Upregulated Protein 1 (VDUP1) is a Regulator for Redox Signaling and Stress-mediated Diseases. J. Dermatol. 2006, 33, 662–669. [Google Scholar] [CrossRef]
- Fedewa, A.; Rao, S.S. Dietary Fructose Intolerance, Fructan Intolerance and FODMAPs. Curr. Gastroenterol. Rep. 2014, 16, 1–8. [Google Scholar] [CrossRef]
- Choi, Y.K.; Johlin, F.C.; Summers, R.W.; Jackson, M.; Rao, S.S. Fructose Intolerance: An Under-Recognized Problem. Am. J. Gastroenterol. 2003, 98, 1348–1353. [Google Scholar] [CrossRef]
- Choi, Y.K.; Kraft, N.; Zimmerman, B.; Jackson, M.; Rao, S.S. Fructose Intolerance in IBS and Utility of Fructose-Restricted Diet. J. Clin. Gastroenterol. 2008, 42, 233–238. [Google Scholar] [CrossRef]
- Buzas, G.M. Fructose and Fructose Intolerance. Orv. Hetil. 2016, 157, 1708–1716. [Google Scholar]
- Rao, S.S.; Attaluri, A.; Anderson, L.; Stumbo, P. Ability of the Normal Human Small Intestine to Absorb Fructose: Evaluation by Breath Testing. Clin. Gastroenterol. Hepatol. 2007, 5, 959–963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, C.K.; Tuck, C.J.; Barrett, J.S.; Canale, K.E.; Philpott, H.L.; Gibson, P.R. Poor Reproducibility of Breath Hydrogen Testing: Implications for its Application in Functional Bowel Disorders. United Eur. Gastroenterol. J. 2017, 5, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Rezaie, A.; Buresi, M.; Lembo, A.; Lin, H.; McCallum, R.; Rao, S.; Schmulson, M.; Valdovinos, M.; Zakko, S.; Pimentel, M. Hydrogen and Methane-Based Breath Testing in Gastrointestinal Disorders: The North American Consensus. Am. J. Gastroenterol. 2017, 112, 775. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.; Han, D.Y.; Triggs, C.M.; Fraser, A.G.; Ferguson, L.R. Brassicaceae: Nutrient Analysis and Investigation of Tolerability in People with Crohn’s Disease in a New Zealand Study. Funct. Foods Health Dis. 2012, 2, 460–486. [Google Scholar] [CrossRef]
- Laughlin, M. Normal Roles for Dietary Fructose in Carbohydrate Metabolism. Nutrients 2014, 6, 3117–3129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neu, J.; Rushing, J. Cesarean Versus Vaginal Delivery: Long-Term Infant Outcomes and the Hygiene Hypothesis. Clin. Perinatol. 2011, 38, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Dominguez-Bello, M.G.; Costello, E.K.; Contreras, M.; Magris, M.; Hidalgo, G.; Fierer, N.; Knight, R. Delivery Mode Shapes the Acquisition and Structure of the Initial Microbiota Across Multiple Body Habitats in Newborns. Proc. Natl. Acad. Sci. USA 2010, 107, 11971–11975. [Google Scholar] [CrossRef]
- Stinson, L.F.; Payne, M.S.; Keelan, J.A. A Critical Review of the Bacterial Baptism Hypothesis and the Impact of Caesarean Delivery on the Infant Microbiome. Front. Med. 2018, 5, 135. [Google Scholar] [CrossRef]
- Donovan, S.M.; Wang, M.; Li, M.; Friedberg, I.; Schwartz, S.L.; Chapkin, R.S. Host-Microbe Interactions in the Neonatal Intestine: Role of Human Milk Oligosaccharides. Adv. Nutr. 2012, 3, 450S–455S. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Tao, N.; German, J.B.; Grimm, R.; Lebrilla, C.B. Development of an Annotated Library of Neutral Human Milk Oligosaccharides. J. Proteome Res. 2010, 9, 4138–4151. [Google Scholar] [CrossRef] [Green Version]
- Lönnerdal, B. Bioactive Proteins in Breast Milk. J. Paediatr. Child Health 2013, 49, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Andreas, N.J.; Kampmann, B.; Le-Doare, K.M. Human Breast Milk: A Review on its Composition and Bioactivity. Early Hum. Dev. 2015, 91, 629–635. [Google Scholar] [CrossRef]
- Abou-Donia, M.B.; El-Masry, E.M.; Abdel-Rahman, A.A.; McLendon, R.E.; Schiffman, S.S. Splenda Alters Gut Microflora and Increases Intestinal P-Glycoprotein and Cytochrome P-450 in Male Rats. J. Toxicol. Environ. Health A 2008, 71, 1415–1429. [Google Scholar] [CrossRef] [PubMed]
- Mattes, R.D.; Popkin, B.M. Nonnutritive Sweetener Consumption in Humans: Effects on Appetite and Food Intake and their Putative Mechanisms. Am. J. Clin. Nutr. 2009, 89, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sylvetsky, A.; Rother, K.I.; Brown, R. Artificial Sweetener use among Children: Epidemiology, Recommendations, Metabolic Outcomes, and Future Directions. Pediatr. Clin. North Am. 2011, 58, 1467–1480. [Google Scholar] [CrossRef]
- Sylvetsky, A.C.; Welsh, J.A.; Brown, R.J.; Vos, M.B. Low-Calorie Sweetener Consumption is Increasing in the United States. Am. J. Clin. Nutr. 2012, 96, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, R.G.; Muir, E.T.; Cook, D.L.; Nutting, E.F. The Biological Properties of Aspartame. II. Actions Involving the Gastrointestinal System. J. Environ. Pathol. Toxicol. 1980, 3, 355–362. [Google Scholar] [PubMed]
- Spencer, M.; Gupta, A.; Dam, L.V.; Shannon, C.; Menees, S.; Chey, W.D. Artificial Sweeteners: A Systematic Review and Primer for Gastroenterologists. J. Neurogastroenterol. Motil. 2016, 22, 168–180. [Google Scholar] [CrossRef] [Green Version]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A. Artificial Sweeteners Induce Glucose Intolerance by Altering the Gut Microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef]
- Prashant, G.; Patil, R.B.; Nagaraj, T.; Patel, V.B. The Antimicrobial Activity of the Three Commercially Available Intense Sweeteners Against Common Periodontal Pathogens: An in Vitro Study. J. Contemp. Dent. Pract. 2012, 13, 749–752. [Google Scholar] [CrossRef]
- Brusick, D.; Borzelleca, J.F.; Gallo, M.; Williams, G.; Kille, J.; Hayes, A.W.; Pi-Sunyer, F.X.; Williams, C.; Burks, W. Expert Panel Report on a Study of Splenda in Male Rats. Regul. Toxicol. Pharmacol. 2009, 55, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, S.S. Rationale for further Medical and Health Research on High-Potency Sweeteners. Chem. Senses 2012, 37, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Suez, J.; Korem, T.; Zilberman-Schapira, G.; Segal, E.; Elinav, E. Non-Caloric Artificial Sweeteners and the Microbiome: Findings and Challenges. Gut Microbes 2015, 6, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Bian, X.; Chi, L.; Gao, B.; Tu, P.; Ru, H.; Lu, K. The Artificial Sweetener Acesulfame Potassium Affects the Gut Microbiome and Body Weight Gain in CD-1 Mice. PLoS ONE 2017, 12, e0178426. [Google Scholar] [CrossRef] [PubMed]
- Chassaing, B.; Koren, O.; Goodrich, J.K.; Poole, A.C.; Srinivasan, S.; Ley, R.E.; Gewirtz, A.T. Dietary Emulsifiers Impact the Mouse Gut Microbiota Promoting Colitis and Metabolic Syndrome. Nature 2015, 519, 92. [Google Scholar] [CrossRef]
- Zinöcker, M.; Lindseth, I. The Western Diet–microbiome-Host Interaction and its Role in Metabolic Disease. Nutrients 2018, 10, 365. [Google Scholar] [CrossRef] [PubMed]
- Wright, G.D. The Antibiotic Resistome: The Nexus of Chemical and Genetic Diversity. Nat. Rev. Microbiol. 2007, 5, 175–186. [Google Scholar] [CrossRef]
- United States Food and Drug Administration. Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals; United States Food and Drug Administration: Silver Spring, MD, USA, 2009.
- Kedgley, S. Parliament, press release. Scoop Independent News, 11 April 2011. [Google Scholar]
- Ministry for Primary Industries NZ. Antbiotic Resistance and Food; Ministry for Primary Industries NZ: Wellington, New Zealand, 2013.
- Ruiz-Garbajosa, P.; Bonten, M.J.; Robinson, D.A.; Top, J.; Nallapareddy, S.R.; Torres, C.; Coque, T.M.; Cantón, R.; Baquero, F.; Murray, B.E. Multilocus Sequence Typing Scheme for Enterococcus Faecalis Reveals Hospital-Adapted Genetic Complexes in a Background of High Rates of Recombination. J. Clin. Microbiol. 2006, 44, 2220–2228. [Google Scholar] [CrossRef]
- Pray, L.; Pillsbury, L.; Tomayko, E. The Human Microbiome, Diet and Health Workshop Summary; The National Academies Press: Washington, DC, USA, 2012; pp. 5–7. [Google Scholar]
- Silbergeld, E.K.; Graham, J.; Price, L.B. Industrial Food Animal Production, Antimicrobial Resistance, and Human Health. Annu. Rev. Public Health 2008, 29, 151–169. [Google Scholar] [CrossRef]
- Lindsey, R.L.; Frye, J.G.; Thitaram, S.N.; Meinersmann, R.J.; Fedorka-Cray, P.J.; Englen, M.D. Characterization of Multidrug-Resistant Escherichia Coli by Antimicrobial Resistance Profiles, Plasmid Replicon Typing, and Pulsed-Field Gel Electrophoresis. Microb. Drug Resist. 2011, 17, 157–163. [Google Scholar] [CrossRef]
- Knight, P.; Campbell, B.J.; Rhodes, J.M. Host-Bacteria Interaction in Inflammatory Bowel Disease. Br. Med. Bull. 2008, 88, 95–113. [Google Scholar] [CrossRef] [PubMed]
- Martin, H.M.; Campbell, B.J.; Hart, C.A.; Mpofu, C.; Nayar, M.; Singh, R.; Englyst, H.; Williams, H.F.; Rhodes, J.M. Enhanced Escherichia Coli Adherence and Invasion in Crohn’s Disease and Colon Cancer. Gastroenterology 2004, 127, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Darfeuille-Michaud, A.; Boudeau, J.; Bulois, P.; Neut, C.; Glasser, A.; Barnich, N.; Bringer, M.; Swidsinski, A.; Beaugerie, L.; Colombel, J. High Prevalence of Adherent-Invasive Escherichia Coli Associated with Ileal Mucosa in Crohn’s Disease. Gastroenterology 2004, 127, 412–421. [Google Scholar] [CrossRef] [PubMed]
- Gearry, R.B.; Irving, P.M.; Barrett, J.S.; Nathan, D.M.; Shepherd, S.J.; Gibson, P.R. Reduction of Dietary Poorly Absorbed Short-Chain Carbohydrates (FODMAPs) Improves Abdominal Symptoms in Patients with Inflammatory Bowel Disease—A Pilot Study. J. Crohns Colitis 2009, 3, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Barbalho, S.M.; Goulart, R.d.A. Aranão, Ana Luíza de Carvalho; de Oliveira, Pamela Grazielle Correa. Inflammatory Bowel Diseases and Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols: An Overview. J. Med. Food 2018, 21, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.A.; Smith, T.; Trebble, T.M. Nutritional Management of Adults with Inflammatory Bowel Disease: Practical Lessons from the Available Evidence. Frontline Gastroenterol. 2012, 3, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Hill, P.; Muir, J.G.; Gibson, P.R. Controversies and Recent Developments of the Low-FODMAP Diet. Gastroenterol. Hepatol. 2017, 13, 36–45. [Google Scholar]
- Sloan, T.J.; Jalanka, J.; Major, G.A.; Krishnasamy, S.; Pritchard, S.; Abdelrazig, S.; Korpela, K.; Singh, G.; Mulvenna, C.; Hoad, C.L. A Low FODMAP Diet is Associated with Changes in the Microbiota and Reduction in Breath Hydrogen but Not Colonic Volume in Healthy Subjects. PloS ONE 2018, 13, e0201410. [Google Scholar] [CrossRef]
- Mital, B.; Steinkraus, K. Utilization of Oligosaccharides by Lactic Acid Bacteria during Fermentation of Soy Milk. J. Food Sci. 1975, 40, 114–118. [Google Scholar] [CrossRef]
- Naessens, M.; Cerdobbel, A.; Soetaert, W.; Vandamme, E.J. Leuconostoc Dextransucrase and Dextran: Production, Properties and Applications. J. Chem. Technol. Biotechnol. 2005, 80, 845–860. [Google Scholar] [CrossRef]
- Van den Ende, W. Multifunctional Fructans and Raffinose Family Oligosaccharides. Front. Plant Sci. 2013, 4, 247. [Google Scholar] [PubMed]
- Kuo, T.M.; VanMiddlesworth, J.F.; Wolf, W.J. Content of Raffinose Oligosaccharides and Sucrose in various Plant Seeds. J. Agric. Food Chem. 1988, 36, 32–36. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, L. Structures and Properties of Commercial Maltodextrins from Corn, Potato, and Rice Starches. Starch-Stärke 2000, 52, 296–304. [Google Scholar] [CrossRef]
- Plaza-Díaz, J.; Martinez Augustin, O.; Gil Hernández, A. Foods as Sources of Mono and Disaccharides: Biochemical and Metabolic Aspects. Nutr. Hosp. 2013, 28, 5–16. [Google Scholar] [PubMed]
- Calorie Control Council. Polyols. 2018. Available online: https://caloriecontrol.org/category/polyols/ (accessed on 5 November 2018).
- Ingram, C.J.; Mulcare, C.A.; Itan, Y.; Thomas, M.G.; Swallow, D.M. Lactose Digestion and the Evolutionary Genetics of Lactase Persistence. Hum. Genet. 2009, 124, 579–591. [Google Scholar] [CrossRef] [PubMed]
- Gerbault, P.; Liebert, A.; Itan, Y.; Powell, A.; Currat, M.; Burger, J.; Swallow, D.M.; Thomas, M.G. Evolution of Lactase Persistence: An Example of Human Niche Construction. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2011, 366, 863–877. [Google Scholar] [CrossRef] [PubMed]
- Brauer, H.A.; Libby, T.E.; Mitchell, B.L.; Li, L.; Chen, C.; Randolph, T.W.; Yasui, Y.Y.; Lampe, J.W.; Lampe, P.D. Cruciferous Vegetable Supplementation in a Controlled Diet Study Alters the Serum Peptidome in a GSTM1-Genotype Dependent Manner. Nutr. J. 2011, 10, 11. [Google Scholar] [CrossRef]
- Kristal, A.R.; Lampe, J.W. Brassica Vegetables and Prostate Cancer Risk: A Review of the Epidemiological Evidence. Nutr. Cancer 2002, 42, 1–9. [Google Scholar] [CrossRef]
- Laing, B.; Han, D.Y.; Ferguson, L.R. Candidate Genes Involved in Beneficial or Adverse Responses to Commonly Eaten Brassica Vegetables in a New Zealand Crohn’s Disease Cohort. Nutrients 2013, 5, 5046–5064. [Google Scholar] [CrossRef]
- Higdon, J.V.; Delage, B.; Williams, D.E.; Dashwood, R.H. Cruciferous Vegetables and Human Cancer Risk: Epidemiologic Evidence and Mechanistic Basis. Pharmacol. Res. 2007, 55, 224–236. [Google Scholar] [CrossRef]
- NIH. Celiac Disease. In Genetics Home Reference; NIH: Stapleton, NY, USA, 2013. [Google Scholar]
- Petermann, I.; Triggs, C.M.; Huebner, C.; Han, D.Y.; Gearry, R.B.; Barclay, M.L.; Demmers, P.S.; McCulloch, A.; Ferguson, L.R. Mushroom Intolerance: A Novel Diet-Gene Interaction in Crohn’s Disease. Br. J. Nutr. 2009, 102, 506. [Google Scholar] [CrossRef] [PubMed]
- Campbell, A.K.; Matthews, S.B.; Vassel, N.; Cox, C.D.; Naseem, R.; Chaich, i.J.; Holland, I.B.; Green, J.; Wann, K.T. Bacterial Metabolic ‘Toxins’: A New Mechanism for Lactose and Food Intolerance, and Irritable Bowel Syndrome. Toxicology 2010, 278, 268–276. [Google Scholar] [CrossRef] [PubMed]
- FAO/WHO. Carbohydrates in Human Nutrition; Report of a Joint FAO/WHO Expert Consultation; FAO Food and Nutrition Paper; FAO: Rome, Italy, 1998. [Google Scholar]
- Hyams, J.S. Sorbitol Intolerance: An Unappreciated Cause of Functional Gastrointestinal Complaints. Gastroenterology 1983, 84, 30–33. [Google Scholar] [PubMed]
- Gibson, P.R.; Shepherd, S.J. Evidence-based Dietary Management of Functional Gastrointestinal Symptoms: The FODMAP Approach. J. Gastroenterol. Hepatol. 2010, 25, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Catassi, G.; Lionetti, E.; Gatti, S.; Catassi, C. The Low FODMAP Diet: Many Question Marks for a Catchy Acronym. Nutrients 2017, 9, 292. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.S.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T. A Human Gut Microbial Gene Catalogue Established by Metagenomic Sequencing. Nature 2010, 464, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Ley, R.E.; Peterson, D.A.; Gordon, J.I. Ecological and Evolutionary Forces Shaping Microbial Diversity in the Human Intestine. Cell 2006, 124, 837–848. [Google Scholar] [CrossRef] [Green Version]
- Turnbaugh, P.J.; Ley, R.E.; Mahowald, M.A.; Magrini, V.; Mardis, E.R.; Gordon, J.I. An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest. Nature 2006, 444, 1027–1131. [Google Scholar] [CrossRef]
- Frank, D.N.; Robertson, C.E.; Hamm, C.M.; Kpadeh, Z.; Zhang, T.; Chen, H.; Zhu, W.; Sartor, R.B.; Boedeker, E.C.; Harpaz, N. Disease Phenotype and Genotype are Associated with Shifts in Intestinal-Associated Microbiota in Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2010, 17, 179–184. [Google Scholar] [CrossRef]
- Frank, D.N.; St Amand, A.L.; Feldman, R.A.; Boedeker, E.C.; Harpaz, N.; Pace, N.R. Molecular-Phylogenetic Characterization of Microbial Community Imbalances in Human Inflammatory Bowel Diseases. Proc. Natl. Acad. Sci. USA 2007, 104, 13780–13785. [Google Scholar] [CrossRef]
- Walker, A.W.; Sanderson, J.D.; Churcher, C.; Parkes, G.C.; Hudspith, B.N.; Rayment, N.; Brostoff, J.; Parkhill, J.; Dougan, G.; Petrovska, L. High-Throughput Clone Library Analysis of the Mucosa-Associated Microbiota Reveals Dysbiosis and Differences between Inflamed and Non-Inflamed Regions of the Intestine in Inflammatory Bowel Disease. BMC Microbiol. 2011, 11, 7. [Google Scholar] [CrossRef] [PubMed]
- Nagalingam, N.A.; Lynch, S.V. Role of the Microbiota in Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2012, 18, 968–984. [Google Scholar] [CrossRef] [PubMed]
- Wacklin, P.; Mäkivuokko, H.; Alakulppi, N.; Nikkilä, J.; Tenkanen, H.; Räbinä, J.; Partanen, J.; Aranko, K.; Mättö, J. Secretor Genotype (FUT2 Gene) is Strongly Associated with the Composition of Bifidobacteria in the Human Intestine. PLoS ONE 2011, 6, e20113. [Google Scholar] [CrossRef] [PubMed]
- McGovern, D.P.; Jones, M.R.; Taylor, K.D.; Marciante, K.; Yan, X.; Dubinsky, M.; Ippoliti, A.; Vasiliauskas, E.; Berel, D.; Derkowski, C. Fucosyltransferase 2 (FUT2) Non-Secretor Status is Associated with Crohn’s Disease. Hum. Mol. Genet. 2010, 19, 3468–3476. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, J.; Yajima, T.; Okamoto, S.; Matsuoka, K.; Inoue, N.; Hisamatsu, T.; Shimamura, K.; Nakazawa, A.; Kanai, T.; Ogata, H. Ectopic Expression of Blood Type Antigens in Inflamed Mucosa with Higher Incidence of FUT2 Secretor Status in Colonic Crohn’s Disease. J. Gastroenterol. 2011, 46, 1056–1063. [Google Scholar] [CrossRef]
- Rausch, P.; Rehman, A.; Künzel, S.; Häsler, R.; Ott, S.J.; Schreiber, S.; Rosenstiel, P.; Franke, A.; Baines, J.F. Colonic Mucosa-Associated Microbiota is Influenced by an Interaction of Crohn Disease and FUT2 (Secretor) Genotype. Proc. Natl. Acad. Sci. USA 2011, 108, 19030–19035. [Google Scholar] [CrossRef] [PubMed]
- Salminen, S.; Gueimonde, M. Gut Microbiota in Infants between 6 and 24 Months of Age. Nestle Nutr. Workshop Ser. Pediatr. Program. 2005, 56, 43–56. [Google Scholar]
- Ebaid, H.; Hassanein, K.A. Comparative Immunomudulating Effects of Five Orally Administrated Bifidobacteria Species in Male Albino Rats. Egypt. J. Biol. 2007, 9, 14–23. [Google Scholar]
- Festen, E.A.; Goyette, P.; Green, T.; Boucher, G.; Beauchamp, C.; Trynka, G.; Dubois, P.C.; Lagacé, C.; Stokkers, P.C.; Hommes, D.W. A Meta-Analysis of Genome-Wide Association Scans Identifies IL18RAP, PTPN2, TAGAP, and PUS10 as Shared Risk Loci for Crohn’s Disease and Celiac Disease. PLoS Genet. 2011, 7, e1001283. [Google Scholar] [CrossRef]
- Visser, R.; Barrett, K.; McCole, D. Regulation of Epithelial Barrier Function by Crohn’s Disease Associated Gene PTPN. BMC Proc. 2012, 6, O41. [Google Scholar] [CrossRef]
- Armstrong, D.; Don-Wauchope, A.C.; Verdu, E.F. Testing for Gluten-Related Disorders in Clinical Practice: The Role of Serology in Managing the Spectrum of Gluten Sensitivity. Can. J. Gastroenterol. 2011, 25, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Mishkin, S. Controversies regarding the Role of Dairy-Products in Inflammatory Bowel Disease. Can. J. Gastroenterol. 1994, 8, 205–212. [Google Scholar] [CrossRef]
- Truelove, S.C. Ulcerative Colitis Provoked by Milk. Br. Med. J. 1961, 1, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Wright, R.; Truelove, S.C. A Controlled Therapeutic Trial of various Diets in Ulcerative Colitis. Br. Med. J. 1965, 2, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Mishkin, S. Dairy Sensitivity, Lactose Malabsorption, and Elimination Diets in Inflammatory Bowel Disease. Am. J. Clin. Nutr. 1997, 65, 564–567. [Google Scholar] [CrossRef]
- Maconi, G.; Ardizzone, S.; Cucino, C.; Bezzio, C.; Russo, A.G.; Bianchi Porro, G. Pre-Illness Changes in Dietary Habits and Diet as a Risk Factor for Inflammatory Bowel Disease: A Case-Control Study. World J. Gastroenterol. 2010, 16, 4297–4304. [Google Scholar] [CrossRef] [PubMed]
- Nolan-Clark, D.; Tapsell, L.C.; Hu, R.; Han, D.Y.; Ferguson, L.R. Effects of Dairy Products on Crohn’s Disease Symptoms are Influenced by Fat Content and Disease Location but Not Lactose Content or Disease Activity Status in a New Zealand Population. J. Am. Diet. Assoc. 2011, 111, 1165–1172. [Google Scholar] [CrossRef]
- Nolan, D.; Han, D.; Lam, W.; Morgan, A.; Fraser, A.; Tapsell, L.; Ferguson, L. Genetic Adult Lactase Persistence is Associated with Risk of Crohn’s Disease in a New Zealand Population. BMC Res. Notes 2010, 3, 339. [Google Scholar] [CrossRef]
- Shrier, I.; Szilagyi, A.; Correa, J.A. Impact of Lactose Containing Foods and the Genetics of Lactase on Diseases: An Analytical Review of Population Data. Nutr. Cancer 2008, 60, 292–300. [Google Scholar] [CrossRef]
- Barbado, M.; Fablet, K.; Ronjat, M.; De Waard, M. Gene Regulation by Voltage-Dependent Calcium Channels. Biochim. Biophys. Acta 2009, 1793, 1096–1104. [Google Scholar] [CrossRef]
- Bernstein, C.N.; Leslie, W.D.; Leboff, M.S. AGA Technical Review on Osteoporosis in Gastrointestinal Diseases. Gastroenterology 2003, 124, 795–841. [Google Scholar] [CrossRef] [PubMed]
- Caniggia, A.; Nuti, R.; Lore, F.; Vattimo, A. Pathophysiology of the Adverse Effects of Glucoactive Corticosteroids on Calcium Metabolism in Man. J. Steroid Biochem. 1981, 15, 153–161. [Google Scholar] [CrossRef]
- New Zealand Nutrition Foundation. Calcium. 2018. Available online: https://nutritionfoundation.org.nz/nutrients-vitamins-and-minerals/calcium (accessed on 15 June 2019).
- Burlingame, B.A.; Milligan, G.; Apimerika, D.; Arthur, J. The Concise New Zealand Food Composition Tables; New Zealand Institute for Crop & Food Research: Auckland, New Zealand, 2009. [Google Scholar]
- Duke, J.; Beckstrom-Sternberg, S. Phytochemical Database USDA-ARS-NGRL; Beltsbille Agricultural Research Center: Beltsbille, MD, USA, 1998.
- Parl, F.F. Glutathione S-Transferase Genotypes and Cancer Risk. Cancer Lett. 2005, 221, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Beckett, G.J.; Hayes, J.D. Glutathione S-Transferases: Biomedical Applications. Adv. Clin. Chem. 1993, 30, 282. [Google Scholar]
- Wilce, M.C.; Parker, M.W. Structure and Function of Glutathione S-Transferases. Biochim. Biophys. Acta 1994, 1205, 1–18. [Google Scholar] [CrossRef]
- Webb, G.; Vaska, V.; Coggan, M.; Board, P. Chromosomal Localization of the Gene for the Human Theta Class Glutathione Transferase (GSTT1). Genomics 1996, 33, 121–123. [Google Scholar] [CrossRef]
- Sheehan, D.; Meade, G.; Foley, V.; Dowd, C. Structure, Function and Evolution of Glutathione Transferases: Implications for Classification of Non-Mammalian Members of an Ancient Enzyme Superfamily. Biochem. J. 2001, 360, 1–16. [Google Scholar] [CrossRef]
- Hayes, J.D.; Strange, R.C. Glutathione S-Transferase Polymorphisms and their Biological Consequences. Pharmacology 2000, 61, 154–166. [Google Scholar] [CrossRef]
- Inskip, A.; Elexperu-Camiruaga, J.; Buxton, N.; Dias, P.; MacIntosh, J.; Campbell, D.; Jones, P.; Yengi, L.; Talbot, J.; Strange, R. Identification of Polymorphism at the Glutathione S-Transferase, GSTM3 Locus: Evidence for Linkage with GSTM1* A. Biochem. J. 1995, 312, 713. [Google Scholar] [CrossRef]
- Seow, A.; Yuan, J.; Sun, C.; Van Den Berg, D.; Lee, H.; Mimi, C.Y. Dietary Isothiocyanates, Glutathione S-Transferase Polymorphisms and Colorectal Cancer Risk in the Singapore Chinese Health Study. Carcinogenesis 2002, 23, 2055–2061. [Google Scholar] [CrossRef]
- Steck, S.E.; Hebert, J.R. GST Polymorphism and Excretion of Heterocyclic Aromatic Amine and Isothiocyanate Metabolites After Brassica Consumption. Environ. Mol. Mutagen. 2009, 50, 238–246. [Google Scholar] [CrossRef]
- Campbell, B.; Han, D.; Jiun, W.; Morgan, A.; Triggs, C.; Fraser, A.C.; Ferguson, L.R. Deletion of the GSTT1 Genotype Linked to Tolerance of Brassicaceae in People with Crohn’s Disease in a New Zealand Cohort. In Proceedings of the Annual Scientific Meeting of the Nutrition Society of New Zealand Auckland, Auckland, New Zealand, 21–22 November 2012. [Google Scholar]
- Gentschew, L.; Bishop, K.S.; Han, D.Y.; Morgan, A.R.; Fraser, A.G.; Lam, W.J.; Karunasinghe, N.; Campbell, B.; Ferguson, L.R. Selenium, Selenoprotein Genes and Crohn’s Disease in a Case-Control Population from Auckland, New Zealand. Nutrients 2012, 4, 1247–1259. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, T.; Marshall, S.E.; Jewell, D. Genetics of Inflammatory Bowel Disease: The Role of the HLA Complex. World J. Gastroenterol. 2006, 12, 3628. [Google Scholar] [CrossRef] [PubMed]
- Lees, C.W.; Satsangi, J. Genetics of Inflammatory Bowel Disease: Implications for Disease Pathogenesis and Natural History. Expert Rev. Gastroenterol. Hepatol. 2009, 3, 513–534. [Google Scholar] [CrossRef] [PubMed]
- Annese, V.; Piepoli, A.; Latiano, A.; Lombardi, G.; Napolitano, G.; Caruso, N.; Cocchiara, E.; Accadia, L.; Perri, F.; Andriulli, A. HLA-DRB1 Alleles may Influence Disease Phenotype in Patients with Inflammatory Bowel Disease: A Critical Reappraisal with Review of the Literature. Dis. Colon. Rectum. 2005, 48, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Moffatt, M.F.; Gut, I.G.; Demenais, F.; Strachan, D.P.; Bouzigon, E.; Heath, S.; Von Mutius, E.; Farrall, M.; Lathrop, M.; Cookson, W.O. A Large-Scale, Consortium-Based Genomewide Association Study of Asthma. N. Engl. J. Med. 2010, 363, 1211–1221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levin, A.; Mathias, R.; Huang, L.R.; Roth, L.A.; Daley, D.; Myers, R.A.; Himes, B.E.; Romieu, I.; Yang, M.; Eng, C.; et al. A Meta-Analysis of Genome Wide Association Studies for Serum Total IgE in Diverse Populations Groups; American Academy of Allergy, Asthma and Immunology: Milwaukee, WI, USA, 2013; p. 1176. [Google Scholar]
- Gould, H.J.; Sutton, B.J.; Beavil, A.J.; Beavil, R.L.; McCloskey, N.; Coker, H.A.; Fear, D.; Smurthwaite, L. The Biology of IgE and the Basis of Allergic Disease. Annu. Rev. Immunol. 2003, 21, 579–628. [Google Scholar] [CrossRef]
- Marlow, G.; Han, D.Y.; Triggs, C.M.; Ferguson, L.R. Food Intolerance: Associations with the rs12212067 Polymorphism of FOXO3 in Crohn’s Disease Patients in New Zealand. J. Nutrigen. Nutrigen. 2015, 8, 70–80. [Google Scholar] [CrossRef]
- Food Safety Authority of Ireland. Food Ingredients that must be Declared as Allergens in the EU. Available online: https://www. fsai. ie/legislation/food_legislation/food_information/14_allergens.html (accessed on 2 February 2019).
- Wedzicha, B.L. Chemistry of Sulphur Dioxide in Foods; Elsevier Applied Science Publishers Ltd.: Amsterdam, The Netherlands, 1984. [Google Scholar]
- Coates, P.M.; Blackman, M.; Betz, J.; Cragg, G.M.; Levine, M.; Moss, J.; White, J.D. Encyclopedia of Dietary Supplements; Informa Healthcare: London, UK, 2010. [Google Scholar]
- Costantini, A.; Pala, M.I. Thiamine and Fatigue in Inflammatory Bowel Diseases: An Open-Label Pilot Study. J. Altern. Complement. Med. 2013, 19, 704–708. [Google Scholar] [CrossRef]
- Magee, E.A.; Edmond, L.M.; Tasker, S.M.; Kong, S.C.; Curno, R.; Cummings, J.H. Associations between Diet and Disease Activity in Ulcerative Colitis Patients using a Novel Method of Data Analysis. Nutr. J. 2005, 4, 7. [Google Scholar] [CrossRef]
- Pitcher, M.C.; Cummings, J.H. Hydrogen Sulphide: A Bacterial Toxin in Ulcerative Colitis? Gut 1996, 39, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Marcus, R.; Watt, J. Seaweeds and Ulcerative Colitis in Laboratory Animals. Lancet 1969, 2, 489–490. [Google Scholar] [CrossRef]
- Marcus, R.; Watt, J. Ulcerative Disease of the Colon in Laboratory Animals Induced by Pepsin Inhibitors. Gastroenterology 1974, 67, 473–483. [Google Scholar] [CrossRef]
- Roediger, W. The Colonic Epithelium in Ulcerative Colitis: An Energy-Deficiency Disease? Lancet 1980, 316, 712–715. [Google Scholar] [CrossRef]
- Peng, L.; Li, Z.; Green, R.S.; Holzman, I.R.; Lin, J. Butyrate Enhances the Intestinal Barrier by Facilitating Tight Junction Assembly Via Activation of AMP-Activated Protein Kinase in Caco-2 Cell Monolayers. J. Nutr. 2009, 139, 1619–1625. [Google Scholar] [CrossRef] [PubMed]
- Carbonero, F.; Benefiel, A.C.; Alizadeh-Ghamsari, A.H.; Gaskins, H.R. Microbial Pathways in Colonic Sulfur Metabolism and Links with Health and Disease. Front. Physiol. 2012, 3, 448. [Google Scholar] [CrossRef] [PubMed]
- Berezowska, A.; Fischer, A.R.; Ronteltap, A.; Lans, I.A.; Trijp, H.C. Consumer Adoption of Personalised Nutrition Services from the Perspective of a Risk–benefit Trade-Off. Genes Nutr. 2015, 10, 42. [Google Scholar] [CrossRef]
- Nutrisearch. Fitgenes (DNA Testing). 2018. Available online: https://www.nutrisearch.co.nz/lab-diagnostics/fitgenes-dna-testing/ (accessed on 13 June 2018).
- Zettler, P.J.; Sherkow, J.S.; Greely, H.T. 23 and Me, the Food and Drug Administration, and the Future of Genetic Testing. JAMA Intern. Med. 2014, 174, 493–494. [Google Scholar] [CrossRef]
- Annas, G.J.; Elias, S. 23andMe and the FDA. N. Engl. J. Med. 2014, 370, 985–988. [Google Scholar] [CrossRef]
| Reference | Vagianos et al. [9] | Stein and Bott [10] | Hartman et al. [15] |
|---|---|---|---|
| Outpatient | Inpatient | Outpatient | |
| Year of Investigation | 2007 | 2008 | 2016 |
| Number of Participants | 71 | na | 68 |
| Gender (Male, Female) | 32, 52 | na | na |
| Age (years) | 37.6 ± 14.3 | Adult | 13.9 ± 3.2 |
| Country | Canada | Germany | Israel |
| Dietary Measurement | FFQ, 4-day records, Anthropometric | na | 3-day records, Anthropometric |
| Laboratory Measurement | Biomarkers for nutrients (CD) | na | Biomarkers for nutrients |
| Dietary Deficiency | |||
| Measures | % <66% RFI | % Inadequate Intake | % <80% of RDA |
| Vitamin B6 | 4.2 | na | 10 |
| Vitamin B12 | 5.6 | 48 | 12 |
| Folate | 20 | 56–62 | 34 |
| Vitamin C | 9.9 | na | 31 |
| Vitamin A | 30 | 11–50 | 57 |
| Vitamin D | 38 | 23–75 | 25 |
| Vitamin E | 59 | na | 65 |
| Calcium | 25 | 13 | 79 |
| Iron | 14 | 25–50 | 22 |
| Magnesium | na | 14–33 | 69 |
| Zinc | 8.5 | 40 | 28 |
| Water Soluble Vitamins | Fat-Soluble Vitamins | Minerals |
|---|---|---|
| Vitamin B2 (riboflavin) | A | Calcium |
| Vitamin B3 (niacin) | D | Fluoride |
| Vitamin B6 family | E | Zinc |
| Vitamin B12 (cobalamin) | Iron | |
| Folic acid (folate) | ||
| Vitamin C (ascorbic acid) |
| Western Diet Food Factors | Effects Related to IBD | Associated Genes |
|---|---|---|
| Foods low in resistant starch and soluble dietary fibre [47] | FFAR2 (The interaction of SCFAs and FFAR2 greatly affects inflammatory processes) [21,70] | |
| Increased consumption of saturated fatty acids with decreased consumption of LC-PUFAs from the increased intake of soy, safflower, corn and sunflower oils and reduced consumption of fish [83,92,93] | FADS1 and FADS2 PPARA, PPARG XRCC1, SCD1 [94,95,96,97,98,99,100,101,102,103,104] | |
| Increased fructose consumption [25,119,120] | TXNIP [128] (associated with promoting inflammation in endothelial cells, mediating hepatic inflammation, and regulating NF-κB) [129,130,131,132,133] | |
| Increased use of infant formula, artificial sweeteners, food emulsifiers and antibiotics [167,168] |
| Genes in the microbiome [168] |
| FODMAPs | Examples of Food Sources | Examples of Associated Genes |
|---|---|---|
| Fructose | Honey, mangoes, watermelon, grapes, fruit juices, high-fructose corn syrup | TXNIP with fructose that is linked to intestinal symptoms of bloating, abdominal pain, diarrhoea in IBD [125,138,139,140,141] |
| Lactose | Dairy products (e.g., milk, ice-cream, yoghurt, soft cheeses) | Lactose intolerance associated with variants of the LCT gene [191,192] |
| Fermentable oligosaccharides | Brussels sprouts, broccoli, cabbage, peas, beetroot, garlic, leeks, onions, wheat or rye bread, pasta, couscous, chickpeas, lentils | GSTMl and GSTTl, and DIO1 variants, with tolerance of brassica vegetables [193,194,195,196]; HLA-DQA1 and HLA-DQB1 variants with gluten intolerance [197] |
| Polyols | Stone fruits, apples, pears, prunes, avocados, mushrooms; sweeteners: mannitol, sorbitol, xylitol, erythritol and isomalt. | OCTN1 with mushrooms [198] |
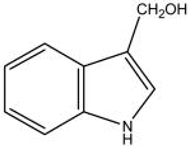
| Glucobrassicin (in bok choy) | Glucoraphanin (in broccoli) |
|---|---|
| Indole-3- | Sulforaphane |
 |  |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laing, B.B.; Lim, A.G.; Ferguson, L.R. A Personalised Dietary Approach—A Way Forward to Manage Nutrient Deficiency, Effects of the Western Diet, and Food Intolerances in Inflammatory Bowel Disease. Nutrients 2019, 11, 1532. https://doi.org/10.3390/nu11071532
Laing BB, Lim AG, Ferguson LR. A Personalised Dietary Approach—A Way Forward to Manage Nutrient Deficiency, Effects of the Western Diet, and Food Intolerances in Inflammatory Bowel Disease. Nutrients. 2019; 11(7):1532. https://doi.org/10.3390/nu11071532
Chicago/Turabian StyleLaing, Bobbi B, Anecita Gigi Lim, and Lynnette R Ferguson. 2019. "A Personalised Dietary Approach—A Way Forward to Manage Nutrient Deficiency, Effects of the Western Diet, and Food Intolerances in Inflammatory Bowel Disease" Nutrients 11, no. 7: 1532. https://doi.org/10.3390/nu11071532






