Changed Amino Acids in NAFLD and Liver Fibrosis: A Large Cross-Sectional Study without Influence of Insulin Resistance
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Transient Elastography
2.3. Serum Amino Acid Profiles
2.4. Clinical Parameters
2.5. Insulin Resistance and Diabetes
2.6. Statistical Analysis
2.7. Statement of Human Rights
2.8. Informed Consent
3. Results
3.1. Participants’ Characteristics and Amino Acid Compositions
3.2. Correlation of Serum Amino Acid Levels and HOMA-IR Index
3.3. Participants’ Characteristics and Amino Acid Compositions after Matching
3.4. Risk Factors for Liver Fibrosis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Loomba, R.; Sanyal, A.J. The global NAFLD epidemic. Nat. Rev. Gastroenterol. Hepatol. 2013, 10, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Kitade, H.; Chen, G.; Ni, Y.; Ota, T. Nonalcoholic fatty liver disease and insulin resistance: New insights and potential new treatments. Nutrients 2017, 9, 387. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Friso, S.; Choi, S.W. Epigenetic mechanisms underlying the link between non-alcoholic fatty liver diseases and nutrition. Nutrients 2014, 6, 3303–3325. [Google Scholar] [CrossRef] [PubMed]
- Newgard, C.B.; An, J.; Bain, J.R.; Muehlbauer, M.J.; Stevens, R.D.; Lien, L.F.; Haqq, A.M.; Shah, S.H.; Arlotto, M.; Slentz, C.A.; et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009, 9, 311–326. [Google Scholar] [CrossRef]
- Floegel, A.; Stefan, N.; Yu, Z.; Mühlenbruch, K.; Drogan, D.; Joost, H.G.; Fritsche, A.; Häring, H.U.; Hrabě de Angelis, M.; Peters, A.; et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes 2013, 62, 639–648. [Google Scholar] [CrossRef]
- Wiklund, P.; Zhang, X.; Pekkala, S.; Autio, R.; Kong, L.; Yang, Y.; Keinänen-Kiukaanniemi, S.; Alen, M.; Cheng, S. Insulin resistance is associated with altered amino acid metabolism and adipose tissue dysfunction in normoglycemic women. Sci. Rep. 2016, 6, 24540. [Google Scholar] [CrossRef]
- Van den Berg, E.H.; Flores-Guerrero, J.L.; Gruppen, E.G.; de Borst, M.H.; Wolak-Dinsmore, J.; Connelly, M.A.; Bakker, S.J.L.; Dullaart, R.P.F. Non-alcoholic fatty liver disease and risk of incident type 2 diabetes: Role of circulating branched-chain amino acids. Nutrients 2019, 11, 705. [Google Scholar] [CrossRef]
- Lake, A.D.; Novak, P.; Shipkova, P.; Aranibar, N.; Robertson, D.G.; Reily, M.D.; Lehman-McKeeman, L.D.; Vaillancourt, R.R.; Cherrington, N.J. Branched chain amino acid metabolism profiles in progressive human nonalcoholic fatty liver disease. Amino Acids 2015, 47, 603–615. [Google Scholar] [CrossRef]
- Mardinoglu, A.; Bjornson, E.; Zhang, C.; Klevstig, M.; Söderlund, S.; Stahlman, M.; Adiels, M.; Hakkarainen, A.; Lundbom, N.; Kilicarslan, M.; et al. Personal model-assisted identification of NAD(+) and glutathione metabolism as intervention target in NAFLD. Mol. Syst. Biol. 2017, 13, 916. [Google Scholar] [CrossRef]
- Gaggini, M.; Carli, F.; Rosso, C.; Buzzigoli, E.; Marietti, M.; Della Latta, V.; Ciociaro, D.; Abate, M.L.; Gambino, R.; Cassader, M.; et al. Altered amino acid concentrations in NAFLD: Impact of obesity and insulin resistance. Hepatology 2018, 67, 145–158. [Google Scholar] [CrossRef]
- Boursier, J.; Zarski, J.P.; de Ledinghen, V.; Rousselet, M.C.; Sturm, N.; Lebail, B.; Fouchard-Hubert, I.; Gallois, Y.; Oberti, F.; Bertrais, S.; et al. Multicentric Group from ANRS/HC/EP23 FIBROSTAR Studies. Determination of reliability criteria for liver stiffness evaluation by transient elastography. Hepatology 2013, 57, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Sasso, M.; Beaugrand, M.; de Ledinghen, V.; Douvin, C.; Marcellin, P.; Poupon, R.; Sandrin, L.; Miette, V. Controlled attenuation parameter (CAP): A novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: Preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med. Biol. 2010, 36, 1825–1835. [Google Scholar] [CrossRef] [PubMed]
- Imajo, K.; Kessoku, T.; Honda, Y.; Tomeno, W.; Ogawa, Y.; Mawatari, H.; Fujita, K.; Yoneda, M.; Taguri, M.; Hyogo, H.; et al. Magnetic resonance imaging more accurately classifies steatosis and fibrosis in patients with nonalcoholic fatty liver disease than transient elastography. Gastroenterology 2016, 150, 626–637. [Google Scholar] [CrossRef] [PubMed]
- Terrlink, T.; van Leeuwen, P.A.; Houdijk, A. Plasma amino acids determined by liquid chromatography within 17 minutes. Clin. Chem. 1994, 40, 245–249. [Google Scholar] [CrossRef]
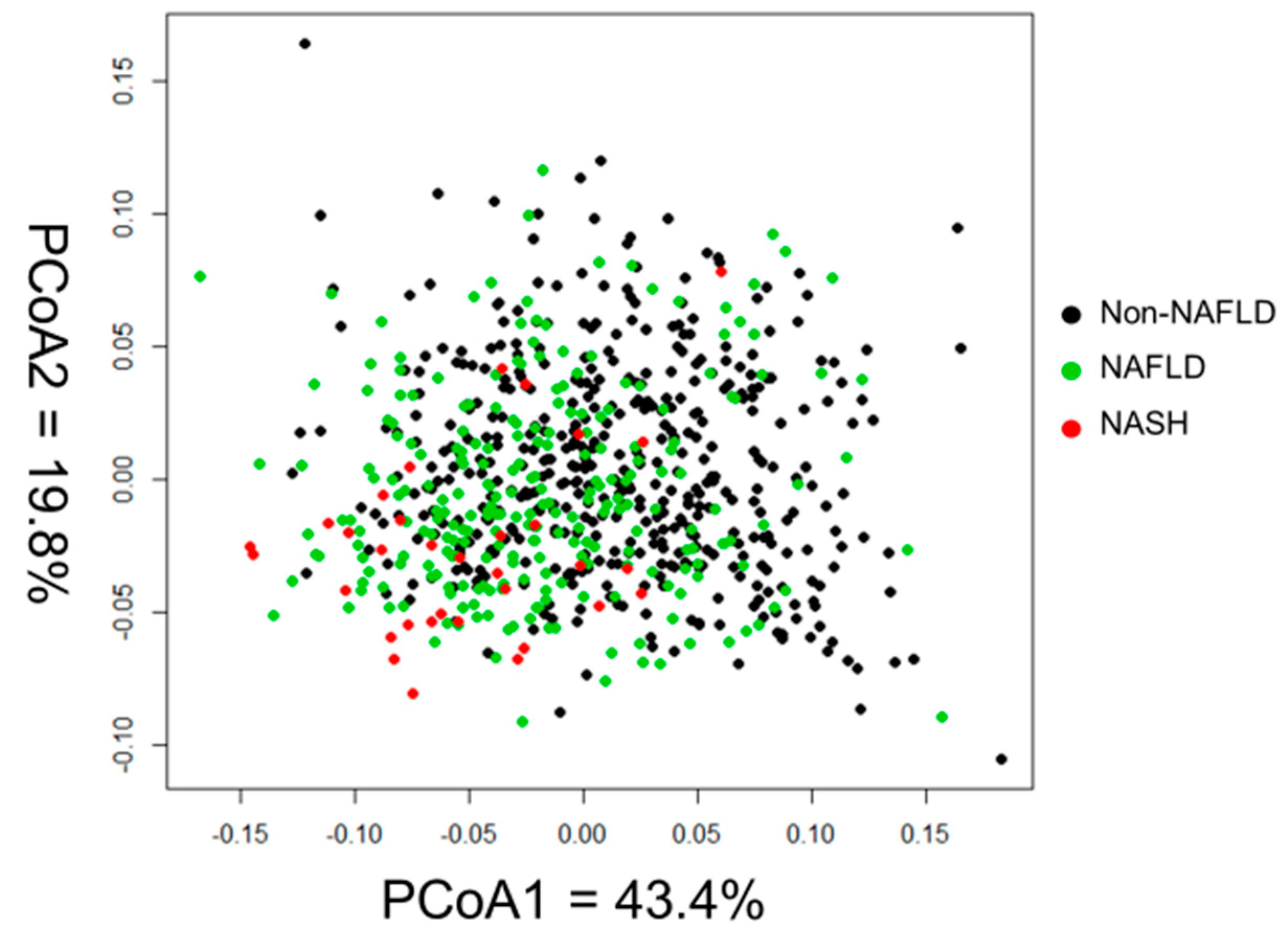
- Iino, C.; Endo, T.; Mikami, K.; Hasegawa, T.; Kimura, M.; Sawada, N.; Nakaji, S.; Fukuda, S. Significant decrease in Faecalibacterium among gut microbiota in nonalcoholic fatty liver disease: A large BMI- and sex-matched population study. Hepatol. Int. 2019, 6, 748–756. [Google Scholar] [CrossRef]
- Kobayashi, S.; Honda, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J. Epidemiol. 2012, 22, 151–159. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef]
- Yamakado, M.; Tanaka, T.; Nagao, K.; Imaizumi, A.; Komatsu, M.; Daimon, T.; Miyano, H.; Tani, M.; Toda, A.; Yamamoto, H.; et al. Plasma amino acid profile associated with fatty liver disease and co-occurrence of metabolic risk factors. Sci. Rep. 2017, 7, 14485. [Google Scholar] [CrossRef]
- Xia, M.F.; Bian, H.; Gao, X. NAFLD and diabetes: Two sides of the same coin? Rationale for gene-based personalized NAFLD treatment. Front. Pharmacol. 2019, 10, 877. [Google Scholar] [CrossRef]
- Gaggini, M.; Morelli, M.; Buzzigoli, E.; DeFronzo, R.A.; Bugianesi, E.; Gastaldelli, A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients 2013, 5, 1544–1560. [Google Scholar] [CrossRef]
- Tai, E.S.; Tan, M.L.; Stevens, R.D.; Low, Y.L.; Muehlbauer, M.J.; Goh, D.L.; Ilkayeva, O.R.; Wenner, B.R.; Bain, J.R.; Lee, J.J.; et al. Insulin resistance is associated with a metabolic profile of altered protein metabolism in Chinese and Asian-Indian men. Diabetologia 2010, 53, 757–767. [Google Scholar] [CrossRef] [PubMed]
- Yan-Do, R.; MacDonald, P.E. Impaired "glycine"-mia in type 2 diabetes and potential mechanisms contributing to glucose homeostasis. Endocrinology 2017, 158, 1064–1073. [Google Scholar] [CrossRef] [PubMed]
- Angulo, P.; Kleiner, D.E.; Dam-Larsen, S.; Adams, L.A.; Bjornsson, E.S.; Charatcharoenwitthaya, P.; Mills, P.R.; Keach, J.C.; Lafferty, H.D.; Stahler, A.; et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015, 149, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Valle, V.; Chávez-Tapia, N.C.; Uribe, M.; Méndez-Sánchez, N. Role of oxidative stress and molecular changes in liver fibrosis: A review. Curr. Med. Chem. 2012, 19, 4850–4860. [Google Scholar] [CrossRef]
- García-Ruiz, C.; Fernández-Checa, J.C. Mitochondrial oxidative stress and antioxidants balance in fatty liver disease. Hepatol. Commun. 2018, 2, 1425–1439. [Google Scholar] [CrossRef]
- Cheng, S.; Rhee, E.P.; Larson, M.G.; Lewis, G.D.; McCabe, E.L.; Shen, D.; Palma, M.J.; Roberts, L.D.; Dejam, A.; Souza, A.L.; et al. Metabolite profiling identifies pathways associated with metabolic risk in humans. Circulation 2012, 125, 2222–2231. [Google Scholar] [CrossRef]
- Chevalier, S.; Burgess, S.C.; Malloy, C.R.; Gougeon, R.; Marliss, E.B.; Morais, J.A. The greater contribution of gluconeogenesis to glucose production in obesity is related to increased whole-body protein catabolism. Diabetes 2006, 55, 675–681. [Google Scholar] [CrossRef]
- Gall, W.E.; Beebe, K.; Lawton, K.A.; Adam, K.P.; Mitchell, M.W.; Nakhle, P.J.; Ryals, J.A.; Milburn, M.V.; Nannipieri, M.; Camastra, S.; et al. Alpha-hydroxybutyrate is an early biomarker of insulin resistance and glucose intolerance in a nondiabetic population. PLoS ONE 2010, 5, e10883. [Google Scholar] [CrossRef]
- Castera, L.; Forns, X.; Alberti, A. Non-invasive evaluation of liver fibrosis using transient elastography. J. Hepatol. 2008, 48, 835–847. [Google Scholar] [CrossRef]
- Rockey, D.C. Noninvasive assessment of liver fibrosis and portal hypertension with transient elastography. Gastroenterology 2008, 134, 8–14. [Google Scholar] [CrossRef]
- Chalasani, N.; Younossi, Z.; Lavine, J.E.; Charlton, M.; Cusi, K.; Rinella, M.; Harrison, S.A.; Brunt, E.M.; Sanyal, A.J. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018, 67, 328–357. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [Google Scholar] [CrossRef] [PubMed]

| Normal | NAFLD | Fibrosis | p Value | p Value | |
|---|---|---|---|---|---|
| Normal vs NAFLD | Normal vs Fibrosis | ||||
| n | 420 | 251 | 33 | ||
| Age (years) | 49.6 ± 16.2 | 54.5 ± 14.9 | 54.1 ± 14.4 | <0.001 | 0.210 |
| Gender, Male | 132 (29.8%) | 100 (39.8%) | 15 (45.5%) | 0.017 | 0.111 |
| BMI (kg/m2) | 21.3 ± 2.7 | 24.3 ± 3.3 | 28.8 ± 5.0 | <0.001 | <0.001 |
| Glucose (mg/dL) | 91 ± 9 | 97 ± 14 | 124 ± 36 | <0.001 | <0.001 |
| Insulin (µU/mL) | 4.7 ± 1.9 | 7.3 ± 8.9 | 11.4 ± 6.1 | <0.001 | <0.001 |
| HOMA-IR | 1.1 ± 0.5 | 1.8 ± 1.9 | 3.6 ± 2.6 | <0.001 | <0.001 |
| Total bilirubin (mg/dL) | 0.9 ± 0.3 | 0.8 ± 0.3 | 0.8 ± 0.3 | 0.010 | 0.376 |
| AST (U/L) | 20.6 ± 5.8 | 23.0 ± 11.4 | 35.8 ± 21.0 | 0.002 | <0.001 |
| ALT (U/L) | 17.4 ± 8.0 | 25.8 ± 27.8 | 50.7 ± 42.3 | <0.001 | <0.001 |
| GGT (U/L) | 23.1 ± 15.9 | 31.9 ± 29.3 | 57.2 ± 62.4 | <0.001 | <0.001 |
| Total cholesterol (mg/dL) | 198 ± 34 | 208 ± 38 | 209 ± 25 | <0.001 | 0.163 |
| Triglycerides (mg/dL) | 76 ± 38 | 103 ± 58 | 136 ± 52 | <0.001 | <0.001 |
| HDL cholesterol (mg/dL) | 68 ± 16 | 61 ± 16 | 54 ± 21 | <0.001 | <0.001 |
| LDL cholesterol (mg/dL) | 113 ± 28 | 126 ± 32 | 127 ± 23 | <0.001 | 0.018 |
| Albumin (g/dL) | 4.4 ± 0.3 | 4.4 ± 0.3 | 4.4 ± 0.3 | 0.310 | 0.920 |
| Platelets (×10⁴/µL) | 26.3 ± 5.9 | 27.1 ± 6.1 | 25.4 ± 5.2 | 0.180 | 0.611 |
| HbA1c (%) | 5.7 ± 0.4 | 5.8 ± 0.5 | 7.0 ± 1.6 | <0.001 | <0.001 |
| Type 2 diabetes | 10 (2.4%) | 15 (6.0%) | 13 (39.4%) | 0.034 | <0.001 |
| Total energy intake (kcal/day) | 1807 ± 547 | 1809 ± 548 | 1796 ± 569 | 0.998 | 0.991 |
| Protein intake (g/day) | 71 ± 26 | 73 ± 27 | 67 ± 28 | 0.705 | 0.622 |
| CAP (dB/m) | 183 ± 36 | 277 ± 32 | 320 ± 31 | <0.001 | <0.001 |
| LS (kPa) | 4.2 ± 1.1 | 4.4 ± 1.1 | 9.8 ± 2.7 | 0.175 | <0.001 |
| Normal | NAFLD | Fibrosis | p Value | p Value | |
|---|---|---|---|---|---|
| Normal vs. NAFLD | Normal vs. Fibrosis | ||||
| Amino acid (nmol/mL) | n = 420 | n = 251 | n = 33 | ||
| Valine | 199 (178–224) | 223 (197–245) | 257 (222–284) | <0.001 | <0.001 |
| Leucine | 102 (92–118) | 115 (100–130) | 132 (112–150) | <0.001 | <0.001 |
| Isoleucine | 52 (46–61) | 58 (49–68) | 69 (57–78) | <0.001 | <0.001 |
| Methionine | 24 (22–27) | 25 (22–27) | 24 (21–27) | 0.111 | 0.781 |
| Lysine | 194 (174–211) | 198 (180–221) | 207 (188–226) | 0.010 | 0.010 |
| Phenylalanine | 54 (50–59) | 56 (52–62) | 58 (53–66) | <0.001 | 0.003 |
| Histidine | 79 (73–84) | 80 (75–85) | 78 (73–82) | 0.020 | 0.712 |
| Threonine | 123 (107–143) | 125 (109–146) | 117 (110–139) | 0.474 | 0.924 |
| Tryptophan | 44 (40–49) | 46 (41–51) | 45 (39–53) | 0.007 | 0.417 |
| Tyrosine | 55 (49–63) | 61 (54–68) | 71 (62–78) | <0.001 | <0.001 |
| Glycine | 241 (211–284) | 223 (196–271) | 192 (165–216) | <0.001 | <0.001 |
| Alanine | 310 (261–369) | 356 (307–402) | 387 (347–419) | <0.001 | <0.001 |
| Serine | 120 (108–138) | 115 (102–130) | 117 (100–128) | 0.002 | 0.077 |
| Arginine | 80 (68–93) | 83 (71–94) | 82 (74–92) | 0.214 | 0.715 |
| Cystine | 27 (20–34) | 31 (25–37) | 34 (28–41) | <0.001 | <0.001 |
| Asparagine | 52 (47–57) | 50 (45–55) | 48 (45–52) | 0.040 | 0.035 |
| Glutamine | 590 (543–637) | 593 (546–637) | 575 (519–613) | 0.953 | 0.157 |
| Proline | 129 (107–157) | 141 (118–174) | 152 (127–166) | <0.001 | 0.002 |
| Aspartic acid | 4 (3–5) | 4 (3–5) | 5 (4–5) | <0.001 | <0.001 |
| Glutamate | 42 (32–53) | 53 (39–67) | 69 (57–85) | <0.001 | <0.001 |
| r | p Value | |
|---|---|---|
| Valine | 0.359 | <0.001 |
| Leucine | 0.253 | <0.001 |
| Isoleucine | 0.274 | <0.001 |
| Methionine | −0.014 | 0.697 |
| Lysine | 0.046 | 0.214 |
| Phenylalanine | 0.164 | <0.001 |
| Histidine | −0.080 | 0.030 |
| Threonine | −0.033 | 0.370 |
| Tryptophan | 0.112 | 0.002 |
| Tyrosine | 0.274 | <0.001 |
| Glycine | −0.227 | <0.001 |
| Alanine | 0.337 | <0.001 |
| Serine | −0.170 | <0.001 |
| Arginine | 0.004 | 0.922 |
| Cystine | 0.241 | <0.001 |
| Asparagine | −0.250 | <0.001 |
| Glutamine | −0.142 | <0.001 |
| Proline | 0.225 | <0.001 |
| Aspartic acid | 0.318 | <0.001 |
| Glutamate | 0.494 | <0.001 |
| Normal | NAFLD | Fibrosis | p Value | p Value | |
|---|---|---|---|---|---|
| Normal vs NAFLD | Normal vs Fibrosis | ||||
| n | 15 | 15 | 15 | ||
| Age (years) | 55.8 ± 14.4 | 53.2 ± 14.4 | 57.4 ± 13.7 | 0.843 | 0.937 |
| Gender, Male | 6 (40.0%) | 3 (20.0%) | 6 (40.0%) | 0.696 | 0.999 |
| BMI (kg/m2) | 22.0 ± 3.4 | 26.9 ± 4.7 | 26.6 ± 4.3 | 0.007 | 0.011 |
| Glucose (mg/dL) | 104 ± 16 | 102 ± 20 | 112 ± 31 | 0.989 | 0.544 |
| Insulin (µU/mL) | 8.1 ± 2.6 | 8.3 ± 2.4 | 7.7 ± 2.5 | 0.981 | 0.884 |
| HOMA-IR | 2.2 ± 1.0 | 2.2 ± 0.9 | 2.2 ± 0.9 | 0.999 | 0.999 |
| Total bilirubin (mg/dL) | 0.9 ± 0.3 | 0.7 ± 0.2 | 0.9 ± 0.3 | 0.134 | 0.852 |
| AST (U/L) | 20.9 ± 5.3 | 25.7 ± 8.2 | 39.9 ± 26.4 | 0.645 | 0.007 |
| ALT (U/L) | 20.2 ± 6.9 | 30.0 ± 13.3 | 58.1 ± 58.6 | 0.680 | 0.012 |
| GGT (U/L) | 27.9 ± 14 | 36.8 ± 15.9 | 54.0 ± 33.5 | 0.487 | 0.008 |
| Total cholesterol (mg/dL) | 203 ± 29 | 210 ± 37 | 211 ± 20 | 0.778 | 0.712 |
| Triglycerides (mg/dL) | 90 ± 41 | 139 ± 70 | 113 ± 33 | 0.026 | 0.366 |
| HDL cholesterol (mg/dL) | 66 ± 16 | 56 ± 14 | 56 ± 13 | 0.127 | 0.156 |
| LDL cholesterol (mg/dL) | 117 ± 26 | 127 ± 28 | 129 ± 17 | 0.444 | 0.286 |
| Albumin (g/dL) | 4.4 ± 0.3 | 4.3 ± 0.3 | 4.4 ± 0.3 | 0.419 | 0.827 |
| Platelets (×10⁴/µL) | 28.3 ± 7.7 | 27.0 ± 5.3 | 25.8 ± 4.8 | 0.805 | 0.466 |
| HbA1c (%) | 6.1 ± 0.8 | 6.1 ± 0.8 | 6.5 ± 1.4 | 0.983 | 0.554 |
| Type 2 diabetes | 0 | 0 | 7 (46.7%) | 0.999 | 0.008 |
| CAP (dB/m) | 186 ± 39 | 280 ± 39 | 306 ± 28 | <0.001 | <0.001 |
| LS (kPa) | 4.8 ± 1.3 | 4.4 ± 1.2 | 9.8 ± 1.9 | 0.754 | <0.001 |
| Normal | NAFLD | Fibrosis | p Value | p Value | |
|---|---|---|---|---|---|
| Normal vs NAFLD | Normal vs Fibrosis | ||||
| Amino acid (nmol/mL) | n = 15 | n = 15 | n = 15 | ||
| Valine | 211 (177–241) | 242 (220–257) | 233 (212–271) | 0.081 | 0.117 |
| Leucine | 102 (94–130) | 118 (108–129) | 117 (110–143) | 0.208 | 0.151 |
| Isoleucine | 52 (45–64) | 59 (53–63) | 63(54–74) | 0.299 | 0.145 |
| Methionine | 23 (21–27) | 25 (23–28) | 24 (22–25) | 0.320 | 0.904 |
| Lysine | 186 (169–214) | 194 (181–222) | 204 (193–230) | 0.546 | 0.178 |
| Phenylalanine | 56 (52–60) | 62 (55–64) | 56 (53–65) | 0.164 | 0.717 |
| Histidine | 76 (70–81) | 81 (79–85) | 80 (78–87) | 0.057 | 0.178 |
| Threonine | 126 (114–135) | 135 (124–153) | 125 (114–140) | 0.260 | 0.992 |
| Tryptophan | 41 (39–47) | 48 (43–51) | 43 (38–50) | 0.127 | 0.872 |
| Tyrosine | 59 (53–67) | 67 (62–70) | 66 (60–75) | 0.138 | 0.260 |
| Glycine | 260 (229–284) | 210 (183–295) | 192 (173–229) | 0.321 | 0.016 |
| Alanine | 332 (310–357) | 369 (362–475) | 360 (321–424) | 0.004 | 0.242 |
| Serine | 120 (110–131) | 109 (99–121) | 108 (100–129) | 0.260 | 0.401 |
| Arginine | 86 (66–92) | 84 (76–91) | 82 (73–85) | 0.999 | 0.992 |
| Cystine | 31(25–42) | 34 (26–40) | 33 (28–41) | 0.985 | 0.998 |
| Asparagine | 51(49–52) | 51 (48–55) | 49 (47–53) | 0.824 | 0.969 |
| Glutamine | 618(586–647) | 593 (540–644) | 610 (538–631) | 0.731 | 0.389 |
| Proline | 138(114–177) | 147 (124–172) | 148 (123–156) | 0.997 | 0.999 |
| Aspartic acid | 4 (3–5) | 4 (3–4) | 4 (4–5) | 0.913 | 0.771 |
| Glutamate | 50 (34–58) | 57 (42–65) | 59 (56–67) | 0.574 | 0.045 |
| Variables | Multivariable | ||
|---|---|---|---|
| OR | 95% CI | p value | |
| HOMA-IR | 1.43 | 1.12–1.91 | <0.001 |
| Glutamate | 1.03 | 1.01–1.05 | <0.001 |
| Glycine | 0.99 | 0.98–0.99 | 0.041 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasegawa, T.; Iino, C.; Endo, T.; Mikami, K.; Kimura, M.; Sawada, N.; Nakaji, S.; Fukuda, S. Changed Amino Acids in NAFLD and Liver Fibrosis: A Large Cross-Sectional Study without Influence of Insulin Resistance. Nutrients 2020, 12, 1450. https://doi.org/10.3390/nu12051450
Hasegawa T, Iino C, Endo T, Mikami K, Kimura M, Sawada N, Nakaji S, Fukuda S. Changed Amino Acids in NAFLD and Liver Fibrosis: A Large Cross-Sectional Study without Influence of Insulin Resistance. Nutrients. 2020; 12(5):1450. https://doi.org/10.3390/nu12051450
Chicago/Turabian StyleHasegawa, Takuma, Chikara Iino, Tetsu Endo, Kenichiro Mikami, Masayo Kimura, Naoya Sawada, Shigeyuki Nakaji, and Shinsaku Fukuda. 2020. "Changed Amino Acids in NAFLD and Liver Fibrosis: A Large Cross-Sectional Study without Influence of Insulin Resistance" Nutrients 12, no. 5: 1450. https://doi.org/10.3390/nu12051450
APA StyleHasegawa, T., Iino, C., Endo, T., Mikami, K., Kimura, M., Sawada, N., Nakaji, S., & Fukuda, S. (2020). Changed Amino Acids in NAFLD and Liver Fibrosis: A Large Cross-Sectional Study without Influence of Insulin Resistance. Nutrients, 12(5), 1450. https://doi.org/10.3390/nu12051450





