Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Outcome and Exploratory Variables
2.2. Statistical Analysis
3. Results
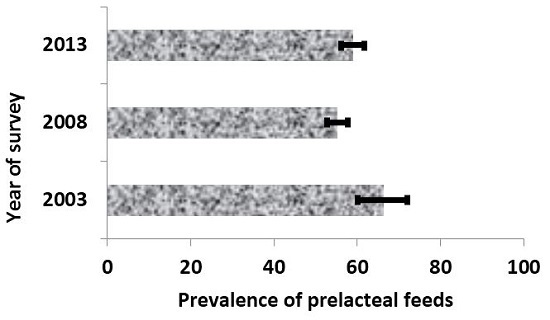
3.1. Trends in Prelacteal Feeds
3.1.1. Trends in Prevalence of Prelacteal Feeds by Key Factors
3.1.2. Multivariable Analysis
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Meshram, I.; Laxmaiah, A.; Venkaiah, K.; Brahmam, G.N.V. Impact of feeding and breastfeeding practices on the nutritional status of infants in a district of Andhra Pradesh, India. Natl. Med. J. India 2012, 25, 201–206. [Google Scholar] [PubMed]
- Bekele, Y.; Mengistie, B.; Mesfine, F. Prelacteal feeding practice and associated factors among mothers attending immunization clinic in Harari region public health facilities, Eastern Ethiopia. Open J. Prev. Med. 2014, 4, 529–534. [Google Scholar] [CrossRef]
- Nguyen, P.H.; Keithly, S.C.; Nguyen, N.T.; Nguyen, T.T.; Tran, L.M.; Hajeebhoy, N. Prelacteal feeding practices in Vietnam: Challenges and associated factors. BMC Public Health 2013. [Google Scholar] [CrossRef] [PubMed]
- Khanal, V.; Adhikari, M.; Sauer, K.; Zhao, Y. Factors associated with the introduction of prelacteal feeds in Nepal: Findings from the Nepal demographic and health survey 2011. Int. Breastfeed. J. 2013. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.M.; Radwan, M.M.; Arafa, S.A.; Habib, M.; DuPont, H.L. Pre-lacteal infant feeding practices in rural Egypt. J. Trop. Pediatr. 1992, 38, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Ogah, A.O.; Ajayi, A.M.; Akib, S.; Okolo, S.N. A cross-sectional study of pre-lacteal feeding practice among women attending Kampala international university teaching hospital maternal and child health clinic, Bushenyi, Western Ugandan. Asian J. Med. Sci. 2012, 4, 79–85. [Google Scholar]
- WHO. Exclusive Breastfeeding; World Health Organization: Geneva, The Netherlands, 2014. [Google Scholar]
- National Population Commission (NPC), Federal Republic of Nigeria. Final Report on Nigeria Demographic and Health Survey 2003; ORC Macro: Calverton, MD, USA, 2003.
- Akuse, R.; Obinya, E. Why healthcare workers give prelacteal feeds. Eur. J. Clin. Nutr. 2002, 56, 729–734. [Google Scholar] [CrossRef] [PubMed]
- El-Gilany, A.E.; Abdel-Hady, D. Newborn first feed and prelacteal feeds in Mansoura, Egypt. Biomed. Res. Int. 2014. [Google Scholar] [CrossRef] [PubMed]
- WHO and UNICEF. Innocenti declaration on the protection, promotion and support of breastfeeding. In Proceedings of the Breastfeeding in the 1990s: A Global Initiative at Spedale Degli Innocenti, Florence, Italy, 30 July–1 August 1990; United Nations Children’s Fund: New York, NY, USA, 1990. [Google Scholar]
- Roy, M.P.; Mohan, U.; Singh, S.K.; Singh, V.K.; Srivastava, A.K. Determinants of prelacteal feeding in rural northern India. Int. J. Prev. Med. 2014, 5, 658–663. [Google Scholar] [PubMed]
- Salve Dawal, S.; Inamdar, I.F.; Saleem, T.; Priyanka, S.; Doibale, M.K. Study of pre lacteal feeding practices and its determinants in a rural area of Maharashtra. Sch. J. Appl. Med. Sci. 2014, 2, 1422–1427. [Google Scholar]
- Boccolini, C.; Pérez-Escamilla, R. Risk factors for prelacteal feedings in seven Latin America and Caribbean countries: A multilevel analysis. FASEB J. 2014, 28 (Suppl. 131.7). [Google Scholar]
- Boccolini, C.S.; Pérez-Escamilla, R.; Giugliani, E.R.; Boccolini, P.M. Inequities in milk-based prelacteal feedings in Latin America and the Caribbean: The role of cesarean section delivery. J. Hum. Lact. 2014, 31, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Fjeld, E.; Siziya, S.; Katepa-Bwalya, M.; Kankasa, C.; Moland, K.M.; Tylleskär, T.; PROMISE-EBF Study Group. No sister, the breast alone is not enough for my baby’ a qualitative assessment of potentials and barriers in the promotion of exclusive breastfeeding in southern Zambia. Int. Breastfeed. J. 2008. [Google Scholar] [CrossRef] [PubMed]
- Adetunji, O.; Joseph, A.; Olusola, E.; Joel-Medewase, V.; Fadero, F.; Oyedeji, G. Pre-lacteal feeding practices of doctors and nurses in a state and teaching hospital in western Nigeria: A cause for concern. Int. J. Nutr. Wellness 2006, 3, 4330. [Google Scholar]
- Hadley, C.; Lindstrom, D.; Belachew, T.; Tessema, F. Ethiopia adolescents’ attitudes and expectations deviate from current infant and young child feeding recommendations. J. Adolesc. Health 2008, 43, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Davies-Adetugbo, A. Sociocultural factors and the promotion of exclusive breastfeeding in rural Yoruba communities of Osun State. Soc. Sci. Med. 1997, 45, 113–125. [Google Scholar] [CrossRef]
- Agho, K.; Dibley, M.J.; Odiase, J.I.; Ogbonmwan, S.M. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy Childbirth 2011. [Google Scholar] [CrossRef] [PubMed]
- Ibadin, O.M.; Ofili, N.A.; Monday, P.; Nwajei, C.J. Prelacteal feeding practices among lactating mothers in Benin City, Nigeria. Niger. J. Paediatr. 2013, 40, 139–144. [Google Scholar]
- National Population Commission, Federal Republic of Nigeria. Final Report on Nigeria Demographic and Health Survey 2013; ICF International: Rockville, MD, USA, 2013.
- National Population Commission, Federal Republic of Nigeria. Final Report on Nigeria Demographic and Health Survey 2008; ICF International: Rockville, MD, USA, 2008.
- Titaley, C.R.; Dibley, M.J.; Roberts, C.L.; Hall, J.; Agho, K. Iron and folic acid supplements and reduced early neonatal deaths in Indonesia. Bull. World Health Organ. 2010, 88, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Rabe-Hesketh, S.; Skrondal, A. Multilevel modelling of complex survey data. J. R. Stat. Soc. Ser. A 2006, 169, 805–827. [Google Scholar] [CrossRef]
- Victora, C.G.; Huttly, S.R.; Fuchs, S.C.; Olinto, M.T. The role of conceptual frameworks in epidemiological analysis: A hierarchical approach. Int. J. Epidemiol. 1997, 26, 224–227. [Google Scholar] [CrossRef] [PubMed]
- WHO. Indicators for Assessing Infant and Young Child Feeding Practices; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Federal Ministry of Health (FMoH). Technical Report on the 2010 National HIV Sentinel Survey among Pregnant Women Attending Antenatal Clinics in Nigeria; Federal Government of Nigeria: Abuja, Nigeria, 2010.
- Fadnes, L.; Engebretsen, I.M.S.; Wamani, H.; Semiyaga, N.B.; Tylleskar, T.; Tumwine, J.K. Infant feeding among HIV-positive mothers and the general population mothers: Comparison of two cross-sectional surveys in Eastern Uganda. BMC Public Health 2009. [Google Scholar] [CrossRef] [PubMed]
- Joshi, P.; Raj Angdembe, M.; Das, S.K.; Ahmed, S.; Faruque, A.S.G.; Ahmed, T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: A cross-sectional study. Int. Breastfeed. J. 2014. [Google Scholar] [CrossRef] [PubMed]
- Coutsoudis, A.; Kubendran, P.; Elizabeth, S.; Louise, K.; Coovadia, H.M. Influence of infant-feeding patterns on early mother-to-child transmission of HIV-1 in Durban, South Africa: A prospective cohort study. Lancet 1999, 354, 471–476. [Google Scholar] [CrossRef]
- Iliff, P.J.; Piwoz, E.G.; Tavengwa, N.V.; Zunguza, C.D.; Marinda, E.T.; Nathoo, K.J.; Moulton, L.H.; Ward, B.J.; Humphrey, J.H.; ZVITAMBO study group. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. Aids 2005, 19, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Ogbo, F.; Page, A.; Idoko, J.; Claudio, F.; Agho, K.E. Trends in complimentary feeding indicators in Nigeria, 2003–2013. BMJ Open 2015. [Google Scholar] [CrossRef] [PubMed]
- Bezner Kerr, R.; Dakishoni, L.; Shumba, L.; Msachi, R.; Chirwa, M. “We grandmothers know plenty”: Breastfeeding, complementary feeding and the multifaceted role of grandmothers in Malawi. Soc. Sci. Med. 2008, 66, 1095–1105. [Google Scholar] [CrossRef] [PubMed]
- Inayati, D.A.; Scherbaum, V.; Purwestri, R.C.; Hormann, E.; Wirawan, N.N.; Suryantan, J.; Hartono, S.; Bloem, M.A.; Pangaribuan, R.V.; Biesalski, H.K.; et al. Infant feeding practices among mildly wasted children: A retrospective study on Nias Island, Indonesia. Int. Breastfeed. J. 2012, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, R.; Anjenaya, S.; Gujar, R. Breastfeeding practices in an urban community of Kalamboli, Navi Mumbai. Indian J. Community Med. 2004, 29, 179–180. [Google Scholar]
- Kumar, D.; Agarwal, N.; Swami, H.M. Socio demographic correlates of breastfeeding in Urban slums of Chandigarh. Indian J. Med. Sci. 2006, 60, 461–466. [Google Scholar] [PubMed]
- Joseph, N.; Unnikrishnan, B.; Naik, V.A.; Mahantshetti, N.S.; Mallapur, M.D.; Kotian, S.M.; Nelliyanil, M. Infant rearing practices in South India: A longitudinal study. J. Family Med. Prim. Care 2013, 2, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Morrow, M. Breastfeeding in Vietnam: Poverty, tradition, and economic transition. J. Hum. Lact. 1996, 12, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Escamilla, R.; Segura-Millán, S.; Canahuati, J.; Allen, H. Prelacteal feeds are negatively associated with breast-feeding outcomes in Honduras. J. Nutr. 1996, 126, 2765–2773. [Google Scholar] [PubMed]
- Onyechi, U.; Nwabuzor, L. The effect of milk formula advertisement on breast feeding and other infant feeding practice in Lagos, Nigeria. Agro Sci. J. Trop. Agric. Food Environ. Ext. 2010, 9, 193–199. [Google Scholar] [CrossRef]
- Ogbo, F.; Agho, K.E.; Page, A. Determinants of suboptimal breastfeeding practices in Nigeria: Evidence from the 2008 demographic and health survey. BMC Public Health 2015. [Google Scholar] [CrossRef] [PubMed]
- National Statistics Office Philiphines. National Demographic and Health Survey 2008; ICF Macro: Manila, Philippines, 2008.
- Qiu, L.; Xie, X.; Lee, A.; Binns, C. Infant’s first feeds in Hangzhou, P.R. China. Asia Pac. J. Clin. Nutr. 2007, 16, 458–461. [Google Scholar] [PubMed]

| Variables | 2003 N (n) | 2008 N (n) | 2013 N (n) |
|---|---|---|---|
| Community-Level Factor | |||
| Geopolitical region | |||
| North Central | 89 (32) | 380 (145) | 429 (235) |
| North East | 149 (124) | 496 (392) | 533 (387) |
| North West | 233 (184) | 818 (549) | 1020 (730) |
| South East | 35 (11) | 271 (145) | 267 (135) |
| South West | 85 (37) | 393 (205) | 277 (124) |
| South South | 67 (49) | 475 (128) | 401 (114) |
| Residence type | |||
| Urban | 180 (132) | 870 (391) | 1016 (475) |
| Rural | 478 (304) | 1961 (1174) | 1910 (1250) |
| Socio-Economic Factors | |||
| Household wealth index | |||
| Poor | 290 (205) | 975 (628) | 1096 (766) |
| Middle | 250 (161) | 1034 (581) | 1324 (748) |
| Rich | 108 (64) | 669 (281) | 467 (189) |
| Mother’s education | |||
| No education | 333 (252) | 1249 (836) | 1427 (1045) |
| Primary | 151 (88) | 625 (321) | 517 (268) |
| Secondary or higher | 175 (96) | 958 (407) | 982 (411) |
| Father’s education | |||
| No education | 254(203) | 993 (649) | 1099 (829) |
| Primary | 143 (95) | 560 (317) | 509 (281) |
| Secondary or higher | 232 (126) | 1150 (525) | 1223 (571) |
| Mother’s working status | |||
| Not working | 293 (199) | 1257 (729) | 1302 (765) |
| Working | 365 (237) | 1564 (828) | 1622 (958) |
| Maternal and Infant Factors | |||
| Mother’s age | |||
| 15–24 | 264 (180) | 947 (562) | 970 (625) |
| 25–34 | 294 (182) | 1360 (709) | 1427 (788) |
| 35–49 | 100 (74) | 524 (294) | 529 (313) |
| Mother’s perceived baby size | |||
| Small | 108 (72) | 465 (270) | 481 (324) |
| Average | 289 (188) | 1103 (652) | 1183 (740) |
| Large | 255 (173) | 1240 (635) | 1251 (653) |
| Sex | |||
| Female | 313 (204) | 1392 (755) | 1479 (857) |
| Male | 345 (233) | 1440 (810) | 1446 (868) |
| Birth order | |||
| 1 | 144 (98) | 563 (321) | 556 (319) |
| 2 to 4 | 296 (180) | 1271 (637) | 1324 (732) |
| ≥5 | 219 (159) | 998 (606) | 1045 (674) |
| Birth interval (months) | |||
| No previous birth | 144 (98) | 563 (321) | 556 (319) |
| <24 | 73 (36) | 362 (191) | 363 (220) |
| ≥24 | 441 (303) | 1900 (1051) | 2003 (1184) |
| Place of birth | |||
| Home | 455 (324) | 1765 (1115) | 1864 (1281) |
| Health facility | 203 (113) | 1067 (450) | 1062 (444) |
| Mode of delivery | |||
| Non-caesarean | 643 (427) | 2780 (1535) | 2843 (1688) |
| Caesarean | 8 (6) | 49 (29) | 57 (28) |
| Antenatal visit | |||
| None | 263 (200) | 1250 (780) | 1019 (718) |
| 1 to 3 | 98 (59) | 344 (198) | 471 (299) |
| ≥4 | 295 (177) | 1238 (586) | 1436 (708) |
| Delivery assistance | |||
| Health professional | 215 (125) | 985 (417) | 1086 (466) |
| Traditional birth attendant | 114 (82) | 576 (375) | 635 (438) |
| other unskilled worker | 236 (160) | 734 (437) | 815 (531) |
| No one | 93 (69) | 537 (336) | 390 (290) |
| Health knowledge factors | |||
| Reading magazine or newspaper | |||
| At least once a week | 48 (20) | 162 (57) | 185 (77) |
| Less than once a week | 57 (33) | 243 (110) | 225 (89) |
| Never | 545 (376) | 2344 (1366) | 2497 (1544) |
| Listening to radio | |||
| At least once a week | 163 (107) | 606 (320) | 1024 (550) |
| Less than once a week | 83 (43) | 445 (245) | 714 (385) |
| Never | 189 (140) | 996 (643) | 1177 (783) |
| Watching TV | |||
| At least once a week | 62 (42) | 355 (175) | 828 (370) |
| Less than once a week | 53 (27) | 303 (161) | 470 (224) |
| Never | 412 (288) | 1617 (1012) | 1613 (1120) |
| Characteristic | Prelacteal Feeding Rate 2003 | Prelacteal Feeding Rate 2008 | Prelacteal Feeding Rate 2013 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| % | (2008–2003) | p | % | (2013–2008) | p | % | (2013–2003) | p | |
| Community-level factor | |||||||||
| Geographical region | |||||||||
| North Central | 35.5 | 2.8 | 0.704 | 38.3 | 16.50 | <0.001 | 54.8 | 19.3 | 0.015 |
| North East | 83.1 | −4.1 | 0.292 | 79.0 | −6.40 | 0.117 | 72.6 | −10.5 | 0.035 |
| North West | 78.8 | −11.6 | 0.006 | 67.2 | 4.40 | 0.143 | 71.6 | −7.2 | 0.087 |
| South East | 31.8 | 21.7 | 0.166 | 53.5 | −2.80 | 0.609 | 50.7 | 18.9 | 0.233 |
| South West | 43.3 | 9.0 | 0.369 | 52.3 | −7.40 | 0.086 | 44.9 | 1.6 | 0.872 |
| South South | 74.3 | −48.3 | <0.001 | 26.0 | 2.30 | 0.740 | 28.3 | −46.0 | <0.001 |
| Residence type | |||||||||
| Urban | 73.7 | −28.8 | <0.001 | 44.9 | 1.90 | 0.573 | 46.8 | −26.9 | <0.001 |
| Rural | 63.6 | −3.8 | 0.368 | 59.8 | 5.60 | 0.012 | 65.4 | 1.8 | 0.674 |
| Socio-economic factors | |||||||||
| Household wealth index | |||||||||
| Poor | 70.7 | −6.3 | 0.123 | 64.4 | 5.50 | 0.055 | 69.9 | −0.8 | 0.833 |
| Middle | 64.3 | −8.1 | 0.137 | 56.2 | 0.30 | 0.916 | 56.5 | −7.8 | 0.151 |
| Rich | 59.2 | −17.1 | 0.046 | 42.1 | −1.60 | 0.679 | 40.5 | −18.7 | 0.033 |
| Mother’s education | |||||||||
| No education | 75.9 | −9.0 | 0.017 | 66.9 | 6.40 | 0.010 | 73.3 | −2.6 | 0.493 |
| Primary | 58.4 | −7.1 | 0.248 | 51.3 | 0.60 | 0.885 | 51.9 | −6.5 | 0.292 |
| Secondary or higher | 55.1 | −12.5 | 0.052 | 42.6 | −0.60 | 0.815 | 42.0 | −13.1 | 0.041 |
| Father’s education | |||||||||
| No education | 79.9 | −14.7 | <0.001 | 65.2 | 10.30 | <0.001 | 75.5 | −4.4 | 0.219 |
| Primary | 66.6 | −9.9 | 0.097 | 56.7 | −1.50 | 0.701 | 55.2 | −11.4 | 0.06 |
| Secondary or higher | 54.5 | −8.8 | 0.073 | 45.7 | 1.00 | 0.671 | 46.7 | −7.8 | 0.115 |
| Mother’s working status | |||||||||
| Not working | 68.1 | −10.1 | 0.013 | 58.0 | 0.80 | 0.748 | 58.8 | −9.3 | 0.027 |
| Working | 65.0 | −12.0 | 0.004 | 53.0 | 6.10 | 0.013 | 59.1 | −5.9 | 0.157 |
| Maternal and infant factors | |||||||||
| Mother’s age | |||||||||
| 15–24 | 68.2 | −8.9 | 0.098 | 59.3 | 5.10 | 0.062 | 64.4 | −3.8 | 0.489 |
| 25–34 | 62.2 | −10.0 | 0.017 | 52.2 | 3.00 | 0.224 | 55.2 | −7.0 | 0.109 |
| 35–49 | 73.9 | −17.9 | 0.002 | 56.0 | 3.10 | 0.388 | 59.1 | −14.8 | 0.013 |
| Mother’s perceived baby size | |||||||||
| Small | 66.4 | −8.2 | 0.277 | 58.2 | 9.20 | 0.013 | 67.4 | 1.0 | 0.901 |
| Average | 64.9 | −5.8 | 0.144 | 59.1 | 3.50 | 0.180 | 62.6 | −2.3 | 0.551 |
| Large | 67.9 | −16.7 | <0.001 | 51.2 | 1.00 | 0.691 | 52.2 | −15.7 | 0.001 |
| Sex | |||||||||
| Female | 65.2 | −11.0 | 0.004 | 54.2 | 3.70 | 0.119 | 57.9 | −7.3 | 0.069 |
| Male | 67.4 | −11.2 | 0.014 | 56.2 | 3.80 | 0.103 | 60.0 | −7.4 | 0.103 |
| Birth order | |||||||||
| 1 | 68.0 | −10.9 | 0.148 | 57.1 | 0.30 | 0.941 | 57.4 | −10.6 | 0.166 |
| 2 to 4 | 60.7 | −10.6 | 0.024 | 50.1 | 5.20 | 0.045 | 55.3 | −5.4 | 0.260 |
| ≥5 | 72.9 | −12.1 | 0.005 | 60.8 | 3.70 | 0.161 | 64.5 | −8.4 | 0.058 |
| Birth interval (months) | |||||||||
| No previous birth | 68.0 | −10.9 | 0.148 | 57.1 | 0.30 | 0.941 | 57.4 | −10.6 | 0.166 |
| <24 | 49.7 | 3.0 | 0.768 | 52.7 | 7.40 | 0.078 | 60.1 | 10.4 | 0.287 |
| ≥24 | 68.6 | −13.2 | <0.001 | 55.4 | 3.70 | 0.084 | 59.1 | −9.5 | 0.009 |
| Place of birth | |||||||||
| Home | 71.2 | −8.0 | 0.022 | 63.2 | 5.50 | 0.008 | 68.7 | −2.5 | 0.478 |
| Health facility | 55.5 | −13.3 | 0.032 | 42.2 | −0.40 | 0.904 | 41.8 | −13.7 | 0.029 |
| Mode of delivery | |||||||||
| Non-caesarean | 66.3 | −11.1 | 0.001 | 55.2 | 4.20 | 0.026 | 59.4 | −6.9 | 0.043 |
| Caesarean | 92.7 | −34.4 | 0.002 | 58.3 | −8.70 | 0.438 | 49.6 | −43.1 | <0.001 |
| Antenatal visit | |||||||||
| None | 76.1 | −13.7 | 0.001 | 62.4 | 8.10 | 0.003 | 70.5 | −5.6 | 0.181 |
| 1 to 3 | 60.6 | −2.8 | 0.721 | 57.8 | 5.60 | 0.182 | 63.4 | 2.8 | 0.713 |
| ≥4 | 60.1 | −12.8 | 0.009 | 47.3 | 2.00 | 0.42 | 49.3 | −10.8 | 0.026 |
| Delivery assistance | |||||||||
| Health professional | 58.2 | −15.9 | 0.007 | 42.3 | 0.60 | 0.828 | 42.9 | −15.3 | 0.009 |
| Traditional birth attendant | 71.7 | −6.5 | 0.319 | 65.2 | 3.80 | 0.291 | 69.0 | −2.7 | 0.676 |
| other unskilled worker | 68.0 | −8.5 | 0.075 | 59.5 | 5.70 | 0.069 | 65.2 | −2.8 | 0.559 |
| No one | 74.5 | −12.0 | 0.053 | 62.5 | 11.80 | 0.001 | 74.3 | −0.2 | 0.984 |
| Health knowledge factors | |||||||||
| Reading magazine or newspaper | |||||||||
| At least once a week | 41.3 | −6.0 | 0.649 | 35.3 | 6.50 | 0.285 | 41.8 | 0.5 | 0.968 |
| Less than once a week | 58.4 | −13.2 | 0.142 | 45.2 | −5.80 | 0.301 | 39.4 | −19.0 | 0.036 |
| Never | 69.0 | −10.7 | 0.001 | 58.3 | 3.50 | 0.073 | 61.8 | −7.2 | 0.026 |
| Listening to radio | |||||||||
| At least once a week | 65.7 | −12.8 | 0.018 | 52.9 | 0.90 | 0.788 | 53.8 | −11.9 | 0.024 |
| Less than once a week | 52.4 | 2.8 | 0.702 | 55.2 | −1.20 | 0.743 | 54.0 | 1.6 | 0.824 |
| Never | 74.2 | −9.7 | 0.031 | 64.5 | 2.00 | 0.481 | 66.5 | −7.7 | 0.098 |
| Watching TV | |||||||||
| At least once a week | 68.1 | −18.7 | 0.034 | 49.4 | −4.70 | 0.248 | 44.7 | −23.4 | 0.006 |
| Less than once a week | 51.5 | 1.7 | 0.869 | 53.2 | −5.60 | 0.193 | 47.6 | −3.9 | 0.701 |
| Never | 70.0 | −7.4 | 0.055 | 62.6 | 6.90 | 0.003 | 69.5 | −0.5 | 0.887 |
| Variables | Unadjusted | Adjusted ^,* |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Year of survey | ||
| 2003 | Ref | Ref |
| 2008 | 0.63 (0.47–0.83) | 0.72 (0.54–0.97) |
| 2013 | 0.73 (0.54–0.98) | 0.79 (0.58–1.06) |
| Geographical region | ||
| South South | Ref | Ref |
| North East | 7.34 (5.41–9.97) | 4.77 (3.41–6.66) |
| North West | 5.38 (4.21–6.89) | 3.31 (2.50–4.39) |
| South East | 2.32 (1.71–3.14) | 2.53 (1.83–3.48) |
| South West | 2.11 (1.61–2.78) | 1.98 (1.48–2.65) |
| North Central | 1.90 (1.43–2.52) | 1.47 (1.11–1.95) |
| Residence type | ||
| Urban | Ref | |
| Rural | 1.80 (1.54–2.10) | |
| Household wealth index | ||
| Poor | Ref | |
| Middle | 0.64 (0.55–0.74) | |
| Rich | 0.36 (0.30–0.43) | |
| Mother’s education | ||
| Secondary or higher | Ref | Ref |
| Primary | 1.44 (1.22–1.71) | 1.13 (0.94–1.37) |
| No education | 3.20 (2.72–3.75) | 1.65 (1.33–2.03) |
| Father’s education | ||
| Secondary or higher | Ref | |
| Primary | 1.51 (1.28–1.78) | |
| No education | 2.86 (2.45–3.35) | |
| Mother’s working status | ||
| Not working | Ref | Ref |
| Working | 0.91 (0.80–1.03) | 1.26 (1.10–1.44) |
| Mother’s age | ||
| 35–49 | Ref | Ref |
| 15–24 | 1.17 (0.99–1.38) | 1.31 (1.04–1.64) |
| 25–34 | 0.83 (0.71–0.97) | 1.02 (0.86–1.21) |
| Mother’s perceived baby size | ||
| Small | Ref | |
| Average | 0.92 (0.78–1.10) | |
| Large | 0.66 (0.55–0.79) | |
| Sex | ||
| Male | Ref | |
| Female | 0.92 (0.82–1.03) | |
| Birth order | ||
| 2 to 4 | Ref | Ref |
| 1 to 3 | 1.22 (1.03–1.44) | 1.25 (1.03–1.52) |
| ≥5 | 1.52 (1.33–1.73) | 1.18 (1.00–1.39) |
| Birth interval (months) | ||
| No previous birth | Ref | |
| <24 | 0.90 (0.72–1.14) | |
| ≥24 | 1.00 (0.85–1.17) | |
| Place of birth | ||
| Health facility | Ref | Ref |
| Home | 2.62 (2.29–3.01) | 1.45 (1.23–1.71) |
| Mode of delivery | ||
| Non-caesarean | Ref | Ref |
| Caesarean | 0.91 (0.58–1.43) | 1.91 (1.17–3.13) |
| Antenatal visit | ||
| None | Ref | |
| 1 to 3 | 0.77 (0.63–0.94) | |
| ≥4 | 0.48 (0.42–0.56) | |
| Delivery assistance | ||
| Health professional | Ref | |
| Traditional birth attendance (TBA) | 2.64 (2.19–3.19) | |
| other unskilled worker | 2.18 (1.86–2.55) | |
| No one | 2.71 (2.23–3.30) | |
| Reading magazine or newspaper | ||
| At least once a week | Ref | |
| Less than once a week | 1.23 (0.89–1.70) | |
| Never | 2.43 (1.88–3.15) | |
| Listening to radio | ||
| At least once a week | Ref | |
| Less than once a week | 0.99 (0.83–1.19) | |
| Never | 1.64 (1.39–1.93) | |
| Watching television | ||
| At least once a week | Ref | |
| Less than once a week | 1.12 (0.90–1.38) | |
| Never | 2.22 (1.87–2.64) | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agho, K.E.; Ogeleka, P.; Ogbo, F.A.; Ezeh, O.K.; Eastwood, J.; Page, A. Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013). Nutrients 2016, 8, 462. https://doi.org/10.3390/nu8080462
Agho KE, Ogeleka P, Ogbo FA, Ezeh OK, Eastwood J, Page A. Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013). Nutrients. 2016; 8(8):462. https://doi.org/10.3390/nu8080462
Chicago/Turabian StyleAgho, Kingsley E., Pascal Ogeleka, Felix A. Ogbo, Osita K. Ezeh, John Eastwood, and Andrew Page. 2016. "Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013)" Nutrients 8, no. 8: 462. https://doi.org/10.3390/nu8080462
APA StyleAgho, K. E., Ogeleka, P., Ogbo, F. A., Ezeh, O. K., Eastwood, J., & Page, A. (2016). Trends and Predictors of Prelacteal Feeding Practices in Nigeria (2003–2013). Nutrients, 8(8), 462. https://doi.org/10.3390/nu8080462