Prognostic Value of Magnesium in COVID-19: Findings from the COMEPA Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Exposure: Serum Mg Levels
2.3. Outcomes
2.4. Covariates
2.5. Statistical Analyses
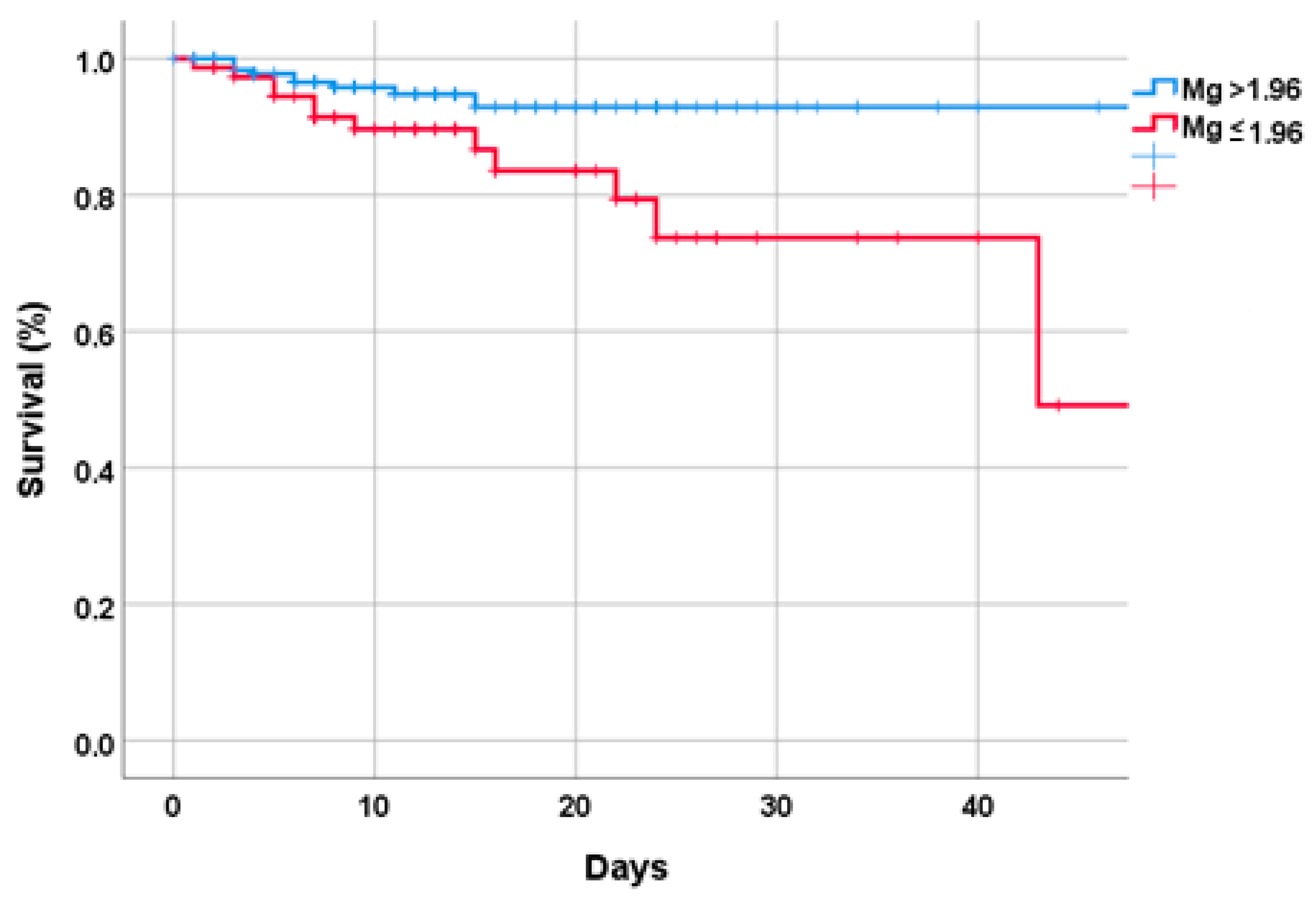
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Faryadi, Q. The magnificent effect of magnesium to human health: A critical review. Int. J. Appl. 2012, 2, 118–126. [Google Scholar]
- Caspi, R.; Altman, T.; Billington, R.; Dreher, K.; Foerster, H.; Fulcher, C.A.; Holland, T.A.; Keseler, I.M.; Kothari, A.; Kubo, A. The MetaCyc database of metabolic pathways and enzymes and the BioCyc collection of Pathway/Genome Databases. Nucleic Acids Res. 2014, 42, D459–D471. [Google Scholar] [CrossRef] [PubMed]
- Saris, N.-E.L.; Mervaala, E.; Karppanen, H.; Khawaja, J.A.; Lewenstam, A. Magnesium: An update on physiological, clinical and analytical aspects. Clin. Chim. Acta 2000, 294, 1–26. [Google Scholar] [CrossRef] [PubMed]
- Barbagallo, M.; Gupta, R.K.; Dominguez, L.J.; Resnick, L.M. Cellular ionic alterations with age: Relation to hypertension and diabetes. J. Am. Geriatr. Soc. 2000, 48, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Veronese, N.; Guerrero-Romero, F.; Barbagallo, M. Magnesium in infectious diseases in older people. Nutrients 2021, 13, 180. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J.; Galioto, A.; Ferlisi, A.; Cani, C.; Malfa, L.; Pineo, A.; Paolisso, G. Role of magnesium in insulin action, diabetes and cardio-metabolic syndrome X. Mol. Asp. Med. 2003, 24, 39–52. [Google Scholar] [CrossRef]
- Gröber, U.; Schmidt, J.; Kisters, K. Magnesium in prevention and therapy. Nutrients 2015, 7, 8199–8226. [Google Scholar] [CrossRef]
- Whang, R. Magnesium deficiency: Pathogenesis, prevalence, and clinical implications. Am. J. Med. 1987, 82, 24–29. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L. Magnesium and aging. Curr. Pharm. Des. 2010, 16, 832–839. [Google Scholar] [CrossRef]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Type 2 Diabetes Mellitus, Obesity, and Metabolic Syndrome. Nutrients 2022, 14, 714. [Google Scholar] [CrossRef]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in aging, health and diseases. Nutrients 2021, 13, 463. [Google Scholar] [CrossRef]
- World Health Organization. Available online: www.who.int/ageing/events/world-report-2015-launch/en (accessed on 10 January 2023).
- Zhang, J.-J.; Dong, X.; Liu, G.-H.; Gao, Y.-D. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin. Rev. Allergy Immunol. 2022, 64, 90–107. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.; Kohli, S.; Devi, A.; Mahajan, S. Serum magnesium level in COPD patients attending a tertiary hospital—A cross sectional study. JK Sci. 2012, 14, 185. [Google Scholar]
- Barbagallo, M.; Belvedere, M.; Dominguez, L.J. Magnesium homeostasis and aging. Magnes. Res. 2009, 22, 235. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.P.; Khandelwal, P.; Nanda, S.; Stoltzfus, J.C.; Fioravanti, G.T. Serum magnesium is an independent predictor of frequent readmissions due to acute exacerbation of chronic obstructive pulmonary disease. Respir. Med. 2008, 102, 999–1003. [Google Scholar] [CrossRef] [PubMed]
- Nasser, R.; Naffaa, M.E.; Mashiach, T.; Azzam, Z.S.; Braun, E. The association between serum magnesium levels and community-acquired pneumonia 30-day mortality. BMC Infect. Dis. 2018, 18, 698. [Google Scholar] [CrossRef]
- Lee, S.-H.; Song, W.-J.; Park, H.-W.; Kim, S.-H.; Park, H.-K.; Kim, S.-H.; Kwon, Y.E.; Kim, T.-B.; Lee, B.-J.; Jee, Y.-K. Serum micronutrients levels and clinical features of elderly asthmatics. Allergy Asthma Respir. Dis. 2017, 5, 223–227. [Google Scholar] [CrossRef]
- Veronese, N.; Demurtas, J.; Pesolillo, G.; Celotto, S.; Barnini, T.; Calusi, G.; Caruso, M.G.; Notarnicola, M.; Reddavide, R.; Stubbs, B. Magnesium and health outcomes: An umbrella review of systematic reviews and meta-analyses of observational and intervention studies. Eur. J. Nutr. 2020, 59, 263–272. [Google Scholar] [CrossRef]
- Emelyanov, A.; Fedoseev, G.; Barnes, P. Reduced intracellular magnesium concentrations in asthmatic patients. Eur. Respir. J. 1999, 13, 38–40. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Barbagallo, M.; Lorenzo, G.D.; Drago, A.; Scola, S.; Morici, G.; Caruso, C. Bronchial reactivity and intracellular magnesium: A possible mechanism for the bronchodilating effects of magnesium in asthma. Clin. Sci. 1998, 95, 137–142. [Google Scholar] [CrossRef]
- Tam, M.; Gomez, S.; Gonzalez-Gross, M.; Marcos, A. Possible roles of magnesium on the immune system. Eur. J. Clin. Nutr. 2003, 57, 1193–1197. [Google Scholar] [CrossRef] [PubMed]
- Charoenngam, N.; Holick, M.F. Immunologic effects of vitamin D on human health and disease. Nutrients 2020, 12, 2097. [Google Scholar] [CrossRef] [PubMed]
- Uwitonze, A.M.; Razzaque, M.S. Role of magnesium in vitamin D activation and function. J. Osteopath. Med. 2018, 118, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Zittermann, A. Magnesium deficit-overlooked cause of low vitamin D status? BMC Med. 2013, 11, 229. [Google Scholar] [CrossRef]
- Trapani, V.; Rosanoff, A.; Baniasadi, S.; Barbagallo, M.; Castiglioni, S.; Guerrero-Romero, F.; Iotti, S.; Mazur, A.; Micke, O.; Pourdowlat, G. The relevance of magnesium homeostasis in COVID-19. Eur. J. Nutr. 2021, 61, 625–636. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Mercado, M.; Rodriguez-Moran, M.; Ramírez-Renteria, C.; Martínez-Aguilar, G.; Marrero-Rodríguez, D.; Ferreira-Hermosillo, A.; Simental-Mendía, L.E.; Remba-Shapiro, I.; Gamboa-Gómez, C.I. Magnesium-to-Calcium Ratio and Mortality from COVID-19. Nutrients 2022, 14, 1686. [Google Scholar] [CrossRef]
- Tan, C.W.; Ho, L.P.; Kalimuddin, S.; Cherng, B.P.Z.; Teh, Y.E.; Thien, S.Y.; Wong, H.M.; Tern, P.J.W.; Chandran, M.; Chay, J.W.M. Cohort study to evaluate the effect of vitamin D, magnesium, and vitamin B12 in combination on progression to severe outcomes in older patients with coronavirus (COVID-19). Nutrition 2020, 79, 111017. [Google Scholar] [CrossRef]
- Zeng, H.L.; Yang, Q.; Yuan, P.; Wang, X.; Cheng, L. Associations of essential and toxic metals/metalloids in whole blood with both disease severity and mortality in patients with COVID-19. FASEB J. 2021, 35, e21392. [Google Scholar] [CrossRef]
- Pulido Perez, P.; Póndigo de Los Angeles, J.A.; Perez Peralta, A.; Ramirez Mojica, E.; Torres Rasgado, E.; Hernandez-Hernandez, M.E.; Romero, J.R. Reduction in Serum Magnesium Levels and Renal Function Are Associated with Increased Mortality in Obese COVID-19 Patients. Nutrients 2022, 14, 4054. [Google Scholar] [CrossRef]
- Veronese, N.; Bonica, R.; Cotugno, S.; Tulone, O.; Camporeale, M.; Smith, L.; Trott, M.; Bruyere, O.; Mirarchi, L.; Rizzo, G. Interventions for improving long COVID-19 symptomatology: A systematic review. Viruses 2022, 14, 1863. [Google Scholar] [CrossRef]
- Barbagallo, M.; Citarrella, R.; Dominguez, L.; Giannitrapani, L.; Licata, A.; Mansueto, P.; Soresi, M.; Veronese, N. COMEPA (COVID-19 Medicina Policlinico Palermo): A study in hospitalized patients. Geriatr. Care 2021, 7, 9895. [Google Scholar]
- Wynants, L.; Van Calster, B.; Collins, G.S.; Riley, R.D.; Heinze, G.; Schuit, E.; Bonten, M.M.; Dahly, D.L.; Damen, J.A.; Debray, T.P. Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal. Bmj 2020, 369, m1328. [Google Scholar] [CrossRef]
- World Health Organization. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post COVID-19 Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Stavem, K.; Ghanima, W.; Olsen, M.K.; Gilboe, H.M.; Einvik, G. Prevalence and determinants of fatigue after COVID-19 in non-hospitalized subjects: A population-based study. Int. J. Environ. Res. Public Health 2021, 18, 2030. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, A.; Shetty, A.; Delanerolle, G.; Zeng, Y.; Zhang, Y.; Raymont, V.; Rathod, S.; Halabi, S.; Elliot, K.; Phiri, P. A systematic review and meta-analysis of Long COVID symptoms. Medrxiv Prepr. Serv. Health Sci. 2022. [Google Scholar] [CrossRef]
- Han, Q.; Zheng, B.; Daines, L.; Sheikh, A. Long-Term sequelae of COVID-19: A systematic review and meta-analysis of one-year follow-up studies on post-COVID symptoms. Pathogens 2022, 11, 269. [Google Scholar] [CrossRef]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale: An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Covelli, H.D.; Nessan, V.J.; Tuttle, W., 3rd. Oxygen derived variables in acute respiratory failure. Crit. Care Med. 1983, 11, 646–649. [Google Scholar] [CrossRef] [PubMed]
- Linn, B.S.; Linn, M.W.; Gurel, L. Cumulative illness rating scale. J. Am. Geriatr. Soc. 1968, 16, 622–626. [Google Scholar] [CrossRef]
- Fluss, R.; Faraggi, D.; Reiser, B. Estimation of the Youden Index and its associated cutoff point. Biom. J. 2005, 47, 458–472. [Google Scholar] [CrossRef]
- Tian, J.; Tang, L.; Liu, X.; Li, Y.; Chen, J.; Huang, W.; Liu, M. Populations in Low-Magnesium Areas Were Associated with Higher Risk of Infection in COVID-19’s Early Transmission: A Nationwide Retrospective Cohort Study in the United States. Nutrients 2022, 14, 909. [Google Scholar] [CrossRef] [PubMed]
- Fajgenbaum, D.C.; June, C.H. Cytokine storm. N. Engl. J. Med. 2020, 383, 2255–2273. [Google Scholar] [CrossRef] [PubMed]
- Perrotta, F.; Corbi, G.; Mazzeo, G.; Boccia, M.; Aronne, L.; D’Agnano, V.; Komici, K.; Mazzarella, G.; Parrella, R.; Bianco, A. COVID-19 and the elderly: Insights into pathogenesis and clinical decision-making. Aging Clin. Exp. Res. 2020, 32, 1599–1608. [Google Scholar] [CrossRef] [PubMed]
- Kalinina, O.; Golovkin, A.; Zaikova, E.; Aquino, A.; Bezrukikh, V.; Melnik, O.; Vasilieva, E.; Karonova, T.; Kudryavtsev, I.; Shlyakhto, E. Cytokine Storm Signature in Patients with Moderate and Severe COVID-19. Int. J. Mol. Sci. 2022, 23, 8879. [Google Scholar] [CrossRef] [PubMed]
- Mazur, A.; Maier, J.A.; Rock, E.; Gueux, E.; Nowacki, W.; Rayssiguier, Y. Magnesium and the inflammatory response: Potential physiopathological implications. Arch. Biochem. Biophys. 2007, 458, 48–56. [Google Scholar] [CrossRef]
- Kramer, J.H.; Mak, I.T.; Phillips, T.M.; Weglicki, W.B. Dietary magnesium intake influences circulating pro-inflammatory neuropeptide levels and loss of myocardial tolerance to postischemic stress. Exp. Biol. Med. 2003, 228, 665–673. [Google Scholar] [CrossRef]
- Stankovic, M.S.; Janjetovic, K.; Velimirovic, M.; Milenkovic, M.; Stojkovic, T.; Puskas, N.; Zaletel, I.; De Luka, S.R.; Jankovic, S.; Stefanovic, S. Effects of IL-33/ST2 pathway in acute inflammation on tissue damage, antioxidative parameters, magnesium concentration and cytokines profile. Exp. Mol. Pathol. 2016, 101, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Malpuech-Brugère, C.; Nowacki, W.; Daveau, M.; Gueux, E.; Linard, C.; Rock, E.; Lebreton, J.-P.; Mazur, A.; Rayssiguier, Y. Inflammatory response following acute magnesium deficiency in the rat. Biochim. Et Biophys. Acta (BBA)-Mol. Basis Dis. 2000, 1501, 91–98. [Google Scholar] [CrossRef]
- King, D.E.; Mainous III, A.G.; Geesey, M.E.; Woolson, R.F. Dietary magnesium and C-reactive protein levels. J. Am. Coll. Nutr. 2005, 24, 166–171. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Bermudez-Peña, C.; Rodríguez-Morán, M. Severe hypomagnesemia and low-grade inflammation in metabolic syndrome. Magnes. Res. 2011, 24, 45–53. [Google Scholar] [CrossRef]
- Song, Y.; Li, T.Y.; Van Dam, R.M.; Manson, J.E.; Hu, F.B. Magnesium intake and plasma concentrations of markers of systemic inflammation and endothelial dysfunction in women. Am. J. Clin. Nutr. 2007, 85, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Ridker, P.M.; Manson, J.E.; Cook, N.R.; Buring, J.E.; Liu, S. Magnesium intake, C-reactive protein, and the prevalence of metabolic syndrome in middle-aged and older US women. Diabetes Care 2005, 28, 1438–1444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazidi, M.; Kengne, A.P.; Mikhailidis, D.P.; Cicero, A.F.; Banach, M. Effects of selected dietary constituents on high-sensitivity C-reactive protein levels in US adults. Ann. Med. 2018, 50, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Konstari, S.; Sares-Jäske, L.; Heliövaara, M.; Rissanen, H.; Knekt, P.; Arokoski, J.; Sundvall, J.; Karppinen, J. Dietary magnesium intake, serum high sensitivity C-reactive protein and the risk of incident knee osteoarthritis leading to hospitalization—A cohort study of 4,953 Finns. PLoS ONE 2019, 14, e0214064. [Google Scholar] [CrossRef] [PubMed]
- Su, N.-Y.; Peng, T.-C.; Tsai, P.-S.; Huang, C.-J. Phosphoinositide 3-kinase/Akt pathway is involved in mediating the anti-inflammation effects of magnesium sulfate. J. Surg. Res. 2013, 185, 726–732. [Google Scholar] [CrossRef]
- Lin, C.; Tsai, P.; Hung, Y.; Huang, C. L-type calcium channels are involved in mediating the anti-inflammatory effects of magnesium sulphate. Br. J. Anaesth. 2010, 104, 44–51. [Google Scholar] [CrossRef]
- Mazidi, M.; Rezaie, P.; Banach, M. Effect of magnesium supplements on serum C-reactive protein: A systematic review and meta-analysis. Arch. Med. Sci. 2018, 14, 707–716. [Google Scholar] [CrossRef]
- Altura, B.M.; Altura, B.T.; Gebrewold, A.; Ising, H.; Gunther, T. Magnesium deficiency and hypertension: Correlation between magnesium-deficient diets and microcirculatory changes in situ. Science 1984, 223, 1315–1317. [Google Scholar] [CrossRef]
- Iseri, L.T.; French, J.H. Magnesium: Natures physiologic calcium blocker. Am. Heart J. 1984, 108, 188–193. [Google Scholar] [CrossRef]
- Louvet, L.; Büchel, J.; Steppan, S.; Passlick-Deetjen, J.; Massy, Z.A. Magnesium prevents phosphate-induced calcification in human aortic vascular smooth muscle cells. Nephrol. Dial. Transplant. 2013, 28, 869–878. [Google Scholar] [CrossRef] [PubMed]
- Escuela, M.P.; Guerra, M.; Añón, J.M.; Martínez-Vizcaíno, V.; Zapatero, M.D.; García-Jalón, A.; Celaya, S. Total and ionized serum magnesium in critically ill patients. Intensive Care Med. 2005, 31, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Hansen, B.-A.; Bruserud, Ø. Hypomagnesemia in critically ill patients. J. Intensive Care 2018, 6, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iotti, S.; Wolf, F.; Mazur, A.; Maier, J. The COVID-19 pandemic: Is there a role for magnesium? Hypotheses and perspectives. Magnes. Res. 2020, 33, 21–27. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef]
- Libby, P.; Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 2020, 41, 3038–3044. [Google Scholar] [CrossRef] [PubMed]
- Evans, P.C.; Rainger, G.E.; Mason, J.C.; Guzik, T.J.; Osto, E.; Stamataki, Z.; Neil, D.; Hoefer, I.E.; Fragiadaki, M.; Waltenberger, J. Endothelial dysfunction in COVID-19: A position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc. Res. 2020, 116, 2177–2184. [Google Scholar] [CrossRef]
- Maier, J.A.; Malpuech-Brugère, C.; Zimowska, W.; Rayssiguier, Y.; Mazur, A. Low magnesium promotes endothelial cell dysfunction: Implications for atherosclerosis, inflammation and thrombosis. Biochim. Et Biophys. Acta (BBA)-Mol. Basis Dis. 2004, 1689, 13–21. [Google Scholar] [CrossRef]
- Barbagallo, M.; Dominguez, L.J.; Galioto, A.; Pineo, A.; Belvedere, M. Oral magnesium supplementation improves vascular function in elderly diabetic patients. Magnes. Res. 2010, 23, 131–137. [Google Scholar]
- Shechter, M.; Sharir, M.; Labrador, M.J.P.; Forrester, J.; Silver, B.; Bairey Merz, C.N. Oral magnesium therapy improves endothelial function in patients with coronary artery disease. Circulation 2000, 102, 2353–2358. [Google Scholar] [CrossRef]
- Marques, B.C.A.A.; Klein, M.R.S.T.; da Cunha, M.R.; de Souza Mattos, S.; de Paula Nogueira, L.; de Paula, T.; Corrêa, F.M.; Oigman, W.; Neves, M.F. Effects of oral magnesium supplementation on vascular function: A systematic review and meta-analysis of randomized controlled trials. High Blood Press. Cardiovasc. Prev. 2020, 27, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Galland, L. Magnesium and immune function: An overview. Magnesium 1988, 7, 290–299. [Google Scholar]
- Bernstein, H.; Sugimoto, J.; Suzuki-Kakisaka, H.; Romani, A. 823: Magnesium decreases inflammatory cytokine production: A novel innate immunomodulatory mechanism. Am. J. Obstet. Gynecol. 2012, 206, S361. [Google Scholar] [CrossRef]
- Feske, S.; Skolnik, E.Y.; Prakriya, M. Ion channels and transporters in lymphocyte function and immunity. Nat. Rev. Immunol. 2012, 12, 532–547. [Google Scholar] [CrossRef]
- Bussière, F.I.; Tridon, A.; Zimowska, W.; Mazur, A.; Rayssiguier, Y. Increase in complement component C3 is an early response to experimental magnesium deficiency in rats. Life Sci. 2003, 73, 499–507. [Google Scholar] [CrossRef]
- Kraeuter, S.L.; Schwartz, R. Blood and mast cell histamine levels in magnesium-deficient rats. J. Nutr. 1980, 110, 851–858. [Google Scholar] [CrossRef]
- TAkEMOTO, S.; Yamamoto, A.; Tomonaga, S.; Funaba, M.; Matsui, T. Magnesium deficiency induces the emergence of mast cells in the liver of rats. J. Nutr. Sci. Vitaminol. 2013, 59, 560–563. [Google Scholar] [CrossRef]
- Chien, M.M.; Zahradka, K.E.; Newell, M.K.; Freed, J.H. Fas-induced B cell apoptosis requires an increase in free cytosolic magnesium as an early event. J. Biol. Chem. 1999, 274, 7059–7066. [Google Scholar] [CrossRef] [PubMed]
- Bussière, F.; Gueux, E.; Rock, E.; Mazur, A.; Rayssiguier, Y. Protective effect of calcium deficiency on the inflammatory response in magnesium-deficient rats. Eur. J. Nutr. 2002, 41, 197–202. [Google Scholar] [CrossRef]
- Petrault, I.; Zimowska, W.; Mathieu, J.; Bayle, D.; Rock, E.; Favier, A.; Rayssiguier, Y.; Mazur, A. Changes in gene expression in rat thymocytes identified by cDNA array support the occurrence of oxidative stress in early magnesium deficiency. Biochim. Et Biophys. Acta (BBA)-Mol. Basis Dis. 2002, 1586, 92–98. [Google Scholar] [CrossRef]
- Zimowska, W.; Girardeau, J.; Kuryszko, J.; Bayle, D.; Rayssiguier, Y.; Mazur, A. Morphological and immune response alterations in the intestinal mucosa of the mouse after short periods on a low-magnesium diet. Br. J. Nutr. 2002, 88, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Li, F.-Y.; Chaigne-Delalande, B.; Kanellopoulou, C.; Davis, J.C.; Matthews, H.F.; Douek, D.C.; Cohen, J.I.; Uzel, G.; Su, H.C.; Lenardo, M.J. Second messenger role for Mg2+ revealed by human T-cell immunodeficiency. Nature 2011, 475, 471–476. [Google Scholar] [CrossRef]
- Chaigne-Delalande, B.; Li, F.-Y.; O’Connor, G.M.; Lukacs, M.J.; Jiang, P.; Zheng, L.; Shatzer, A.; Biancalana, M.; Pittaluga, S.; Matthews, H.F. Mg2+ regulates cytotoxic functions of NK and CD8 T cells in chronic EBV infection through NKG2D. Science 2013, 341, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Li, F.-Y.; Chaigne-Delalande, B.; Su, H.; Uzel, G.; Matthews, H.; Lenardo, M.J. XMEN disease: A new primary immunodeficiency affecting Mg2+ regulation of immunity against Epstein-Barr virus. Blood J. Am. Soc. Hematol. 2014, 123, 2148–2152. [Google Scholar] [CrossRef]
- Mason, R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur. Respiratory Soc. 2020, 55, 2000607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theoharides, T.C. COVID-19, pulmonary mast cells, cytokine storms, and beneficial actions of luteolin. Biofactors 2020, 46, 306–308. [Google Scholar] [CrossRef]
- Veronese, N.; Pizzol, D.; Smith, L.; Dominguez, L.J.; Barbagallo, M. Effect of Magnesium Supplementation on Inflammatory Parameters: A Meta-Analysis of Randomized Controlled Trials. Nutrients 2022, 14, 679. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Belati, A.; Tulone, O.; Diella, L.; Fiore Bavaro, D.; Bonica, R.; Genna, V.; Smith, L.; Trott, M.; Bruyere, O.; et al. Incidence of long COVID-19 in people with previous SARS-Cov2 infection: A systematic review and meta-analysis of 120,970 patients. Intern. Emerg. Med. 2022, 1–9. [Google Scholar] [CrossRef]
- Gushcha, S.; Oleshko, A.Y.; Bakholdina, E.; Badiuk, N.; Zabolotna, I. Correction of disturbances of functional activity of the central nervous system in rats with the post-traumatic stress disorder model using remedy with a high magnesium content. 2021, Volume 1, pp. 12–19. Available online: https://pharmacologyonline.silae.it/files/archives/2021/vol1/PhOL_2021_1_A003_Gushcha.pdf (accessed on 31 April 2021).

| Parameter | Serum Mg > 1.96 mg/dL (n = 186) | Serum Mg ≤ 1.96 mg/dL (n = 74) | p-Value |
|---|---|---|---|
| Demographics | |||
| Age (years) | 63.9 (15.7) | 69.1 (13.4) | 0.01 |
| Males (%) | 51.6 | 59.5 | 0.27 |
| Current smoking (%) | 12.1 | 9.8 | 0.80 |
| Alcohol abuse (%) | 6.1 | 10.4 | 0.34 |
| Laboratory parameters (1–4 days) | |||
| Creatinine clearance (mL/min) | 91.7 (32.0) | 87.8 (45.5) | 0.50 |
| Hemoglobin (g/dL) | 13.1 (1.9) | 11.6 (2.2) | <0.0001 |
| White blood cells (units/μL) | 7940 (4214) | 7212 (3264) | 0.14 |
| CRP (mg/mL) | 51.2 (48.9) | 60.0 (64.6) | 0.31 |
| IL-6 (pg/mL) | 36.4 (71.0) | 59.8 (136.1) | 0.19 |
| Procalcitonin (ng/mL) | 0.82 (6.84) | 0.43 (1.26) | 0.68 |
| PaO2/FiO2 ratio | 324 (104) | 344 (142) | 0.29 |
| Serum 25OHD (ng/mL) | 24 (19) | 23 (14) | 0.78 |
| AST (U/L) | 31 (25) | 26 (15) | 0.21 |
| ALT (U/L) | 37 (46) | 25 (19) | 0.003 |
| Fasting plasma glucose (mg/dL) | 131 (62) | 141 (71) | 0.29 |
| Na (mmol/L) | 139 (4) | 139 (4) | 0.88 |
| Ca++ (mmol/L) | 8.94 (0.93) | 8.95 (0.63) | 0.99 |
| K (mg/dL) | 4.38 (0.67) | 4.43 (0.58) | 0.10 |
| Albumin (g/L) | 3.57 (0.51) | 3.36 (0.47) | 0.002 |
| Clinical data | |||
| Any COVID-19 symptomatology (%) | 82.3 | 63.0 | 0.002 |
| CIRS-SI | 1.41 (1.42) | 2.74 (1.81) | <0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Carrubba, A.; Veronese, N.; Di Bella, G.; Cusumano, C.; Di Prazza, A.; Ciriminna, S.; Ganci, A.; Naro, L.; Dominguez, L.J.; Barbagallo, M.; et al. Prognostic Value of Magnesium in COVID-19: Findings from the COMEPA Study. Nutrients 2023, 15, 830. https://doi.org/10.3390/nu15040830
La Carrubba A, Veronese N, Di Bella G, Cusumano C, Di Prazza A, Ciriminna S, Ganci A, Naro L, Dominguez LJ, Barbagallo M, et al. Prognostic Value of Magnesium in COVID-19: Findings from the COMEPA Study. Nutrients. 2023; 15(4):830. https://doi.org/10.3390/nu15040830
Chicago/Turabian StyleLa Carrubba, Anna, Nicola Veronese, Giovanna Di Bella, Claudia Cusumano, Agnese Di Prazza, Stefano Ciriminna, Antonina Ganci, Liliana Naro, Ligia J. Dominguez, Mario Barbagallo, and et al. 2023. "Prognostic Value of Magnesium in COVID-19: Findings from the COMEPA Study" Nutrients 15, no. 4: 830. https://doi.org/10.3390/nu15040830






