Bacillus anthracis Factors for Phagosomal Escape
Abstract
:1. Introduction
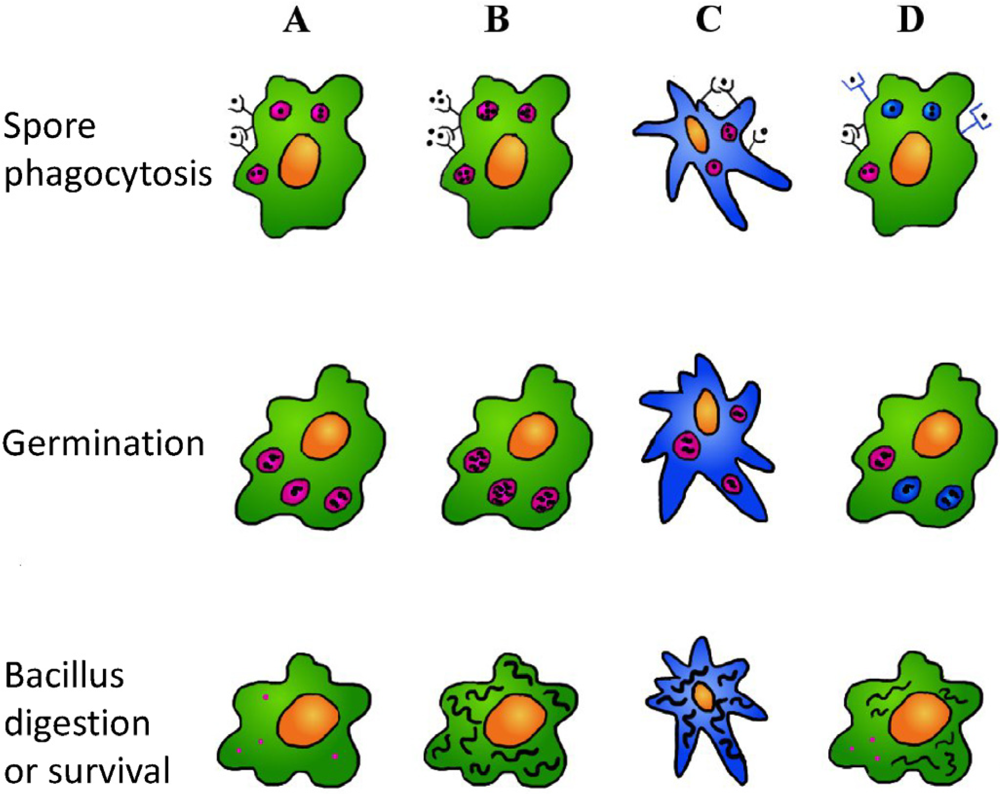
2.Bacillus Anthracis Entry into the Phagocytes
3. Bacillus Anthracis Factors that Can Interfere with the Phagosome Maturation Process
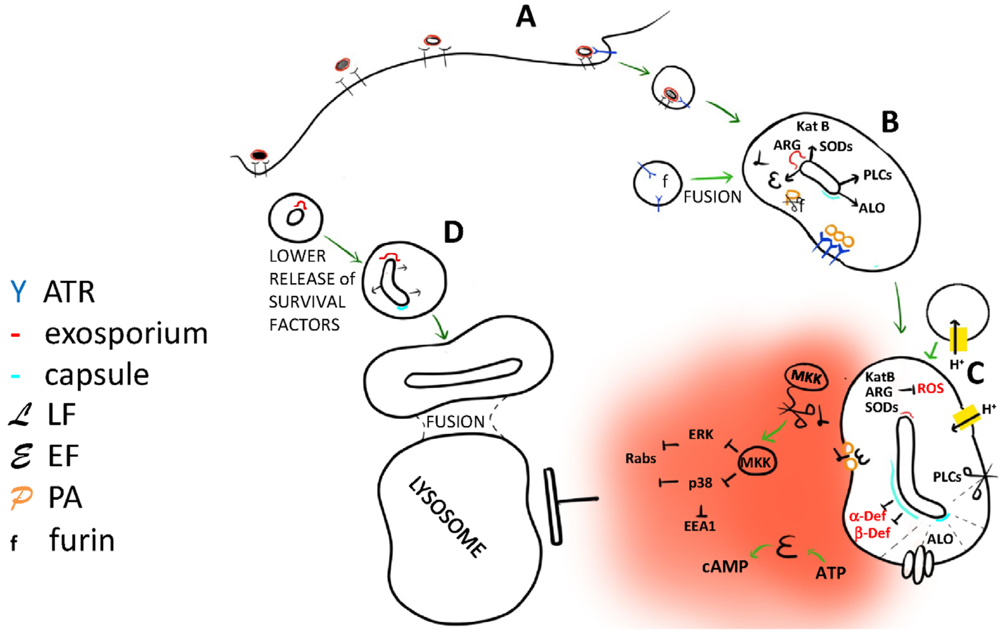
4. Lethal and Edema Toxins
5. Anthrolysin O
6. Phospholipases C
7. Antioxidant Enzymes
8. The Capsule
9. In the Battle between Phagosome and B. Anthracis, What Circumstances Facilitate the Pathogen?
10. Conclusions
Acknowledgements
References
- Dixon, T.C.; Meselson, M.; Guillemin, J.; Hanna, P.C. Anthrax. N. Engl. J. Med. 1999, 341, 815–826. [Google Scholar]
- Frankel, A.E.; Kuo, S.R.; Dostal, D.; Watson, L.; Duesbery, N.S.; Cheng, C.P.; Cheng, H.J.; Leppla, S.H. Pathophysiology of anthrax. Front Biosci. 2009, 14, 4516–4524. [Google Scholar]
- Baldari, C.T.; Tonello, F.; Paccani, S.R.; Montecucco, C. Anthrax toxins: A paradigm of bacterial immune suppression. Trends Immunol. 2006, 27, 434–440. [Google Scholar]
- Ezzell, J.W.; Welkos, S.L. The capsule of bacillus anthracis, a review. J. Appl. Microbiol. 1999, 87, 250. [Google Scholar]
- Ross, J.M. The pathogenesis of anthrax following the administration of spores by the respiratory route. J. Pathol. Bacteriol. 1957, 73, 485–494. [Google Scholar]
- Cote, C.K.; Welkos, S.L.; Bozue, J. Key aspects of the molecular and cellular basis of inhalational anthrax. Microbes Infect. 2011, 13, 1146–1155. [Google Scholar]
- Russell, B.H.; Vasan, R.; Keene, D.R.; Koehler, T.M.; Xu, Y. Potential dissemination of Bacillus anthracis utilizing human lung epithelial cells. Cell Microbiol. 2008, 10, 945–957. [Google Scholar] [CrossRef]
- Weiner, Z.P.; Glomski, I.J. Updating Perspectives on the Initiation of Bacillus anthracis Growth and Dissemination through Its Host. Infect. Immun. 2012, 80, 1626–1633. [Google Scholar] [CrossRef]
- Oliva, C.; Turnbough, C.L.; Kearney, J.F. CD14-Mac-1 interactions in Bacillus anthracis spore internalization by macrophages. Proc. Natl. Acad. Sci. USA 2009, 106, 13957–13962. [Google Scholar]
- Oliva, C.R.; Swiecki, M.K.; Griguer, C.E.; Lisanby, M.W.; Bullard, D.C.; Turnbough, C.L.; Kearney, J.F. The integrin Mac-1 (CR3) mediates internalization and directs Bacillus anthracis spores into professional phagocytes. Proc. Natl. Acad. Sci. USA 2008, 105, 1261–1266. [Google Scholar]
- Hughes, M.A.; Green, C.S.; Lowchyj, L.; Lee, G.M.; Grippe, V.K.; Smith, M.F., Jr.; Huang, L.-Y.; Harvill, E.T.; Merkel, T.J. MyD88-dependent signaling contributes to protection following Bacillus anthracis spore challenge of mice: implications for Toll-like receptor signaling. Infect. Immun. 2005, 73, 7535–7540. [Google Scholar]
- Bozue, J.; Cote, C.K.; Moody, K.L.; Welkos, S.L. Fully virulent Bacillus anthracis does not require the immunodominant protein BclA for pathogenesis. Infect. Immun. 2007, 75, 508–511. [Google Scholar]
- Bozue, J.; Moody, K.L.; Cote, C.K.; Stiles, B.G.; Friedlander, A.M.; Welkos, S.L.; Hale, M.L. Bacillus anthracis Spores of the bclA Mutant Exhibit Increased Adherence to Epithelial Cells, Fibroblasts, and Endothelial Cells but Not to Macrophages. Infect. Immu.n 2007, 75, 4498–4505. [Google Scholar] [CrossRef]
- Premanandan, C.; Storozuk, C.A.; Clay, C.D.; Lairmore, M.D.; Schlesinger, L.S.; Phipps, A.J. Complement protein C3 binding to Bacillus anthracis spores enhances phagocytosis by human macrophages. Microb. Pathog. 2009, 46, 306–314. [Google Scholar] [CrossRef]
- Gu, C.; Jenkins, S.A.; Xue, Q.; Xu, Y. Activation of the Classical Complement Pathway by Bacillus anthracis Is the Primary Mechanism for Spore Phagocytosis and Involves the Spore Surface Protein BclA. J Immunol. 2012, 188, 4421–4431. [Google Scholar] [CrossRef]
- Chung, M.C.; Tonry, J.H.; Narayanan, A.; Manes, N.P.; Mackie, R.S.; Gutting, B.; Mukherjee, D.V.; Popova, T.G.; Kashanchi, F.; Bailey, C.L.; et al. Bacillus anthracis interacts with plasmin(ogen) to evade C3b-dependent innate immunity. PLoS One 2011, 6, e18119. [Google Scholar]
- Stuart, L.M.; Ezekowitz, R.A. Phagocytosis: elegant complexity. Immunity 2005, 22, 539–550. [Google Scholar]
- Alix, E.; Mukherjee, S.; Roy, C.R. Subversion of membrane transport pathways by vacuolar pathogens. J. Cell Biol. 2011, 195, 943–952. [Google Scholar]
- Diacovich, L.; Gorvel, J.P. Bacterial manipulation of innate immunity to promote infection. Nat. Rev. Microbiol. 2010, 8, 117–128. [Google Scholar]
- Blanchet, F.P.; Piguet, V. Immunoamphisomes in dendritic cells amplify TLR signaling and enhance exogenous antigen presentation on MHC-II. Autophagy 2010, 6, 816–818. [Google Scholar]
- Sanjuan, M.A.; Milasta, S.; Green, D.R. Toll-like receptor signaling in the lysosomal pathways. Immunol. Rev. 2009, 227, 203–220. [Google Scholar]
- Kumar, Y.; Valdivia, R.H. Leading a sheltered life: intracellular pathogens and maintenance of vacuolar compartments. Cell Host Microbe. 2009, 5, 593–601. [Google Scholar]
- Guidi-Rontani, C.; Weber-Levy, M.; Labruyere, E.; Mock, M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 1999, 31, 9–17. [Google Scholar] [CrossRef]
- Banks, D.J.; Barnajian, M.; Maldonado-Arocho, F.J.; Sanchez, A.M.; Bradley, K.A. Anthrax toxin receptor 2 mediates Bacillus anthracis killing of macrophages following spore challenge. Cell Microbiol. 2005, 7, 1173–1185. [Google Scholar]
- Barry, A.O.; Mege, J.L.; Ghigo, E. Hijacked phagosomes and leukocyte activation: an intimate relationship. J. Leukoc. Biol. 2011, 89, 373–382. [Google Scholar]
- Hu, H.; Sa, Q.; Koehler, T.M.; Aronson, A.I.; Zhou, D. Inactivation of Bacillus anthracis spores in murine primary macrophages. Cell Microbiol. 2006, 8, 1634–1642. [Google Scholar] [CrossRef]
- Welkos, S.; Friedlander, A.; Weeks, S.; Little, S.; Mendelson, I. In-vitro characterisation of the phagocytosis and fate of anthrax spores in macrophages and the effects of anti-PA antibody. J. Med. Microbiol. 2002, 51, 821–831. [Google Scholar]
- Bergman, N.H.; Anderson, E.C.; Swenson, E.E.; Janes, B.K.; Fisher, N.; Niemeyer, M.M.; Miyoshi, A.D.; Hanna, P.C. Transcriptional profiling of Bacillus anthracis during infection of host macrophages. Infect. Immun. 2007, 75, 3434–3444. [Google Scholar]
- van der Goot, G.; Young, J.A. Receptors of anthrax toxin and cell entry. Mol. Aspects Med. 2009, 30, 406–412. [Google Scholar]
- Collier, R.J. Membrane translocation by anthrax toxin. Mol. Aspects Med. 2009, 30, 413–422. [Google Scholar]
- Tonello, F.; Montecucco, C. The anthrax lethal factor and its MAPK kinase-specific metalloprotease activity. Mol. Aspects Med. 2009, 30, 431–438. [Google Scholar]
- Moayeri, M.; Leppla, S.H. Cellular and systemic effects of anthrax lethal toxin and edema toxin. Mol. Aspects Med. 2009, 30, 439–455. [Google Scholar]
- Yeager, L.A.; Chopra, A.K.; Peterson, J.W. Bacillus anthracis edema toxin suppresses human macrophage phagocytosis and cytoskeletal remodeling via the protein kinase A and exchange protein activated by cyclic AMP pathways. Infect. Immun. 2009, 77, 2530–2543. [Google Scholar] [CrossRef]
- Rossi Paccani, S.; Tonello, F.; Patrussi, L.; Capitani, N.; Simonato, M.; Montecucco, C.; Baldari, C.T. Anthrax toxins inhibit immune cell chemotaxis by perturbing chemokine receptor signalling. Cell Microbiol. 2007, 9, 924–929. [Google Scholar]
- Tournier, J.N.; Rossi Paccani, S.; Quesnel-Hellmann, A.; Baldari, C.T. Anthrax toxins: a weapon to systematically dismantle the host immune defenses. Mol. Aspects Med. 2009, 30, 456–466. [Google Scholar]
- Boyden, E.D.; Dietrich, W.F. Nalp1b controls mouse macrophage susceptibility to anthrax lethal toxin. Nat. Genet. 2006, 38, 240–244. [Google Scholar]
- Terra, J.K.; Cote, C.K.; France, B.; Jenkins, A.L.; Bozue, J.A.; Welkos, S.L.; LeVine, S.M.; Bradley, K.A. Cutting edge: resistance to Bacillus anthracis infection mediated by a lethal toxin sensitive allele of Nalp1b/Nlrp1b. J. Immunol. 2010, 184, 17–20. [Google Scholar]
- Moayeri, M.; Crown, D.; Newman, Z.L.; Okugawa, S.; Eckhaus, M.; Cataisson, C.; Liu, S.; Sastalla, I.; Leppla, S.H. Inflammasome sensor Nlrp1b-dependent resistance to anthrax is mediated by caspase-1, IL-1 signaling and neutrophil recruitment. PLoS Pathog. 2010, 6, e1001222. [Google Scholar]
- Hahn, B.L.; Bischof, T.S.; Sohnle, P.G. Superficial exudates of neutrophils prevent invasion of Bacillus anthracis bacilli into abraded skin of resistant mice. Int. J. Exp. Pathol. 2008, 89, 180–187. [Google Scholar]
- Mayer-Scholl, A.; Hurwitz, R.; Brinkmann, V.; Schmid, M.; Jungblut, P.; Weinrauch, Y.; Zychlinsky, A. Human neutrophils kill Bacillus anthracis. PLoS Pathog. 2005, 1, e23. [Google Scholar] [CrossRef]
- Terra, J.K.; France, B.; Cote, C.K.; Jenkins, A.; Bozue, J.A.; Welkos, S.L.; Bhargava, R.; Ho, C.L.; Mehrabian, M.; Pan, C.; et al. Allelic variation on murine chromosome 11 modifies host inflammatory responses and resistance to Bacillus anthracis. PLoS Pathog. 2011, 7, e1002469. [Google Scholar] [CrossRef]
- Cote, C.K.; Rossi, C.A.; Kang, A.S.; Morrow, P.R.; Lee, J.S.; Welkos, S.L. The detection of protective antigen (PA) associated with spores of Bacillus anthracis and the effects of anti-PA antibodies on spore germination and macrophage interactions. Microb. Pathog. 2005, 38, 209–225. [Google Scholar] [CrossRef]
- Scobie, H.M.; Rainey, G.J.; Bradley, K.A.; Young, J.A. Human capillary morphogenesis protein 2 functions as an anthrax toxin receptor. Proc. Natl. Acad. Sci. USA 2003, 100, 5170–5174. [Google Scholar]
- Reeves, C.V.; Dufraine, J.; Young, J.A.; Kitajewski, J. Anthrax toxin receptor 2 is expressed in murine and tumor vasculature and functions in endothelial proliferation and morphogenesis. Oncogene 2010, 29, 789–801. [Google Scholar]
- Klimpel, K.R.; Molloy, S.S.; Thomas, G.; Leppla, S.H. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc. Natl. Acad. Sci. USA 1992, 89, 10277–10281. [Google Scholar]
- Panchal, R.G.; Halverson, K.M.; Ribot, W.; Lane, D.; Kenny, T.; Abshire, T.G.; Ezzell, J.W.; Hoover, T.A.; Powell, B.; Little, S.; et al. Purified Bacillus anthracis lethal toxin complex formed in vitro and during infection exhibits functional and biological activity. J. Biol. Chem. 2005, 280, 10834–10839. [Google Scholar]
- Molloy, S.S.; Anderson, E.D.; Jean, F.; Thomas, G. Bi-cycling the furin pathway: from TGN localization to pathogen activation and embryogenesis. Trends Cell Biol. 1999, 9, 28–35. [Google Scholar]
- Komiyama, T.; Coppola, J.M.; Larsen, M.J.; van Dort, M.E.; Ross, B.D.; Day, R.; Rehemtulla, A.; Fuller, R.S. Inhibition of furin/proprotein convertase-catalyzed surface and intracellular processing by small molecules. J. Biol. Chem. 2009, 284, 15729–15738. [Google Scholar]
- Anes, E.; Peyron, P.; Staali, L.; Jordao, L.; Gutierrez, M.G.; Kress, H.; Hagedorn, M.; Maridonneau-Parini, I.; Skinner, M.A.; Wildeman, A.G.; et al. Dynamic life and death interactions between Mycobacterium smegmatis and J774 macrophages. Cell Microbiol. 2006, 8, 939–960. [Google Scholar] [CrossRef]
- Kalamidas, S.A.; Kuehnel, M.P.; Peyron, P.; Rybin, V.; Rauch, S.; Kotoulas, O.B.; Houslay, M.; Hemmings, B.A.; Gutierrez, M.G.; Anes, E.; et al. cAMP synthesis and degradation by phagosomes regulate actin assembly and fusion events: consequences for mycobacteria. J. Cell. Sci. 2006, 119, 3686–3694. [Google Scholar]
- Gimenez, A.P.; Wu, Y.-Z.; Paya, M.; Delclaux, C.; Touqui, L.; Goossens, P.L. High bactericidal efficiency of type iia phospholipase A2 against Bacillus anthracis and inhibition of its secretion by the lethal toxin. J. Immunol. 2004, 173, 521–530. [Google Scholar]
- Raymond, B.; Ravaux, L.; Mémet, S.; Wu, Y.; Sturny-Leclère, A.; Leduc, D.; Denoyelle, C.; Goossens, P.L.; Payá, M.; Raymondjean, M.; et al. Anthrax lethal toxin down-regulates type-IIA secreted phospholipase A(2) expression through MAPK/NF-kappaB inactivation. Biochem. Pharmacol. 2010, 79, 1149–1155. [Google Scholar]
- Steinberg, B.E.; Grinstein, S. Pathogen destruction versus intracellular survival: the role of lipids as phagosomal fate determinants. J. Clin. Invest. 2008, 118, 2002–2011. [Google Scholar]
- Cote, C.K.; DiMezzo, T.L.; Banks, D.J.; France, B.; Bradley, K.A.; Welkos, S.L. Early interactions between fully virulent Bacillus anthracis and macrophages that influence the balance between spore clearance and development of a lethal infection. Microbes. Infect. 2008, 10, 613–619. [Google Scholar] [CrossRef]
- Tan, Y.K.; Vu, H.A.; Kusuma, C.M.; Wu, A. Implications of autophagy in anthrax pathogenicity. Autophagy 2009, 5, 734–735. [Google Scholar]
- Ebrahimi, C.M.; Sheen, T.R.; Renken, C.W.; Gottlieb, R.A.; Doran, K.S. Contribution of lethal toxin and edema toxin to the pathogenesis of anthrax meningitis. Infect. Immun. 2011, 79, 2510–2518. [Google Scholar] [CrossRef]
- Shahnazari, S.; Namolovan, A.; Mogridge, J.; Kim, P.K.; Brumell, J.H. Bacterial toxins can inhibit host cell autophagy through cAMP generation. Autophagy 2011, 7, 957–965. [Google Scholar]
- Tweten, R.K. Cholesterol-dependent cytolysins, a family of versatile pore-forming toxins. Infect. Immun. 2005, 73, 6199–6209. [Google Scholar]
- Shannon, J.G.; Ross, C.L.; Koehler, T.M.; Rest, R.F. Characterization of anthrolysin O, the Bacillus anthracis cholesterol-dependent cytolysin. Infect. Immun. 2003, 71, 3183–3189. [Google Scholar] [CrossRef]
- Mosser, E.M.; Rest, R.F. The Bacillus anthracis cholesterol-dependent cytolysin, Anthrolysin O, kills human neutrophils, monocytes and macrophages. BMC Microbiol. 2006, 6, 56. [Google Scholar] [CrossRef]
- Cocklin, S.; Jost, M.; Robertson, N.M.; Weeks, S.D.; Weber, H.-W.; Young, E.; Seal, S.; Zhang, C.; Mosser, E.; Loll, P.J.; et al. Real-time monitoring of the membrane-binding and insertion properties of the cholesterol-dependent cytolysin anthrolysin O from Bacillus anthracis. J. Mol. Recognit. 2006, 19, 354–362. [Google Scholar] [CrossRef]
- Bourdeau, R.W.; Malito, E.; Chenal, A.; Bishop, B.L.; Musch, M.W.; Villereal, M.L.; Chang, E.B.; Mosser, E.M.; Rest, R.F.; Tang, W.J. Cellular functions and X-ray structure of anthrolysin O, a cholesterol-dependent cytolysin secreted by Bacillus anthracis. J. Biol. Chem. 2009, 284, 14645–14656. [Google Scholar]
- Bishop, B.L.; Lodolce, J.P.; Kolodziej, L.E.; Boone, D.L.; Tang, W.J. The role of anthrolysin O in gut epithelial barrier disruption during Bacillus anthracis infection. Biochem. Biophys. Res. Commun 2010, 394, 254–259. [Google Scholar] [CrossRef]
- Klichko, V.I.; Miller, J.; Wu, A.; Popov, S.G.; Alibek, K. Anaerobic induction of Bacillus anthracis hemolytic activity. Biochem. Biophys. Res. Commun. 2003, 303, 855–862. [Google Scholar] [CrossRef]
- Gilbert, R.J. Cholesterol-dependent cytolysins. Adv. Exp. Med. Biol. 2010, 677, 56–66. [Google Scholar]
- Schnupf, P.; Portnoy, D.A. Listeriolysin O: a phagosome-specific lysin. Microbes Infect. 2007, 9, 1176–1187. [Google Scholar]
- Wei, Z.; Schnupf, P.; Poussin, M.A.; Zenewicz, L.A.; Shen, H.; Goldfine, H. Characterization of Listeria monocytogenes expressing anthrolysin O and phosphatidylinositol-specific phospholipase C from Bacillus anthracis. Infect. Immun. 2005, 73, 6639–6646. [Google Scholar] [CrossRef]
- Heffernan, B.J.; Thomason, B.; Herring-Palmer, A.; Hanna, P. Bacillus anthracis anthrolysin O and three phospholipases C are functionally redundant in a murine model of inhalation anthrax. FEMS Microbiol. Lett. 2007, 271, 98–105. [Google Scholar] [CrossRef]
- Read, T.D.; Peterson, S.N.; Tourasse, N.; Baillie, L.W.; Paulsen, I.T.; Nelson, K.E.; Tettelin, H.; Fouts, D.E.; Eisen, J.A.; Gill, S.R.; et al. The genome sequence of Bacillus anthracis Ames and comparison to closely related bacteria. Nature 2003, 423, 81–86. [Google Scholar]
- Heffernan, B.J.; Thomason, B.; Herring-Palmer, A.; Shaughnessy, L.; McDonald, R.; Fisher, N.; Huffnagle, G.B.; Hanna, P. Bacillus anthracis phospholipases C facilitate macrophage-associated growth and contribute to virulence in a murine model of inhalation anthrax. Infect. Immun. 2006, 74, 3756–3764. [Google Scholar]
- Alberti-Segui, C.; Goeden, K.R.; Higgins, D.E. Differential function of Listeria monocytogenes listeriolysin O and phospholipases C in vacuolar dissolution following cell-to-cell spread. Cell Microbiol. 2007, 9, 179–195. [Google Scholar] [CrossRef]
- Raines, K.W.; Kang, T.J.; Hibbs, S.; Cao, G.-L.; Weaver, J.; Tsai, P.; Baillie, L.; Cross, A.S.; Rosen, G.M. Importance of nitric oxide synthase in the control of infection by Bacillus anthracis. Infect. Immun. 2006, 74, 2268–2276. [Google Scholar]
- Weaver, J.; Kang, T.J.; Raines, K.W.; Cao, G.L.; Hibbs, S.; Tsai, P.; Baillie, L.; Rosen, G.M.; Cross, A.S. Protective role of Bacillus anthracis exosporium in macrophage-mediated killing by nitric oxide. Infect. Immun. 2007, 75, 3894–3901. [Google Scholar]
- Porasuphatana, S.; Cao, G.L.; Tsai, P.; Tavakkoli, F.; Huwar, T.; Baillie, L.; Cross, A.S.; Shapiro, P.; Rosen, G.M. Bacillus anthracis endospores regulate ornithine decarboxylase and inducible nitric oxide synthase through ERK1/2 and p38 mitogen-activated protein kinases. Curr. Microbiol. 2010, 61, 567–573. [Google Scholar]
- Viator, R.J.; Rest, R.F.; Hildebrandt, E.; McGee, D.J. Characterization of Bacillus anthracis arginase: effects of pH, temperature, and cell viability on metal preference. BMC Biochem. 2008, 9, 15. [Google Scholar] [CrossRef]
- Cybulski, R.J.; Sanz, P.; Alem, F.; Stibitz, S.; Bull, R.L.; O’Brien, A.D. Four superoxide dismutases contribute to Bacillus anthracis virulence and provide spores with redundant protection from oxidative stress. Infect. Immun. 2009, 77, 274–285. [Google Scholar]
- Zamocky, M.; Furtmüller, P.G.; Obinger, C. Evolution of catalases from bacteria to humans. Antioxid Redox Signal. 2008, 10, 1527–1548. [Google Scholar]
- Shatalin, K.; Gusarov, I.; Avetissova, E.; Shatalina, Y.; McQuade, L.E.; Lippard, S.J.; Nudler, E. Bacillus anthracis-derived nitric oxide is essential for pathogen virulence and survival in macrophages. Proc. Natl. Acad. Sci. USA 2008, 105, 1009–1013. [Google Scholar]
- Makino, S.; Watarai, M.; Cheun, H.I.; Shirahata, T.; Uchida, I. Effect of the lower molecular capsule released from the cell surface of Bacillus anthracis on the pathogenesis of anthrax. J. Infect. Dis. 2002, 186, 227–233. [Google Scholar] [CrossRef]
- Scorpio, A.; Chabot, D.J.; Day, W.A.; O’Brien, D.K.; Vietri, N.J.; Itoh, Y.; Mohamadzadeh, M.; Friedlander, A.M. Poly-γ-glutamate capsule-degrading enzyme treatment enhances phagocytosis and killing of encapsulated Bacillus anthracis. Antimicrob. Agents Chemother. 2007, 51, 215–222. [Google Scholar] [CrossRef]
- Scorpio, A.; Chabot, D.J.; Day, W.A.; Hoover, T.A.; Friedlander, A.M. Capsule depolymerase overexpression reduces Bacillus anthracis virulence. Microbiology 2010, 156, 1459–1467. [Google Scholar] [CrossRef]
- Ryter, A.; Frehel, C.; Rastogi, N.; David, H.L. Macrophage interaction with mycobacteria including M. leprae. Acta Leprol. 1984, 2, 211–226. [Google Scholar]
- Hart, P.D.; Young, M.R. Polyanionic agents inhibit phagosome-lysosome fusion in cultured macrophages: a reply to the suggestion of Goren, Vatter, and Fiscus to the contrary. J. Leukoc. Biol. 1988, 43, 179–182. [Google Scholar]
- Yessine, M.A.; Leroux, J.C. Membrane-destabilizing polyanions: interaction with lipid bilayers and endosomal escape of biomacromolecules. Adv. Drug Deliv. Rev. 2004, 56, 999–1021. [Google Scholar]
- Boyer, A.E.; Quinn, C.P.; Hoffmaster, A.R.; Kozel, T.R.; Saile, E.; Marston, C.K.; Percival, A.; Plikaytis, B.D.; Woolfitt, A.R.; Gallegos, M.; et al. Kinetics of lethal factor and poly-D-glutamic acid antigenemia during inhalation anthrax in rhesus macaques. Infect. Immun. 2009, 77, 3432–3441. [Google Scholar]
- Cote, C.K.; Rea, K.M.; Norris, S.L.; van Rooijen, N.; Welkos, S.L. The use of a model of in vivo macrophage depletion to study the role of macrophages during infection with Bacillus anthracis spores. Microb. Pathog. 2004, 37, 169–175. [Google Scholar] [CrossRef]
- Kang, T.J.; Fenton, M.J.; Weiner, M.A.; Hibbs, S.; Basu, S.; Baillie, L.; Cross, A.S. Murine macrophages kill the vegetative form of Bacillus anthracis. Infect. Immun. 2005, 73, 7495–7501. [Google Scholar] [CrossRef]
- Gut, I.M.; Tamilselvam, B.; Prouty, A.M.; Stojkovic, B.; Czeschin, S.; van der Donk, W.A.; Blanke, S.R. Bacillus anthracis spore interactions with mammalian cells: relationship between germination state and the outcome of in vitro. BMC Microbiol. 2011, 11, 46. [Google Scholar] [CrossRef]
- Cote, C.K.; Van Rooijen, N.; Welkos, S.L. Roles of macrophages and neutrophils in the early host response to Bacillus anthracis spores in a mouse model of infection. Infect. Immun. 2006, 74, 469–480. [Google Scholar] [CrossRef]
- Cleret, A.; Quesnel-Hellmann, A.; Vallon-Eberhard, A.; Verrier, B.; Jung, S.; Vidal, D.; Mathieu, J.; Tournier, J.N. Lung dendritic cells rapidly mediate anthrax spore entry through the pulmonary route. J. Immunol. 2007, 178, 7994–8001. [Google Scholar]
- Shetron-Rama, L.M.; Herring-Palmer, A.C.; Huffnagle, G.B.; Hanna, P. Transport of Bacillus anthracis from the lungs to the draining lymph nodes is a rapid process facilitated by CD11c+ cells. Microb. Pathog. 2010, 49, 38–46. [Google Scholar] [CrossRef]
- Savina, A.; Jancic, C.; Hugues, S.; Guermonprez, P.; Vargas, P.; Moura, I.C.; Lennon-Duménil, A.M.; Seabra, M.C.; Raposo, G.; Amigorena, S. NOX2 controls phagosomal pH to regulate antigen processing during crosspresentation by dendritic cells. Cell 2006, 126, 205–218. [Google Scholar]
- Russell, D.G.; Vanderven, B.C.; Glennie, S.; Mwandumba, H.; Heyderman, R.S. The macrophage marches on its phagosome: dynamic assays of phagosome function. Nat. Rev. Immunol. 2009, 9, 594–600. [Google Scholar]
- Schwartz, M. Dr. Jekyll and Mr. Hyde: a short history of anthrax. Mol. Aspects Med. 2009, 30, 347–355. [Google Scholar] [CrossRef]
© 2012 by the authors; licensee MDPI, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Tonello, F.; Zornetta, I. Bacillus anthracis Factors for Phagosomal Escape. Toxins 2012, 4, 536-553. https://doi.org/10.3390/toxins4070536
Tonello F, Zornetta I. Bacillus anthracis Factors for Phagosomal Escape. Toxins. 2012; 4(7):536-553. https://doi.org/10.3390/toxins4070536
Chicago/Turabian StyleTonello, Fiorella, and Irene Zornetta. 2012. "Bacillus anthracis Factors for Phagosomal Escape" Toxins 4, no. 7: 536-553. https://doi.org/10.3390/toxins4070536




