Effect of a Partially Hydrolysed Whey Infant Formula Supplemented with Starch and Lactobacillus reuteri DSM 17938 on Regurgitation and Gastric Motility
Abstract
:1. Introduction
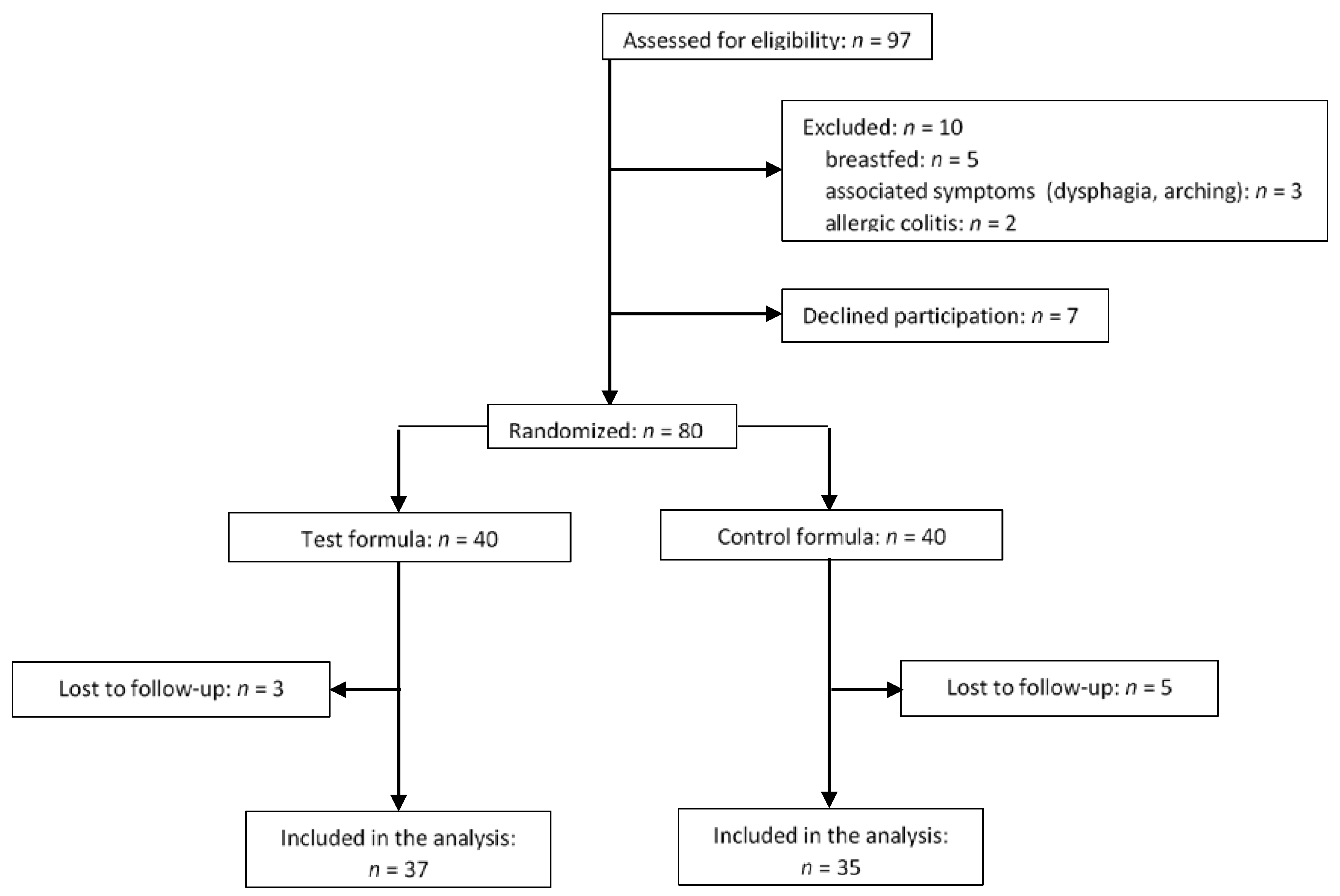
2. Methods
2.1. Study Population
2.2. Study Design
2.3. Outcome Evaluation
2.4. Statistical Analysis
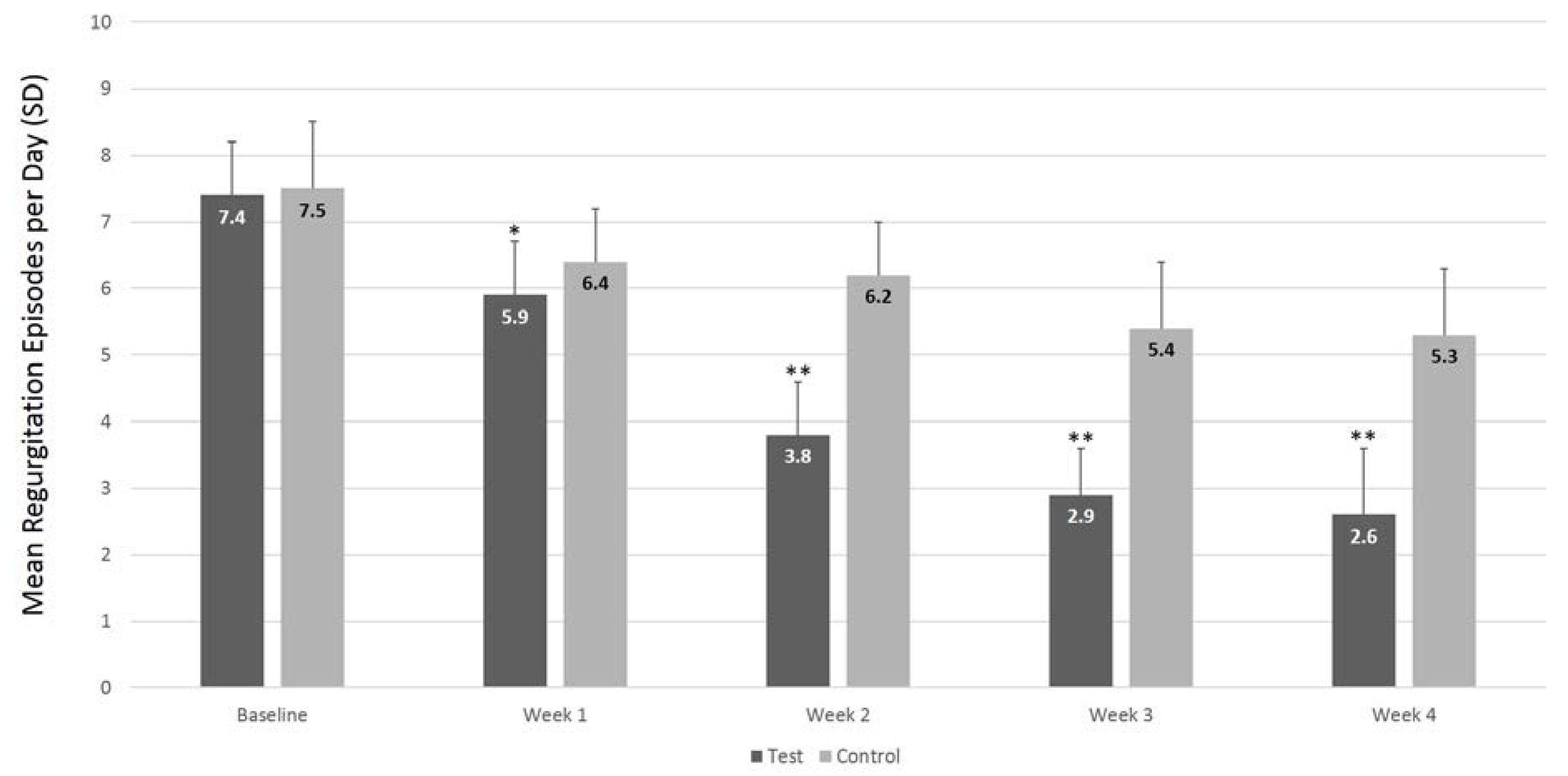
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sherman, P.M.; Hassall, E.; Fagundes-Neto, U. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am. J. Gastroenterol. 2009, 104, 1278–1295. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.P.; Chen, E.H.; Syniar, G.M.; Christoffel, K.K. Prevalence of symptoms of gastroesophageal reflux during infancy: A pediatric practice-based survey. Pediatric Practice Research Group. Arch. Pediatr. Adolesc. Med. 1997, 151, 569–572. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Rudolph, C.D.; Di Lorenzo, C. Pediatric gastroesophageal reflux clinical practice guidelines: Joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 498–547. [Google Scholar] [PubMed]
- Henry, S.M. Discerning differences: Gastroesophageal reflux and gastroesophageal reflux disease in infants. Adv. Neonatal Care 2004, 4, 235–247. [Google Scholar] [CrossRef] [PubMed]
- Smart, J.; Hiscock, H. Early infant crying and sleeping problems: A pilot study of impact on parental well-being and parent-endorsed strategies for management. J. Paediatr. Child Health 2007, 43, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Di Mauro, A.; Di Mauro, A. Prevention of functional gastrointestinal disorders in neonates: Clinical and socioeconomic impact. Benef. Microbes 2015, 6, 195–198. [Google Scholar] [CrossRef] [PubMed]
- Iacono, G.; Merolla, R.; D’Amico, D. Gastrointestinal symptoms in infancy: A population-based prospective study. Dig. Liver Dis. 2005, 37, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Brown, P. Medical management of gastroesophageal reflux. Curr. Opin. Pediatr. 2000, 12, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Lightdale, J.R.; Gremse, D.A. Section on gastroenterology, hepatology, and nutrition. gastroesophageal reflux: management guidance for the pediatrician. Pediatrics 2013, 131, e1684–e1695. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Alarcon, P.; Alliet, P. Algorithms for managing infant constipation, colic, regurgitation and cow’s milk allergy in formula-fed infants. Acta Paediatr. 2015, 104, 449–457. [Google Scholar] [CrossRef] [PubMed]
- Davies, I.; Burman-Roy, S.; Murphy, M.S. Gastro-oesophageal reflux disease in children: NICE guidance. BMJ 2015, 350, g7703. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Leluyer, B.; Cazaubiel, M.; Housez, B.; Bocquet, A. Double-blind comparative trial with 2 antiregurgitation formulae. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Perez-Burgos, A.; Wang, L.; McVey Neufeld, K.-A. The TRPV1 channel in rodents is a major target for antinociceptive effect of the probiotic Lactobacillus reuteri DSM 17938. J. Physiol. 2015, 593, 3943–3957. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Riezzo, G.; Raimondi, F.; Bisceglia, M.; Cavallo, L.; Francavilla, R. The effects of probiotics on feeding tolerance, bowel habits, and gastrointestinal motility in preterm newborns. J. Pediatr. 2008, 152, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Di Mauro, A.; Riezzo, G.; Civardi, E.; Intini, C.; Corvaglia, L.; Ballardini, E.; Bisceglia, M.; Cinquetti, M.; Brazzoduro, E.; et al. Prophylactic use of a probiotic in the prevention of colic, regurgitation, and functional constipation: A randomized clinical trial. JAMA Pediatr. 2014, 168, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Benninga, M.A.; Nurko, S.; Faure, C.; Hyman, P.E.; St. James Roberts, I.; Schechter, N.L. Childhood functional gastrointestinal disorders: Neonate/toddler. Gastroenterology 2016, 150, 1443–1455. [Google Scholar] [CrossRef] [PubMed]
- Hyman, P.E.; Milla, P.J.; Benninga, M.A.; Davidson, G.P.; Fleisher, D.F.; Taminiau, J. Childhood functional gastrointestinal disorders: Neonate/toddler. Gastroenterology 2006, 130, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Svedlund, J.; Sjodin, I.; Dotevall, G. GSRS—A clinical rating scale for gastrointestinal symptoms in patients with irritable bowel syndrome and peptic ulcer disease. Dig. Dis. Sci. 1988, 33, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Bolondi, L.; Gaiani, S.; Barbara, L. Ecografia Funzionale Ed Ecodoppler in Gastroenterologia; Masson: Milano, Italy, 1989. [Google Scholar]
- Darwiche, G.; Björgell, O.; Thorsson, O.; Almér, L.-O. Correlation between simultaneous scintigraphic and ultrasonographic measurement of gastric emptying in patients with type 1 diabetes mellitus. J. Ultrasound Med. 2003, 22, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Singendonk, M.M.J.; Rommel, N.; Omari, T.I.; Benninga, M.A.; van Wijk, M.P. Upper gastrointestinal motility: Prenatal development and problems in infancy. Nat. Rev. Gastroenterol. Hepatol. 2014, 11, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Massey, B.T.; Simuncak, C.; LeCapitaine–Dana, N.J.; Pudur, S. Transient lower esophageal sphincter relaxations do not result from passive opening of the cardia by gastric distention. Gastroenterology 2006, 130, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Penagini, R.; Carmagnola, S.; Cantù, P.; Allocca, M.; Bianchi, P.A. Mechanoreceptors of the proximal stomach: Role in triggering transient lower esophageal sphincter relaxation. Gastroenterology 2004, 126, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Davidson, G. The role of lower esophageal sphincter function and dysmotility in gastroesophageal reflux in premature infants and in the first year of life. J. Pediatr. Gastroenterol. Nutr. 2003, 37 (Suppl. 1), S17–S22. [Google Scholar] [CrossRef] [PubMed]
- Guarino, M.P.L.; Cicala, M.; Putignani, L.; Severi, C. Gastrointestinal neuromuscular apparatus: An underestimated target of gut microbiota. World J. Gastroenterol. 2016, 22, 9871. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Riezzo, G.; Raimondi, F. Lactobacillus reuteri accelerates gastric emptying and improves regurgitation in infants. Eur. J. Clin. Investig. 2011, 41, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Hyams, J.S.; Treem, W.R.; Etienne, N.L. Effect of infant formula on stool characteristics of young infants. Pediatrics 1995, 95, 50–54. [Google Scholar] [PubMed]
- Mihatsch, W.A.; Franz, A.R.; Högel, J.; Pohlandt, F. Hydrolyzed protein accelerates feeding advancement in very low birth weight infants. Pediatrics 2002, 110, 1199–1203. [Google Scholar] [CrossRef] [PubMed]
- Riezzo, G.; Indrio, F.; Montagna, O. Gastric electrical activity and gastric emptying in preterm newborns fed standard and hydrolysate formulas. J. Pediatr. Gastroenterol. Nutr. 2001, 33, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Tolia, V.; Lin, C.H.; Kuhns, L.R. Gastric emptying using three different formulas in infants with gastroesophageal reflux. J. Pediatr. Gastroenterol. Nutr. 1992, 15, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Billeaud, C.; Guillet, J.; Sandler, B. Gastric emptying in infants with or without gastro-oesophageal reflux according to the type of milk. Eur. J. Clin. Nutr. 1990, 44, 577–583. [Google Scholar] [PubMed]
- Staelens, S.; Van den Driessche, M.; Barclay, D. Gastric emptying in healthy newborns fed an intact protein formula, a partially and an extensively hydrolysed formula. Clin. Nutr. 2008, 27, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Vandenplas, Y.; Cruchet, S.; Faure, C. When should we use partially hydrolysed formulae for frequent gastrointestinal symptoms and allergy prevention? Acta Paediatr. 2014, 103, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Savino, F.; Cresi, F.; Maccario, S. “Minor” feeding problems during the first months of life: Effect of a partially hydrolysed milk formula containing fructo- and galacto-oligosaccharides. Acta Paediatr. 2003, 91, 86–90. [Google Scholar] [CrossRef]
- Underwood, M.A.; German, J.B.; Lebrilla, C.B.; Mills, D.A. Bifidobacterium longum subspecies infantis: Champion colonizer of the infant gut. Pediatr. Res. 2015, 77, 229–235. [Google Scholar] [CrossRef] [PubMed]
- De Leoz, M.L.; Kalanetra, K.M.; Bokulich, N.A. Human milk glycomics and gut microbial genomics in infant feces show a correlation between human milk oligosaccharides and gut microbiota: A proof-of-concept study. J. Proteome Res. 2015, 14, 491–502. [Google Scholar] [CrossRef] [PubMed]
- Indrio, F.; Di Mauro, A.; Riezzo, G.; Cavallo, L.; Francavilla, R. Infantile colic, regurgitation, and constipation: An early traumatic insult in the development of functional gastrointestinal disorders in children? Eur. J. Pediatr. 2015, 174, 841–842. [Google Scholar] [CrossRef] [PubMed]
| Test (n = 37) | Control (n = 35) | p-Value | |||
|---|---|---|---|---|---|
| Week 0 | Week 4 | Week 0 | Week 4 | ||
| Fasting antral area, cm2 | 2.7 (2.0, 3.1) | 3.5 (2.0–4.6) | 2.7 (1.4, 3.1) | 4.6 (2.4, 6.0) | 0.01 a |
| GErate percent change from week 0 to week 4, % | 12.3 (−3.9, 22.0) | 9.1 (−27.0, 25.5) | <0.01 b | ||
| Test (n = 37) | Control (n = 35) | p-Value a | |||
|---|---|---|---|---|---|
| Week 0 | Week 4 | Week 0 | Week 4 | ||
| Age, days | 59 ± 8.2 | 92 ± 4.3 | 60 ± 5.3 | 93 ± 3.3 | NS |
| Weight, g | 5590 ± 631 | 6280 ± 391 | 5670 ± 739 | 6320 ± 239 | NS |
| Length, cm | 53.7 ± 1.8 | 58.1 ± 0.8 | 54.1 ± 1.5 | 57.7 ± 1.1 | NS |
| Head circumference, cm | 40.8 ± 1.3 | 42.3 ± 0.3 | 39.7 ± 1.1 | 41.8 ± 0.7 | NS |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Indrio, F.; Riezzo, G.; Giordano, P.; Ficarella, M.; Miolla, M.P.; Martini, S.; Corvaglia, L.; Francavilla, R. Effect of a Partially Hydrolysed Whey Infant Formula Supplemented with Starch and Lactobacillus reuteri DSM 17938 on Regurgitation and Gastric Motility. Nutrients 2017, 9, 1181. https://doi.org/10.3390/nu9111181
Indrio F, Riezzo G, Giordano P, Ficarella M, Miolla MP, Martini S, Corvaglia L, Francavilla R. Effect of a Partially Hydrolysed Whey Infant Formula Supplemented with Starch and Lactobacillus reuteri DSM 17938 on Regurgitation and Gastric Motility. Nutrients. 2017; 9(11):1181. https://doi.org/10.3390/nu9111181
Chicago/Turabian StyleIndrio, Flavia, Giuseppe Riezzo, Paola Giordano, Maria Ficarella, Maria Paola Miolla, Silvia Martini, Luigi Corvaglia, and Ruggiero Francavilla. 2017. "Effect of a Partially Hydrolysed Whey Infant Formula Supplemented with Starch and Lactobacillus reuteri DSM 17938 on Regurgitation and Gastric Motility" Nutrients 9, no. 11: 1181. https://doi.org/10.3390/nu9111181





