Probiotics in Pediatrics. A Review and Practical Guide
Abstract
:1. Introduction
2. Methods
3. Results: Evidence of Efficacy of Probiotics
3.1. Diarrhea
3.1.1. Acute Gastroenteritis
3.1.2. Antibiotic-Associated Diarrhea
3.1.3. Clostridioides Difficile-Associated Diarrhea (CDAD)
3.1.4. Nosocomial Diarrhea
3.2. Functional Gastrointestinal Disorders
3.2.1. Infantile Colic
3.2.2. Regurgitation
3.2.3. Irritable Bowel Syndrome
3.2.4. Functional Constipation
3.3. Inflammatory Bowel Disease
3.3.1. Ulcerative Colitis (UC)
3.3.2. Crohn’s Disease
3.4. Helicobacter (H.) pylori
3.5. Necrotizing Enterocolitis and Late-Onset Sepsis
3.6. Allergic Diseases
3.6.1. Atopic Dermatitis
3.6.2. Asthma and Allergic Rhinitis
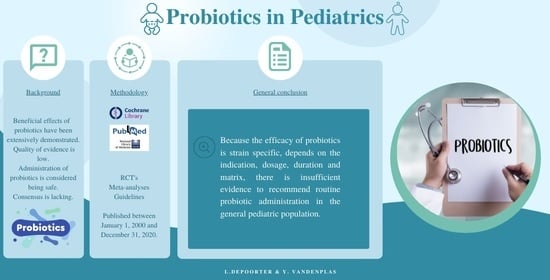
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hojsak, I.; Fabiano, V.; Pop, T.L.; Goulet, O.; Zuccotti, G.V.; Çokuğraş, F.C.; Pettoello-Mantovani, M.; Kolaček, S. Guidance on the Use of Probiotics in Clinical Practice in Children with Selected Clinical Conditions and in Specific Vulnerable Groups. Acta Paediatr. Int. J. Paediatr. 2018, 107, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Kołodziej, M.; Gieruszczak-Białek, D.; Skórka, A.; Ruszczyński, M.; Shamir, R. Systematic Review with Meta-Analysis: Lactobacillus rhamnosus GG for Treating Acute Gastroenteritis in Children—A 2019 Update. Aliment. Pharmacol. Ther. 2019, 49, 1376–1384. [Google Scholar] [CrossRef]
- Fiocchi, A.; Pawankar, R.; Cuello-Garcia, C.; Ahn, K.; Al-Hammadi, S.; Agarwal, A.; Beyer, K.; Burks, W.; Canonica, G.W.; Ebisawa, M.; et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Probiotics. World Allergy Organ. J. 2015, 8, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hill, C.; Guarner, F.; Reid, G.; Gibson, G.R.; Merenstein, D.J.; Pot, B.; Morelli, L.; Canani, R.B.; Flint, H.J.; Salminen, S.; et al. Expert Consensus Document: The International Scientific Association for Probiotics and Prebiotics Consensus Statement on the Scope and Appropriate Use of the Term Probiotic. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 506–514. [Google Scholar] [CrossRef] [Green Version]
- Kolaček, S.; Hojsak, I.; Berni Canani, R.; Guarino, A.; Indrio, F.; Orel, R.; Pot, B.; Shamir, R.; Szajewska, H.; Vandenplas, Y.; et al. Commercial Probiotic Products: A Call for Improved Quality Control. A Position Paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 117–124. [Google Scholar] [CrossRef] [PubMed]
- De Simone, C. The Unregulated Probiotic Market. Clin. Gastroenterol. Hepatol. 2019, 17, 809–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, G.L.; Ko, C.W.; Bercik, P.; Falck-Ytter, Y.; Sultan, S.; Weizman, A.V.; Morgan, R.L. AGA Clinical Practice Guidelines on the Role of Probiotics in the Management of Gastrointestinal Disorders. Gastroenterology 2020, 159, 697–705. [Google Scholar] [CrossRef]
- Suez, J.; Zmora, N.; Segal, E.; Elinav, E. The Pros, Cons, and Many Unknowns of Probiotics. Nat. Med. 2019, 25, 716–729. [Google Scholar] [CrossRef]
- Koutsoumanis, K.; Allende, A.; Alvarez-Ordóñez, A.; Bolton, D.; Bover-Cid, S.; Chemaly, M.; Davies, R.; De Cesare, A.; Hilbert, F.; Lindqvist, R.; et al. Scientific Opinion on the Update of the List of QPS-Recommended Biological Agents Intentionally Added to Food or Feed as Notified to EFSA (2017–2019). EFSA J. 2020, 18, 5966. [Google Scholar] [CrossRef] [Green Version]
- Markowiak, P.; Ślizewska, K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients 2017, 9, 1021. [Google Scholar] [CrossRef]
- Szajewska, H.; Guarino, A.; Hojsak, I.; Indrio, F.; Kolacek, S.; Orel, R.; Salvatore, S.; Shamir, R.; van Goudoever, J.B.; Vandenplas, Y.; et al. Use of Probiotics for the Management of Acute Gastroenteritis in Children: An Update. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 261–269. [Google Scholar] [CrossRef]
- Van den Akker, C.H.P.; van Goudoever, J.B.; Shamir, R.; Domellöf, M.; Embleton, N.D.; Hojsak, I.; Lapillonne, A.; Mihatsch, W.A.; Berni Canani, R.; Bronsky, J.; et al. Probiotics and Preterm Infants: A Position Paper by the European Society for Paediatric Gastroenterology Hepatology and Nutrition Committee on Nutrition and the European Society for Paediatric Gastroenterology Hepatology and Nutrition Working Group for Probiotics and Prebiotics. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 664–680. [Google Scholar] [CrossRef]
- Poindexter, B.; Committee on Fetus and Newborn. Use of Probiotics in Preterm Infants. Pediatrics 2021, 147, e2021051485. [Google Scholar] [CrossRef]
- McFarland, L.V.; Evans, C.T.; Goldstein, E.J.C. Strain-Specificity and Disease-Specificity of Probiotic Efficacy: A Systematic Review and Meta-Analysis. Front. Med. 2018, 5, 124. [Google Scholar] [CrossRef] [PubMed]
- Pot, B.; Vandenplas, Y. Factors That Influence Clinical Efficacy of Live Biotherapeutic Products. Eur. J. Med. Res. 2021, 26, 1–10. [Google Scholar] [CrossRef]
- Guarino, A.; Ashkenazi, S.; Gendrel, D.; Lo Vecchio, A.; Shamir, R.; Szajewska, H. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition/European Society for Pediatric Infectious Diseases Evidence-Based Guidelines for the Management of Acute Gastroenteritis in Children in Europe: Update 2014. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 132–152. [Google Scholar] [CrossRef]
- Allen, S.J.; Martinez, E.G.; Gregorio, G.V.; Dans, L.F. Probiotics for Treating Acute Infectious Diarrhea. Cochrane Database Syst. Rev. 2010, 2010, CD003048. [Google Scholar] [CrossRef] [Green Version]
- Szajewska, H.; Guarino, A.; Hojsak, I.; Indrio, F.; Kolacek, S.; Shamir, R.; Vandenplas, Y.; Weizman, Z. Use of Probiotics for Management of Acute Gastroenteritis: A Position Paper by the ESPGHAN Working Group for Probiotics and Prebiotics. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 531–539. [Google Scholar] [CrossRef] [Green Version]
- Szajewska, H.; Kołodziej, M.; Zalewski, B.M. Systematic Review with Meta-Analysis: Saccharomyces boulardii for Treating Acute Gastroenteritis in Children—A 2020 Update. Aliment. Pharmacol. Ther. 2020, 51, 678–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feizizadeh, S.; Salehi-Abargouei, A.; Akbari, V. Efficacy and Safety of Saccharomyces boulardii for Acute Diarrhea. Pediatrics 2014, 134, e176–e191. [Google Scholar] [CrossRef] [Green Version]
- Patro-Gołąb, B.; Szajewska, H. Systematic Review with Meta-Analysis: Lactobacillus reuteri DSM 17938 for Treating Acute Gastroenteritis in Children. An Update. Nutrients 2019, 11, 2762. [Google Scholar] [CrossRef] [Green Version]
- Rosenfeldt, V.; Michaelsen, K.F.; Jakobsen, M.; Larsen, C.N.; Møller, P.L.; Tvede, M.; Weyrehter, H.; Valerius, N.H.; Paerregaard, A. Effect of Probiotic Lactobacillus Strains on Acute Diarrhea in a Cohort of Nonhospitalized Children Attending Day-Care Centers. Pediatr. Infect. Dis. J. 2002, 21, 417–419. [Google Scholar] [CrossRef]
- Collinson, S.; Deans, A.; Padua-Zamora, A.; Gregorio, G.V.; Li, C.; Dans, L.F.; Allen, S.J. Probiotics for Treating Acute Infectious Diarrhoea. Cochrane Database Syst. Rev. 2020, 12, CD003048. [Google Scholar] [CrossRef] [PubMed]
- Vassilopoulou, L.; Spyromitrou-Xioufi, P.; Ladomenou, F. Effectiveness of Probiotics and Synbiotics in Reducing Duration of Acute Infectious Diarrhea in Pediatric Patients in Developed Countries: A Systematic Review and Meta-Analysis. Eur. J. Pediatr. 2021. [Google Scholar] [CrossRef] [PubMed]
- Urbańska, M.; Szajewska, H. The Efficacy of Lactobacillus reuteri DSM 17938 in Infants and Children: A Review of the Current Evidence. Eur. J. Pediatr. 2014, 173, 1327–1337. [Google Scholar] [CrossRef] [PubMed]
- Szajewska, H.; Wanke, M.; Patro, B. Meta-Analysis: The Effects of Lactobacillus rhamnosus GG Supplementation for the Prevention of Healthcare-Associated Diarrhoea in Children. Aliment. Pharmacol. Ther. 2011, 34, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Castrellon, P.; Lopez-Velazquez, G.; Diaz-Garcia, L.; Jimenez-Gutierrez, C.; Mancilla-Ramirez, J.; Estevez-Jimenez, J.; Parra, M. Diarrhea in Preschool Children and Lactobacillus reuteri: A Randomized Controlled Trial. Pediatrics 2014, 133, e904–e909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McFarland, L.V. Antibiotic-Associated Diarrhea: Epidemiology, Trends and Treatment. Future Microbiol. 2008, 3, 563–578. [Google Scholar] [CrossRef]
- Mantegazza, C.; Molinari, P.; D’Auria, E.; Sonnino, M.; Morelli, L.; Zuccotti, G.V. Probiotics and Antibiotic-Associated Diarrhea in Children: A Review and New Evidence on Lactobacillus rhamnosus GG during and after Antibiotic Treatment. Pharmacol. Res. 2018, 128, 63–72. [Google Scholar] [CrossRef]
- Guo, Q.; Goldenberg, J.Z.; Humphrey, C.; El Dib, R.; Johnston, B.C. Probiotics for the Prevention of Pediatric Antibiotic-Associated Diarrhea. Cochrane Database Syst. Rev. 2019, 4, CD004827. [Google Scholar] [CrossRef]
- Ma, Y.; Yang, J.Y.; Peng, X.; Xiao, K.Y.; Xu, Q.; Wang, C. Which Probiotic Has the Best Effect on Preventing Clostridium Difficile-Associated Diarrhea? A Systematic Review and Network Meta-Analysis. J. Dig. Dis. 2020, 21, 69–80. [Google Scholar] [CrossRef]
- Kullar, R.; Johnson, S.; McFarland, L.V.; Goldstein, E.J.C. Potential Roles for Probiotics in the Treatment of COVID-19 Patients and Prevention of Complications Associated with Increased Antibiotic Use. Antibiotics 2021, 10, 408. [Google Scholar] [CrossRef]
- Szajewska, H.; Canani, R.B.; Guarino, A.; Hojsak, I.; Indrio, F.; Kolacek, S.; Orel, R.; Shamir, R.; Vandenplas, Y.; Van Goudoever, J.B.; et al. Probiotics for the Prevention of Antibiotic-Associated Diarrhea in Children. J. Pediatr. Gastroenterol. Nutr. 2016, 62, 495–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldenberg, J.Z.; Mertz, D.; Johnston, B.C. Probiotics to Prevent Clostridium Difficile Infection in Patients Receiving Antibiotics. JAMA J. Am. Med. Assoc. 2018, 320, 499–500. [Google Scholar] [CrossRef] [Green Version]
- Goldenberg, J.Z.; Yap, C.; Lytvyn, L.; Lo, C.K.F.; Beardsley, J.; Mertz, D.J.B. Probiotics for the Prevention of Clostridium difficile-Associated Diarrhea in Adults and Children. Cochrane Database Syst. Rev. 2017, 12, CD006095. [Google Scholar] [CrossRef]
- WHO. Prevention of Hospital-Acquired Infections. A Practical Guide; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Hojsak, I.; Szajewska, H.; Canani, R.B.; Guarino, A.; Indrio, F.; Kolacek, S.; Orel, R.; Shamir, R.; Vandenplas, Y.; Van Goudoever, J.B.; et al. Probiotics for the Prevention of Nosocomial Diarrhea in Children. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 3–9. [Google Scholar] [CrossRef]
- Bruzzese, E.; Fedele, M.; Bruzzese, D.; Viscovo, S.; Giannattasio, A.; Mandato, C.; Siani, P.; Guarino, A. Randomised Clinical Trial: A Lactobacillus GG and Micronutrient-Containing Mixture Is Effective in Reducing Nosocomial Infections in Children, vs. Placebo. Aliment. Pharmacol. Ther. 2016, 44, 568–575. [Google Scholar] [CrossRef]
- Wanke, M.; Szajewska, H. Lack of an Effect of Lactobacillus reuteri DSM 17938 in Preventing Nosocomial Diarrhea in Children: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Pediatr. 2012, 161, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Urbańska, M.; Gieruszczak-Białek, D.; Szymański, H.; Szajewska, H. Effectiveness of Lactobacillus reuteri DSM 17938 for the Prevention of Nosocomial Diarrhea in Children: A Randomized, Double-Blind, Placebo-Controlled Trial. Pediatr. Infect. Dis. J. 2016, 35, 142–145. [Google Scholar] [CrossRef]
- Hojsak, I.; Pivac, V.T.; Pavić, A.M.; Pasini, A.M.; Kolaček, S. Bifidobacterium animalis Subsp. Lactis Fails to Prevent Common Infections in Hospitalized Children: A Randomized, Double-Blind, Placebo-Controlled Study. Am. J. Clin. Nutr. 2015, 101, 680–684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wessel, M.A.; Cobb, J.C.; Jackson, E.B.; Harris, G.S.; Detwiler, A.C. Paroxysmal Fussing in Infancy, Sometimes Called Colic. Pediatrics 1954, 14, 421–435. [Google Scholar]
- Ong, T.G.; Gordon, M.; Banks, S.S.C.; Thomas, M.R.; Akobeng, A.K. Probiotics to Prevent Infantile Colic. Cochrane Database Syst. Rev. 2019, 3, CD012473. [Google Scholar] [CrossRef] [PubMed]
- Sung, V.; D’Amico, F.; Cabana, M.D.; Chau, K.; Koren, G.; Savino, F.; Szajewska, H.; Deshpande, G.; Dupont, C.; Indrio, F.; et al. Lactobacillus reuteri to Treat Infant Colic: A Meta-Analysis. Pediatrics 2018, 141, e20171811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harb, T.; Matsuyama, M.; David, M.; Hill, R.J. Infant Colic—What Works: A Systematic Review of Interventions for Breast-Fed Infants. J. Pediatr. Gastroenterol. Nutr. 2016, 62, 668–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schreck Bird, A.; Gregory, P.J.; Jalloh, M.A.; Risoldi Cochrane, Z.; Hein, D.J. Probiotics for the Treatment of Infantile Colic: A Systematic Review. J. Pharm. Pract. 2017, 30, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Simonson, J.; Haglund, K.; Weber, E.; Fial, A.; Hanson, L. Probiotics for the Management of Infantile Colic: A Systematic Review. Am. J. Matern. Child Nurs. 2021, 46, 88–96. [Google Scholar] [CrossRef]
- Dryl, R.; Szajewska, H. Probiotics for Management of Infantile Colic: A Systematic Review of Randomized Controlled Trials. Arch. Med. Sci. 2018, 14, 1137–1143. [Google Scholar] [CrossRef] [Green Version]
- Gutiérrez-Castrellón, P.; Indrio, F.; Bolio-Galvis, A.; Jiménez-Gutiérrez, C.; Jimenez-Escobar, I.; López-Velázquez, G. Efficacy of Lactobacillus reuteri DSM 17938 for Infantile Colic: Systematic Review with Network Meta-Analysis. Medicine 2017, 96, e9375. [Google Scholar] [CrossRef]
- Sung, V.; Hiscock, H.; Tang, M.L.K.; Mensah, F.K.; Nation, M.L.; Satzke, C.; Heine, R.G.; Stock, A.; Barr, R.G.; Wake, M. Treating Infant Colic with the Probiotic Lactobacillus reuteri: Double Blind, Placebo Controlled Randomised Trial. BMJ 2014, 348, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Giglione, E.; Prodam, F.; Bellone, S.; Monticone, S.; Beux, S.; Marolda, A.; Pagani, A.; Di Gioia, D.; Del Piano, M.; Mogna, G.; et al. The Association of Bifidobacterium breve BR03 and B632 Is Effective to Prevent Colics in Bottle-Fed Infants. J. Clin. Gastroenterol. 2016, 50, S164–S167. [Google Scholar] [CrossRef]
- Aloisio, I.; Prodam, F.; Giglione, E.; Bozzi Cionci, N.; Solito, A.; Bellone, S.; Baffoni, L.; Mogna, L.; Pane, M.; Bona, G.; et al. Three-Month Feeding Integration with Bifidobacterium Strains Prevents Gastrointestinal Symptoms in Healthy Newborns. Front. Nutr. 2018, 5, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Savino, F.; Ceratto, S.; Poggi, E.; Cartosio, M.E.; Cordero di Montezemolo, L.; Giannattasio, A. Preventive Effects of Oral Probiotic on Infantile Colic: A Prospective, Randomised, Blinded, Controlled Trial Using Lactobacillus reuteri DSM 17938. Benef. Microbes 2015, 6, 245–251. [Google Scholar] [CrossRef]
- Rosen, R.; Vandenplas, Y.; Singendonk, M.; Cabana, M.; Di Lorenzo, C.; Gottrand, F.; Gupta, S.; Langendam, M.; Staiano, A.; Thapar, N.; et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 2018, 66, 516–554. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Hon, K.L. Gastroesophageal Reflux in Children: An Updated Review. Drugs Context 2019, 8, 1–12. [Google Scholar] [CrossRef]
- Perceval, C.; Szajewska, H.; Indrio, F.; Weizman, Z.; Vandenplas, Y. Prophylactic Use of Probiotics for Gastrointestinal Disorders in Children. Lancet Child Adolesc. Health 2019, 3, 655–662. [Google Scholar] [CrossRef]
- Garofoli, F.; Civardi, E.; Indrio, F.; Mazzucchelli, I.; Angelini, M.; Tinelli, C.; Stronati, M. The Early Administration of Lactobacillus reuteri DSM 17938 Controls Regurgitation Episodes in Full-Term Breastfed Infants. Int. J. Food Sci. Nutr. 2014, 65, 646–648. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Di Mauro, A.; Riezzo, G.; Civardi, E.; Intini, C.; Corvaglia, L.; Ballardini, E.; Bisceglia, M.; Cinquetti, M.; Brazzoduro, E.; et al. Prophylactic Use of a Probiotic in the Prevention of Colic, Regurgitation, and Functional Constipation a Randomized Clinical Trial. JAMA Pediatr. 2014, 168, 228–233. [Google Scholar] [CrossRef]
- Indrio, F.; Riezzo, G.; Raimondi, F.; Bisceglia, M.; Filannino, A.; Cavallo, L.; Francavilla, R. Lactobacillus reuteri Accelerates Gastric Emptying and Improves Regurgitation in Infants. Eur. J. Clin. Investig. 2011, 41, 417–422. [Google Scholar] [CrossRef]
- Vandenplas, Y.; Analitis, A.; Tziouvara, C.; Kountzoglou, A.; Drakou, A.; Tsouvalas, M.; Mavroudi, A.; Xinias, I. Safety of a New Synbiotic Starter Formula. Pediatr. Gastroenterol. Hepatol. Nutr. 2017, 20, 167–177. [Google Scholar] [CrossRef]
- Sandhu, B.K.; Paul, S.P. Irritable Bowel Syndrome in Children: Pathogenesis, Diagnosis and Evidence-Based Treatment. World J. Gastroenterol. 2014, 20, 6013–6023. [Google Scholar] [CrossRef]
- Korterink, J.J.; Diederen, K.; Benninga, M.A.; Tabbers, M.M. Epidemiology of Pediatric Functional Abdominal Pain Disorders: A Meta-Analysis. PLoS ONE 2015, 10, e0126982. [Google Scholar] [CrossRef] [Green Version]
- Pärtty, A.; Rautava, S.; Kalliomäki, M. Probiotics on Pediatric Functional Gastrointestinal Disorders. Nutrients 2018, 10, 1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maragkoudaki, M.; Chouliaras, G.; Orel, R.; Horvath, A.; Szajewska, H.; Papadopoulou, A. Lactobacillus reuteri DSM 17938 and a Placebo Both Significantly Reduced Symptoms in Children with Functional Abdominal Pain. Acta Paediatr. Int. J. Paediatr. 2017, 106, 1857–1862. [Google Scholar] [CrossRef]
- Romano, C.; Ferrau’, V.; Cavataio, F.; Iacono, G.; Spina, M.; Lionetti, E.; Comisi, F.; Famiani, A.; Comito, D. Lactobacillus reuteri in Children with Functional Abdominal Pain (FAP). J. Paediatr. Child. Health 2014, 50, E68–E71. [Google Scholar] [CrossRef] [PubMed]
- Horvath, A.; Dziechciarz, P.; Szajewska, H. Meta-Analysis: Lactobacillus rhamnosus GG for Abdominal Pain-Related Functional Gastrointestinal Disorders in Childhood. Aliment. Pharmacol. Ther. 2011, 33, 1302–1310. [Google Scholar] [CrossRef]
- Francavilla, R.; Miniello, V.; Magistà, A.M.; De Canio, A.; Bucci, N.; Gagliardi, F.; Lionetti, E.; Castellaneta, S.; Polimeno, L.; Peccarisi, L.; et al. A Randomized Controlled Trial of Lactobacillus GG in Children with Functional Abdominal Pain. Pediatrics 2010, 126, e1445–e1452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guandalini, S.; Magazzù, G.; Chiaro, A.; La Balestra, V.; Di Nardo, G.; Gopalan, S.; Sibal, A.; Romano, C.; Canani, R.B.; Lionetti, P.; et al. VSL#3 Improves Symptoms in Children with Irritable Bowel Syndrome: A Multicenter, Randomized, Placebo-Controlled, Double-Blind, Crossover Study. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Rutten, J.M.T.M.; Korterink, J.J.; Venmans, L.M.A.J.; Benninga, M.A.; Tabbers, M.M. Nonpharmacologic Treatment of Functional Abdominal Pain Disorders: A Systematic Review. Pediatrics 2015, 135, 522–535. [Google Scholar] [CrossRef] [Green Version]
- Hyams, J.S.; Di Lorenzo, C.; Saps, M.; Shulman, R.J.; Staiano, A.; Van Tilburg, M. Childhood Functional Gastrointestinal Disorders: Child/Adolescent. Gastroenterology 2016, 150, 1456–1468.e2. [Google Scholar] [CrossRef]
- Benninga, M.A.; Nurko, S.; Faure, C.; Hyman, P.E.; St James Roberts, I.; Schechter, N.L. Childhood Functional Gastrointestinal Disorders: Neonate/Toddler. Gastroenterology 2016, 150, 1443–1455.e2. [Google Scholar] [CrossRef]
- Huang, R.; Hu, J. Positive Effect of Probiotics on Constipation in Children: A Systematic Review and Meta-Analysis of Six Randomized Controlled Trials. Front. Cell. Infect. Microbiol. 2017, 7, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koppen, I.; Benninga, M.; Tabbers, M. Is There a Role for Pre-, pro- and Synbiotics in the Treatment of Functional Constipation in Children? A Systematic Review. J. Pediatr. Gastroenterol. Nutr. 2016, 63 (Suppl. 1), S27–S35. [Google Scholar] [PubMed]
- Wojtyniak, K.; Szajewska, H. Systematic Review: Probiotics for Functional Constipation in Children. Eur. J. Pediatr. 2017, 176, 1155–1162. [Google Scholar] [CrossRef] [Green Version]
- Tabbers, M.M.; Dilorenzo, C.; Berger, M.Y.; Faure, C.; Langendam, M.W.; Nurko, S.; Staiano, A.; Vandenplas, Y.; Benninga, M.A. Evaluation and Treatment of Functional Constipation in Infants and Children: Evidence-Based Recommendations from ESPGHAN and NASPGHAN. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 258–274. [Google Scholar] [CrossRef]
- Miele, E.; Shamir, R.; Aloi, M.; Assa, A.; Braegger, C.; Bronsky, J.; De Ridder, L.; Escher, J.C.; Hojsak, I.; Kolaček, S.; et al. Nutrition in Pediatric Inflammatory Bowel Disease: A Position Paper on Behalf of the Porto Inflammatory Bowel Disease Group of the European Society of Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 687–708. [Google Scholar] [CrossRef] [Green Version]
- Rosen, M.; Dhawan, A.; AS, S. Inflammatory Bowel Disease in Children and Adolescents. JAMA Pediatr. 2015, 169, 1053–1060. [Google Scholar] [CrossRef] [Green Version]
- Henker, J.; Müller, S.; Laass, M.W.; Schreiner, A.; Schulze, J. Probiotic Escherichia coli Nissle 1917 (EcN) for Successful Remission Maintenance of Ulcerative Colitis in Children and Adolescents: An Open-Label Pilot Study. Z. Gastroenterol. 2008, 46, 874–875. [Google Scholar] [CrossRef]
- Scaldaferri, F.; Gerardi, V.; Mangiola, F.; Lopetuso, L.R.; Pizzoferrato, M.; Petito, V.; Papa, A.; Stojanovic, J.; Poscia, A.; Cammarota, G.; et al. Role and Mechanisms of Action of Escherichia coli Nissle 1917 in the Maintenance of Remission in Ulcerative Colitis Patients: An Update. World J. Gastroenterol. 2016, 22, 5505–5511. [Google Scholar] [CrossRef]
- Petersen, A.M.; Mirsepasi, H.; Halkjær, S.I.; Mortensen, E.M.; Nordgaard-Lassen, I.; Krogfelt, K.A. Ciprofloxacin and Probiotic Escherichia coli Nissle Add-on Treatment in Active Ulcerative Colitis: A Double-Blind Randomized Placebo Controlled Clinical Trial. J. Crohn’s Colitis 2014, 8, 1498–1505. [Google Scholar] [CrossRef]
- Miele, E.; Pascarella, F.; Giannetti, E.; Quaglietta, L.; Baldassano, R.N.; Staiano, A. Effect of a Probiotic Preparation (VSL#3) on Induction and Maintenance of Remission in Children with Ulcerative Colitis. Am. J. Gastroenterol. 2009, 104, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Huynh, H.Q.; deBruyn, J.; Guari, L.; Diaz, H.; Li, M.; Girgis, S.; Turner, J.; Fedorak, R.; Madsen, K. Probiotic Preparation VSL#3 Induces Remission in Children with Mild to Moderate Acute Ulcerative Colitis: A Pilot Study. Inflamm. Bowel Dis. 2009, 15, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Oliva, S.; Di Nardo, G.; Ferrari, F.; Mallardo, S.; Rossi, P.; Patrizi, G.; Cucchiara, S.; Stronati, L. Randomised Clinical Trial: The Effectiveness of Lactobacillus reuteri ATCC 55730 Rectal Enema in Children with Active Distal Ulcerative Colitis. Aliment. Pharmacol. Ther. 2012, 35, 327–334. [Google Scholar] [CrossRef]
- Iheozor-Ejiofor, Z.; Kaur, L.; Gordon, M.; Baines, P.A.; Sinopoulou, V.; Akobeng, A.K. Probiotics for Maintenance of Remission in Ulcerative Colitis. Cochrane Database Syst. Rev. 2020, 2020, CD007443. [Google Scholar] [CrossRef] [PubMed]
- Scarpato, E.; Russo, M.; Staiano, A. Probiotics in Pediatric Gastroenterology. Emerging Indications in Inflammatory Bowel Diseases. J. Clin. Gastroenterol. 2018, 52, S7–S9. [Google Scholar] [CrossRef]
- Bousvaros, A.; Guandalini, S.; Baldassano, R.N.; Botelho, C.; Evans, J.; Ferry, G.D.; Goldin, B.; Hartigan, L.; Kugathasan, S.; Levy, J.; et al. A Randomized, Double-Blind Trial of Lactobacillus GG versus Placebo in Addition to Standard Maintenance Therapy for Children with Crohn’s Disease. Inflamm. Bowel Dis. 2005, 11, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Ran, H.Z.; Yin, M.H.; Zhou, T.X.; Xiao, D.S. Meta-Analysis: The Effect and Adverse Events of Lactobacilli versus Placebo in Maintenance Therapy for Crohn Disease. Intern. Med. J. 2009, 39, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Guslandi, M.; Mezzi, G.; Sorghi, M.; Testoni, P.A. Saccharomyces boulardii in Maintenance Treatment of Crohn’s Disease. Dig. Dis. Sci. 2000, 45, 1462–1464. [Google Scholar] [CrossRef]
- Bourreille, A.; Cadiot, G.; Le Dreau, G.; Laharie, D.; Beaugerie, L.; Dupas, J.L.; Marteau, P.; Rampal, P.; Moyse, D.; Saleh, A.; et al. Saccharomyces boulardii Does Not Prevent Relapse of Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2013, 11, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Sivananthan, K.; Petersen, A.M. Review of Saccharomyces boulardii as a Treatment Option in IBD. Immunopharmacol. Immunotoxicol. 2018, 40, 465–475. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori Infection-the Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Huang, X.L.; Sui, J.Z.; Chen, S.Y.; Xie, Y.T.; Deng, Y.; Wang, J.; Xie, L.; Li, T.J.; He, Y.; et al. Meta-Analysis of Randomized Controlled Trials on the Efficacy of Probiotics in Helicobacter pylori Eradication Therapy in Children. Eur. J. Pediatr. 2014, 173, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.R.; Zhang, G.Q.; Cheng, J.Y.; Li, Z.Y. Efficacy of Lactobacillus-Supplemented Triple Therapy for Helicobacter pylori Infection in Children: A Meta-Analysis of Randomized Controlled Trials. Eur. J. Pediatr. 2019, 178, 7–16. [Google Scholar] [CrossRef]
- Szajewska, H.; Horvath, A.; Kołodziej, M. Systematic Review with Meta-Analysis: Saccharomyces boulardii Supplementation and Eradication of Helicobacter pylori Infection. Aliment. Pharmacol. Ther. 2015, 41, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Gomella, T.; Cunningham, M.; Eyal, F. Neonatology: Management, Procedures, On-Call Problems, Diseases, and Drugs, 7th ed.; McGraw-Hill Medical Books: New York, NY, USA, 2013. [Google Scholar]
- Neu, J.; Walker, W. Necrotizing Enterocolitis. N. Engl. J. Med. 2011, 364, 255–264. [Google Scholar] [CrossRef] [Green Version]
- Berrington, J.E.; Hearn, R.I.; Bythell, M.; Wright, C.; Embleton, N.D. Deaths in Preterm Infants: Changing Pathology over 2 Decades. J. Pediatr. 2012, 160, 49–53.e1. [Google Scholar] [CrossRef]
- Berrington, J.E.; Stewart, C.J.; Cummings, S.P.; Embleton, N.D. The Neonatal Bowel Microbiome in Health and Infection. Curr. Opin. Infect. Dis. 2014, 27, 236–243. [Google Scholar] [CrossRef]
- Morrow, A.L.; Lagomarcino, A.J.; Schibler, K.R.; Taft, D.H.; Yu, Z.; Wang, B.; Altaye, M.; Wagner, M.; Gevers, D.; Ward, D.V.; et al. Early Microbial and Metabolomic Signatures Predict Later Onset of Necrotizing Enterocolitis in Preterm Infants. Microbiome 2013, 1, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Van Den Akker, C.H.P.; Van Goudoever, J.B.; Szajewska, H.; Embleton, N.D.; Hojsak, I.; Reid, D.; Shamir, R. Probiotics for Preterm Infants: A Strain-Specific Systematic Review and Network Meta-Analysis. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 103–122. [Google Scholar] [CrossRef]
- Morgan, R.L.; Preidis, G.A.; Kashyap, P.C.; Weizman, A.V.; Sadeghirad, B.; Chang, Y.; Florez, I.D.; Foroutan, F.; Shahid, S.; Zeraatkar, D. Probiotics Reduce Mortality and Morbidity in Preterm, Low-Birth-Weight Infants: A Systematic Review and Network Meta-Analysis of Randomized Trials. Gastroenterology 2020, 159, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Sharif, S.; Meader, N.; Oddie, S.; Rojas-Reyes, M.; McGuire, W. Probiotics to Prevent Necrotising Enterocolitis in Very Preterm or Very Low Birth Weight Infants Infants. Cochrane Database Syst. Rev. 2020, 10, CD005496. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.; Bassler, D.; Darlow, B.A.; Lui, K.; Reichman, B.; Hakansson, S.; Norman, M.; Lee, S.K.; Helenius, K.K.; Lehtonen, L.; et al. Preventive Strategies and Factors Associated with Surgically Treated Necrotising Enterocolitis in Extremely Preterm Infants: An International Unit Survey Linked with Retrospective Cohort Data Analysis. BMJ Open 2019, 9, e031086. [Google Scholar] [CrossRef] [Green Version]
- Zbinden, A.; Zbinden, R.; Berger, C.; Arlettaz, R. Case Series of Bifidobacterium longum Bacteremia in Three Preterm Infants on Probiotic Therapy. Neonatology 2015, 107, 56–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunz, A.N.; Noel, J.M.; Fairchok, M.P. Two Cases of Lactobacillus Bacteremia During Probiotic Treatment of Short Gut Syndrome. J. Pediatr. Gastroenterol. Nutr. 2004, 38, 457–458. [Google Scholar] [CrossRef] [PubMed]
- Chiang, M.C.; Chen, C.L.; Feng, Y.; Chen, C.C.; Lien, R.; Chiu, C.H. Lactobacillus rhamnosus Sepsis Associated with Probiotic Therapy in an Extremely Preterm Infant: Pathogenesis and a Review for Clinicians. J. Microbiol. Immunol. Infect. 2020. [Google Scholar] [CrossRef]
- Martinelli, M.; Banderali, G.; Bobbio, M.; Civardi, E.; Chiara, A.; D’Elios, S.; Lo Vecchio, A.; Olivero, M.; Peroni, D.; Romano, C.; et al. Probiotics’ Efficacy in Paediatric Diseases: Which Is the Evidence? A Critical Review on Behalf of the Italian Society of Pediatrics. Ital. J. Pediatr. 2020, 46, 104, Erratum in 2020, 46, 116. [Google Scholar] [CrossRef] [PubMed]
- Seghesio, E.; De Geyter, C.; Vandenplas, Y. Probiotics in the Prevention and Treatment of Necrotizing Enterocolitis. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Akelma, A.Z.; Biten, A.A. Probiotics and Infantile Atopic Eczema. Pediatr. Health Med. Ther. 2015, 6, 147–151. [Google Scholar] [CrossRef] [Green Version]
- Cuello-Garcia, C.A.; Brozek, J.L.; Fiocchi, A.; Pawankar, R.; Yepes-Nuñez, J.J.; Terracciano, L.; Gandhi, S.; Agarwal, A.; Zhang, Y.; Schünemann, H.J. Probiotics for the Prevention of Allergy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Allergy Clin. Immunol. 2015, 136, 952–961. [Google Scholar] [CrossRef] [PubMed]
- Boyce, J.A. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel. J. Allergy Clin. Immunol. 2010, 126, S1–S58. [Google Scholar] [CrossRef]
- Muraro, A.; Halken, S.; Arshad, S.H.; Beyer, K.; Dubois, A.E.J.; Du Toit, G.; Eigenmann, P.A.; Grimshaw, K.E.C.; Hoest, A.; Lack, G.; et al. EAACI Food Allergy and Anaphylaxis Guidelines. Primary Prevention of Food Allergy. Allergy Eur. J. Allergy Clin. Immunol. 2014, 69, 590–601. [Google Scholar] [CrossRef]
- Szajewska, H.; Horvath, A. Lactobacillus rhamnosus GG in the Primary Prevention of Eczema in Children: A Systematic Review and Meta-Analysis. Nutrients 2018, 10, 1319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wickens, K.; Barthow, C.; Mitchell, E.A.; Stanley, T.V.; Purdie, G.; Rowden, J.; Kang, J.; Hood, F.; van den Elsen, L.; Forbes-Blom, E.; et al. Maternal Supplementation Alone with Lactobacillus rhamnosus HN001 during Pregnancy and Breastfeeding Does Not Reduce Infant Eczema. Pediatr. Allergy Immunol. 2018, 29, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Han, Z.; Niu, X.; Zhang, G.; Jia, Y.; Zhang, S.; He, C. Probiotic Supplementation for Prevention of Atopic Dermatitis in Infants and Children: A Systematic Review and Meta-Analysis. Am. J. Clin. Dermatol. 2019, 20, 367–377. [Google Scholar] [CrossRef] [PubMed]
- Makrgeorgou, A.; Leonardi-Bee, J.; Bath-hextall, F.; Murrell, D.; Tang, M.; Roberts, A.; Boyle, R. Probiotics for Treating Eczema. Cochrane Database Syst. Rev. 2018, 2018, CD006135. [Google Scholar] [CrossRef]
- Global Initiative on Asthma. Global Strategy for Asthma Management and Prevention: Socioeconomics. 2020. Available online: https://ginasthma.org/wp-content/uploads/2019/04/wmsGINA-2017-main-report-final_V2.pdf (accessed on 5 April 2021).
- Scadding, G.K.; Kariyawasam, H.H.; Scadding, G.; Mirakian, R.; Buckley, R.J.; Dixon, T.; Durham, S.R.; Farooque, S.; Jones, N.; Leech, S.; et al. BSACI Guideline for the Diagnosis and Management of Allergic and Non-Allergic Rhinitis (Revised Edition 2017; First Edition 2007). Clin. Exp. Allergy 2017, 47, 856–889. [Google Scholar] [CrossRef]
- Roberts, G.; Xatzipsalti, M.; Borrego, L.M.; Custovic, A.; Halken, S.; Hellings, P.W.; Papadopoulos, N.G.; Rotiroti, G.; Scadding, G.; Timmermans, F.; et al. Paediatric Rhinitis: Position Paper of the European Academy of Allergy and Clinical Immunology. Allergy Eur. J. Allergy Clin. Immunol. 2013, 68, 1102–1116. [Google Scholar] [CrossRef]
- Azad, M.B.; Coneys, G.J.; Kozyrskyj, A.L.; Field, C.J.; Ramsey, C.D.; Becker, A.B.; Friesen, C.; Abou-Setta, A.M.; Zarychanski, R. Probiotic Supplementation during Pregnancy or Infancy for the Prevention of Asthma and Wheeze: Systematic Review and Meta-Analysis. BMJ 2013, 347, f6471. [Google Scholar] [CrossRef] [Green Version]
- Wei, X.; Jiang, P.; Liu, J.; Sun, R.; Zhu, L. Association between Probiotic Supplementation and Asthma Incidence in Infants: A Meta-Analysis of Randomized Controlled Trials. J. Asthma 2020, 57, 167–178. [Google Scholar] [CrossRef]
- Spacova, I.; Petrova, M.I.; Fremau, A.; Pollaris, L.; Vanoirbeek, J.; Ceuppens, J.L.; Seys, S.; Lebeer, S. Intranasal Administration of Probiotic Lactobacillus rhamnosus GG Prevents Birch Pollen-Induced Allergic Asthma in a Murine Model. Allergy Eur. J. Allergy Clin. Immunol. 2019, 74, 100–110. [Google Scholar] [CrossRef]
- Feleszko, W.; Jaworska, J.; Rha, R.D.; Steinhausen, S.; Avagyan, A.; Jaudszus, A.; Ahrens, B.; Groneberg, D.A.; Wahn, U.; Hamelmann, E. Probiotic-Induced Suppression of Allergic Sensitization and Airway Inflammation Is Associated with an Increase of T Regulatory-Dependent Mechanisms in a Murine Model of Asthma. Clin. Exp. Allergy 2007, 37, 498–505. [Google Scholar] [CrossRef]
- Wickens, K.; Barthow, C.; Mitchell, E.A.; Kang, J.; van Zyl, N.; Purdie, G.; Stanley, T.; Fitzharris, P.; Murphy, R.; Crane, J. Effects of Lactobacillus rhamnosus HN001 in Early Life on the Cumulative Prevalence of Allergic Disease to 11 Years. Pediatr. Allergy Immunol. 2018, 29, 808–814. [Google Scholar] [CrossRef] [PubMed]
- Das, R.R.; Naik, S.S.; Singh, M. Probiotics as Additives on Therapy in Allergic Airway Diseases: A Systematic Review of Benefits and Risks. BioMed Res. Int. 2013, 2013, 231979. [Google Scholar] [CrossRef]
- Chen, Y.S.; Lin, Y.L.; Jan, R.L.; Chen, H.H.; Wang, J.Y. Randomized Placebo-Controlled Trial of Lactobacillus on Asthmatic Children with Allergic Rhinitis. Pediatr. Pulmonol. 2010, 45, 1111–1120. [Google Scholar] [CrossRef]
- Wu, C.T.; Chen, P.J.; Lee, Y.T.; Ko, J.L.; Lue, K.H. Effects of Immunomodulatory Supplementation with Lactobacillus rhamnosus on Airway Inflammation in a Mouse Asthma Model. J. Microbiol. Immunol. Infect. 2016, 49, 625–635. [Google Scholar] [CrossRef] [Green Version]
- Peng, Y.; Li, A.; Yu, L.; Qin, G. The Role of Probiotics in Prevention and Treatment for Patients with Allergic Rhinitis: A Systematic Review. Am. J. Rhinol. Allergy 2015, 29, 292–298. [Google Scholar] [CrossRef]
- Du, X.; Wang, L.; Wu, S.; Yuan, L.; Tang, S.; Xiang, Y.; Qu, X.; Liu, H.; Qin, X.; Liu, C. Efficacy of Probiotic Supplementary Therapy for Asthma, Allergic Rhinitis, and Wheeze: A Meta-Analysis of Randomized Controlled Trials. Allergy Asthma Proc. 2019, 40, 250–260. [Google Scholar] [CrossRef]
- Dimitri-Pinheiro, S.; Soares, R.; Barata, P. The Microbiome of the Nose—Friend or Foe? Allergy Rhinol. 2020, 11, 2152656720911605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranjan Das, R.; Singh, M.; Shafiq, N. Probiotics in Treatment of Allergic Rhinitis. World Allergy Organ. J. 2010, 3, 239–244. [Google Scholar] [CrossRef] [Green Version]
- Zajac, A.E.; Adams, A.S.; Turner, J.H. A Systematic Review and Meta-Analysis of Probiotics for the Treatment of Allergic Rhinitis. Int. Forum Allergy Rhinol. 2015, 5, 524–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishida, Y.; Nakamura, F.; Kanzato, H.; Sawada, D.; Hirata, H.; Nishimura, A.; Kajimoto, O.; Fujiwara, S. Clinical Effects of Lactobacillus acidophilus Strain L-92 on Perennial Allergic Rhinitis: A Double-Blind, Placebo-Controlled Study. J. Dairy Sci. 2005, 88, 527–533. [Google Scholar] [CrossRef] [Green Version]
- Lin, W.Y.; Fu, L.S.; Lin, H.K.; Shen, C.Y.; Chen, Y.J. Evaluation of the Effect of Lactobacillus paracasei (HF.A00232) in Children (6–13 Years Old) with Perennial Allergic Rhinitis: A 12-Week, Double-Blind, Randomized, Placebo-Controlled Study. Pediatr. Neonatol. 2014, 55, 181–188. [Google Scholar] [CrossRef] [Green Version]
- Jalali, M.M.; Soleimani, R.; Alavi Foumani, A.; Ganjeh Khosravi, H. Add-on Probiotics in Patients with Persistent Allergic Rhinitis: A Randomized Crossover Clinical Trial. Laryngoscope 2019, 129, 1744–1750. [Google Scholar] [CrossRef] [PubMed]
- Jerzynska, J.; Stelmach, W.; Balcerak, J.; Woicka-Kolejwa, K.; Rychlik, B.; Blauz, A.; Wachulec, M.; Stelmach, P.; Majak, P.; Stelmach, I. Effect of Lactobacillus rhamnosus GG and Vitamin D Supplementation on the Immunologic Effectiveness of Grass-Specific Sublingual Immunotherapy in Children with Allergy. Allergy Asthma Proc. 2016, 37, 324–334. [Google Scholar] [CrossRef] [PubMed]
- Meirlaen, L.; Levy, E.; Vandenplas, Y. Prevention and Management with Pro-,Pre and Synbiotics in Children with Asthma and Allergic Rhinitis: A Narrative Review. Nutrients 2021, 13, 934. [Google Scholar] [CrossRef] [PubMed]
| Population | Infant Child | |
|---|---|---|
| Intervention | Probiotic therapy | |
| Comparison | Placebo | |
| Probiotic therapy | ||
| Standard treatment | ||
| Outcome | AGE | IBD |
| AAD and CDAD | H. pylori | |
| Nosocomial diarrhea | NEC | |
| Infantile colic | LOS | |
| Regurgitation | Atopic dermatitis | |
| IBS | Asthma | |
| Constipation | Allergic rhinitis | |
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Allen et al., 2010 Cochrane Review [17] | 8014 (6489/352/1173) | L. rhamnosus GG ATCC53103 S. boulardii CNCM I-745 Enterococcus LAB | NA | ↓ duration of diarrhea +/− 25 h |
| Szajewska et al., 2014 ESPGHAN guidelines [18] | NA | L. rhamnosus GG ATCC53103 S. boulardii CNCM I-745 | ≥1010 CFU/d, 5–7 d 250–750 mg/d, 5–7 d | ↓ duration of diarrhea |
| Szajewska et al., 2020 ESPGHAN guidelines [11] | NA | L. reuteri DSM 17938 L. rhamnosus 19070-2 and L. reuteri DSM 2246 | 1 × 108–4 × 108 CFU, 5–7 d 1010 CFU 2×/d, 5 d | ↓ duration of diarrhea |
| Collinson et al., 2020 Cochrane Review [23] | 12,127 (11,526/412/189) | Several | NA | Uncertain effect |
| Su et al., 2020 AGA guidelines [7] | NA | Several | NA | Recommendation against use of probiotics |
| Vassilipoulou et al., 2021 [24] | 3469 (3469/0/0) | Several | Several | No sufficient clinical impact |
| In summary: Recent reviews conclude there is insufficient evidence to recommend the systematic administration of probiotics to prevent AGE, although—as listed in the Table above—many meta-analyses and systematic reviews recommend some specific strains. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Szajewska et al., 2016 ESPGHAN guidelines [33] | NA | L. rhamnosus GG ATCC 53103 S. boulardii CNCM I-745 | Uncertain >250 mg and <500 mg | ↓ incidence of AAD |
| Guo Q et al., 2019 Cochrane review [30] | 6352 (6352/0/0) | L. rhamnosus GG ATCC 53103 and S. boulardii CNCM I-745 | 5–40 × 109 CFU/d for the duration of antibiotic treatment | ↓ incidence of AAD |
| Ma et al., 2020 [31] | 4692 (NA) | L. casei | 50–100 × 1010 CFU/d | ↓ incidence of AAD |
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Szajewska et al., 2016 ESPGHAN guidelines [33] | NA | S. boulardii CNCM I-745 | >250 mg and <500 mg in children | ↓ risk of CDAD |
| Goldenberg et al., 2017 Cochrane Review [35] | 9955 (1114/7036/1805) | Several | NA | ↓ risk of CDAD |
| Su et al., 2020 AGA guidelines [7] | NA | Several, but also S. boulardii CNCM I-745 | NA | ↓ risk of CDAD |
| In summary: There is soms evidence for S. boulardii CNCM I-745 to reduce the risk of CDAD. | ||||
| N° Patients (Children/Adults/NS) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Szajewska et al., 2011 [26] | 1092 (1092/0/0) | L. rhamnosus GG ATCC 53103 | at least 109 CFU/d | ↓ risk of nosocomial diarrhea |
| Hojsak et al., 2018 ESPGHAN guidelines [37] | NA | L. rhamnosus GG ATCC 53103 | at least 109 CFU/d for the duration of hospital stay | ↓ risk of nosocomial diarrhea |
| In summary: There is evidence for L. rhamnosus GG ATCC53103to reduce the risk of nosocomial diarrhea | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Harb et al., 2016 [45] | NA | L. reuteri DSM 17938 | NA | Effective against colic in breastfed infants |
| Schreck et al., 2017 [46] | NA | L. reuteri DSM 17938 | 108 CFU/d 21 to 28 days | Effective against colic in breastfed infants |
| Sung et al., 2018 [44] | 345 (345/0/0) | L. reuteri DSM 17938 | 0.2 × 108 CFU/drop, 5 drops orally/d | Effective against colic in breastfed infants |
| Ong et al., 2019 Cochrane Review [43] | NA | L. reuteri DSM 17938 | NA | Probably effective against colic in children |
| Simonson et al., 2020 [47] | NA | Several, but recommending L. reuteri DSM 17938 | NA | Probably effective against colic in children |
| In summary: L. reuteri DSM 17938 reduces infant colic in breastfed infants.; however, no recommendation can be made in formula fed infants. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Indrio et al., 2011 [59] | 42 (42/0/0) | L. reuteri DSM 17938 | 108 CFU/d for 30 d | ↓ daily regurgitation |
| Garofoli et al., 2014 [57] | 40 (40/0/0) | L. reuteri DSM 17938 | 108 CFU/d = 5 drops/d for 28 d | ↓ daily regurgitation |
| Indrio et al., 2014 [58] | 589 (589/0/0) | L. reuteri SM 17938 | 108 CFU/d = 5 drops/d for 90 d | ↓ daily regurgitation (prevention) |
| Vandenplas et al., 2017 [60] | 280 (280/0/0) | Bifidobqcterium lactis | 107 CFU/g powder | ↓ daily regurgitation |
| In summary: Although there is some data suggesting benefit of L. reuteri DSM 17938, the evidence is insufficient to recommend the routine administration of this probiotic in the prevention or managament of regurgitation. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Guandalini et al., 2010 [68] | 59 (59/0/0) | VSL#3® | NA, 6 weeks | Improves relief of symptoms |
| Horvath et al., 2011 [66] | 290 (NA) | L. rhamnosus GG ATCC 5 3103 | 1 × 109–3 × 109 2×/d for at least 4 weeks | Significant higher rate of treatment responders |
| Pärrty et al., 2018 [63] | NA | L. reuteri DSM 17938 | NA | Conflicting results |
| In summary: There are insufficient data to recommend routine administration of probiotic strains in the management of IBS. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Tabbers et al., 2014 ESPGHAN & NASPGHAN guidelines [75] | NA | Several | Several | No significant effects |
| Koppen et al., 2016 [73] | 424 (424/0/0) | Several | Several | No significant effects |
| Huang et al., 2017 [72] | 49 (NA) | Several | Several | ↑ Stool frequency |
| Wojtyniak et al., 2017 [74] | 515 (515/0/0) | Several | Several | No significant effects |
| In summary: No meta-analysis or guideline recommends the administration of a specific strain in the management of functional constipation. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Miele et al., 2018 [76] ESPGHAN position paper | NA | L. reuteri ATCC 55730 VSL#3® | NA | Limited evidence of benefit |
| Iheozor-Ejiofor et al., 2020 [84] Cochrane Review | 1473 (NA, mainly adults) | Several | NA | Uncertain benefit |
| In summary: There is insufficient evidence to recommend probiotics in ulcerative colitis. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Sivanthan et al., 2018 [90] | NA | S. boulardii | NA | No significant effects |
| Miele et al., 2018 [76] ESPGHAN position paper | NA | Several | NA | No recommendation |
| In summary: There is insufficient evidence to recommend probiotics in Crohns’ disease. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Li et al., 2013 [92] | 508 (508/0/0) | Several | Several | ↑ eradication rate ↓ side effects |
| Malfertheiner et al., 2016 Maastricht V consensus report [91] | NA | Several Lactobacillus strains S. boulardii | NA | ↓ side effects |
| In summary: There is insufficient evidence to recommend probiotics in H. pylori. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| van den Akker et al., 2018 [100] | 11,231 (11,231/0/0) | Several (see text) | Several | ↓ incidence and mortality |
| Morgan et al., 2020 [101] | 15,712 (15,712/0/0) | Several (see text) | Several | ↓ NEC development |
| Sharif et al., 2020 Cochrane Review [102] | 10,812 (10,812/0/0) | Several (see text) | Several | ↓ NEC, mortality and late-onset invasive infections |
| In summary: Systematic administration of probiotic bacteria to prevent NEC is still debated in literature; therefore routine administration cannot be recommended. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Muraro et al., 2014 EAACI guidelines [112] | NA | NA | NA | No efficacy in prevention |
| Cuello-Garcia et al., 2015 [110] | 3447 (3447/0/0) | Several (see text) | Several | ↓ risk of eczema |
| Makrgeorgou et al., 2018 Cochrane Review [116] | 2599 (NA) | Several (see text) | Several | Little or no difference in eczema symptoms |
| Szajewska et al., 2018 [113] | 889 (NA) | L. rhamnosus GG ATCC 53103 | Several | No efficacy in prevention |
| Li et al., 2019 [115] | 3595 (3595/0/0) | Several | Several | Prevention of atopic dermatitis |
| In summary: Insufficient evidence to recommend routine use of probiotics in the treatment of atopic dermatitis; L. rhamnonsus GG ATCC 53103 can be considered. | ||||
| N° Patients (Children/Adults/NA) | Probiotic | Dose and Duration | Outcome | |
|---|---|---|---|---|
| Ranjan et al., 2010 [131] | 610 (357/253/0) | Several (see text) | Several | ↑ Quality of life ↓ Episodes of rhinitis/year |
| Azad et al., 2013 [120] | 3257 (3257/0/0) | Several (see text) | Several | No protection against asthma or childhood wheeze |
| Das et al., 2013 [125] | 899 (571/292/36) | Several (see text) | Several | ↑ time between episodes of rhinitis and asthma. No improvement in quality of life. |
| Peng et al., 2015 [128] | NA | Several (see text) | Several | No prevention of allergic rhinits |
| Du et al., 2019 [129] | 5264 (5264/0/0) | Several (see text), L. rhamnosus GG | Several | Prevention of asthma |
| Wei et al., 2020 [121] | 5717 (5717/0/0) | Several (see text) | Several | No protection against asthma or childhood wheeze |
| In summary: No evidence to recommend probiotics to prevent asthma and allergic rhinitis; none of the reviews recommends specific strains. | ||||
| Conditions | Strains | Dose | Recommended |
|---|---|---|---|
| Acute gastro-enteritis Treatment | S. boulardii CNCM I-745 | 250–750 mg/day, for 5–7 days | ? |
| L. rhamnosus GG ATCC53103 | minimal dose of 1010 CFU/ day, for 5–7 days | ? | |
| L. reuteri DSM 17938 | 1–4 × 108 CFU/day, for 5–7 days | ? | |
| L. rhamnosus 19070-2 and L. reuteri DSM 12246 | 1010 CFU of each strain twice daily, for 5 days | ? | |
| Acute gastro-enteritis Prevention | L. reuteri DSM17938 | 108 CFU/day | ? |
| Antibiotic-associated diarrhea Prevention | L. rhamnosus GG ATCC53103 | 5–40 × 109 CFU/day, for the duration of antibiotic treatment | + |
| S. boulardii CNCM I-745 | >250 mg and <500 mg | + | |
| L. casei | 50–100 × 1010 CFU/day | +/− | |
| C. difficile associated diarrhea Prevention | S. boulardii CNCM I-745 | >250 mg and <500 mg in children | + |
| Nosocomial diarrhea Prevention | L. rhamnosus GG ATCC53103 | >109 CFU/day, for the duration of hospital stay | + |
| Infantile colic Prevention and Treatment | L. reuteri DSM 17938 | 108 CFU/day, for 21–28 days | + in breastfed No in formula fed |
| Regurgitation Prevention and Treatment | L. reuteri DSM 17938 | 108 CFU/day, for at least 30 days | No |
| Irritable Bowel Syndrome Treatment | L. rhamnosus GG ATCC53103 | 1–3 × 109 2×/day, for at least 4 weeks | ? |
| VSL#3® | NA, at least 6 weeks | No | |
| Constipation Treatment | No significant effect of probiotics. | No | |
| Ulcerative Colitis Treatment | L. reuteri ATCC 55730 | NA | No |
| VSL#3® | NA | No | |
| Crohn’s Disease Treatment | No significant effect of probiotics. | No | |
| H. pylori Treatment | Lactobacilli (acidophilus, rhamnosus GG ATCC53103, reuteri DSM 17938, L. casei) | NA | No |
| S. boulardii CNCM I-745 | NA | No | |
| NEC and Late-onset sepsis Treatment | L. rhamnosus GG ATCC53103 | NA | ? |
| The combination of B. infantis Bb-02, B. lactis Bb-12 and Streptococcus thermophilus TH-4 | NA | ? | |
| Atopic Dermatitis Prevention and Treatment | L. rhamnosus GG ATCC53103 | NA | No |
| Asthma and Allergic rhinitis Prevention and Treatment | No significant effect of probiotics | No | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Depoorter, L.; Vandenplas, Y. Probiotics in Pediatrics. A Review and Practical Guide. Nutrients 2021, 13, 2176. https://doi.org/10.3390/nu13072176
Depoorter L, Vandenplas Y. Probiotics in Pediatrics. A Review and Practical Guide. Nutrients. 2021; 13(7):2176. https://doi.org/10.3390/nu13072176
Chicago/Turabian StyleDepoorter, Leontien, and Yvan Vandenplas. 2021. "Probiotics in Pediatrics. A Review and Practical Guide" Nutrients 13, no. 7: 2176. https://doi.org/10.3390/nu13072176