Fabrication of a Malaria-Ab ELISA Bioassay Platform with Utilization of Syringe-Based and 3D Printed Assay Automation
Abstract
:1. Introduction
1.1. Preface
1.2. Fabrication Techniques for Microfluidic Devices
1.2.1. Soft Lithography
1.2.2. Inkjet 3D Printing (i3DP)
1.2.3. Two-Photon Polymerization (2PP)
1.2.4. Fused Deposition Modeling (FDM)
1.2.5. Stereolithography (SLA)
1.3. Combining Several Fabrication Techniques to Manufacture an Automated Fluidic Malaria Enzyme-Linked Immunosorbent Assay (ELISA) Bioassay Platform
2. Materials and Methods
2.1. Fused Deposition Modeling and Stereolithography
2.2. Automation of Malaria-Ab Colorimetric ELISA
- (1)
- Pipette 50 µL of sample into the wells (O). Incubate for 1 hr at room temperature.
- (2)
- Aspirate the sample from the well. Flush the well with wash solution contained within the elastomeric dome (N). The wash solution is dispensed using the movable arm (M) to compress the dome.
- (3)
- Aspirate the dirty wash solution from the well using an aspiration syringe located on the bottom platform. Repeat three times.
- (4)
- Dispense 50 µL of malaria conjugate into the reagent well (O) from a syringe (F). The barrel of this syringe is pushed using a servomotor (H). Incubate for 30 min at room temperature.
- (5)
- Aspirate the conjugate from the well. Repeat step 3.
- (6)
- Dispense 50 µL of the TMB substrate solution into the reagent well (O) from a syringe on the syringe platform (F). The barrel of this syringe is pushed using a servomotor (G). Incubate for 15 min at room temperature.
- (7)
- Dispense 50 µL of stop solution into the reagent well (O) from a syringe on the syringe platform (F). The barrel of this syringe is pushed using a servomotor (E).
- (8)
- Visually inspect the color change if the platform is used for qualitative, rather than quantitative analysis. Alternatively, position a cell phone on the frame (P) and align the phone camera to the reagent wells (O) to read the results using a special colorimetric detection app, Color Catcher (Cloud Innovation Team, Austin, TX, USA) [66]. This app reads RBG values from scanned or photographed images.
2.3. Hardware
3. Results
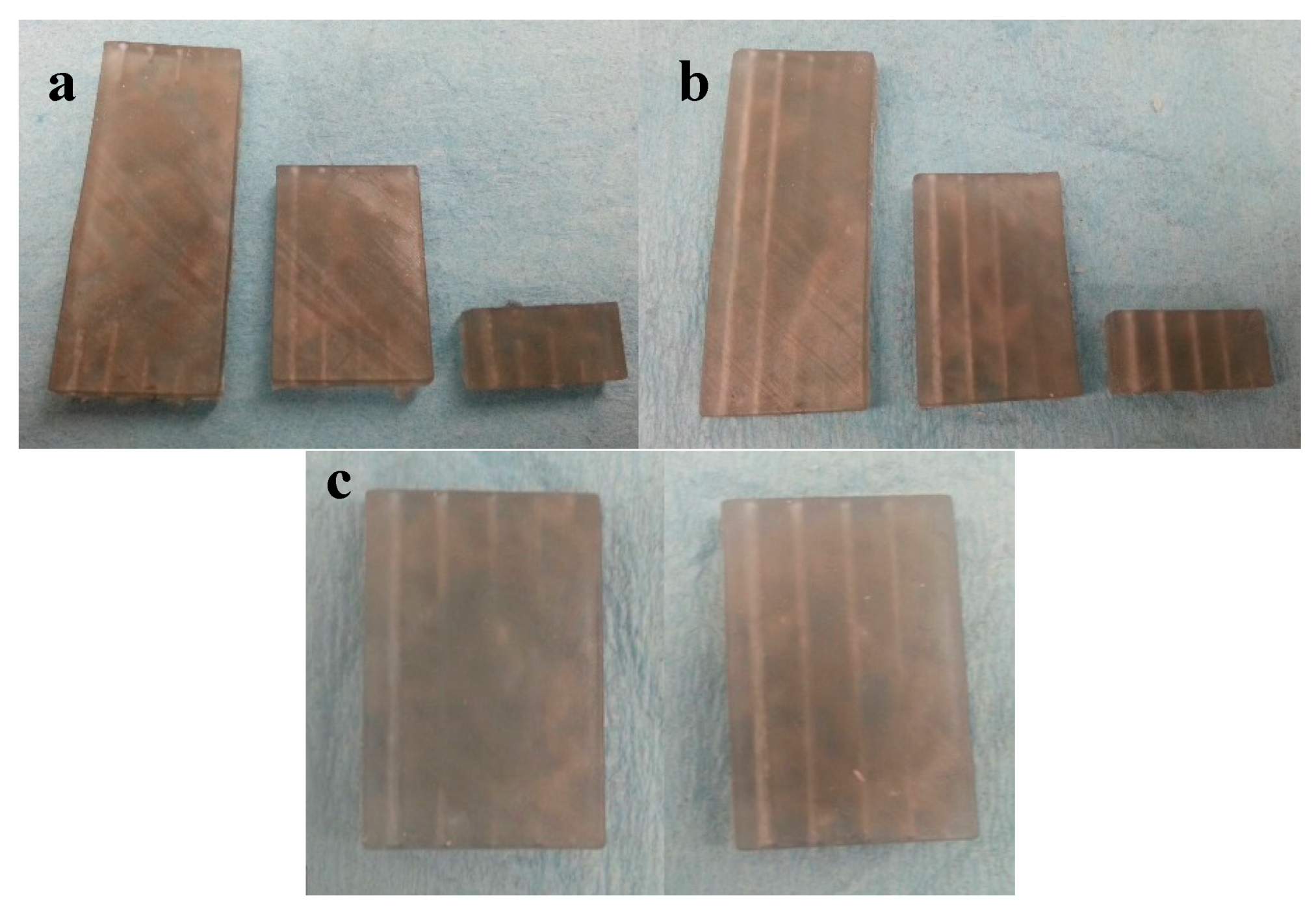
3.1. Fused Deposition Modeling Optimization
3.2. Stereolithographic Fabrication Optimization
3.3. Channel Deformation
3.4. Performance of the Automated System
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Urrios, A.; Parra-Cabrera, C.; Bhattacharjee, N.; Gonzalez-Suarez, A.M.; Rigat-Brugarolas, L.G.; Nallapatti, U.; Samitier, J.; DeForest, C.A.; Posas, F.; Garcia-Cordero, J.L.; et al. 3D-printing of transparent bio-microfluidic devices in PEG-DA. Lab Chip 2016, 16, 2287–2294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crowther, J. The Elisa Guidebook; Springer Science & Business Media: Berlin, Germany, 2009; p. 54. [Google Scholar]
- Wiltbank, T.; McCaroll, D.; Wartick, M. An undetectable source of technical error that could lead to false negative results in enzyme linked immunosorbent assay of antibodies to HIV-1. Rapid Commun. 1988, 29, 75–77. [Google Scholar] [CrossRef]
- Knowlton, S.; Yu, C.H.; Ersoy, F.; Emadi, S.; Khademhosseini, A.; Tasoglu, S. 3D-printed microfluidic Chips with patterned, cell-laden hydrogel constructs. Biofabrication 2016, 8, 025019. [Google Scholar] [CrossRef] [PubMed]
- Ellerbee, A.K.; Phillips, S.T.; Siegel, A.C.; Mirica, K.A.; Martinez, A.W.; Striehl, P.; Jain, N.; Prentiss, M.; Whitesides, G.M. Quantifying colorimetric assays in paper-based microfluidic devices by measuring the transmission of light through paper. Anal. Chem. 2009, 81, 8447–8452. [Google Scholar] [CrossRef] [PubMed]
- Lutz, B.; Liang, T.; Fu, E.; Ramachandran, S.; Kauffman, P.; Yager, P. Dissolvable fluidic time delays for programming multi-step assays in instrument-free paper diagnostics. Lab Chip 2013, 13, 2840–2847. [Google Scholar] [CrossRef] [PubMed]
- Schaller, V.; Sanz-Velasco, A.; Kalabukhov, A.; Schneiderman, J.F.; Öisjöen, F.; Jesorka, A.; Astalan, A.P.; Krozer, A.; Rusu, C.; Enoksson, P.; et al. Towards an electrowetting-based digital microfluidic platform for magnetic immunoassays. Lab Chip 2009, 9, 3433–3436. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Hejazian, M.; Ooi, C.H.; Kashaninejad, N. Recent advances and future perspectives on microfluidic liquid handling. Micromachines 2017, 8, 186. [Google Scholar] [CrossRef]
- Cevenini, L.; Calabretta, M.M.; Tarantino, G.; Michelini, E.; Roda, A. Smartphone-interfaced 3D printed toxicity biosensor integrating bioluminescent “sentinel cells”. Sens. Actuators 2016, 225, 249–257. [Google Scholar] [CrossRef]
- Comina, A.; Suska, A.; Filippini, G. A 3D printed device for quantitative enzymatic detection using cell phones. Anal. Methods 2016, 8, 6135–6142. [Google Scholar] [CrossRef]
- Bauer, M.; Kulinksy, L. Fabrication of a lab-on-chip device using material extrusion (3D printing) and demonstration via Malaria-Ab ELISA. Micromachines 2018, 9, 27. [Google Scholar] [CrossRef]
- Crowther, J. The Elisa Guidebook; Springer Science & Business Media: Berlin, Germany, 2009; p. 332. [Google Scholar]
- Becker, H.; Locascio, L. Polymer microfluidic devices. Talanta 2002, 56, 267–287. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, L.; Kane, S.; Deng, Y.; Jung, Y.G.; Lee, G.H.; Zhang, J. Additive manufacturing of metallic materials: A review. J. Mater. Eng. Perform. 2018, 27, 1–13. [Google Scholar] [CrossRef]
- Parra-Cabrera, C.; Achille, C.; Kuhn, S.; Ameloot, R. 3D printing in chemical engineering and catalytic technology: Structured catalysts, mixers and reactors. Chem. Soc. Rev. 2018, 47, 209–230. [Google Scholar] [CrossRef] [PubMed]
- Betancourt, T.; Brannon-Peppas, L. Micro- and nanofabrication methods in nanotechnological medical and pharmaceutical devices. Int. J. Nanomed. 2006, 1, 483–495. [Google Scholar] [CrossRef] [Green Version]
- Sugioka, K.; Cheng, Y. Femtosecond laser processing for optofluidic fabrication. Lab Chip 2012, 12, 3576. [Google Scholar] [CrossRef] [PubMed]
- Yalikun, Y.; Hosokawa, Y.; Lino, T.; Tanaka, Y. An all-glass 12 μm ultra-thin and flexible micro-fluidic chip fabricated by femtosecond laser processing. Lab Chip 2016, 16, 2427–2433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rolland, J.P.; Van Dam, R.M.; Schorzman, D.A.; Quake, S.R.; DeSimone, J.M. Solvent-resistant photocurable “liquid teflon” for microfluidic device fabrication. J. Am. Chem. Soc. 2004, 126, 232. [Google Scholar] [CrossRef] [PubMed]
- Beebe, D.J.; Moore, J.S.; Yu, Q.; Liu, R.H.; Kraft, M.L.; Jo, B.H.; Devadoss, C. Microfluidic tectonics: A comprehensive construction platform for microfluidic systems. Proc. Natl. Acad. Sci. USA 2000, 97, 13488–13493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.; Kim, H.; Lee, W.; Kim, J. Finger-triggered portable PDMS suction cup for equipment-free microfluidic pumping. Micro Nano Syst. Lett. 2018, 6, 1–5. [Google Scholar] [CrossRef]
- Yazdi, A.; Popma, A.; Wong, W.; Nguyen, T.; Pan, Y.; Xu, J. 3D printing: an emerging tool for novel microfluidics and lab-on-a-chip applications. Microfluid. Nanofluid. 2016, 20, 50. [Google Scholar] [CrossRef]
- He, Y.; Wu, Y.; Fu, J.Z.; Gao, Q.; Qiu, J.J. Developments of 3D printing microfluidics and applications in chemistry and biology: A review. Electroanalysis 2016, 28, 1658–1678. [Google Scholar] [CrossRef]
- Zhang, C.; Bills, B.; Manicke, N. Rapid prototyping using 3D printing in bioanalytical research. Bioanalysis 2017, 9, 329–331. [Google Scholar] [CrossRef] [PubMed]
- Tang, S.; Whitesides, G. Basic Microfluidic and Soft Lithographic Techniques. Available online: https://gmwgroup.harvard.edu/pubs/pdf/1073.pdf (accessed on 25 May 2018).
- Unger, M.A.; Chou, H.P.; Thorsen, T.; Scherer, A.; Quake, S.R. Monolithic microfabricated valves and pumps by multilayer soft lithography. Science 2000, 288, 113–116. [Google Scholar] [CrossRef] [PubMed]
- Thorsen, S.; Maerkl, S.J.; Quake, S.R. Microfluidic large-scale integration. Science 2002, 298, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Waheed, S.; Cabot, J.M.; Macdonald, N.P.; Lewis, T.; Guijt, R.M.; Paull, B.; Breadmore, M.C. 3D printed microfluidic devices: Enablers and barriers. Lab Chip 2016, 16, 1993–2013. [Google Scholar] [CrossRef] [PubMed]
- Hopkinson, N.; Smith, P. Handbook of Industrial Inkjet Printing: A full System; John Wiley & Sons: Hoboken, NJ, USA, 2018. [Google Scholar]
- Pilipović, A.; Raos, P.; Šercer, M. Experimental analysis of properties of materials for rapid prototyping. Int. J. Adv. Des. Manuf. Technol. 2009, 40, 105–115. [Google Scholar] [CrossRef]
- Mueller, J.; Courty, D.; Spielhofer, M.; Spolenak, R.; Shea, K. Mechanical properties of interfaces in inkjet 3D printed single- and multi-material parts. 3D Print. Addit. Manuf. 2017, 4, 193–199. [Google Scholar] [CrossRef]
- Anderson, K.B.; Lockwood, S.Y.; Martin, R.S.; Spence, D.M. A 3D printed fluidic device that enables integrated features. Anal. Chem. 2013, 85, 5622–5626. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, S.Y.; Meisel, J.E.; Monsma, F.J., Jr.; Spence, D.M. A diffusion-based and dynamic 3D-printed device that enables parallel in vitro pharmacokinetic profiling of molecules. Anal. Chem. 2016, 88, 1864–1870. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Y.; Paydar, O.; Candler, R. 3D printed molds for non-planar PDMS microfluidic channels. Sens. Actuators A Phys. 2015, 226, 137–142. [Google Scholar] [CrossRef]
- Paydar, O.H.; Paredes, C.N.; Hwang, Y.; Paz, J.; Shah, N.B.; Candler, R.N. Characterization of 3D-printed microfluidic chip interconnects with integrated O-rings. Sens. Actuators A Phys. 2014, 205, 199–203. [Google Scholar] [CrossRef]
- Staudinger, U.; Zyla, G.; Krause, B.; Janke, A.; Fischer, D.; Esen, C. Development of electrically conductive microstructures based on polymer/CNT nanocomposites via two-photon polymerization. Microelectron. Eng. 2017, 179, 48–55. [Google Scholar] [CrossRef]
- Xing, J.F.; Zheng, M.L.; Duan, X.M. Two-photon polymerization microfabrication of hydrogels: An advanced 3D printing technology for tissue engineering and drug delivery. Chem. Soc. Rev. 2015, 44, 5031–5039. [Google Scholar] [CrossRef] [PubMed]
- Kumi, G.; Yanez, C.; Belfield, K.; Fourkas, J.T. High-speed multiphoton absorption polymerization: Fabrication of microfluidic channels with arbitrary cross-sections and high aspect ratios. Lab Chip 2010, 10, 1057–1060. [Google Scholar] [CrossRef] [PubMed]
- Kawata, S.; Sun, H.B.; Tanaka, T.; Takada, K. Finer features for functional microdevices. Nature 2001, 412, 697–698. [Google Scholar] [CrossRef] [PubMed]
- Sugioka, K.; Cheng, Y. Femtosecond laser three-dimensional micro- and nanofabrication. Appl. Phys. Rev. 2014, 1, 041303. [Google Scholar] [CrossRef] [Green Version]
- Ziemian, C.M.; Crawn, P.M. Computer aided decision support for fused deposition modelling. Rapid Prototyp. J. 2001, 7, 138–147. [Google Scholar] [CrossRef]
- Modjarrad, K.; Ebnesajjad, S. Handbook of Polymer Applications in Medicine and Medical Devices; William Andrew Publishing: Norwich, NY, USA, 2014. [Google Scholar]
- Chia, H.; Wu, B. Recent advances in 3D printing of biomaterials. J. Biol. Eng. 2015, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Zhang, M.; Yeong, W. Characterization and evaluation of 3D printed microfluidic chip for cell processing. Microfluid. Nanofluid. 2016, 20, 1–15. [Google Scholar] [CrossRef]
- Kitson, P.J.; Symes, M.D.; Dragone, V.; Cronin, L. Combining 3D printing and liquid handling to produce user-friendly reactionware for chemical synthesis and purification. Chem. Sci. 2013, 4, 3099–3103. [Google Scholar] [CrossRef] [Green Version]
- Bishop, G.W.; Satterwhite, J.E.; Bhakta, S.; Kadimisetty, K.; Gillette, K.M.; Chen, E.; Rusling, J.F. 3D-printed fluidic devices for nanoparticle preparation and flow-injection amperometry using integrated prussian blue nanoparticle-modified electrodes. Anal. Chem. 2015, 87, 5437–5443. [Google Scholar] [CrossRef] [PubMed]
- Sher, D. “Dolomite’s Fluidic Factory 3D Prints $1 Microfluidic Chips.” 3D Printing Industry, 2015. Available online: https://3dprintingindustry.com/news/dolomites-fluidic-factory-3d-prints-1-microfluidic-chips-60883/ (accessed on 25 May 2018).
- 3D Systems, Inc. Available online: https://www.3dsystems.com/ (accessed on 25 May 2018).
- Au, A.; Lee, W.; Folch, A. Mail-order microfluidics: Evaluation of stereolithography for the production of microfluidic devices. Lab Chip 2014, 14, 1294–1301. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Chen, Y.; Yang, Z.G.; Khoshnevis, B. Development of a multi-material mask-image-projection-based stereolithography for the fabrication of digital materials. Rapid Prototyp. J. 2013, 19, 153–165. [Google Scholar] [CrossRef]
- Zhang, X.; Jiang, X.N.; Sun, C. Micro-stereolithography of polymeric and ceramic microstructures. Sens. Actuators A Phys. 1999, 77, 149–156. [Google Scholar] [CrossRef]
- Amend, P.; Hentschel, O.; Scheitler, C.; Baum, M.; Heberle, J.; Roth, S.; Schmidt, M. Fast and flexible generation of conductive circuits. J. Laser Micro/Nanoeng. 2013, 8, 276–286. [Google Scholar] [CrossRef]
- Comina, G.; Suska, A.; Filippini, D. PDMS lab-on-a-chip fabrication using 3D printed templates. Lab Chip 2014, 14, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Comina, G.; Suska, A.; Filippini, D. Low cost lab-on-a-chip prototyping with a consumer grade 3D printer. Lab Chip 2014, 14, 2978–2982. [Google Scholar] [CrossRef] [PubMed]
- Comina, G.; Suska, A.; Filippini, D. Autonomous chemical sensing interface for universal cell phone readout. Chem. Int. Ed. 2015, 54, 8708–8712. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cai, X.; Guo, Q.; Zhang, T.; Kobe, B.; Yang, J. i3DP, a robust 3D printing approach enabling genetic post-printing surface modification. Chem. Commun. 2013, 49, 10064–10066. [Google Scholar] [CrossRef] [PubMed]
- Shallan, A.I.; Smejkal, P.; Corban, M.; Guijt, R.M.; Breadmore, M.C. Cost-Effective Three-Dimensional Printing of Visibly Transparent Microchips within Minutes. Anal. Chem. 2014, 86, 3124–3130. [Google Scholar] [CrossRef] [PubMed]
- Patrick, W.G.; Nielsen, A.A.; Keating, S.J.; Levy, T.J.; Wang, C.W.; Rivera, J.J.; Mondragón-Palomino, O.; Carr, P.A.; Voigt, C.A.; Oxman, N.; et al. DNA assembly in 3D printed fluidics. PLoS ONE 2015, 10, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.G.; Park, K.J.; Seok, S.; Shin, S.; Park, J.Y.; Heo, Y.S.; Lee, S.J.; Lee, J.L. 3D printed modules for integrated microfluidic devices. RSC Adv. 2014, 4, 32876–32880. [Google Scholar] [CrossRef]
- Bhargava, K.; Thompson, B.; Malmstadt, N. Discrete elements for 3D microfluidics. PNAS 2014, 111, 15013–150138. [Google Scholar] [CrossRef] [PubMed]
- Lai, H.; Folch, A. Design and dynamic characterization of “single-stroke” peristaltic PDMS micropumps. Lab Chip 2011, 11, 336–342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhushan, B.; Caspers, M. An overview of additive manufacturing (3D printing) for microfabrication. Microsyst. Technol. 2017, 23, 1117. [Google Scholar] [CrossRef]
- Garcia, J.; Yang, Z.; Mongrain, R.; Leask, R.L.; Lachapelle, K. 3D printing materials and their use in medical education: A review of current technology and trends for the future. BMJ. Simul. Technol. Enhanc. Learn. 2018, 4, 27–40. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Malaria. Available online: http://www.who.int/mediacentre/factsheets/fs094/en (accessed on 26 May 2018).
- Malaria-Ab-ELISA. Available online: http://www.ibl-international.com/media/catalog/product/R/E/RE58601_IFU_en_Malaria-Ab_ELISA_V4_2011-08-03_sym3.pdf (accessed on 26 May 2018).
- Color Catcher. Available online: http://appcrawlr.com/android/color-catcher-free (accessed on 26 May 2018).
- Zhou, Y. The recent development and applications of fluidic channels by 3D printing. J. Biomed. Sci. 2017, 24, 80. [Google Scholar] [CrossRef] [PubMed]





| ELISA Step | Malaria-Ab ELISA Kit Instruction | Automated Assay Modifications |
|---|---|---|
| Sample | Add 50 μL of the undiluted sample to a coated well. Mix on a plate shaker for 30 s. Incubate (covered) at 37 °C for 30 min. | 50 µL of sample is pipetted into the wells (O). Incubation occurs for 1 hr at room temperature. |
| Wash | Wash five times with 300 μL of working strength wash buffer. A short soak time of about 30 s is recommended between each wash cycle. Tap out excess liquid. | The well is flushed with 300 μL wash solution contained within the elastomeric dome (N) as the movable arm (M) compresses the dome. The arm is controlled by the servomotor (L) and Arduino board (J). The dirty wash solution is aspirated from the well using an aspiration syringe located on the bottom platform. The syringe is driven by 3D printed rack-and-gear set (B) and the servomotor (C). The wash/aspiration cycle is repeated three times. |
| Conjugate Incubation | Add 50 μL of diluted (1:10) conjugate to each well. Incubate (covered) at 37 °C for 30 min. | 50 µL of diluted malaria conjugate is dispensed into the reagent well (O) from a syringe (F). The barrel of this syringe is pushed using a servomotor (H) controlled by the Arduino board (D). Incubation occurs for 30 min at room temperature. |
| Wash | See wash step above. | See wash step above. |
| Substrate Incubation | Add 50 μL substrate /chromogen Tetramethylbenzidine (TMB) mixture to each well. Incubate at room temperature for 30 min. As the substrate is photosensitive, it is recommended that the plate be protected from light during this incubation. | 50 µL of TMB substrate solution is dispensed into the reagent well (O) from a syringe on the syringe platform (F). The barrel of this syringe is pushed using a servomotor (G) controlled by the Arduino board (D). Incubation occurs for 15 min. |
| Stop | Add 50 μL stop solution to each well. (Blue color changes to yellow). | 50 µL of stop solution is dispensed into the reagent well (O) from a syringe (F). The barrel of this syringe is pushed using a servomotor (E) controlled by the Arduino board (D). |
| Detection | Read with fluorescent microplate reader at 450 nm (A450). Use of a reference filter at 620–690 nm will eliminate the effects of scratches, bubbles, etc. | A color change is accessed visually or via a cell phone positioned on the frame (P) with phone camera aligned to the reagent wells (O) to read the results using a colorimetric detection application. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, C.; Lee, Y.; Kulinsky, L. Fabrication of a Malaria-Ab ELISA Bioassay Platform with Utilization of Syringe-Based and 3D Printed Assay Automation. Micromachines 2018, 9, 502. https://doi.org/10.3390/mi9100502
Lim C, Lee Y, Kulinsky L. Fabrication of a Malaria-Ab ELISA Bioassay Platform with Utilization of Syringe-Based and 3D Printed Assay Automation. Micromachines. 2018; 9(10):502. https://doi.org/10.3390/mi9100502
Chicago/Turabian StyleLim, Christopher, Yangchung Lee, and Lawrence Kulinsky. 2018. "Fabrication of a Malaria-Ab ELISA Bioassay Platform with Utilization of Syringe-Based and 3D Printed Assay Automation" Micromachines 9, no. 10: 502. https://doi.org/10.3390/mi9100502





