Association between Micronutrients and Hyperhomocysteinemia: A Case-Control Study in Northeast China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Experimental Instruments and Reagents
2.3. Sample Collection, DNA Preparation, and MTHFR Genotyping
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Comparison of Hcy Concentration among Different Genotypes
3.3. Nutrient Differences among Participants
3.4. Associations between Zn and HHcy ORs
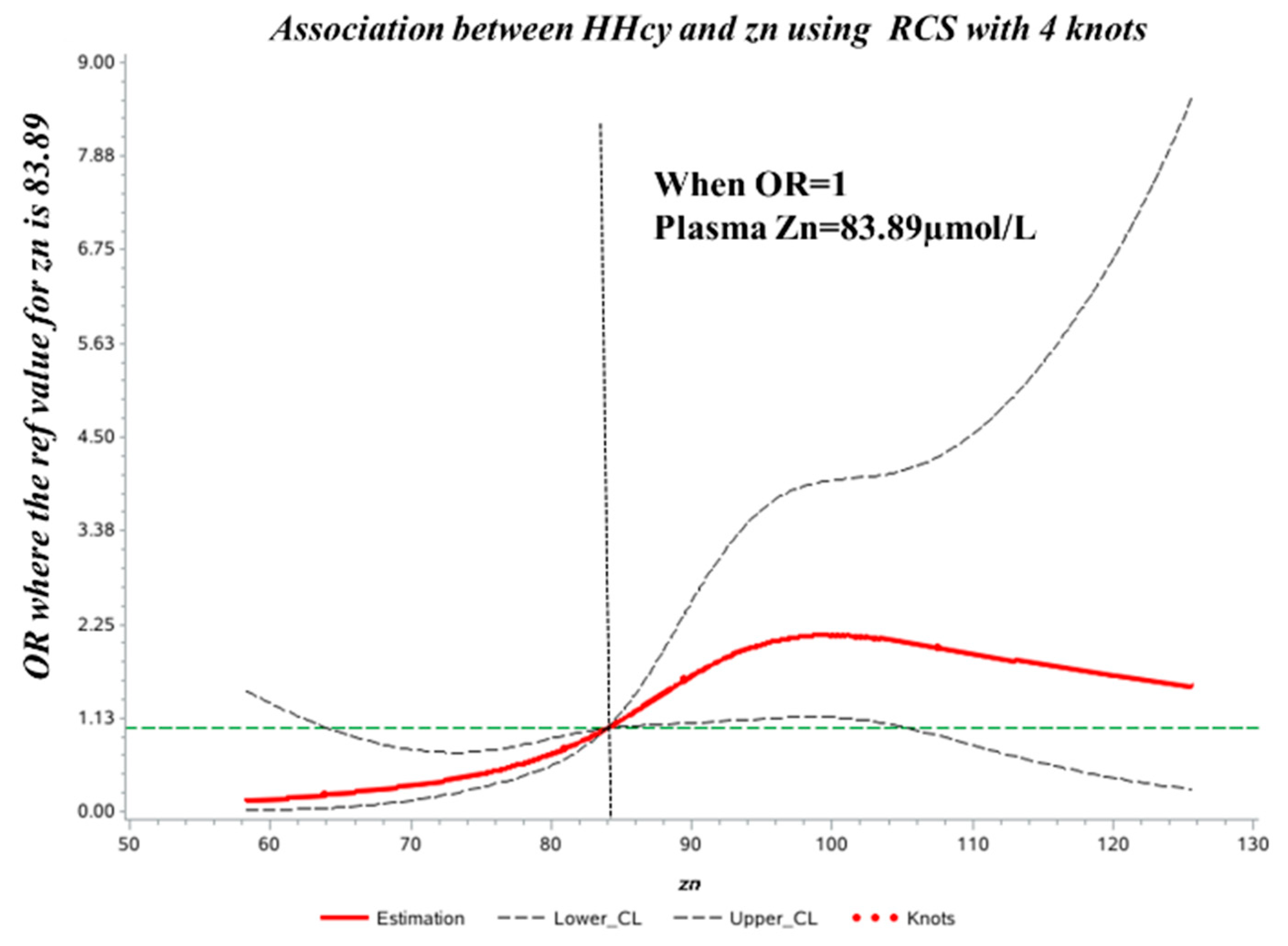
3.5. Dose–Response Association between Plasma Zn Level and HHcy Risk
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alam, S.F.; Kumar, S.; Ganguly, P. Measurement of homocysteine: A historical perspective. J. Clin. Biochem. Nutr. 2019, 65, 171–177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, Y.; Wang, X.; Kong, W. Hyperhomocysteinaemia and vascular injury: Advances in mechanisms and drug targets. Br. J. Pharmacol. 2018, 175, 1173–1189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fezeu, L.K.; Ducros, V.; Guéant, J.L.; Guilland, J.C.; Andreeva, V.A.; Hercberg, S.; Galan, P. MTHFR 677C → T genotype modulates the effect of a 5-year supplementation with B-vitamins on homocysteine concentration: The SU.FOL.OM3 randomized controlled trial. PLoS ONE 2018, 13, e0193352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaric, B.L.; Obradovic, M.; Bajic, V.; Haidara, M.A.; Jovanovic, M.; Isenovic, E.R. Homocysteine and Hyperhomocysteinaemia. Curr. Med. Chem. 2019, 26, 2948–2961. [Google Scholar] [CrossRef] [PubMed]
- Liew, S.C.; Gupta, E.D. Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: Epidemiology, metabolism and the associated diseases. Eur. J. Med. Genet. 2015, 58, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ventura, P.; Panini, R.; Verlato, C.; Scarpetta, G.; Salvioli, G. Hyperhomocysteinemia and related factors in 600 hospitalized elderly subjects. Metab. Clin. Exp. 2001, 50, 1466–1471. [Google Scholar] [CrossRef]
- Maron, B.A.; Loscalzo, J. The treatment of hyperhomocysteinemia. Annu. Rev. Med. 2009, 60, 39–54. [Google Scholar] [CrossRef] [Green Version]
- Xu, W.; Tan, L.; Wang, H.F.; Jiang, T.; Tan, M.S.; Tan, L.; Zhao, Q.F.; Li, J.Q.; Wang, J.; Yu, J.T. Meta-analysis of modifiable risk factors for Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry 2015, 86, 1299–1306. [Google Scholar] [CrossRef]
- Sakamoto, W.; Isomura, H.; Fujie, K.; Deyama, Y.; Kato, A.; Nishihira, J.; Izumi, H. Homocysteine attenuates the expression of osteocalcin but enhances osteopontin in MC3T3-E1 preosteoblastic cells. Biochim. Biophys. Acta 2005, 1740, 12–16. [Google Scholar] [CrossRef] [Green Version]
- Price, B.R.; Wilcock, D.M.; Weekman, E.M. Hyperhomocysteinemia as a Risk Factor for Vascular Contributions to Cognitive Impairment and Dementia. Front. Aging Neurosci. 2018, 10, 350. [Google Scholar] [CrossRef] [Green Version]
- Födinger, M.; Buchmayer, H.; Sunder-Plassmann, G. Molecular genetics of homocysteine metabolism. Miner. Electrolyte Metab. 1999, 25, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Locasale, J.W. Serine, glycine and one-carbon units: Cancer metabolism in full circle. Nat. Rev. Cancer 2013, 13, 572–583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frosst, P.; Blom, H.J.; Milos, R.; Goyette, P.; Sheppard, C.A.; Matthews, R.G.; Boers, G.J.; den Heijer, M.; Kluijtmans, L.A.; van den Heuvel, L.P.; et al. A candidate genetic risk factor for vascular disease: A common mutation in methylenetetrahydrofolate reductase. Nat. Genet. 1995, 10, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Moll, S.; Varga, E.A. Homocysteine and MTHFR Mutations. Circulation 2015, 132, e6–e9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, P.; Hou, J.; Wu, H.; Zhong, M. Analysis of genetic polymorphism of methylenetetrahydrofolate reductase in a large ethnic Hakka population in southern China. Medicine 2018, 97, e13332. [Google Scholar] [CrossRef] [PubMed]
- Fong, C.S.; Shyu, H.Y.; Shieh, J.C.; Fu, Y.P.; Chin, T.Y.; Wang, H.W.; Cheng, C.W. Association of MTHFR, MTR, and MTRR polymorphisms with Parkinson’s disease among ethnic Chinese in Taiwan. Clin. Chim. Acta Int. J. Clin. Chem. 2011, 412, 332–338. [Google Scholar] [CrossRef]
- Lajin, B.; Alhaj Sakur, A.; Michati, R.; Alachkar, A. Association between MTHFR C677T and A1298C, and MTRR A66G polymorphisms and susceptibility to schizophrenia in a Syrian study cohort. Asian J. Psychiatry 2012, 5, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Kaya, E.F.; Karakus, N.; Ulusoy, A.N.; Özaslan, C.; Kara, N. Association of the MTHFR Gene C677T Polymorphism with Breast Cancer in a Turkish Population. Oncol. Res. Treat. 2016, 39, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Silva, A.; Figuera, L.E.; Soto-Quintana, O.M.; Puebla-Pérez, A.M.; Ramírez-Patiño, R.; Gutiérrez-Hurtado, I.; Carrillo-Moreno, D.I.; Zúñiga-González, G.M.; Dávalos-Rodríguez, I.P.; Gallegos-Arreola, M.P. Association of the C677T polymorphism in the methylenetetrahydrofolate reductase gene with breast cancer in a Mexican population. Genet. Mol. Res. GMR 2015, 14, 4015–4026. [Google Scholar] [CrossRef]
- Couto, F.D.; Adorno, E.V.; Menezes, J.F.; Moura Neto, J.P.; Rêgo, M.A.; Reis, M.G.; Gonçalves, M.S. C677T polymorphism of the MTHFR gene and variant hemoglobins: A study in newborns from Salvador, Bahia, Brazil. Cad. De Saude Publica 2004, 20, 529–533. [Google Scholar] [CrossRef] [Green Version]
- Ford, T.C.; Downey, L.A.; Simpson, T. The Effect of a High-Dose Vitamin B Multivitamin Supplement on the Relationship between Brain Metabolism and Blood Biomarkers of Oxidative Stress: A Randomized Control Trial. Nutrients 2018, 10, 1860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, A.D.; Refsum, H. Homocysteine, B Vitamins, and Cognitive Impairment. Annu. Rev. Nutr. 2016, 36, 211–239. [Google Scholar] [CrossRef] [PubMed]
- Scaglione, F.; Panzavolta, G. Folate, folic acid and 5-methyltetrahydrofolate are not the same thing. Xenobiotica Fate Foreign Compd. Biol. Syst. 2014, 44, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Al-Bayyari, N.; Al-Zeidaneen, S.; Hailat, R.; Hamadneh, J. Vitamin D(3) prevents cardiovascular diseases by lowering serum total homocysteine concentrations in overweight reproductive women: A randomized, placebo-controlled clinical trial. Nutr. Res. 2018, 59, 65–71. [Google Scholar] [CrossRef]
- Wu, L.; Zhou, X.; Li, T.; He, J.; Huang, L.; Ouyang, Z.; He, L.; Wei, T.; He, Q. Improved Sp1 and Betaine Homocysteine-S-Methyltransferase Expression and Homocysteine Clearance Are Involved in the Effects of Zinc on Oxidative Stress in High-Fat-Diet-Pretreated Mice. Biol. Trace Elem. Res. 2018, 184, 436–441. [Google Scholar] [CrossRef]
- Baggott, J.E.; Tamura, T. Homocysteine, iron and cardiovascular disease: A hypothesis. Nutrients 2015, 7, 1108–1118. [Google Scholar] [CrossRef] [Green Version]
- Józefczuk, J.; Kasprzycka, W.; Czarnecki, R.; Graczyk, A.; Józefczuk, P.; Magda, K.; Lampart, U. Homocysteine as a Diagnostic and Etiopathogenic Factor in Children with Autism Spectrum Disorder. J. Med. Food 2017, 20, 744–749. [Google Scholar] [CrossRef]
- Dragan, S.; Buleu, F.; Christodorescu, R.; Cobzariu, F.; Iurciuc, S.; Velimirovici, D.; Xiao, J.; Luca, C.T. Benefits of multiple micronutrient supplementation in heart failure: A comprehensive review. Crit. Rev. Food Sci. Nutr. 2019, 59, 965–981. [Google Scholar] [CrossRef]
- Houston, M. The role of nutrition and nutraceutical supplements in the treatment of hypertension. World J. Cardiol. 2014, 6, 38–66. [Google Scholar] [CrossRef] [Green Version]
- Matsui, S.; Hiraishi, C.; Sato, R.; Kojima, T.; Ando, K.; Fujimoto, K.; Yoshida, H. Associations of Homocysteine with B Vitamins and Zinc in Serum Levels of Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study. J. Nutr. Sci. Vitaminol. 2021, 67, 417–423. [Google Scholar] [CrossRef]
- Heidarian, E.; Amini, M.; Parham, M.; Aminorroaya, A. Effect of zinc supplementation on serum homocysteine in type 2 diabetic patients with microalbuminuria. Rev. Diabet. Stud. 2009, 6, 64–70. [Google Scholar] [CrossRef] [Green Version]
- Ducros, V.; Andriollo-Sanchez, M.; Arnaud, J.; Meunier, N.; Laporte, F.; Hininger-Favier, I.; Coudray, C.; Ferry, M.; Roussel, A.M. Zinc supplementation does not alter plasma homocysteine, vitamin B12 and red blood cell folate concentrations in French elderly subjects. J. Trace Elem. Med. Biol. 2009, 23, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Yin, Y.; Zhen, B.; Sun, J.; Ouyang, J.; Na, N. Detection of glutathione, cysteine, and homocysteine by online derivatization-based electrospray mass spectrometry. Rapid Commun. Mass Spectrom. 2022, 36, e9291. [Google Scholar] [CrossRef] [PubMed]
- Słowiński, D.; Świerczyńska, M.; Romański, J.; Podsiadły, R. HPLC Study of Product Formed in the Reaction of NBD-Derived Fluorescent Probe with Hydrogen Sulfide, Cysteine, N-acetylcysteine, and Glutathione. Molecules 2022, 27, 8305. [Google Scholar] [CrossRef] [PubMed]
- Komarova, T.; McKeating, D.; Perkins, A.V.; Tinggi, U. Trace Element Analysis in Whole Blood and Plasma for Reference Levels in a Selected Queensland Population, Australia. Int. J. Environ. Res. Public Health 2021, 18, 2652. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, M.; Deng, Y.; Qiu, J.; Zhang, X.; Tan, J. Associations of toxic and essential trace elements in serum, follicular fluid, and seminal plasma with In vitro fertilization outcomes. Ecotoxicol. Environ. Saf. 2020, 204, 110965. [Google Scholar] [CrossRef]
- Stokes, C.S.; Lammert, F.; Volmer, D.A. Analytical Methods for Quantification of Vitamin D and Implications for Research and Clinical Practice. Anticancer Res. 2018, 38, 1137–1144. [Google Scholar] [CrossRef]
- Lin, H.; Ding, L.; Zhang, B.; Huang, J. Detection of nitrite based on fluorescent carbon dots by the hydrothermal method with folic acid. R. Soc. Open Sci. 2018, 5, 172149. [Google Scholar] [CrossRef] [Green Version]
- Ma, F.; Zhou, X.; Li, Q.; Zhao, J.; Song, A.; An, P.; Du, Y.; Xu, W.; Huang, G. Effects of Folic Acid and Vitamin B12, Alone and in Combination on Cognitive Function and Inflammatory Factors in the Elderly with Mild Cognitive Impairment: A Single-blind Experimental Design. Curr. Alzheimer Res. 2019, 16, 622–632. [Google Scholar] [CrossRef]
- Qiu, L.; Wang, W.; Sa, R.; Liu, F. Prevalence and Risk Factors of Hypertension, Diabetes, and Dyslipidemia among Adults in Northwest China. Int. J. Hypertens. 2021, 2021, 5528007. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, J.; Xiong, Z.; Yao, X.; Zhang, Y.; Ning, X.; Zhong, Y.; Liu, Z.; Zhang, Y.; Zhao, T.; et al. Prevalence and clinical demography of hyperhomocysteinemia in Han Chinese patients with schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 2021, 271, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Thawnashom, K.; Tungtrongchitr, R.; Petmitr, S.; Pongpaew, P.; Phonrat, B.; Tungtrongchitr, A.; Schelp, F.P. Methylenetetrahydrofolate reductase (MTHFR) polymorphism (C677T) in relation to homocysteine concentration in overweight and obese Thais. Southeast Asian J. Trop. Med. Public Health 2005, 36, 459–466. [Google Scholar] [PubMed]
- Gallistl, S.; Sudi, K.; Mangge, H.; Erwa, W.; Borkenstein, M. Insulin is an independent correlate of plasma homocysteine levels in obese children and adolescents. Diabetes Care 2000, 23, 1348–1352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, B.; Liu, Y.; Li, Y.; Fan, S.; Zhi, X.; Lu, X.; Wang, D.; Zheng, Q.; Wang, Y.; Wang, Y.; et al. Geographical distribution of MTHFR C677T, A1298C and MTRR A66G gene polymorphisms in China: Findings from 15357 adults of Han nationality. PLoS ONE 2013, 8, e57917. [Google Scholar] [CrossRef]
- Oliveira, I.O.; Silva, L.P.; Borges, M.C.; Cruz, O.M.; Tessmann, J.W.; Motta, J.V.; Seixas, F.K.; Horta, B.L.; Gigante, D.P. Interactions between lifestyle and MTHFR polymorphisms on homocysteine concentrations in young adults belonging to the 1982 Pelotas Birth Cohort. Eur. J. Clin. Nutr. 2017, 71, 259–266. [Google Scholar] [CrossRef] [Green Version]
- Zappacosta, B.; Graziano, M.; Persichilli, S.; Di Castelnuovo, A.; Mastroiacovo, P.; Iacoviello, L. 5,10-Methylenetetrahydrofolate reductase (MTHFR) C677T and A1298C polymorphisms: Genotype frequency and association with homocysteine and folate levels in middle-southern Italian adults. Cell Biochem. Funct. 2014, 32, 1–4. [Google Scholar] [CrossRef]
- Jing, M.; Rech, L.; Wu, Y.; Goltz, D.; Taylor, C.G.; House, J.D. Effects of zinc deficiency and zinc supplementation on homocysteine levels and related enzyme expression in rats. J. Trace Elem. Med. Biol. Organ Soc. Miner. Trace Elem. 2015, 30, 77–82. [Google Scholar] [CrossRef]
- Dilli, D.; Dogan, N.N.; Orun, U.A.; Koc, M.; Zenciroglu, A.; Karademir, S.; Akduman, H. Maternal and neonatal micronutrient levels in newborns with CHD. Cardiol. Young 2018, 28, 523–529. [Google Scholar] [CrossRef]
- Vázquez-Lorente, H.; Herrera-Quintana, L.; Molina-López, J.; Gamarra, Y.; Planells, E. Effect of zinc supplementation on circulating concentrations of homocysteine, vitamin B(12), and folate in a postmenopausal population. J. Trace Elem. Med. Biol. 2022, 71, 126942. [Google Scholar] [CrossRef]
- Maywald, M.; Wessels, I.; Rink, L. Zinc Signals and Immunity. Int. J. Mol. Sci. 2017, 18, 2222. [Google Scholar] [CrossRef] [Green Version]
- He, P.; Li, H.; Liu, M.; Zhang, Z.; Zhang, Y.; Zhou, C.; Li, Q.; Liu, C.; Qin, X. U-shaped Association Between Dietary Zinc Intake and New-onset Diabetes: A Nationwide Cohort Study in China. J. Clin. Endocrinol. Metab. 2022, 107, e815–e824. [Google Scholar] [CrossRef] [PubMed]
- Maret, W.; Sandstead, H.H. Zinc requirements and the risks and benefits of zinc supplementation. J. Trace Elem. Med. Biol. 2006, 20, 3–18. [Google Scholar] [CrossRef] [PubMed]

| Index | Control (n = 135) | HHcy Group (n = 68) | p-Value |
|---|---|---|---|
| Sex | 0.000 | ||
| Male, n (%) | 62 (45.9%) | 51 (75.0%) | |
| Female, n (%) | 73 (54.1%) | 17 (25.0%) | |
| Age, years (± SD) | 24.72 ± 18.05 | 27.22 ± 14.84 | 0.057 |
| Height, cm (± SD) | 153.71 ± 19.32 | 164.64 ± 30.45 | 0.631 |
| Weight, kg (±SD) | 53.00 ± 21.89 | 69.20 ± 26.28 | 0.138 |
| BMI ± SD | 21.40 ± 5.58 | 24.56 ± 7.16 | 0.001 |
| BMI Group | 0.021 | ||
| BMI < 18.5, n (%) | 44 (32.60%) | 13 (19.10%) | |
| 18.5 ≤ BMI ≤ 23.9, n (%) | 50 (37.00%) | 28 (41.20%) | |
| 24 ≤ BMI ≤ 28, n (%) | 22 (16.30%) | 7 (10.30%) | |
| BMI > 28, n (%) | 19 (14.10%) | 20 (29.40%) | |
| ALKP, U/L (± SD) | 159.61 ± 85.03 | 131.89 ± 74.16 | 0.023 |
| UA, mmol/L (±SD) | 410.61 ± 72.17 | 475.43 ± 116.52 | <0.001 |
| Hcy, µmol/L (± SD) | 9.26 ± 2.74 | 35.89 ± 20.11 | <0.001 |
| MTHFR 677 | <0.001 | ||
| CC, n (%) | 28 (20.70%) | 5 (7.40%) | |
| CT, n (%) | 77 (57.00%) | 28 (41.20%) | |
| TT, n (%) | 30 (22.20%) | 35 (51.50%) | |
| MTHFR 1269 | 0.083 | ||
| AA, n (%) | 94 (69.63%) | 57 (83.80%) | |
| AC, n (%) | 36 (26.67%) | 10 (14.70%) | |
| CC, n (%) | 5 (3.70%) | 1 (1.50%) | |
| MTRR 66 | 0.853 | ||
| AA, n (%) | 70 (51.85%) | 35 (51.50%) | |
| AG, n (%) | 56 (41.48%) | 27 (39.70%) | |
| GG, n (%) | 9 (6.70%) | 6 (8.80%) |
| Genotype | n | Hcy Concentrations (µmol/L) | p-Value 1 | p-Value 2 | p-Value 3 | ||
|---|---|---|---|---|---|---|---|
| Total | Male | Female | |||||
| MTHFR 677 CC | 33 | 11.40 ± 7.39 | 11.97 ± 6.33 | 10.86 ± 8.45 | <0.001 | <0.001 | 0.095 |
| MTHFR 677 CT | 105 | 14.22 ± 11.39 | 15.56 ± 10.30 | 12.63 ± 8.49 | |||
| MTHFR 677 TT | 65 | 28.01 ± 23.54 | 33.38 ± 14.39 | 19.41 ± 9.64 | |||
| MTHFR 1298 AA | 151 | 19.46 ± 18.17 | 23.53 ± 8.11 | 14.52 ± 7.97 | 0.196 | 0.107 | 0.911 |
| MTHFR 1298 AC | 46 | 14.54 ± 14.47 | 14.91 ± 8.96 | 14.07 ± 7.53 | |||
| MTHFR 1298 CC | 6 | 13.74 ± 6.38 | 16.64 ± 7.97 | 10.84 ± 3.31 | |||
| MTRR 66 AA | 105 | 17.00 ± 14.56 | 20.81 ± 6.79 | 12.49 ± 9.12 | 0.526 | 0.695 | 0.408 |
| MTRR 66 AG | 83 | 19.03 ± 20.36 | 20.99 ± 7.09 | 16.71 ± 9.46 | |||
| MTRR 66 GG | 15 | 21.64 ± 16.42 | 26.19 ± 8.10 | 12.55 ± 7.16 | |||
| Characteristics | Control (n = 135) | HHcy Group (n = 68) | p-Value |
|---|---|---|---|
| Vitamin D, ng/mL (±SD) | 22.55 ± 10.04 | 20.56 ± 8.61 | 0.160 |
| Zn, µmol/L (±SD) | 83.57 ± 12.79 | 90.54 ± 11.71 | <0.001 |
| Vitamin B12, pg/mL (±SD) | 478.19 ± 241.07 | 266.62 ± 146.63 | <0.001 |
| fol, ng/mL (±SD) | 9.76 ± 5.04 | 6.38 ± 3.29 | <0.001 |
| Fe, µmol/L (±SD) | 15.65 ± 5.30 | 17.45 ± 5.03 | 0.020 |
| Pb, ug/L (±SD) | 24.16 ± 6.55 | 24.13 ± 6.42 | 0.970 |
| Cu, µmol/L (±SD) | 14.93 ± 3.09 | 14.38 ± 2.10 | 0.190 |
| Ca, mmol/L (±SD) | 2.34 ± 0.09 | 2.33 ± 0.08 | 0.350 |
| Mg, µmol/L (±SD) | 1.06 ± 1.50 | 0.93 ± 0.06 | 0.490 |
| Vitamin A, pg/mL (±SD) | 496.18 ± 54.47 | 536.08 ± 111.54 | 0.001 |
| P, mmol/L (±SD) | 1.39 ± 0.25 | 1.32 ± 0.22 | 0.040 |
| Quartiles of Plasma Zn (µmol/L) | |||||
|---|---|---|---|---|---|
| Model | Q1 | Q2 | Q3 | Q4 | p-Value |
| (<78.06) | (78.06–83.89) | (83.89–93.06) | (≥93.06) | ||
| Control/HHcy | 44/7 | 35/16 | 30/21 | 26/24 | 0.419 |
| Model 1 | 0.172 (0.065, 0.455) | 0.495 (0.220, 1.114) | 0.758 (0.345, 1.665) | 1 (ref.) | 0.003 |
| Model 2 | 0.273 (0.092, 0.813) | 0.631 (0.258, 1.54) | 1.131 (0.468, 2.733) | 1 (ref.) | <0.001 |
| Model 3 | 0.148 (0.034, 0.646) | 1.159 (0.376, 3.571) | 1.137 (0.386, 3.354) | 1 (ref.) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, C.; Ding, D.; Wen, Z.; Zhang, C.; Kong, J. Association between Micronutrients and Hyperhomocysteinemia: A Case-Control Study in Northeast China. Nutrients 2023, 15, 1895. https://doi.org/10.3390/nu15081895
Sun C, Ding D, Wen Z, Zhang C, Kong J. Association between Micronutrients and Hyperhomocysteinemia: A Case-Control Study in Northeast China. Nutrients. 2023; 15(8):1895. https://doi.org/10.3390/nu15081895
Chicago/Turabian StyleSun, Can, Ding Ding, Zhouyu Wen, Chengmei Zhang, and Juan Kong. 2023. "Association between Micronutrients and Hyperhomocysteinemia: A Case-Control Study in Northeast China" Nutrients 15, no. 8: 1895. https://doi.org/10.3390/nu15081895





