Breastfeeding Duration and Residential Isolation amid Aboriginal Children in Western Australia
Abstract
:1. Introduction
2. Experimental Section
2.1. Population and Sampling
2.2. Estimation
2.3. Ethics Approval
2.4. Outcome and Exposures
2.4.1. Outcome
2.4.2. Exposures
2.4.3. Birth Linkage Data
2.5. Analyses
3. Results
| Exposures and confounding measures | % | n | ||
|---|---|---|---|---|
| Demographic variables | ||||
| Level of Relative Isolation (LORI) | ||||
| None | 37.8 | 8360 | ||
| Low | 25.7 | 5680 | ||
| Moderate | 20.0 | 4420 | ||
| High | 9.1 | 2010 | ||
| Extreme | 7.4 | 1640 | ||
| Number of children in the household | ||||
| Four or more children | 43.9 | 9690 | ||
| Infant characteristics | ||||
| Gender | ||||
| Male | 51.1 | 11,300 | ||
| Female | 48.9 | 10,800 | ||
| Birth weight † | ||||
| <2500 g | 9.0 | 2000 | ||
| >2500 g | 79.0 | 17,500 | ||
| Maternal characteristics | ||||
| Primary caregiver: attainment § | ||||
| Did not attend school | 1.4 | 310 | ||
| 1–9 years of education | 17.8 | 3930 | ||
| 10 years | 46.7 | 10,300 | ||
| 11–12 years | 26.3 | 5800 | ||
| >13 years | 5.9 | 1300 | ||
| Family financial strain ║ | ||||
| Spending more money than we get | 8.5 | 1870 | ||
| We have just enough money to get by | 45.2 | 10,000 | ||
| Some money left over but we just spend it | 13.2 | 2910 | ||
| Can save a bit now and again | 26.6 | 5880 | ||
| Can save a lot | 4.5 | 1000 | ||
| Smoking in pregnancy | ||||
| Yes | 46.3 | 10,200 | ||
| Mother chewed tobacco during pregnancy | ||||
| Yes | 3.5 | 760 | ||
| Occupation skill level ¶ | ||||
| Managers, administrators, professionals | 3.9 | 870 | ||
| Associate professionals | 3.4 | 740 | ||
| Tradespersons, advanced clerical, service workers | 2.5 | 540 | ||
| Intermediate production and transport workers | 13.9 | 3070 | ||
| Elementary clerical, sales & services, labourers | 8.2 | 1810 | ||
| Not in the labour force or unemployed | 66.2 | 14,600 | ||
| Socioeconomic disadvantage | ||||
| Bottom 5% | 56.7 | 12,500 | ||
| >5%–10% | 25.6 | 5650 | ||
| >10%–25% | 13.1 | 2890 | ||
| >25%–50% | 4.2 | 930 | ||
| Top 50% | 0.4 | 100 | ||
3.1. Bivariate and Multivariate Analyses
| Breastfeeding Never or <3 months (%) | Breastfeeding >3 months (%) | ||||
|---|---|---|---|---|---|
| Exposures | % | 95% CI | % | 95% CI | |
| Demographic characteristics | |||||
| Levels of Relative Isolation (LORI) | |||||
| None | 40.6 | 36.5, 44.9 | 59.4 | 55.1, 63.5 | |
| Low | 33.4 | 29.2, 37.8 | 66.6 | 62.2, 70.8 | |
| Moderate | 16.0 | 12.9, 19.6 | 84.0 | 80.4, 87.1 | |
| High | 12.9 | 9.3, 17.5 | 87.1 | 82.5, 90.7 | |
| Extreme | 8.6 | 5.6, 13.0 | 91.4 | 87.0, 94.4 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Number of children in the family—grouped | |||||
| Three or less | 34.2 | 30.9, 37.5 | 65.8 | 62.5, 69.1 | |
| Four or more | 22.2 | 19.7, 24.8 | 77.8 | 75.2, 80.3 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Infant characteristics | |||||
| Gender | |||||
| Male | 30.3 | 27.5, 33.4 | 69.7 | 66.6, 72.5 | |
| Female | 27.5 | 24.9, 30.2 | 72.5 | 69.8, 75.1 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Birth weight | |||||
| Less than 2500 g | 41.1 | 34.4, 48.6 | 58.9 | 51.4, 65.6 | |
| 2500 g or more | 27.5 | 25.2, 29.8 | 72.5 | 70.2, 74.8 | |
| Missing | 29.3 | 23.6, 35.4 | 70.7 | 64.6, 76.4 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Maternal characteristics | |||||
| Primary caregiver: level of educational attainment | |||||
| Did not attend school | 24.3 | 10.7, 44.9 | 75.7 | 55.1, 89.3 | |
| 1–9 years education | 33.4 | 28.0, 39.5 | 66.6 | 60.5, 72.0 | |
| 10 years education | 30.5 | 27.3, 33.7 | 69.5 | 66.3, 72.7 | |
| 11–12 years education | 25.2 | 21.0, 29.6 | 74.8 | 70.4, 79.0 | |
| >13 years education | 24.5 | 15.3, 36.1 | 75.5 | 63.9, 84.7 | |
| Not Stated | 19.1 | 6.8, 40.7 | 80.9 | 59.3, 93.2 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Family financial strain | |||||
| Spending more money than we get | 38.4 | 29.6, 47.9 | 61.6 | 52.1, 70.4 | |
| We have just enough money to get by | 27.6 | 24.7, 30.6 | 72.4 | 69.4, 75.3 | |
| Some money left over but we just spend it | 33.1 | 26.9, 40.3 | 66.9 | 59.7, 73.1 | |
| Can save a bit now and again | 27.3 | 23.0, 32.1 | 72.7 | 67.9, 77.0 | |
| Can save a lot | 26.3 | 17.6, 37.8 | 73.7 | 62.2, 82.4 | |
| Smoking in pregnancy | |||||
| Yes | 32.8 | 29.6, 36.2 | 67.2 | 63.8, 70.4 | |
| No | 25.6 | 22.9, 28.4 | 74.4 | 71.6, 77.1 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Mother chewed tobacco during pregnancy | |||||
| Yes | 13.1 | 7.8, 20.1 | 86.9 | 79.9, 92.2 | |
| No | 29.5 | 27.4, 31.7 | 70.5 | 68.3, 72.6 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Primary caregiver: occupation skill level | |||||
| Managers, administrators, professionals | 21.1 | 13.7, 31.2 | 78.9 | 69.4, 86.6 | |
| Associate professionals | 29.0 | 17.1, 43.1 | 71.0 | 56.9, 82.9 | |
| Tradespersons, advanced clerical, service workers | 22.9 | 9.0, 43.6 | 77.1 | 56.4, 91.0 | |
| Intermediate production and transport workers | 22.3 | 16.5, 29.0 | 77.7 | 71.0, 83.5 | |
| Elementary clerical, sales & services, labourers | 25.5 | 18.9, 32.6 | 74.5 | 67.4, 81.1 | |
| Not in labour force or unemployed | 31.7 | 29.1, 34.5 | 68.3 | 65.5, 70.9 | |
| Missing | 19.1 | 6.8, 40.7 | 80.9 | 59.3, 93.2 | |
| Total | 28.9 | 26.9, 31.1 | 71.1 | 68.9, 73.1 | |
| Quintiles of Socio-economic disadvantage | |||||
| Bottom Quintile | 27.2 | 24.7, 30.0 | 72.8 | 70.0, 75.3 | |
| Second Quintile | 31.5 | 26.6, 36.6 | 68.5 | 63.4, 73.4 | |
| Third Quintile | 28.9 | 22.5, 35.6 | 71.1 | 64.4, 77.5 | |
| Fourth Quintile | 36.2 | 19.4, 57.6 | 63.8 | 42.4, 80.6 | |
| Top Quintile | 26.7 | 0.8, 90.6 | 73.3 | 9.4, 99.2 | |
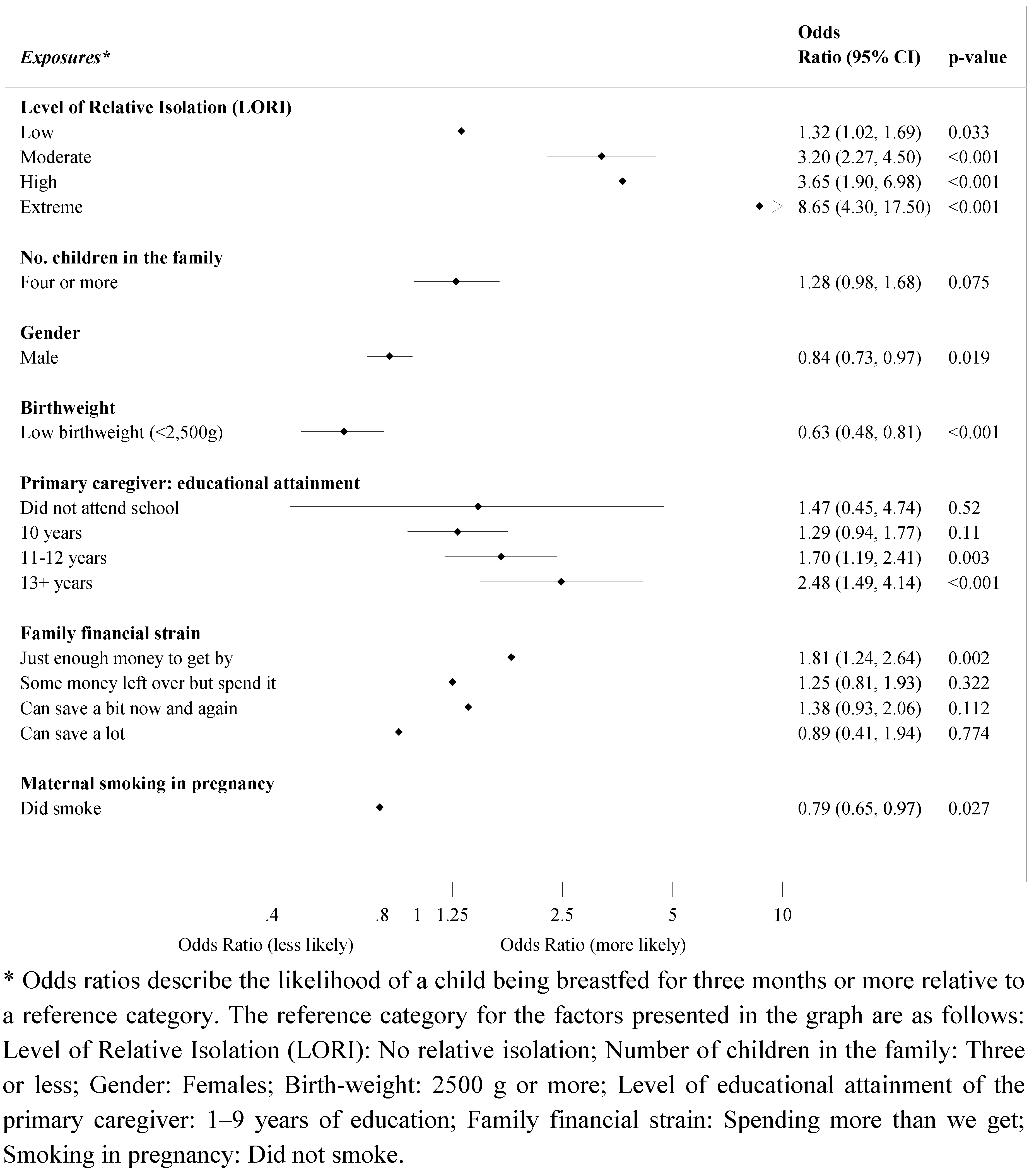
3.1.1. LORI
3.1.2. Confounding Measures
4. Discussion
Strengths and Limitations
5. Conclusions
Acknowledgments
Conflict of Interest
References
- Facts for Life Health and Nutrition, 3rd ed; United Nations Children’s Fund: New York, NY, USA, 2002.
- Progress for Children: A Report Card on Nutrition (Number 4). United Nations Children’s Fund: New York, NY, USA, 2006.
- Infant and Young Child Nutrition and Progress in Implementing the International Code of Marketing of Breast Milk Substitutes; EB113/38 Rev.2. World Health Organisation: Geneva, Switherland, 15 January 2004.
- Global childhood malnutrition. Lancet 2006, 367, 1459. [CrossRef]
- Gracey, M. Historical, cultural, political, and social influences on dietary patterns and nutrition in Australian Aboriginal children. Am. J. Clin. Nutr. 2000, 72, 1361S–1367S. [Google Scholar]
- Scott, J.A.; Binns, C.W. Factors associated with the initiation and duration of breastfeeding: A review of the literature. Aust. J. Nutr. Diet. 1998, 55, 51–61. [Google Scholar]
- Zubrick, S.R.; Lawrence, D.M.; Silburn, S.R.; Blair, E.; Milroy, H.; Wilkes, E.; Eades, S.; D’Antoine, H.; Read, A.; Ishiguchi, P.; Doyle, S. The Western Australian Aboriginal Child Health Survey: The Health of Aboriginal Children and Young People; Telethon Institute for Child Health Research: Perth, Australia, 2004. [Google Scholar]
- Zubrick, S.R.; Silburn, S.R.; Lawrence, D.M.; Mitrou, F.G.; Dalby, R.B.; Blair, E.M.; Griffin, J.; Milroy, H.; de Maio, J.A.; Cox, A.; Li, J. The Western Australian Aboriginal Child Health Survey: The Social and Emotional Wellbeing of Aboriginal Children and Young People; Telethon Institute for Child Health Research: Perth, Australia, 2005. [Google Scholar]
- Silburn, S.R.; Zubrick, S.R.; de Maio, J.A.; Shepherd, C.; Griffin, J.A.; Mitrou, F.G.; Dalby, R.B.; Hayward, C.; Pearson, G. The Western Australian Aboriginal Child Health Survey: Strengthening the Capacity of Aboriginal Children, Families and Communities; Curtin University of Technology and Telethon Institute for Child Health Research: Perth, Australia, 2006. [Google Scholar]
- Zubrick, S.R.; Silburn, S.R.; de Maio, J.A.; Shepherd, C.; Griffin, J.A.; Dalby, R.B.; Mitrou, F.G.; Lawrence, D.M.; Hayward, C.; Pearson, G.; Milroy, H.; Milroy, J.; Cox, A. The Western Australian Aboriginal Child Health Survey: Improving the Educational Experiences of Aboriginal Children and Young People; Curtin University of Technology and Telethon Institute for Child Health Research: Perth, Australia, 2006. [Google Scholar]
- Wolter, K.M. Introduction to Variance Estimation, 1st ed; Springer Verlag: New York, NY, USA, 1985. [Google Scholar]
- Jones, H.L. Jackknife estimation of functions of stratum means. Biometrics 1974, 61, 343–348. [Google Scholar]
- Child Health Questionnaire (0–3 years). In Western Australian Aboriginal Child Health Survey; Telethon Institute for Child Health Research: Perth, Australia, 2000.
- Child Health Questionnaire (4–18 years). In Western Australian Aboriginal Child Health Survey; Telethon Institute for Child Health Research: Perth, Australia, 2000.
- Silburn, S.R.; Zubrick, S.R.; Lawrence, D.M.; Mitrou, F.G.; de Maio, J.A.; Blair, E.; Cox, A.; Dalby, R.B.; Griffin, J.A.; Pearson, G.; Hayward, C. The intergenerational effects of forced separation on the social and emotional wellbeing of Aboriginal children and young people. In Family Matters; Australian Institute of Family Studies: Melbourne, Australia, 2006; pp. 10–17. [Google Scholar]
- SAS version 9, SAS Institute Inc.: Cary, NC, USA, 2002.
- Donath, S.; Amir, L. Rates of breastfeeding in Australia by State and socio-economic status: Evidence from the 1995 National Health Survey. J. Paediatr. Child Health 2000, 36, 164–168. [Google Scholar] [CrossRef]
- Binns, C.; Gilchrist, D.; Gracey, M.; Zhang, M.; Scott, J.; Lee, A. Factors associated with the initiation of breast-feeding by Aboriginal mothers in Perth. Public Health Nutr. 2004, 7, 857–861. [Google Scholar]
- Holmes, W.; Phillips, J.; Thorpe, L. Initiation rate and duration of breast-feeding in the Melbourne Aboriginal community. Aust. N. Z. J. Public Health 1997, 21, 500–503. [Google Scholar] [CrossRef]
- Hayman, N.; Kanhutu, J.; Bond, S.; Marks, G.C. Breast-feeding and weaning practices of an urban community of indigenous Australians. Asia Pacific J. Clin. Nutr. 2000, 9, 232–234. [Google Scholar] [CrossRef]
- Oddy, W.H.; Kickett-Tucker, C.; de Maio, J.; Lawrence, D.; Cox, A.; Silburn, S.R.; Stanley, F.J.; Zubrick, S. The association of infant feeding with parent-reported infection and hospitalisations in the West Australian Aboriginal Child Health Survey. Aust. N. Z. J. Public Health 2008, 32, 207–215. [Google Scholar] [CrossRef]
- Mackerras, D. Breastfeeding in Indigenous Australians. Aust. J. Nutr. Diet. 2006, 63, 5–7. [Google Scholar] [CrossRef]
- Nutrition in Aboriginal and Torres Strait Islander Peoples: An Informative Paper. National Health and Medical Research Council: Canberra, Australia, 2000.
- National Health Survey: Aboriginal and Torres Strait Islander Results. Australian Bureau of Statistics: Canberra, Australia, 2002.
- Records of the American-Australian Scientific Expedition to Arnhem Land; Mountford, C. (Ed.) Melbourne University Press: Melbourne, Australia, 1948.
- Cunningham, J. Occasional Paper: Cigarette Smoking among Indigenous Australians; Australian Bureau of Statistics: Canberra, Australia, 1994. [Google Scholar]
- Simard, I.; O’Brien, H.T.; Beaudoin, A.; Turcotte, D.; Damant, D.; Ferland, S.; Marcotte, M.-J.; Jauvin, N.; Champoux, L. Factors Influencing the Initiation and Duration of Breastfeeding Among Low-Income Women Followed by the Canada Prenatal Nutrition Program in 4 Regions of Quebec. J. Hum. Lact. 2005, 21, 327–337. [Google Scholar] [CrossRef]
- Scott, J.A.; Binns, C.W. Breastfeeding: are boys missing out? Birth 1999, 26, 276–277. [Google Scholar]
- Holmes, W.; Thorpe, L.; Phillips, J. Influences on infant-feeding beliefs and practices in an urban Aboriginal community. Aust. N. Z. J. Public Health 1997, 21, 504–510. [Google Scholar] [CrossRef]
- Dodgson, J.E.; Duckett, L.; Garwick, A.; Graham, B.L. An Ecological Perspective of Breastfeeding in an Indigenous Community. J. Nurs. Scholarsh. 2002, 34, 235–241. [Google Scholar]
- Shepherd, C.C.J.; Li, J.; Mitrou, F.; Zubrick, S.R. Socioeconomic disparities in the mental health of Indigenous children in Western Australia. BMC Public Health 2012, 12, 756. [Google Scholar] [CrossRef]
- Li, R.; Scanlon, K.; Serdula, M. The Validity and Reliability of Maternal Recall of Breastfeeding Practice. Nutr. Rev. 2005, 63, 103–110. [Google Scholar] [CrossRef]
- Jordan, S.; Emery, S.; Watkins, A.; Evans, J.; Storey, M.; Morgan, G. Associations of drugs routinely given in labour with breastfeeding at 48 hours: Analysis of the Cardiff Births Survey. BJOG 2009, 116, 1622–1630. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Cromie, E.A.S.; Shepherd, C.C.J.; Zubrick, S.R.; Oddy, W.H. Breastfeeding Duration and Residential Isolation amid Aboriginal Children in Western Australia. Nutrients 2012, 4, 2020-2034. https://doi.org/10.3390/nu4122020
Cromie EAS, Shepherd CCJ, Zubrick SR, Oddy WH. Breastfeeding Duration and Residential Isolation amid Aboriginal Children in Western Australia. Nutrients. 2012; 4(12):2020-2034. https://doi.org/10.3390/nu4122020
Chicago/Turabian StyleCromie, Elizabeth A. S., Carrington C. J. Shepherd, Stephen R. Zubrick, and Wendy H. Oddy. 2012. "Breastfeeding Duration and Residential Isolation amid Aboriginal Children in Western Australia" Nutrients 4, no. 12: 2020-2034. https://doi.org/10.3390/nu4122020




