Knowledge, Attitude, and Practice (KAP) of Dairy Products in Chinese Urban Population and the Effects on Dairy Intake Quality
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
2.3. Ethics
2.4. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics of Participants
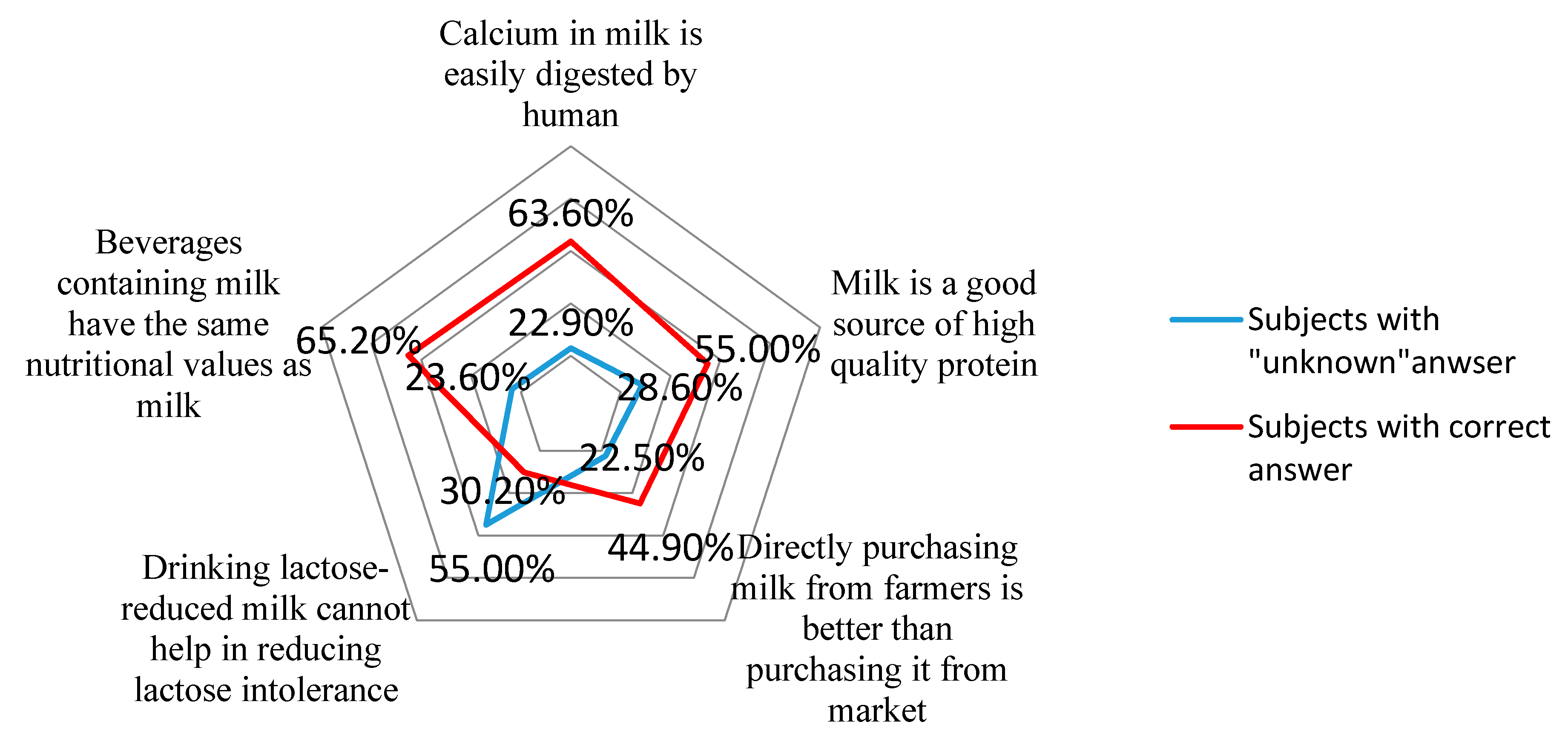
3.2. Knowledge of Dairy among Participants
3.3. Attitude toward Dairy Products among Participants
3.4. Diet Quality and Associated Predictors
4. Discussion
4.1. Knowledge of Dairy Products
4.2. Attitude toward Dairy Products
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- 2015–2020 Dietary Guidelines for Americans, 8th ed. Available online: https://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 14 December 2016).
- Chinese Nutrition Association. Dietary Guidelines for Chinese Residents 2016; People’s Medical Publishing House: Beijing, China, 2016; p. 3. [Google Scholar]
- Rozenberg, S.; Body, J.J.; Bruyere, O.; Bergmann, P.; Brandi, M.L.; Cooper, C.; Devogelaer, J.P.; Gielen, E.; Goemaere, S.; Kaufman, J.M.; et al. Effects of dairy products consumption on health: Benefits and beliefs—A commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif. Tissue Int. 2016, 98, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Gao, D.; Ning, N.; Wang, C.; Wang, Y.; Li, Q.; Meng, Z.; Liu, Y.; Li, Q. Dairy products consumption and risk of type 2 diabetes: Systematic review and dose-response meta-analysis. PLoS ONE 2013, 8, e73965. [Google Scholar] [CrossRef] [PubMed]
- Doidge, J.C.; Segal, L.; Gospodarevskaya, E. Attributable risk analysis reveals potential healthcare savings from increased consumption of dairy products. J. Nutr. 2012, 142, 1772–1780. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Szeto, I.M.Y.; Chen, L.; Han, S.; Li, Y.; Hekezen, R.; Qin, L.Q. Dairy products consumption and metabolic syndrome in adults: Systematic review and meta-analysis of observational studies. Sci. Rep. 2015, 5, 14606. [Google Scholar] [CrossRef] [PubMed]
- McGrane, M.M.; Essery, E.; Obbagy, J.; Lyon, J.; Macneil, P.; Spahn, J.; Van Horn, L. Dairy consumption, blood pressure, and risk of hypertension: An evidence-based review of recent literature. Curr. Cardiovasc. Risk Rep. 2011, 5, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Wu, Y.; Zhang, X.; Zhang, M.; Huang, G. Dietary changes over 25 years in Tianjin residents: Findings from the 1986–1988, 2000–2004, and 2008–2011 nutrition surveys. Nutrients 2016, 8, 62. [Google Scholar] [CrossRef] [PubMed]
- Zhao, A.; Xue, Y.; Zhang, Y.; Li, W.; Yu, K.; Wang, P. Nutrition concerns of insufficient and excessive intake of dietary minerals in lactating women: A cross-sectional survey in three cities of China. PLoS ONE 2016, 11, e146483. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, A. Adaptation to lactose in lactase non persistent people: Effects on intolerance and the relationship between dairy food consumption and evaluation of diseases. Nutrients 2015, 7, 6751–6779. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P. Dairy intake, dietary adequacy, and lactose intolerance. Adv. Nutr. 2013, 4, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.G.; Yan, Y.S.; Xu, J.J.; Du, R.F.; Flatz, S.D.; Kuhnau, W.; Flatz, G. Prevalence of primary adult lactose malabsorption in three populations of northern China. Hum. Genet. 1984, 67, 103–106. [Google Scholar] [PubMed]
- Yang, Y.X.; He, M.; Cui, H.M.; Bian, L.H.; Jianyu, L.; Cheng, W.F; Xu, H.F.; Feng, W. Study on the incidence of lactose intolerance of children in China. J. Hyg. Res. 1999, 28, 44–46. [Google Scholar]
- Deng, Y.; Misselwitz, B.; Dai, N.; Fox, M. Lactose intolerance in adults: Biological mechanism and dietary management. Nutrients 2015, 7, 8020–8035. [Google Scholar] [CrossRef] [PubMed]
- Alkerwi, A.; Sauvageot, N.; Malan, L.; Shivappa, N.; Hebert, J.R. Association between nutritional awareness and diet quality: Evidence from the observation of cardiovascular risk factors in Luxembourg (ORISCAV-LUX) study. Nutrients 2015, 7, 2823–2838. [Google Scholar] [CrossRef] [PubMed]
- Ahadi, Z.; Heshmat, R.; Sanaei, M.; Shafiee, G.; Ghaderpanahi, M.; Rezaei, H.M.; Salehi, F.; Abdollahi, Z.; Azemati, B.; Larijani, B. Knowledge, attitude and practice of urban and rural households towards principles of nutrition in Iran: Results of NUTRIKAP survey. J. Diabetes Metab. Disord. 2014, 13, 100. [Google Scholar] [CrossRef] [PubMed]
- Naghashpour, M.; Shakerinejad, G.; Lourizadeh, M.R.; Hajinajaf, S.; Jarvandi, F. Nutrition education based on health belief model improves dietary calcium intake among female students of junior high schools. J. Health Popul. Nutr. 2014, 32, 420–429. [Google Scholar] [PubMed]
- Yang, Y. China Food Composition, 2nd ed.; Peking University Medical Press: Beijing, China, 2009. [Google Scholar]
- Chinese Nutrition Association. Chinese Dietary Reference Intakes (2013); Science Press: Beijing, China, 2014. [Google Scholar]
- Masuku, S.K.; Lan, S.J. Nutritional knowledge, attitude, and practices among pregnant and lactating women living with HIV in the Manzini region of Swaziland. J. Health Popul. Nutr. 2014, 32, 261–269. [Google Scholar] [PubMed]
- Son, S.; Ro, Y.; Hyun, H.; Lee, H.; Song, K. A comparative study on dietary behavior, nutritional knowledge and life stress between Korean and Chinese female high school students. Nutr. Res. Pract. 2014, 2, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.J.; Chen, X.M.; Li, H.W.; Luo, H. A study of nutritional knowledge, attitude and dietary behavior of students in a medical college (In Chinese). Mod. Prev. Med. 2007, 34, 794–795. [Google Scholar]
- Sharma, S.V.; Hoelscher, D.M.; Kelder, S.H.; Diamond, P.; Day, R.S.; Hergenroeder, A. Psychosocial factors influencing calcium intake and bone quality in middle school girls. J. Am. Diet. Assoc. 2010, 110, 932–936. [Google Scholar] [CrossRef] [PubMed]
- Girois, S.B.; Kumanyika, S.K.; Morabia, A.; Mauger, E. A comparison of knowledge and attitudes about diet and health among 35- to 75-year-old adults in the United States and Geneva, Switzerland. Am. J. Health Popul. 2001, 91, 418–424. [Google Scholar]
- Shrier, I.; Szilagyi, A.; Correa, J.A. Impact of lactose containing foods and the genetics of lactase on diseases: An analytical review of population data. Nutr. Cancer 2008, 60, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.H.; Liu, S.G.; Gao, R. Application of biotechnology in the prevention and control of lactose intolerance (in Chinese). China Dairy Ind. 2002, 30, 44–47. [Google Scholar]
| N | % | ||
|---|---|---|---|
| City level | First-tier cities | 654 | 38.2 |
| Non–first tier cities | 1060 | 61.8 | |
| Gender | Male | 582 | 34.0 |
| Female | 1132 | 66.0 | |
| Age | 18–44 years | 634 | 37.0 |
| 45–64 years | 578 | 33.7 | |
| ≥65 years | 502 | 29.3 | |
| Education | Junior high school or below | 565 | 33.1 |
| Senior high school | 704 | 41.2 | |
| Bachelor’s degree or above | 439 | 25.7 | |
| Family monthly income (RMB: yuan) | <3000 | 361 | 21.2 |
| 3000–4999 | 489 | 28.7 | |
| 5000–7999 | 367 | 21.5 | |
| ≥8000 | 488 | 28.6 | |
| Family monthly expenditure on food (RMB: yuan) | <1000 | 511 | 29.9 |
| 1000–2999 | 880 | 51.4 | |
| ≥3000 | 320 | 18.8 | |
| Average personal monthly expenditure on dairy products (RMB: yuan) | <10 | 423 | 24.7 |
| 11–50 | 479 | 28.0 | |
| >100 | 810 | 47.3 |
| Indicator Variable | ORs | 95% CI | p | |
|---|---|---|---|---|
| City level | First-tier cities | −0.04 | −0.25, 0.16 | 0.691 |
| Non–first tier cities | ||||
| Gender | Male | −0.24 | −0.44, −0.05 | 0.016 |
| Female | ||||
| Age | 18–44 years | 0.18 | −0.08, 0.45 | 0.169 |
| 45–64 years | 0.19 | −0.04, 0.42 | 0.111 | |
| ≥65 years | ||||
| Education | Junior high school or below | −1.20 | −1.50, −0.90 | <0.001 |
| Senior high school | −0.36 | −0.61, −0.13 | 0.004 | |
| Bachelor’s degree or above | ||||
| Family monthly income (RMB: yuan) | <3000 | −0.35 | −0.66, −0.05 | 0.024 |
| 3000–4999 | −0.13 | −0.40, 0.13 | 0.328 | |
| 5000–7999 | −0.17 | −0.44, 0.10 | 0.229 | |
| ≥8000 | ||||
| Family monthly expenditure on food (RMB: yuan) | <1000 | −0.34 | −0.65, −0.03 | 0.033 |
| 1000–2999 | −0.00 | −0.26, 0.27 | 0.975 | |
| ≥3000 | ||||
| Average personal monthly expenditure on dairy products (RMB: yuan) | <10 | −0.35 | −0.59, −0.20 | 0.006 |
| 11–50 | 0.03 | −0.24, 0.30 | 0.827 | |
| >100 | ||||
| Dairy Product and Nutrients Intake | Score of Dairy Knowledge | p | Self-Reception of LI-Related Symptoms | p | |||||
|---|---|---|---|---|---|---|---|---|---|
| −4 to 0 | 1 to 3 | 4 to 6 | Yes | No | Unsure | ||||
| N = 478 | N = 695 | N = 523 | N = 260 | N = 1289 | N = 165 | ||||
| Total dairy products (g/day) | Mean | 77.8 | 118.5 | 136.5 | 78.5 | 125.5 | 66.1 | ||
| Median (25th, 75th) | 8.6 (0.0, 107.1) | 85.7 (0.0, 200.0) | 107.1 (25.0, 220.0) | <0.001 | 21.4 (0.0, 107.1) | 96.4 (8.3, 220.0) | 0.0 (0.0, 0.0) | <0.001 | |
| Low fat and fat-free dairy products (g/day) | Mean | 13.9 | 16.2 | 20.0 | 22.3 | 15.5 | 19.9 | ||
| Median (25th, 75th) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.002 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.146 | |
| Yogurt intake (g/day) | Mean | 13.9 | 16.2 | 20.0 | 28.8 | 27.5 | 16.5 | ||
| Median (25th, 75th) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.595 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.771 | |
| Lactose-reduced dairy products (g/day) | Mean | 1.9 | 3.0 | 1.3 | 2.6 | 2.3 | 0.6 | ||
| Median (25th, 75th) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.595 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.671 | |
| Predictors | Unstandardized Coefficient | 95% (CI) | t | p |
|---|---|---|---|---|
| Calcium (mg/day) | ||||
| Model 1 a | 36.3 | (5.3, 67.3) | 2.294 | 0.022 |
| Model 2 b | 25.6 | (−5.8, 57.0) | 1.598 | 0.110 |
| Protein (g/day) | ||||
| Model 1 a | 1.84 | (−0.07, 3.76) | 1.886 | 0.059 |
| Model 2 b | 1.45 | (−0.49, 3.40) | 1.467 | 0.147 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, A.; Szeto, I.M.-Y.; Wang, Y.; Li, C.; Pan, M.; Li, T.; Wang, P.; Zhang, Y. Knowledge, Attitude, and Practice (KAP) of Dairy Products in Chinese Urban Population and the Effects on Dairy Intake Quality. Nutrients 2017, 9, 668. https://doi.org/10.3390/nu9070668
Zhao A, Szeto IM-Y, Wang Y, Li C, Pan M, Li T, Wang P, Zhang Y. Knowledge, Attitude, and Practice (KAP) of Dairy Products in Chinese Urban Population and the Effects on Dairy Intake Quality. Nutrients. 2017; 9(7):668. https://doi.org/10.3390/nu9070668
Chicago/Turabian StyleZhao, Ai, Ignatius Man-Yau Szeto, Yan Wang, Ce Li, Min Pan, Ting Li, Peiyu Wang, and Yumei Zhang. 2017. "Knowledge, Attitude, and Practice (KAP) of Dairy Products in Chinese Urban Population and the Effects on Dairy Intake Quality" Nutrients 9, no. 7: 668. https://doi.org/10.3390/nu9070668





