Bacillus anthracis, “la maladie du charbon”, Toxins, and Institut Pasteur
Abstract
:1. Introduction
This section mainly relies on the archives kept at the Centre de ressources en information scientifique (CeRIS) at Institut Pasteur. As archival research is never completed, there is an opportunity for further studies in this domain (for editorial reasons, the footnotes have been inserted into the text; they can be read or skipped according to readers’ preference).
Pasteur and Koch were engaged, at the time, in a fierce scientific competition in the nascent field of microbiology. Many factors interfered, leading to this clash of personalities: their age, scientific recognition, and the language barrier with unfortunate consequences ranging from a lack of knowledge of prior publications to deep misunderstandings (such as during the September 1882 Geneva congress), not forgetting the political context after the Franco-Prussian 1870 war. These details come from the highly informative book on the interactions between Pasteur and Koch, which is available in French [2] with a German translation [3]; an English translation would be invaluable for the scientific community.
Rabies was a frightening disease that struck people’s imagination. As a zoonosis transmissible to humans, it was an ideal research field for Louis Pasteur for the application of the notion of pathogen attenuation to vaccination. This research was developed in Pasteur’s laboratory, then in École Normale rue d’Ulm in Paris, from 1880 until the first human vaccinations of Joseph Meister and Jean-Baptiste Jupille [6].
2. The First Golden Age of B. anthracis Research: The Vaccines
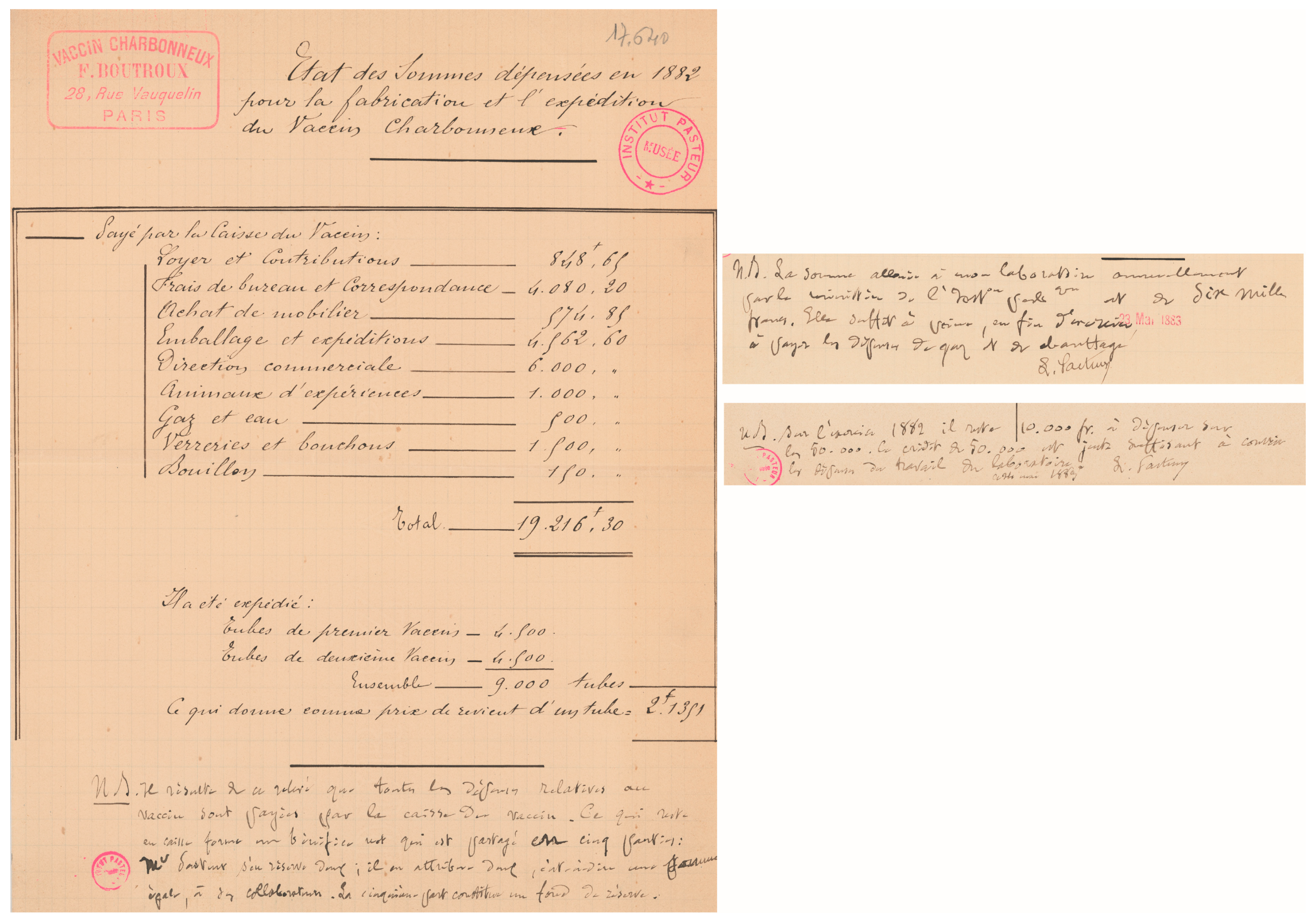
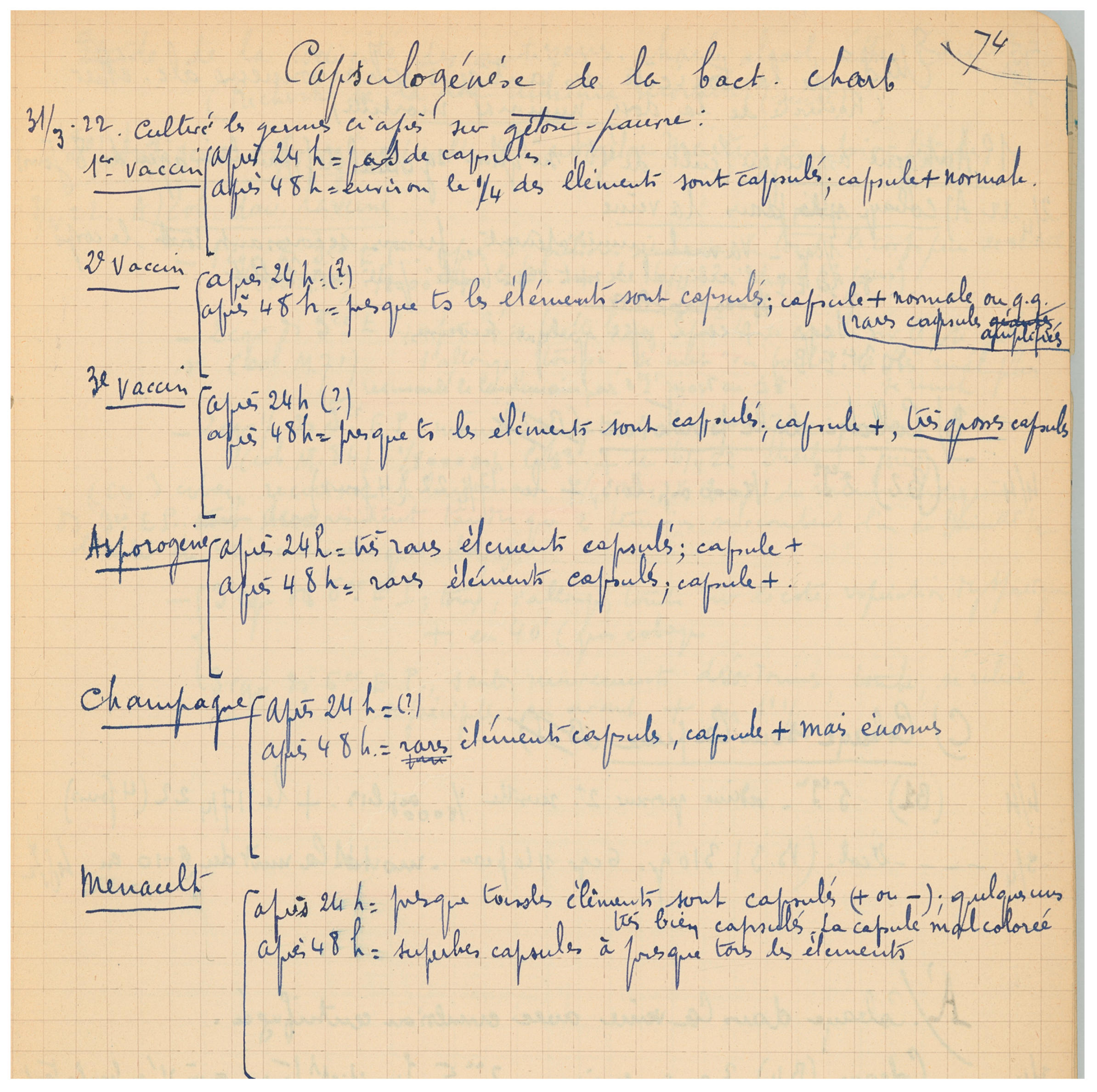
Pasteur initiated his research on B. anthracis in 1877 at École Normale. From the archives at Musée Pasteur, it appears that the “vaccin charbonneux” was produced as early as 1882 on premises rue Vauquelin close to the École Normale (AIP PAS. G1 46).
The exact date has not yet been found in the Archives at Institut Pasteur. Jouan then created the well-known laboratory equipment enterprise that still carries his name (see the following link for the 1933 catalogue: http://www.bium.univ-paris5.fr/histmed/medica/cote?extaphpin014, accessed on 5 November 2023). (All the information in this paragraph was researched and kindly communicated by Sandra Legout, CeRIS, Institut Pasteur)
The conservation of biological samples in a museum is an interesting topic, raising ethical concerns in terms of human sources and the regulatory concerns relevant to specific regulations (see Section 5). Different approaches are usually considered, ranging from destruction—and the loss of biological patrimony— to storage and access according to regulations. Valorisation could be a key mission for a museum [18,19]; in this respect, the collection in the Musée Pasteur might provide valuable data. Constant vigilance should, nevertheless, be exerted, following the evolution of the regulations and the consequences for biological patrimony through the degree of stringency of their application/implementation in each institution, Institut Pasteur included) to avoid irreversible decisions that might be regretted later.
“Le plus ancien de nos services pratiques est celui des vaccins charbonneux, il date de la célèbre expérience de Pouilly-le-Fort, en 1881, et fut organisé par Chamberland. Bientôt le vaccin du rouget des porcs vint s’ajouter à celui du charbon et depuis trente-deux ans que le service fonctionne, il a délivré 41 649 592 doses de vaccin charbonneux et 10 716 906 doses de vaccin du rouget. MM. Jouan et Staub, qui assurent la préparation de ces vaccins, ont droit à la reconnaissance des agriculteurs ” (discours de M le Docteur Roux, Le XXVe Anniversaire de l’Institut Pasteur. In: Revue internationale de l’enseignement, tome 67, Janvier–Juin 1914. pp. 60–82).
https://www.persee.fr/doc/revin_1775–6014_1914_num_67_1_6822 (accessed on 5 November 2023).
3. Anthrax Toxins: The Puzzle of a Complex Research Domain
4. The Second Golden Age of B. anthracis Research
4.1. On Toxins
4.2. On Bacterial Cell Surface
4.3. On Pathophysiology
The influence of the local tissular micro-environment on pathogen-host interactions occurs in other diseases, such as cutaneous vs. visceral Leishmaniasis, in terms of temperature or Mycobacterium tuberculosis colonisation in different areas of the lungs, depending on the O2 tension: top vs. posterior areas for biped vs. quadruped behaviour (Gilles Marchal and Geneviève Milon, personal communication).
4.4. On Therapeutics
4.4.1. Preventive Therapies
As will become apparent in Section 5, the development of an anthrax human vaccine is subject to many hurdles; manipulating B. anthracis is not an easy task under current regulations. Drawing on our experience in such development, it seems judicious and reasonable to favour working on a strain belonging to the B. cereus group outside anthracis to produce spores, specific spore antigens, or the capsular poly-gamma-D-glutamate through the expression of its biosynthesis operon; unpublished experiments in the anthrax Pasteur laboratory found that B. cereus spores could replace B. anthracis spores, albeit with a small decrease in efficiency. Recombinant PA and LF as key vaccine components are already produced in E. coli. Due to the 500 bp rule of the French regulations governing any samples that may contain genetic material from B. anthracis (see below), such vaccine development concerning a human vaccine seems, for the time being, probably more easily (while safe) managed at the European level outside France.
4.4.2. Curative Therapies
5. “MOT” (Special Agents) Regulation
Links showing some of the evolutions of the French regulation (accessed on 5 November 2023):
The sanctions in 2023 are up to 5–7 years’ imprisonment and a EUR 375,000–750,000 fine
Historically, when these regulations were first implemented and their implication not yet mastered, any longer than 500 bp of DNA purified from B. anthracis was considered “MOT”, even if the same exact sequence could be found in another non-“MOT” micro-organism; similarly, any molecule purified from B. anthracis could be considered MOT, even if it was a molecule found in any living cells such as ATP. Fortunately, scientific soundness rapidly prevailed, and the regulations were more precisely specified.
6. Some Points of Discussion
- -
- First, let us stress one technical (although seeming trivial at first sight), in fact, a crucial aspect for a valid interpretation of the anthracidal effects of a given anti-bacterial agent, i.e., sporicidal vs. bactericidal. Usually, a certain incubation time for the tested molecule is required, during which germination may occur and the antibacterial molecule exerts its effect. Data interpretation should, thus, be drawn carefully, distinguishing between direct sporicidal activity and killing of germinated spores.
- -
- Through our studies, we observed that the cellular effects of the toxins were mediated in fine through epigenetic modifications of the intoxinated cell [121]. This opens the path of alternative therapeutics aimed at restoring the functionality of the intoxinated cells in reversing these epigenetic modifications. Such “resuscitation” therapeutics are not confined to anthrax and have been considered in other pathologies where epigenetic memory is thought to be part of the persistence of homeostasis perturbation [122].
- -
- Lung B. anthracis infection is a secondary infection from within capillaries, with the blood-circulating encapsulated bacteria being trapped due to their large diameter [123]. This phenomenon was already suggested at the beginning of the 20th century (cited in [124]). Conceptually, this may represent a more general way for a pathogen to reach the lungs; as a secondary event, this is an interesting concept to consider (for example, for encapsulated Streptococcus pneumoniae or Yersinia pestis at a given dissemination stage).
- -
- B. anthracis toxins and spores could be detected in the blood, liver, and/or spleen as early as 1 h after intra-nasal delivery [99]. Such rapid crossing of the respiratory epithelium might be a more general way for a pathogen to interact with its host. Protein delivery through the respiratory epithelium has, indeed, been well-studied for therapeutic means [125,126], though the exact mechanisms are still debated (through pores, between adjacent cells, transcytosis, etc.).
- -
- A crucial challenge is the induction of a respiratory immune response that will control inhalational anthrax. A recent report using BCG [127,128] raises the interesting concept that an immune response generated from within the lung capillaries could trigger a more effective protective immunity than from the aerial space. B. anthracis could be a valid candidate for such exploration.
7. Conclusions
Many parameters obviously shape the way a given scientific activity can develop, such as the available technologies, the amount of investment in times of lack of financial resources, their mode of attribution/allocation, the degree of scientific openness and the way society aims to control it through specific regulations. The evolution of the global organisation and function of scientific structures in the 21st century led to a shortening of laboratory life duration and the advent of short-to-middle-term projects (typically two to three years).
All this aspects obviously influence the quality and orientation of research at the level of society. Moreover it questions their impact on the emergence of new concepts, technologies, or applications, as their basic and applied significance can be unpredictable, unexpected, and often unrealised until circumstances are suitable for their development.
The French author Georges Perec explored this intriguing aspect in some of his works, such as “Tentative d’épuisement d’un lieu parisien” (An Attempt at Exhausting a Place in Paris), where the impossibility of describing absolutely everything was more than obvious. Michael Baxandall analysed similar attempts at describing pictures (Pattern of intentions, Introduction, Yale University Press) and reached the same conclusion.
Georges Perec was keen to exploit constraints when stimulating creation in his works. Among the many playing with constraints, two are impressive: “la disparition” (translated as “a void”), around 300 pages without the vowel E, or “Les Revenentes” (translated as “The Exeter Text: Jewels, Secrets, Sex”) a novel of around 60 pages with only the vowel E, excluding all the others. In another artistic domain, Nadia Boulanger gave the same advice to jazzman Quincy Jones “Mieux il saura écrire avec des contraintes, plus il deviendra libre” (“the more he would know how to write with constraints, the freer he will be”;
(“L’autonomie de la vie se révèle imprévisiblement, le tout est de saisir le fait apparemment contradictoire à l’observation commune et de l’intégrer dans la connaissance au lieu de le rejeter comme une aberration de la nature […] car en expérimentation biologique, l’essentiel n’est pas de poursuivre toujours le but que l’on cherchait, mais de voir aussi ce qu’on n’y cherchait pas” p. 140)[137]
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
- This contribution covers a domain that possesses a long history. My respect and admiration go to our historical predecessors. Their names are present at the top of their publications, often freely available in numeric form. From the present, I will be unable to mention all my colleagues in Michèle Mock’s lab; suffice to recognise them as they are present as co-authors on all the published papers from the lab; let me mention more specifically Thomas Candela, Michel ‘TCM’ Haustant and the memory of Fabien Brossier. I would like to recognise the pleasure of working with the scientists in formation or post-formation to whom I hope I was able to transmit a constructive view of science and help to develop their, each unique, potential, they gave me so much in return, Alex, Manue, Ian, Benoît, Emilie, Maria, Clémence, Fabien, Mathieu and Guillain.
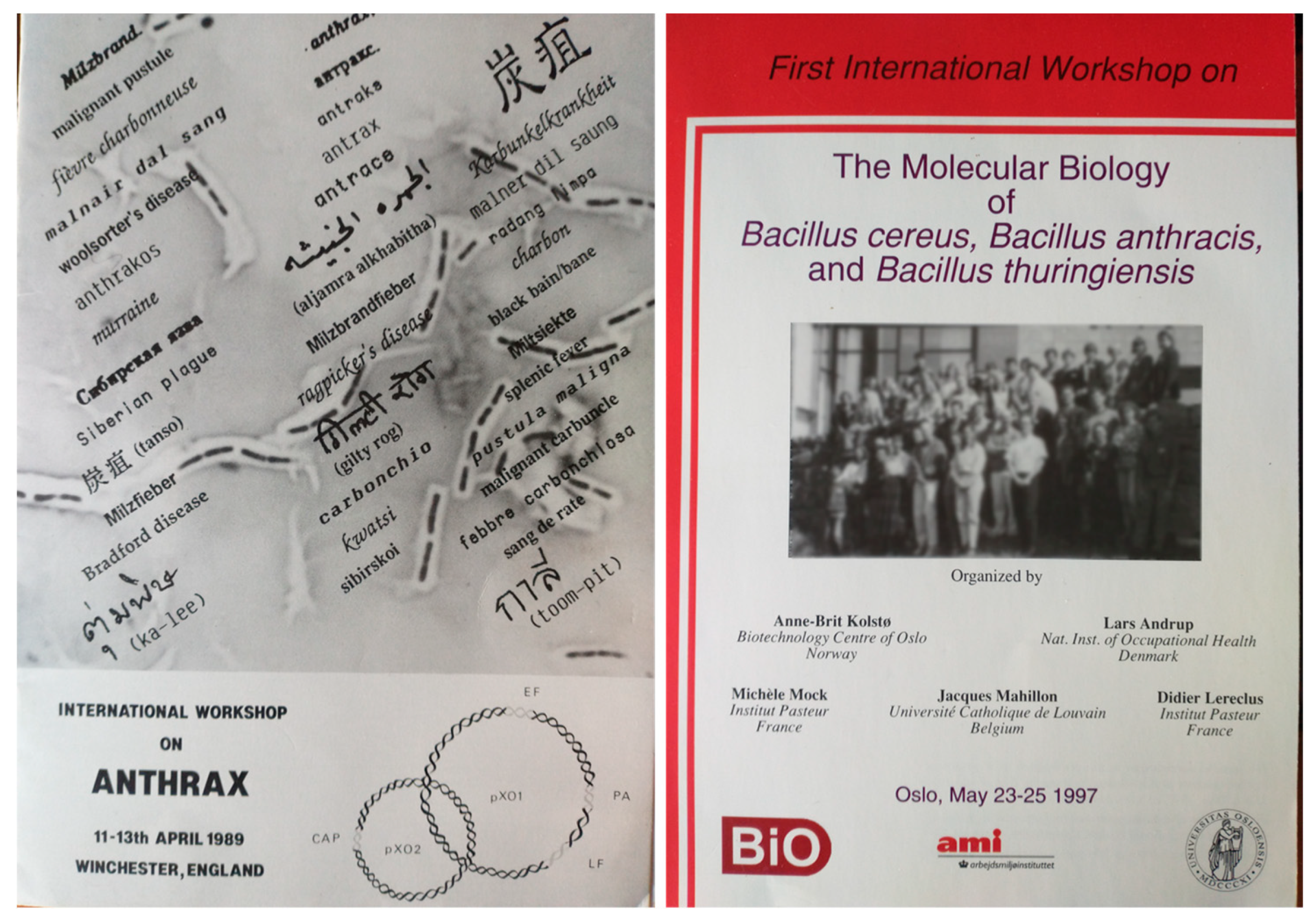
- In the Bacillus anthracis field (and cereus!), I had the pleasure of interacting with many colleagues during all these years; among them, a specific thought is paid to Art Friedlander, Ann-Brit Kolsto, Anne Moir, Silke Klee, and Mahtab Moyaeri. A dear memory is the encounter and collective discussion with Harry Smith at the Santa Fe BACT-2005 meeting; live history is always priceless.
- I wish to thank my colleagues from the Anthrax Euronet group, among them, especially, Wolfgang Beyer, Bassam Hallis, Michael Hudson, Silke Klee, and Cesare Montecucco. This European grant brought together vastly different expertise, initiating discussions and collaborations. One of these collaborations was with Silke Klee and Susann Dupke at the RKI, with Roland Grunow and Fabian Leendertz. It was such a great pleasure to collaborate on a thrilling subject, share our expertise, and start a scientific collaboration between Institut Pasteur and Robert Koch Institute, which, due to historical reasons, did not happen at the time of Louis Pasteur and Robert Koch.
- One of the great pleasures in science relies on the collaborations that sometimes emerge unexpectedly; I especially remember Wei-Jen Tang in Chicago, Gilles Guichard in Bordeaux; Lhousseine Touqui at Institut Pasteur, and Grégory Jouvion and Michel Huerre when histopathology expertise was still available at Institut Pasteur; François Bécher, Eric Ezan, Daniel Gillet, and Nathalie Morel at CEA. A specific collaboration flourished with IRBA; I cannot cite all colleagues during these almost 20 years in the immunology, bacteriology, and virology fields. They should know I deeply value our scientific interactions and hope I was able to forward what I received from my colleagues during my career. A special thought for Jean-Nicolas Tournier, with whom a collaboration developed from almost the time of my arrival in Michèle Mock’s lab; our scientific discussions and sharing of experiments, technologies, and friendship were precious. I fully appreciated the exchanges with Patrice Binder, his vast experience and his support for the anthrax field. A warm remembrance of the late Jacques Viret, from our first encounter in 1982 at CRSSA in Clamart to the last at IRBA in Grenoble, his soft spot for Jung and René Thom and our discussions on many other stimulating topics.
- This contribution deals with history; I would have been unable to delve into old and less-old documents in the Institut Pasteur archives and photothèque without the help of especially Sandra Legout, Chantal Pflieger, Christian Sany, Catherine Cécilio and Michaël Davy. I would like to stress the invaluable contribution of Sandra Legout, who has developed a deep knowledge of Institut Pasteur and its personnel in addition to her other archival research interests.
- I wish to acknowledge my immense gratitude to Javier Pizarro-Cerda, and Olivier Dussurget. Javier accepted me in his lab at a delicate period. I sincerely hope that I have been able to contribute the knowledge and scientific vision I was able to acquire during my career to my lab colleagues. I am immensely grateful to Geneviève Milon, who supported me in difficult times at Pasteur, and for our impromptu discussions; as Marivaux wrote “Dans ce monde, il faut être un peu trop bon pour l’être assez”. I also remember my life as a newborn “pasteurien” in her and Gilles Marchal’s group in Robert Fauve’s lab. Their vision of science and transmission was enlightening. A wonderful memory is, thanks to Gilles and Geneviève, my CIBA foundation bursary and the following short period in Ralph Steinman’s lab in Zanvil Cohn’s department; this was an incredible scientific period full of discoveries including the fascinating mobile dendritic cell. Last but not least, I am deeply indebted to Michèle Mock for these wonderful years of research; she accepted my sometimes-unorthodox queries, creating a trusting environment where everything could be considered and discussed without prejudice. She never ceased to discuss and critically read my manuscripts even after the anthrax lab closure; the current one included—many thanks also to Maxime Schwartz for his constructive criticism and remarks. Dominique Goossens has always been by my side during all these years, “I have forgot why I did call thee back—Let me stand here till thou remember it—I shall forget, to have thee still stand there, Rememb’ring how I love thy company—And I’ll still stay, to have thee still forget”.
Conflicts of Interest
Abbreviations
| AIP | Archives de l’Institut Pasteur |
| AMP | Anti-Microbial Peptides |
| EF | Edema Factor |
| ET | Edema Toxin |
| FIS | Formaldehyde-Inactivated Spores |
| LF | Letal Factor |
| LT | Letal Toxin |
| PA | Protective Antigen |
| PDGA | Poly-gamma D-Glutamic Acid |
| PGC | Capsule naturally coupled to PeptidoGlycan |
| SMA | Service de Microbiologie Animale |
| SVV | Service des Vaccins Vétérinaires |
References
- Davaine, C. Recherches relatives à l’action de la chaleur sur le virus charbonneux. C. R. Acad. Sci. 1873, 77, 726–729. [Google Scholar]
- Perrot, A.C.; Schwartz, M. Pasteur et Koch: Un Duel de Géants Dans le Monde des Microbes; Ed. Odile Jacob: Paris, France, 2014. [Google Scholar]
- Perrot, A.C.; Schwartz, M. Robert Koch und Louis Pasteur: Duell Zweier Giganten; Ed. Theiss: Darmstadt, Germany, 2015. [Google Scholar]
- Schwartz, M. Jekyll and Mr. Hyde: A short history of anthrax. Mol. Asp. Med. 2009, 30, 347–355. [Google Scholar] [CrossRef]
- Pasteur, L.; Chamberland, C.; Roux, E. Compte rendu sommaire des expériences faites à Pouilly-le-Fort, près Melun, sur la vaccination charbonneuse. In Comptes Rendus Hebdomadaires des Séances de l’Académie des Sciences; 1881; Volume XCII, p. 1378. [Google Scholar]
- Perrot, A.; Schwartz, M. Pasteur et ses Lieutenants; Ed. Odile Jacob: Paris, France, 2013. [Google Scholar]
- Delaunay, A. L’Institut Pasteur des Origines à Aujourd’hui; Ed. France-Empire: Paris, France, 1962. [Google Scholar]
- Beyer, W.; Turnbull, P.C. Anthrax in animals. Mol. Aspects Med. 2009, 30, 481–489. [Google Scholar] [CrossRef]
- Hugh-Jones, M.; Blackburn, J. The ecology of Bacillus anthracis. Mol. Asp. Med. 2009, 30, 356–367. [Google Scholar] [CrossRef]
- Mock, M.; Montecucco, C. Editorial. Mol. Asp. Med. 2009, 30, 345–346. [Google Scholar] [CrossRef]
- Smith, H. Discovery of the anthrax toxin: The beginning of studies of virulence determinants regulated in vivo. Int. J. Med. Microbiol. 2002, 291, 411–417. [Google Scholar] [CrossRef]
- Mikesell, P.; Ivins, B.E.; Ristroph, J.D.; Dreier, T.M. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 1983, 39, 371–376. [Google Scholar] [CrossRef]
- Green, B.D.; Battisti, L.; Koehler, T.M.; Thorne, C.B.; Ivins, B.E. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 1985, 49, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Uchida, I.; Sekizaki, T.; Hashimoto, K.; Terakado, N. Association of the encapsulation of Bacillus anthracis with a 60 megadalton plasmid. J. Gen. Microbiol. 1985, 131, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Perrot, A.; Schwartz, M. Le Neveu de Pasteur: Ou la vie Aventureuse d’Adrien Loir, Savant et Globe-Trotter (1862–1941); Ed. Odile Jacob: Paris, France, 2020. [Google Scholar]
- Antwerpen, M.; Beyer, W.; Bassy, O.; Ortega-Garcia, M.V.; Cabria-Ramos, J.C.; Grass, G.; Wolfel, R. Phylogenetic Placement of Isolates within the Trans-Eurasian Clade A.Br.008/009 of Bacillus anthracis. Microorganisms 2019, 7, 689. [Google Scholar] [CrossRef] [PubMed]
- Girault, G.; Blouin, Y.; Vergnaud, G.; Derzelle, S. High-throughput sequencing of Bacillus anthracis in France: Investigating genome diversity and population structure using whole-genome SNP discovery. BMC Genom. 2014, 15, 288. [Google Scholar] [CrossRef]
- Nakahama, N. Museum specimens: An overlooked and valuable material for conservation genetics. Ecol. Res. 2021, 36, 13–23. [Google Scholar] [CrossRef]
- Yeates, D.; Zwick, A.; Mikheyev, A. Museums are biobanks: Unlocking the genetic potential of the three billion specimens in the world’s biological collections. Curr. Opin. Insect Sci. 2016, 18, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Lewis, K.; Epstein, S.; Godoy, V.G.; Hong, S.H. Intact DNA in ancient permafrost. Trends Microbiol. 2008, 16, 92–94. [Google Scholar] [CrossRef]
- Price, P.B. Microbial life in glacial ice and implications for a cold origin of life. FEMS Microbiol. Ecol. 2007, 59, 217–231. [Google Scholar] [CrossRef]
- Price, P.B. Microbial genesis, life and death in glacial ice. Can. J. Microbiol. 2009, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stamatin, N.; Stamatin, L. Le pouvoir immunisant de souches acapsulogènes du B. anthracis. C. R. Soc. Biol. 1936, 122, 491–493. [Google Scholar]
- Sterne, M. The use of anthrax vaccines prepared from avirulent (unencapsulated) variants of Bacillus anthracis. Onderstepoort J. Vet. Sci. Anim. Ind. 1939, 13, 307–312. [Google Scholar]
- Shlyakhov, E.; Vata, A.; Platkov, E. Immunological diagnosis in vivo and acapsular anthrax vaccine: A pioneer achievement of romanian medical science. J. Prev. Med. 2001, 9, 52–56. [Google Scholar]
- Stamatin, N. L’immunisation anticharbonneuse au moyen d’une souche de Bacillus anthracis acapsulogène chez le mouton. C.R. Soc. Biol. Paris 1937, 125(pt6), 90–92. Available online: https://gallica.bnf.fr/ark:/12148/bpt6k6541878j/f96.item (accessed on 5 November 2023).
- Staub, A.M.; Virat, B.; Levaditi, J. Pouvoir létal de certaines souches acapsulogènes de B. anthracis. Ann. Inst. Pasteur 1955, 88, 244–246. [Google Scholar]
- Ramon, G.; Staub, A. Essais sur l’immunisation contre le charbon. Sur une nouvelle formule de vaccination charbonneuse. Rev. d’immunologie 1936, 2, 401–414. [Google Scholar] [CrossRef]
- Jacotot, H.; Virat, B. Longevity of B. anthracis spores (Pasteur’s first vaccine). Ann. Inst. Pasteur 1954, 87, 215–217. [Google Scholar]
- Virat, B. La vaccination anticharbonneuse. Econ. Méd. Anim. 1967, 8, 17–21. [Google Scholar]
- Fauve, R.M.; Delaunay, A. Résistance cellulaire à l’infection bactérienne. V. Modifications cytoplasmiques observées in vitro, dans des macrophages de souris, après injection de bactéries capables ou non de multiplication intracellulaire [Cellular resistance to bacterial infection. V. Cytoplasm modifications in vitro in mouse macrophages after injection of bacteria capable or incapable of intracellular multiplication]. Ann. Inst. Pasteur 1966, 111, 78–84. [Google Scholar]
- von Behring, E.; Kitasato, S. Ueber das zustandekommen der diphtherie-immunität und der tetanus-immunität bei thieren. Dtsch. Med. Wochenschr. 1890, 49, 1–6. [Google Scholar]
- Kitasato, S. Ueber den tetanusbacillus. Zeitschr. Hyg. 1889, 7, 225–234. [Google Scholar] [CrossRef]
- Nocard, E. Sur la sérothérapie du tétanos: Essais de traitement préventif. Bull. Soc. Cent. Méd. Vét. 1895, 407–418. [Google Scholar]
- Roux, E.; Yersin, A. Contribution à l’étude de la diphtérie. Ann. Inst. Pasteur 1888, 12, 629–661. [Google Scholar]
- Cavaillon, J.-M. From Bacterial Poisons to Toxins: The Early Works of Pasteurians. Toxins 2022, 14, 759. [Google Scholar] [CrossRef] [PubMed]
- Popoff, M.R.; Legout, S. Anaerobes and Toxins, a Tradition of the Institut Pasteur. Toxins 2023, 15, 43. [Google Scholar] [CrossRef]
- Maquart, B. Louis Pasteur, Le Visionnaire, Sous la Direction d’Annick Perrot et Maxime Schwartz; Ed. La Martinière: Paris, France, 2017. [Google Scholar]
- Grabar, P.; Staub, A.M. Recherches immunochimiques sur la bactéridie charbonneuse: II.-Les fractions protéidiques du liquide d’oedème charbonneux et des extraits de B. anthracis. Ann. Inst. Pasteur 1944, 70, 12–143. [Google Scholar]
- Staub, A.M.; Grabar, P. Recherches immunochimiques sur la bactéridie charbonneuse: I.-Le liquide d’oedème de cobaye et les polyosides. Ann. Inst. Pasteur 1944, 7, 16–32. [Google Scholar]
- Kintzer, A.F.; Thoren, K.L.; Sterling, H.J.; Dong, K.C.; Feld, G.K.; Tang, I.I.; Zhang, T.T.; Williams, E.R.; Berger, J.M.; Krantz, B.A. The protective antigen component of anthrax toxin forms functional octameric complexes. J. Mol. Biol. 2009, 392, 614–629. [Google Scholar] [CrossRef]
- Brossier, F.; Mock, M. Toxins of Bacillus anthracis. Toxicon 2001, 39, 1747–1755. [Google Scholar] [CrossRef] [PubMed]
- Moayeri, M.; Leppla, S.H. Cellular and systemic effects of anthrax lethal toxin and edema toxin. Mol. Asp. Med. 2009, 30, 439–455. [Google Scholar] [CrossRef]
- Moayeri, M.; Leppla, S.H.; Vrentas, C.; Pomerantsev, A.P.; Liu, S. Anthrax Pathogenesis. Annu. Rev. Microbiol. 2015, 69, 185–208. [Google Scholar] [CrossRef]
- Tournier, J.N.; Rossi Paccani, S.; Quesnel-Hellmann, A.; Baldari, C.T. Anthrax toxins: A weapon to systematically dismantle the host immune defenses. Mol. Asp. Med. 2009, 30, 456–466. [Google Scholar] [CrossRef] [PubMed]
- Leppla, S.H. Anthrax toxin edema factor: A bacterial adenylate cyclase that increases cyclic AMP concentrations of eukaryotic cells. Proc. Natl. Acad. Sci. USA 1982, 79, 3162–3166. [Google Scholar] [CrossRef]
- Duesbery, N.S.; Webb, C.P.; Leppla, S.H.; Gordon, V.M.; Klimpel, K.R.; Copeland, T.D.; Ahn, N.G.; Oskarsson, M.K.; Fukasawa, K.; Paull, K.D.; et al. Proteolytic inactivation of MAP-kinase-kinase by anthrax lethal factor. Science 1998, 280, 734–737. [Google Scholar] [CrossRef]
- Klimpel, K.R.; Arora, N.; Leppla, S.H. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol. Microbiol. 1994, 13, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Vitale, G.; Pellizzari, R.; Recchi, C.; Napolitani, G.; Mock, M.; Montecucco, C. Anthrax lethal factor cleaves the N-terminus of MAPKKS and induces tyrosine/threonine phosphorylation of MAPKS in cultured macrophages. J. Appl. Microbiol. 1999, 87, 288. [Google Scholar] [CrossRef] [PubMed]
- Rossetto, O.; Scorzeto, M.; Megighian, A.; Montecucco, C. Tetanus neurotoxin. Toxicon 2013, 66, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Meynell, E.; Meynell, G.G. The Roles of Serum and Carbon Dioxide in Capsule Formation by Bacillus anthracis. J. Gen. Microbiol. 1964, 34, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Sirard, J.C.; Mock, M.; Fouet, A. The three Bacillus anthracis toxin genes are coordinately regulated by bicarbonate and temperature. J. Bacteriol. 1994, 176, 5188–5192. [Google Scholar] [CrossRef]
- Morange, M. A History of Biology; Princeton University Press: Princeton, NJ, USA, 2021. [Google Scholar]
- Mock, M.; Schwartz, M. Mutations which affect the structure and activity of colicin E3. J. Bacteriol. 1980, 142, 384–390. [Google Scholar] [CrossRef] [PubMed]
- Mock, M.; Miyada, C.G.; Collier, R.J. Genetic analysis of the functional relationship between colicin E3 and its immunity protein. J. Bacteriol. 1984, 159, 658–662. [Google Scholar] [CrossRef]
- Trieu-Cuot, P.; Gerbaud, G.; Lambert, T.; Courvalin, P. In vivo transfer of genetic information between gram-positive and gram-negative bacteria. EMBO J. 1985, 4, 3583–3587. [Google Scholar] [CrossRef]
- Brossier, F.; Levy, M.; Mock, M. Anthrax spores make an essential contribution to vaccine efficacy. Infect. Immun. 2002, 70, 661–664. [Google Scholar] [CrossRef]
- Cataldi, A.; Labruyere, E.; Mock, M. Construction and characterization of a protective antigen-deficient Bacillus anthracis strain. Mol. Microbiol. 1990, 4, 1111–1117. [Google Scholar] [CrossRef]
- Labruyere, E.; Mock, M.; Surewicz, W.K.; Mantsch, H.H.; Rose, T.; Munier, H.; Sarfati, R.S.; Barzu, O. Structural and ligand-binding properties of a truncated form of Bacillus anthracis adenylate cyclase and of a catalytically inactive variant in which glutamine substitutes for lysine-346. Biochemistry 1991, 30, 2619–2624. [Google Scholar] [CrossRef]
- Pezard, C.; Duflot, E.; Mock, M. Construction of Bacillus anthracis mutant strains producing a single toxin component. J. Gen. Microbiol. 1993, 139, 2459–2463. [Google Scholar] [CrossRef] [PubMed]
- Chateau, A.; van Schaik, W.; Six, A.; Aucher, W.; Fouet, A. CodY regulation is required for full virulence and heme iron acquisition in Bacillus anthracis. FASEB J. 2011, 25, 4445–4456. [Google Scholar] [CrossRef] [PubMed]
- Fouet, A. AtxA, a Bacillus anthracis global virulence regulator. Res. Microbiol. 2010, 161, 735–742. [Google Scholar] [CrossRef]
- Fouet, A.; Mock, M. Regulatory networks for virulence and persistence of Bacillus anthracis. Curr. Opin. Microbiol. 2006, 9, 160–166. [Google Scholar] [CrossRef]
- Mignot, T.; Couture-Tosi, E.; Mesnage, S.; Mock, M.; Fouet, A. In vivo Bacillus anthracis gene expression requires PagR as an intermediate effector of the AtxA signalling cascade. Int. J. Med. Microbiol. 2004, 293, 619–624. [Google Scholar] [CrossRef] [PubMed]
- van Schaik, W.; Chateau, A.; Dillies, M.A.; Coppee, J.Y.; Sonenshein, A.L.; Fouet, A. The global regulator CodY regulates toxin gene expression in Bacillus anthracis and is required for full virulence. Infect. Immun. 2009, 77, 4437–4445. [Google Scholar] [CrossRef]
- Fouet, A.; Mesnage, S. Bacillus anthracis cell envelope components. Curr. Top. Microbiol. Immunol. 2002, 271, 87–113. [Google Scholar] [CrossRef]
- Fouet, A.; Mesnage, S.; Tosi-Couture, E.; Gounon, P.; Mock, M. Bacillus anthracis surface: Capsule and S-layer. J. Appl. Microbiol. 1999, 87, 251–255. [Google Scholar] [CrossRef]
- Mesnage, S.; Tosi-Couture, E.; Gounon, P.; Mock, M.; Fouet, A. The capsule and S-layer: Two independent and yet compatible macromolecular structures in Bacillus anthracis. J. Bacteriol. 1998, 180, 52–58. [Google Scholar] [CrossRef]
- Mignot, T.; Mesnage, S.; Couture-Tosi, E.; Mock, M.; Fouet, A. Developmental switch of S-layer protein synthesis in Bacillus anthracis. Mol. Microbiol. 2002, 43, 1615–1627. [Google Scholar] [CrossRef]
- Candela, T.; Dumetz, F.; Tosi-Couture, E.; Mock, M.; Goossens, P.L.; Fouet, A. Cell-wall preparation containing poly-gamma-D-glutamate covalently linked to peptidoglycan, a straightforward extractable molecule, protects mice against experimental anthrax infection. Vaccine 2012, 31, 171–175. [Google Scholar] [CrossRef]
- Candela, T.; Fouet, A. Bacillus anthracis CapD, belonging to the gamma-glutamyltranspeptidase family, is required for the covalent anchoring of capsule to peptidoglycan. Mol. Microbiol. 2005, 57, 717–726. [Google Scholar] [CrossRef]
- Candela, T.; Mock, M.; Fouet, A. CapE, a 47-amino-acid peptide, is necessary for Bacillus anthracis polyglutamate capsule synthesis. J. Bacteriol. 2005, 187, 7765–7772. [Google Scholar] [CrossRef] [PubMed]
- Aucher, W.; Davison, S.; Fouet, A. Characterization of the sortase repertoire in Bacillus anthracis. PLoS ONE 2011, 6, e27411. [Google Scholar] [CrossRef] [PubMed]
- Davison, S.; Couture-Tosi, E.; Candela, T.; Mock, M.; Fouet, A. Identification of the Bacillus anthracis (gamma) phage receptor. J. Bacteriol. 2005, 187, 6742–6749. [Google Scholar] [CrossRef] [PubMed]
- Sylvestre, P.; Couture-Tosi, E.; Mock, M. A collagen-like surface glycoprotein is a structural component of the Bacillus anthracis exosporium. Mol. Microbiol. 2002, 45, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Sylvestre, P.; Couture-Tosi, E.; Mock, M. Contribution of ExsFA and ExsFB proteins to the localization of BclA on the spore surface and to the stability of the Bacillus anthracis exosporium. J. Bacteriol. 2005, 187, 5122–5128. [Google Scholar] [CrossRef] [PubMed]
- Brossier, F.; Weber-Levy, M.; Mock, M.; Sirard, J.C. Role of toxin functional domains in anthrax pathogenesis. Infect. Immun. 2000, 68, 1781–1786. [Google Scholar] [CrossRef] [PubMed]
- Pezard, C.; Berche, P.; Mock, M. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect. Immun. 1991, 59, 3472–3477. [Google Scholar] [CrossRef]
- Sirard, J.C.; Guidi-Rontani, C.; Fouet, A.; Mock, M. Characterization of a plasmid region involved in Bacillus anthracis toxin production and pathogenesis. Int. J. Med. Microbiol. 2000, 290, 313–316. [Google Scholar] [CrossRef]
- Goossens, P.L. Animal models of human anthrax: The Quest for the Holy Grail. Mol. Asp. Med. 2009, 30, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Glomski, I.J.; Piris-Gimenez, A.; Huerre, M.; Mock, M.; Goossens, P.L. Primary involvement of pharynx and peyer’s patch in inhalational and intestinal anthrax. PLoS Pathog. 2007, 3, e76. [Google Scholar] [CrossRef] [PubMed]
- Piris-Gimenez, A.; Corre, J.P.; Jouvion, G.; Candela, T.; Khun, H.; Goossens, P.L. Encapsulated Bacillus anthracis interacts closely with liver endothelium. J. Infect. Dis. 2009, 200, 1381–1389. [Google Scholar] [CrossRef] [PubMed]
- Glomski, I.J.; Corre, J.P.; Mock, M.; Goossens, P.L. Noncapsulated toxinogenic Bacillus anthracis presents a specific growth and dissemination pattern in naive and protective antigen-immune mice. Infect. Immun. 2007, 75, 4754–4761. [Google Scholar] [CrossRef] [PubMed]
- Glomski, I.J.; Dumetz, F.; Jouvion, G.; Huerre, M.R.; Mock, M.; Goossens, P.L. Inhaled non-capsulated Bacillus anthracis in A/J mice: Nasopharynx and alveolar space as dual portals of entry, delayed dissemination, and specific organ targeting. Microbes Infect. 2008, 10, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Dumetz, F.; Jouvion, G.; Khun, H.; Glomski, I.J.; Corre, J.P.; Rougeaux, C.; Tang, W.J.; Mock, M.; Huerre, M.; Goossens, P.L. Noninvasive imaging technologies reveal edema toxin as a key virulence factor in anthrax. Am. J. Pathol. 2011, 178, 2523–2535. [Google Scholar] [CrossRef] [PubMed]
- Bennett, E.; Hall, I.M.; Pottage, T.; Silman, N.J.; Bennett, A.M. Drumming-associated anthrax incidents: Exposures to low levels of indoor environmental contamination. Epidemiol. Infect. 2018, 146, 1519–1525. [Google Scholar] [CrossRef]
- Price, E.P.; Seymour, M.L.; Sarovich, D.S.; Latham, J.; Wolken, S.R.; Mason, J.; Vincent, G.; Drees, K.P.; Beckstrom-Sternberg, S.M.; Phillippy, A.M.; et al. Molecular epidemiologic investigation of an anthrax outbreak among heroin users, Europe. Emerg. Infect. Dis. 2012, 18, 1307–1313. [Google Scholar] [CrossRef]
- WHO. Anthrax in Humans and Animals; WHO: Geneva, Switzerland, 2008; ISBN 9789241547536. [Google Scholar]
- Guillemin, J. Anthrax: The investigation of a deadly outbreak. N. Engl. J. Med 2000, 343, 1198. [Google Scholar] [CrossRef]
- Guillemin, J. Detecting Anthrax: What We Learned from the 1979 Sverdlovsk Outbreak; Springer: Dordrecht, The Netherlands, 2001; Volume 35, pp. 75–85. [Google Scholar]
- Guillemin, J. Biological Weapons: From the Invention of State-Sponsored Programs to Contemporary Bioterrorism; Columbia University Press: New York, NY, USA, 2004. [Google Scholar]
- Turner, J.N. Amérithrax; Ed. de l’aube/L’aube Noire: La Tour d’Aigues, France, 2014. [Google Scholar]
- Cossart, P.; Schwartz, M. Pasteur, a visionary: Comptes Rendus. Biologies 2022, 345, 1–5. Available online: https://comptes-rendus.academie-sciences.fr/biologies/item/10.5802/crbiol.97.pdf (accessed on 5 November 2023). [CrossRef] [PubMed]
- Fiole, D.; Deman, P.; Trescos, Y.; Mayol, J.F.; Mathieu, J.; Vial, J.C.; Douady, J.; Tournier, J.N. Two-photon intravital imaging of lungs during anthrax infection reveals long-lasting macrophage-dendritic cell contacts. Infect. Immun. 2014, 82, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, Y.P.; Tournier, J.N.; Paucod, J.C.; Corre, J.P.; Mock, M.; Goossens, P.L.; Vidal, D.R. Efficacy of a vaccine based on protective antigen and killed spores against experimental inhalational anthrax. Infect. Immun. 2009, 77, 1197–1207. [Google Scholar] [CrossRef] [PubMed]
- Klezovich-Benard, M.; Corre, J.P.; Jusforgues-Saklani, H.; Fiole, D.; Burjek, N.; Tournier, J.N.; Goossens, P.L. Mechanisms of NK cell-macrophage Bacillus anthracis crosstalk: A balance between stimulation by spores and differential disruption by toxins. PLoS Pathog. 2012, 8, e1002481. [Google Scholar] [CrossRef]
- Le Gars, M.; Haustant, M.; Klezovich-Benard, M.; Paget, C.; Trottein, F.; Goossens, P.L.; Tournier, J.N. Mechanisms of Invariant NKT Cell Activity in Restraining Bacillus anthracis Systemic Dissemination. J. Immunol. 2016, 197, 3225–3232. [Google Scholar] [CrossRef]
- Rougeaux, C.; Becher, F.; Ezan, E.; Tournier, J.N.; Goossens, P.L. In vivo dynamics of active edema and lethal factors during anthrax. Sci. Rep. 2016, 6, 23346. [Google Scholar] [CrossRef]
- Rougeaux, C.; Becher, F.; Goossens, P.L.; Tournier, J.N. Very Early Blood Diffusion of the Active Lethal and Edema Factors of Bacillus anthracis After Intranasal Infection. J. Infect. Dis. 2020, 221, 660–667. [Google Scholar] [CrossRef]
- Tournier, J.N.; Quesnel-Hellmann, A.; Mathieu, J.; Montecucco, C.; Tang, W.J.; Mock, M.; Vidal, D.R.; Goossens, P.L. Anthrax edema toxin cooperates with lethal toxin to impair cytokine secretion during infection of dendritic cells. J. Immunol. 2005, 174, 4934–4941. [Google Scholar] [CrossRef]
- Trescos, Y.; Tessier, E.; Rougeaux, C.; Goossens, P.L.; Tournier, J.N. Micropatterned macrophage analysis reveals global cytoskeleton constraints induced by Bacillus anthracis edema toxin. Infect. Immun. 2015, 83, 3114–3125. [Google Scholar] [CrossRef]
- Chenau, J.; Fenaille, F.; Caro, V.; Haustant, M.; Diancourt, L.; Klee, S.R.; Junot, C.; Ezan, E.; Goossens, P.L.; Becher, F. Identification and validation of specific markers of Bacillus anthracis spores by proteomics and genomics approaches. Mol. Cell. Proteom. 2014, 13, 716–732. [Google Scholar] [CrossRef]
- Chenau, J.; Fenaille, F.; Ezan, E.; Morel, N.; Lamourette, P.; Goossens, P.L.; Becher, F. Sensitive detection of Bacillus anthracis spores by immunocapture and liquid chromatography-tandem mass spectrometry. Anal. Chem. 2011, 83, 8675–8682. [Google Scholar] [CrossRef]
- Duriez, E.; Goossens, P.L.; Becher, F.; Ezan, E. Femtomolar detection of the anthrax edema factor in human and animal plasma. Anal. Chem. 2009, 81, 5935–5941. [Google Scholar] [CrossRef] [PubMed]
- Morel, N.; Volland, H.; Dano, J.; Lamourette, P.; Sylvestre, P.; Mock, M.; Creminon, C. Fast and sensitive detection of Bacillus anthracis spores by immunoassay. Appl. Environ. Microbiol. 2012, 78, 6491–6498. [Google Scholar] [CrossRef]
- Sykes, A.; Brooks, T.; Dusmet, M.; Nicholson, A.G.; Hansell, D.M.; Wilson, R. Inhalational anthrax in a vaccinated soldier. Eur. Respir. J. 2013, 42, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Mock, M.; Fouet, A. Anthrax. Annu. Rev. Microbiol. 2001, 55, 647–671. [Google Scholar] [CrossRef]
- Chabot, D.J.; Ribot, W.J.; Joyce, J.; Cook, J.; Hepler, R.; Nahas, D.; Chua, J.; Friedlander, A.M. Protection of rhesus macaques against inhalational anthrax with a Bacillus anthracis capsule conjugate vaccine. Vaccine 2016, 34, 4012–4016. [Google Scholar] [CrossRef]
- Wang, J.Y.; Roehrl, M.H. Anthrax vaccine design: Strategies to achieve comprehensive protection against spore, bacillus, and toxin. Med. Immunol. 2005, 4, 4. [Google Scholar] [CrossRef]
- Brossier, F.; Levy, M.; Landier, A.; Lafaye, P.; Mock, M. Functional analysis of Bacillus anthracis protective antigen by using neutralizing monoclonal antibodies. Infect. Immun. 2004, 72, 6313–6317. [Google Scholar] [CrossRef]
- Brossier, F.; Sirard, J.C.; Guidi-Rontani, C.; Duflot, E.; Mock, M. Functional analysis of the carboxy-terminal domain of Bacillus anthracis protective antigen. Infect. Immun. 1999, 67, 964–967. [Google Scholar] [CrossRef]
- Antunes, S.; Corre, J.P.; Mikaty, G.; Douat, C.; Goossens, P.L.; Guichard, G. Effect of replacing main-chain ureas with thiourea and guanidinium surrogates on the bactericidal activity of membrane active oligourea foldamers. Bioorg. Med. Chem. 2017, 25, 4245–4252. [Google Scholar] [CrossRef]
- Teyssieres, E.; Corre, J.P.; Antunes, S.; Rougeot, C.; Dugave, C.; Jouvion, G.; Claudon, P.; Mikaty, G.; Douat, C.; Goossens, P.L.; et al. Proteolytically Stable Foldamer Mimics of Host-Defense Peptides with Protective Activities in a Murine Model of Bacterial Infection. J. Med. Chem. 2016, 59, 8221–8232. [Google Scholar] [CrossRef]
- Gimenez, A.P.; Wu, Y.Z.; Paya, M.; Delclaux, C.; Touqui, L.; Goossens, P.L. High bactericidal efficiency of type IIa phospholipase A2 against Bacillus anthracis and inhibition of its secretion by the lethal toxin. J. Immunol. 2004, 173, 521–530. [Google Scholar] [CrossRef]
- Piris-Gimenez, A.; Paya, M.; Lambeau, G.; Chignard, M.; Mock, M.; Touqui, L.; Goossens, P.L. In vivo protective role of human group IIa phospholipase A2 against experimental anthrax. J. Immunol. 2005, 175, 6786–6791. [Google Scholar] [CrossRef] [PubMed]
- Raymond, B.; Ravaux, L.; Memet, S.; Wu, Y.; Sturny-Leclere, A.; Leduc, D.; Denoyelle, C.; Goossens, P.L.; Paya, M.; Raymondjean, M.; et al. Anthrax lethal toxin down-regulates type-IIA secreted phospholipase A2 expression through MAPK/NF-κB inactivation. Biochem. Pharmacol. 2010, 79, 1149–1155. [Google Scholar] [CrossRef]
- Ankri, S.; Mirelman, D. Antimicrobial properties of allicin from garlic. Microbes Infect. 1999, 1, 125–129. [Google Scholar] [CrossRef]
- Harris, J.C.; Cottrell, S.L.; Plummer, S.; Lloyd, D. Antimicrobial properties of Allium sativum (garlic). Appl. Microbiol. Biotechnol. 2001, 57, 282–286. [Google Scholar] [CrossRef] [PubMed]
- Gastrointestinal anthrax after an animal-hide drumming event—New Hampshire and Massachusetts, 2009. MMWR Morb. Mortal Wkly. Rep. 2010, 59, 872–877.
- Marston, C.K.; Allen, C.A.; Beaudry, J.; Price, E.P.; Wolken, S.R.; Pearson, T.; Keim, P.; Hoffmaster, A.R. Molecular epidemiology of anthrax cases associated with recreational use of animal hides and yarn in the United States. PLoS ONE 2011, 6, e28274. [Google Scholar] [CrossRef] [PubMed]
- Raymond, B.; Batsche, E.; Boutillon, F.; Wu, Y.Z.; Leduc, D.; Balloy, V.; Raoust, E.; Muchardt, C.; Goossens, P.L.; Touqui, L. Anthrax lethal toxin impairs IL-8 expression in epithelial cells through inhibition of histone H3 modification. PLoS Pathog. 2009, 5, e1000359. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.H.; Hayano, M.; Griffin, P.T.; Amorim, J.A.; Bonkowski, M.S.; Apostolides, J.K.; Salfati, E.L.; Blanchette, M.; Munding, E.M.; Bhakta, M.; et al. Loss of epigenetic information as a cause of mammalian aging. Cell 2023, 186, 305–326.e327. [Google Scholar] [CrossRef]
- Jouvion, G.; Corre, J.P.; Khun, H.; Moya-Nilges, M.; Roux, P.; Latroche, C.; Tournier, J.N.; Huerre, M.; Chretien, F.; Goossens, P.L. Physical Sequestration of Bacillus anthracis in the Pulmonary Capillaries in Terminal Infection. J. Infect. Dis. 2016, 214, 281–287. [Google Scholar] [CrossRef]
- Bloom, W.L.; Mc, G.W. Studies on infection with Bacillus anthracis; physiological changes in experimental animals during the course of infection with B. anthracis. J. Infect. Dis. 1947, 80, 137–144. [Google Scholar] [CrossRef]
- Brain, J.D. Inhalation, deposition, and fate of insulin and other therapeutic proteins. Diabetes Technol. Ther. 2007, 9 (Suppl. S1), S4–S15. [Google Scholar] [CrossRef]
- Hastings, R.H.; Folkesson, H.G.; Matthay, M.A. Mechanisms of alveolar protein clearance in the intact lung. Am. J. Physiol. Lung Cell. Mol. Physiol. 2004, 286, L679–L689. [Google Scholar] [CrossRef]
- Darrah, P.A.; Zeppa, J.J.; Maiello, P.; Hackney, J.A.; Wadsworth, M.H., 2nd; Hughes, T.K.; Pokkali, S.; Swanson, P.A., 2nd; Grant, N.L.; Rodgers, M.A.; et al. Prevention of tuberculosis in macaques after intravenous BCG immunization. Nature 2020, 577, 95–102. [Google Scholar] [CrossRef]
- Larson, E.C.; Ellis-Connell, A.L.; Rodgers, M.A.; Gubernat, A.K.; Gleim, J.L.; Moriarty, R.V.; Balgeman, A.J.; Ameel, C.L.; Jauro, S.; Tomko, J.A.; et al. Intravenous Bacille Calmette-Guérin vaccination protects simian immunodeficiency virus-infected macaques from tuberculosis. Nat. Microbiol. 2023, 8, 2080–2092. [Google Scholar] [CrossRef] [PubMed]
- Helgason, E.; Okstad, O.A.; Caugant, D.A.; Johansen, H.A.; Fouet, A.; Mock, M.; Hegna, I.; Kolsto, A.B. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis—One species on the basis of genetic evidence. Appl. Environ. Microbiol. 2000, 66, 2627–2630. [Google Scholar] [CrossRef] [PubMed]
- Hoffmaster, A.R.; Hill, K.K.; Gee, J.E.; Marston, C.K.; De, B.K.; Popovic, T.; Sue, D.; Wilkins, P.P.; Avashia, S.B.; Drumgoole, R.; et al. Characterization of Bacillus cereus isolates associated with fatal pneumonias: Strains are closely related to Bacillus anthracis and harbor B. anthracis virulence genes. J. Clin. Microbiol. 2006, 44, 3352–3360. [Google Scholar] [CrossRef]
- Hoffmaster, A.R.; Ravel, J.; Rasko, D.A.; Chapman, G.D.; Chute, M.D.; Marston, C.K.; De, B.K.; Sacchi, C.T.; Fitzgerald, C.; Mayer, L.W.; et al. Identification of anthrax toxin genes in a Bacillus cereus associated with an illness resembling inhalation anthrax. Proc. Natl. Acad. Sci. USA 2004, 101, 8449–8454. [Google Scholar] [CrossRef] [PubMed]
- Klee, S.R.; Ozel, M.; Appel, B.; Boesch, C.; Ellerbrok, H.; Jacob, D.; Holland, G.; Leendertz, F.H.; Pauli, G.; Grunow, R.; et al. Characterization of Bacillus anthracis-like bacteria isolated from wild great apes from Cote d’Ivoire and Cameroon. J. Bacteriol. 2006, 188, 5333–5344. [Google Scholar] [CrossRef]
- Hudson, M.J.; Beyer, W.; Böhm, R.; Fasanella, A.; Garofolo, G.; Golinski, R.; Goossens, P.L.; Hahn, U.; Hallis, B.; King, A.; et al. Bacillus anthracis: Balancing innocent research with dual-use potential. Int. J. Med. Microbiol. 2008, 298, 345–364. [Google Scholar] [CrossRef] [PubMed]
- Brezillon, C.; Haustant, M.; Dupke, S.; Corre, J.P.; Lander, A.; Franz, T.; Monot, M.; Couture-Tosi, E.; Jouvion, G.; Leendertz, F.H.; et al. Capsules, toxins and AtxA as virulence factors of emerging Bacillus cereus biovar anthracis. PLoS Negl. Trop. Dis. 2015, 9, e0003455. [Google Scholar] [CrossRef] [PubMed]
- Feder, T. Q&A: Harry Collins on acquiring and using scientific knowledge. Phys. Today 2021. [Google Scholar] [CrossRef]
- Lefebvre, J.; Testenoire, P.-Y. Blancs de l’écrit, blancs de l’écriture. Linguistique L’écrit 2019, 1, 1–16. [Google Scholar] [CrossRef]
- Goossens, R. Les Fermentations Antibiotiques: Essai sur le Déterminisme Expérimental dans les Biosynthèses. Ph.D. Thesis, University of Paris, Paris, France, 1957. Available online: http://cadic.pasteur.fr/exl-php/vue-consult/ipp_recherche/ISO00015109 (accessed on 5 November 2023).








Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goossens, P.L. Bacillus anthracis, “la maladie du charbon”, Toxins, and Institut Pasteur. Toxins 2024, 16, 66. https://doi.org/10.3390/toxins16020066
Goossens PL. Bacillus anthracis, “la maladie du charbon”, Toxins, and Institut Pasteur. Toxins. 2024; 16(2):66. https://doi.org/10.3390/toxins16020066
Chicago/Turabian StyleGoossens, Pierre L. 2024. "Bacillus anthracis, “la maladie du charbon”, Toxins, and Institut Pasteur" Toxins 16, no. 2: 66. https://doi.org/10.3390/toxins16020066



