Fabrication and Evaluation of a Novel Non-Invasive Stretchable and Wearable Respiratory Rate Sensor Based on Silver Nanoparticles Using Inkjet Printing Technology
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials and Equipment
2.1.1. Processing of PDMS Substrates
2.1.2. Inkjet Printing
2.1.3. Design of Conductive Patterns
2.2. Sensor Fabrication
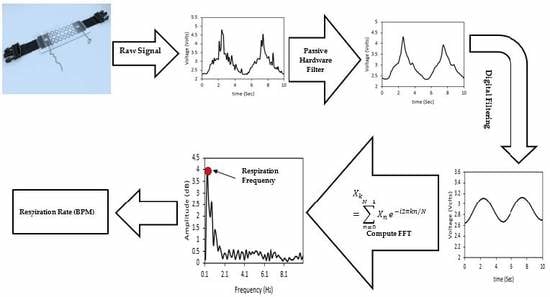
2.3. Electronics Implementation for Respiratory Rate Derivation
2.4. Sensor Validation: Sustainability, Durability, Repeatability, and Reproducibility Tests
2.4.1. Sustainability and Durability Test on the Automated Stretcher
2.4.2. Repeatability and Reproducibility Tests on Respiratory Simulator
2.5. Sensor Evaluation on Healthy Human Subjects
3. Results
3.1. Patterns Comparison: Sustainability and Durability
3.2. Sensor Testing on Respiratory Simulator: Repeatability and Reproducibility
3.3. Sensor Validation on Human Subjects
4. Discussion
4.1. Characteristics of the Developed Sensor: Sustainability, Durability, Repeatability, and Reproducibility
4.2. Accuracy of the IJP PDMS-Based Sensor
4.3. Respiration Waveform Features
4.4. Limitations of the IJP PDMS-Based Sensor
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| # | Gender | Age | Respiratory Rate (BPM) | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | |||||||
| e-Health | Developed | Difference | e-Health | Developed | Difference | |||
| 1 | M | 28 | 19.56 | 19.56 | 0 | 19.56 | 19.56 | 0 |
| 2 | M | 23 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 3 | F | 21 | 11.7 | 11.7 | 0 | 15.6 | 15.6 | 0 |
| 4 | M | 24 | 23.46 | 23.46 | 0 | 23.46 | 23.46 | 0 |
| 5 | M | 24 | 11.7 | 11.7 | 0 | 11.7 | 11.7 | 0 |
| 6 | M | 23 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 7 | M | 19 | 11.7 | 11.7 | 0 | 11.7 | 11.7 | 0 |
| 8 | F | 22 | 15.6 | 15.6 | 0 | 23.46 | 23.46 | 0 |
| 9 | M | 19 | 15.6 | 15.6 | 0 | 19.56 | 19.56 | 0 |
| 10 | M | 25 | 23.46 | 23.46 | 0 | 23.46 | 23.46 | 0 |
| 11 | M | 24 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 12 | M | 24 | 35.16 | 35.16 | 0 | 27.36 | 27.36 | 0 |
| 13 | M | 25 | 27.36 | 27.36 | 0 | 27.36 | 27.36 | 0 |
| 14 | F | 22 | 23.46 | 23.46 | 0 | 23.46 | 23.46 | 0 |
| 15 | M | 25 | 15.6 | 15.6 | 0 | 11.7 | 11.7 | 0 |
| 16 | M | 25 | 23.46 | 23.46 | 0 | 15.6 | 15.6 | 0 |
| 17 | M | 24 | 11.7 | 11.7 | 0 | 11.7 | 11.7 | 0 |
| 18 | M | 24 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 19 | M | 24 | 19.56 | 19.56 | 0 | 11.7 | 11.7 | 0 |
| 20 | M | 25 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 21 | M | 24 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 22 | F | 20 | 11.7 | 11.7 | 0 | 19.56 | 19.56 | 0 |
| 23 | F | 21 | 19.56 | 19.56 | 0 | 11.7 | 11.7 | 0 |
| 24 | F | 19 | 23.46 | 23.46 | 0 | 11.7 | 11.7 | 0 |
| 25 | M | 23 | 15.6 | 15.6 | 0 | 11.7 | 11.7 | 0 |
| 26 | M | 26 | 19.56 | 19.56 | 0 | 19.56 | 19.56 | 0 |
| 27 | M | 22 | 19.56 | 19.56 | 0 | 15.6 | 15.6 | 0 |
| 28 | M | 23 | 23.46 | 23.46 | 0 | 23.46 | 23.46 | 0 |
| 29 | M | 20 | 15.6 | 15.6 | 0 | 15.6 | 15.6 | 0 |
| 30 | M | 19 | 15.6 | 15.6 | 0 | 19.56 | 19.56 | 0 |
| 31 | F | 21 | 19.56 | 19.56 | 0 | 19.56 | 19.56 | 0 |
| 32 | M | 25 | 19.02 | 19.02 | 0 | 13.86 | 13.86 | 0 |
| 33 | M | 28 | 10.98 | 10.98 | 0 | 13.14 | 13.14 | 0 |
| 34 | M | 34 | 13.14 | 13.14 | 0 | 11.31 | 11.31 | 0 |
| 35 | M | 25 | 19.56 | 19.56 | 0 | 15.6 | 15.6 | 0 |
| 36 | M | 23 | 15.6 | 15.6 | 0 | 23.46 | 23.46 | 0 |
| 37 | M | 24 | 35.16 | 35.16 | 0 | 23.46 | 23.46 | 0 |
References
- Saatchi, R.; Burke, D.; Elphick, H.; Tan, S. Respiration Rate Monitoring Methods: A Review. Pediatr. Pulmonol. 2011, 529, 523–529. [Google Scholar]
- Wu, D.; Wang, L.; Zhang, Y.; Huang, B.; Wang, B.; Lin, S.; Xu, X. A wearable respiration monitoring system based on digital respiratory inductive plethysmography. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 4844–4847. [Google Scholar]
- Lee, P.J. Clinical evaluation of a novel respiratory rate monitor. J. Clin. Monit. Comput. 2016, 30, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Talha, S.; Hamdani, A.; Fernando, A. The Application of a Piezo-Resistive Cardiorespiratory Sensor System in an Automobile Safety Belt. Sensors 2015, 15, 7742–7753. [Google Scholar] [Green Version]
- Ciocchetti, M.; Massaroni, C.; Saccomandi, P.; Caponero, M.A.; Polimadei, A.; Formica, D.; Schena, E. Smart Textile Based on Fiber Bragg Grating Sensors for Respiratory Monitoring: Design and Preliminary Trials. Biosensors 2015, 5, 602–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koch, E.; Dietzel, A. Stretchable Sensor Array for Respiratory Monitoring. In Proceedings of the 2017 19th International Conference on Solid-State Sensors, Actuators and Microsystems (TRANSDUCERS), Kaohsiung, Taiwan, 18–22 June 2017; pp. 2227–2230. [Google Scholar]
- Di Fiore, J.M. Neonatal cardiorespiratory monitoring techniques. Semin. Neonatol. 2004, 9, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Ginsburg, A.S.; Lenahan, J.L.; Izadnegahdar, R.; Ansermino, J.M. A Systematic Review of Tools to Measure Respiratory Rate in Order to Identify Childhood Pneumonia. Am. J. Respir. Crit. Care Med. 2018, 197, 1116–1127. [Google Scholar] [CrossRef]
- Piuzzi, E.; Pisa, S.; Member, S.; Pittella, E.; Podestà, L.; Sangiovanni, S. Low-Cost and Portable Impedance Plethysmography System for the Simultaneous Detection of Respiratory and Heart Activities. IEEE Sens. J. 2019, 19, 2735–2746. [Google Scholar] [CrossRef]
- Zhang, Z.; Zheng, J.; Wu, H.; Wang, W.; Wang, B.; Liu, H. Development of a respiratory inductive plethysmography module supporting multiple sensors for wearable systems. Sensors 2012, 12, 13167–13184. [Google Scholar] [CrossRef]
- Hesse, M.; Christ, P.; Hörmann, T.; Rückert, U. A respiration sensor for a chest-strap based wireless body sensor. Proc. IEEE Sens. 2014, 2014, 490–493. [Google Scholar]
- Al-Ghussain, L. Global warming: review on driving forces and mitigation. Environ. Prog. Sustain. Energy 2018, 38, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Darwish Ahmad, A.; Abubaker, A.M.; Salaimeh, A.A.; Akafuah, N.K. Schlieren Visualization of Shaping Air during Operation of an Electrostatic Rotary Bell Sprayer: Impact of Shaping Air on Droplet Atomization and Transport. Coatings 2018, 8, 279. [Google Scholar] [CrossRef]
- Wilson, J.E.; Grib, S.W.; Darwish Ahmad, A.; Renfro, M.W.; Adams, S.A.; Salaimeh, A.A. Study of near-cup droplet breakup of an automotive electrostatic rotary bell (esrb) atomizer using high-speed shadowgraph imaging. Coatings 2018, 8, 174. [Google Scholar] [CrossRef]
- Al-Halhouli, A.; Qitouqa, H.; Alashqar, A.; Abu-Khalaf, J. Inkjet printing for the fabrication of flexible/stretchable wearable electronic devices and sensors. Sens. Rev. 2018, 38, 438–452. [Google Scholar] [CrossRef]
- Abu-khalaf, J.M.; Saraireh, R.; Eisa, S.M.; Al-halhouli, A. Experimental Characterization of Inkjet-Printed Stretchable Circuits for Wearable Sensor Applications. Sensors 2018, 18, 3476. [Google Scholar] [CrossRef] [PubMed]
- Lacour, S.P.; Jones, J.; Suo, Z.; Wagner, S. Design and performance of thin metal film interconnects for skin-like electronic circuits. IEEE Electron Device Lett. 2004, 25, 179–181. [Google Scholar] [CrossRef]
- Brosteaux, D.; Axisa, F.; Gonzalez, M.; Vanfleteren, J. Design and fabrication of elastic interconnections for stretchable electronic circuits. IEEE Electron Device Lett. 2007, 28, 552–554. [Google Scholar] [CrossRef]
- Amjadi, M.; Kyung, K.U.; Park, I.; Sitti, M. Stretchable, Skin-Mountable, and Wearable Strain Sensors and Their Potential Applications: A Review. Adv. Funct. Mater. 2016, 26, 1678–1698. [Google Scholar] [CrossRef]
- Xu, H.; Lu, Y.F.; Xiang, J.X.; Zhang, M.K.; Zhao, Y.J.; Xie, Z.Y.; Gu, Z.Z. A multifunctional wearable sensor based on a graphene/inverse opal cellulose film for simultaneous, in situ monitoring of human motion and sweat. Nanoscale 2018, 10, 2090–2098. [Google Scholar] [CrossRef]
- He, Z.; Zhou, G.; Byun, J.H.; Lee, S.K.; Um, M.K.; Park, B.; Kim, T.; Lee, S.B.; Chou, T.W. Highly stretchable multi-walled carbon nanotube/thermoplastic polyurethane composite fibers for ultrasensitive, wearable strain sensors. Nanoscale 2019, 11, 5884–5890. [Google Scholar] [CrossRef]
- Yao, S.; Zhu, Y. Wearable multifunctional sensors using printed stretchable conductors made of silver nanowires. Nanoscale 2014, 6, 2345–2352. [Google Scholar] [CrossRef]
- Adrega, T.; Lacour, S.P. Stretchable gold conductors embedded in PDMS and patterned by photolithography: Fabrication and electromechanical characterization. J. Micromech. Microeng. 2010, 20, 055025. [Google Scholar] [CrossRef]
- Larmagnac, A.; Eggenberger, S.; Janossy, H.; Vörös, J. Stretchable electronics based on Ag-PDMS composites. Sci. Rep. 2014, 4, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Jung, K.H.; Jung, S.B. Design and fabrication of screen-printed silver circuits for stretchable electronics. Microelectron. Eng. 2014, 120, 216–220. [Google Scholar] [CrossRef]
- Liang, J.; Tong, K.; Pei, Q. A Water-Based Silver-Nanowire Screen-Print Ink for the Fabrication of Stretchable Conductors and Wearable Thin-Film Transistors. Adv. Mater. 2016, 28, 5986–5996. [Google Scholar] [CrossRef] [PubMed]
- Liimatta, T.; Halonen, E.; Sillanpaa, H.; Niittynen, J.; Mantysalo, M. Inkjet printing in manufacturing of stretchable interconnects. In Proceedings of the 2014 IEEE 64th Electronic Components and Technology Conference (ECTC), Lake Buena Vista, FL, USA, 27–30 May 2014; pp. 151–156. [Google Scholar]
- Abu-Khalaf, J.M.; Park, J.W.; Mascaro, D.J.; Mascaro, S.A. Stretchable fingernail sensors for measurement of fingertip force. In Proceedings of the World Haptics 2009-Third Joint EuroHaptics conference and Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems, Salt Lake City, UT, USA, 18–20 March 2009; pp. 625–626. [Google Scholar]
- Jiang, J.; Bao, B.; Li, M.; Sun, J.; Zhang, C.; Li, Y.; Li, F.; Yao, X.; Song, Y. Fabrication of Transparent Multilayer Circuits by Inkjet Printing. Adv. Mater. 2016, 28, 1420–1426. [Google Scholar] [CrossRef]
- Huang, Q.; Al-Milaji, K.N.; Zhao, H. Inkjet Printing of Silver Nanowires for Stretchable Heaters. ACS Appl. Nano Mater. 2018, 1, 4528–4536. [Google Scholar] [CrossRef]
- Chen, B.; Kruse, M.; Xu, B.; Tutika, R.; Zheng, W.; Bartlett, M.D.; Wu, Y.; Claussen, J.C. Flexible thermoelectric generators with inkjet-printed bismuth telluride nanowires and liquid metal contacts. Nanoscale 2019, 11, 5222–5230. [Google Scholar] [CrossRef]
- Chung, H.U.; Kim, B.H.; Lee, J.Y.; Lee, J.; Xie, Z.; Ibler, E.M.; Lee, K.H.; Banks, A.; Jeong, J.Y.; Kim, J.; et al. Binodal, wireless epidermal electronic systems with in-sensor analytics for neonatal intensive care. Science 2019, 363, 780. [Google Scholar] [CrossRef]
- Chu, M.; Nguyen, T.; Pandey, V.; Zhou, Y.; Pham, H.N.; Bar-Yoseph, R.; Radom-Aizik, S.; Jain, R.; Cooper, D.M.; Khine, M. Respiration rate and volume measurements using wearable strain sensors. NPJ Digit. Med. 2019, 2, 8. [Google Scholar] [CrossRef]
- Turnbull, H.; Kasereka, M.C.; Amirav, I.; Sahika, S.E.; Solomon, I.; Aldar, Y.; Hawkes, M.T. Development of a novel device for objective respiratory rate measurement in low-resource settings. BMJ Innov. 2018, 4, 185–191. [Google Scholar] [CrossRef]
- Dickey, M.D. Stretchable and Soft Electronics using Liquid Metals. Adv. Mater. 2017, 29, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.A.; Someya, T.; Huang, Y. Materials and mechanics for stretchable electronics. Science 2010, 327, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Jiang, J.; Bao, B.; Wang, S.; He, M.; Zhang, X.; Song, Y. Fabrication of Bendable Circuits on a Polydimethylsiloxane (PDMS) Surface by Inkjet Printing Semi-Wrapped Structures. Materials 2016, 9, 253. [Google Scholar] [CrossRef] [PubMed]
- Abu-Khalaf, J.; Al-Ghussain, L.; Al-Halhouli, A. Fabrication of Stretchable Circuits on Polydimethylsiloxane (PDMS) Pre-Stretched Substrates by Inkjet Printing Silver Nanoparticles. Materials 2018, 11, 2377. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Ren, X.; Kim, J.W.; Noh, H. Direct inkjet printing of micro-scale silver electrodes on polydimethylsiloxane (PDMS) microchip. J. Micromech. Microeng. 2014, 24, 115010. [Google Scholar] [CrossRef]
- Wu, J.; Wang, R.; Yu, H.; Li, G.; Xu, K.; Tien, N.C.; Roberts, R.C.; Li, D. Inkjet-printed microelectrodes on PDMS as biosensors for functionalized microfluidic systems. Lab Chip 2015, 15, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Driver, M.; Wyman, P.; Best, S.M.; Hassler, M.; De Nardo, L.; Altomare, L.; Del Curto, B.; Cigada, A.; Draghi, L.; Wang, J.H.; et al. Coatings for Biomedical Applications. In Coatings for Biomedical Applications; Driver, M., Ed.; Woodhead Publishing Series in Biomaterials; Woodhead Publishing: Cambridge, UK, 2012; ISBN 978-1-84569-568-2. [Google Scholar]
- Cummins, G.; Desmulliez, M.P.Y.; Cummins, G.; Marc, P.; Desmulliez, Y. Inkjet printing of conductive materials: A review. Circuit World 2013, 38, 193–213. [Google Scholar] [CrossRef]
- Dimatix Materials Printer DMP-2850. 2013. Available online: https://www.fujifilmusa.com/products/industrial_inkjet_printheads/deposition-products/dmp-2800/ (accessed on 22 April 2016).
- Paredes-Madrid, L.; Matute, A.; Bareño, J.O.; Vargas, C.A.P.; Velásquez, E.I.G. Underlying physics of conductive polymer composites and Force Sensing Resistors (FSRs). A study on creep response and dynamic loading. Materials 2017, 10, 1334. [Google Scholar] [CrossRef]
- Rajan, K.; Roppolo, I.; Chiappone, A.; Bocchini, S.; Perrone, D.; Chiolerio, A. Nanotechnology, Science and Applications Dovepress Silver nanoparticle ink technology: State of the art. Nanotechnol. Sci. Appl. 2016, 9, 1–13. [Google Scholar]
- Biabangard Oskouyi, A.; Sundararaj, U.; Mertiny, P. Current-voltage characteristics of nano-platelet based conductive nano-composites. ICCM Int. Conf. Compos. Mater. 2013, 2013, 9264–9269. [Google Scholar]
- Radial Stretching System|Scientific Open Source/Hardware Test Equipment. Available online: http://www.somap.jku.at/rss/ (accessed on 27 February 2018).
- Reuter, S.; Moser, C.; Baack, M. Respiratory Distress in the Newborn. Pediatr. Rev. 2014, 35, 417–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Doershuk, C.F.; Matthews, L.R.W. Airway resistance and lung volume in the newborn infant. Pediatr. Res. 1969, 3, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Shehzad, K. Neonatal birth-weights and reference intervals in sonographically monitored normal fetuses. Int. J. Health Sci. 2011, 5, 27. [Google Scholar]
- Needham, C.D.; Rogan, M.C.; Mcdonald, I. Normal Standards for Lung Volumes, Intrapul-Monary Gas-Mixing, and Maximum Breathing Capacity. Thorax 1954, 9, 313. [Google Scholar] [CrossRef] [PubMed]
- Yuan, G.; Drost, N.; McIvor, A. Respiratory Rate and Breathing Pattern. McMaster Univ. Med. J. 2013, 10, 23–25. [Google Scholar]
- Voscopoulos, C.; Brayanov, J.; Ladd, D.; Lalli, M.; Panasyuk, A.; Freeman, J. Evaluation of a Novel Noninvasive Respiration Monitor Providing Continuous Measurement of Minute Ventilation in Ambulatory Subjects in a Variety of Clinical Scenarios. Anesth. Analg. 2013, 117, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Bayo-Monton, J.L.; Martinez-Millana, A.; Han, W.; Fernandez-Llatas, C.; Sun, Y.; Traver, V. Wearable Sensors Integrated with Internet of Things for Advancing eHealth Care. Sensors 2018, 18, 1851. [Google Scholar] [CrossRef]
- Rákay, R.; Višňovský, M.; Galajdová, A.; Šimšík, D. Testing Properties of E-health System Based on Arduino. J. Autom. Control 2015, 3, 122–126. [Google Scholar]
- Hacks, C. e-Health Sensor Platform V2.0 for Arduino and Raspberry Pi [Biometric/Medical Applications]. Available online: https://www.cooking-hacks.com/documentation/tutorials/ehealth-biometric-sensor-platform-arduino-raspberry-pi-medical (accessed on 20 February 2019).
- Liu, H.; Guo, S.; Zheng, K.; Guo, X.; Kuramoto-Ahuja, T.; Sato, T.; Onoda, K.; Maruyama, H. Reliability and validity of measuring respiration movement using a wearable strain sensor in healthy subjects. J. Phys. Ther. Sci. 2017, 29, 1543–1547. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, J.; Li, Y.; Rehg, J.M.; Picard, R.W. BioGlass: Physiological parameter estimation using a head-mounted wearable device. In Proceedings of the 2014 4th International Conference on Wireless Mobile Communication and Healthcare-Transforming Healthcare Through Innovations in Mobile and Wireless Technologies (MOBIHEALTH), Athens, Greece, 3–5 November 2014. [Google Scholar]
- Van Loon, K.; Breteler, M.J.M.; van Wolfwinkel, L.; Rheineck Leyssius, A.T.; Kossen, S.; Kalkman, C.J.; van Zaane, B.; Peelen, L.M. Wireless non-invasive continuous respiratory monitoring with FMCW radar: A clinical validation study. J. Clin. Monit. Comput. 2016, 30, 797–805. [Google Scholar] [CrossRef]
- Guechi, Y.; Pichot, A.; Frasca, D.; Rayeh-Pelardy, F.; Lardeur, J.-Y.; Mimoz, O. Assessment of noninvasive acoustic respiration rate monitoring in patients admitted to an Emergency Department for drug or alcoholic poisoning. J. Clin. Monit. Comput. 2015, 29, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.-L.; Huang, T.-H.; Hsu, P.-C.; Ko, Y.-C.; Chen, F.-L.; Wang, W.-C.; Kao, T.; Chan, C.-T. Respiratory Rate Estimation by Using ECG, Impedance, and Motion Sensing in Smart Clothing. J. Med. Biol. Eng. 2017, 37, 826–842. [Google Scholar] [CrossRef] [PubMed]
- Breteler, M.J.M.; Huizinga, E.; van Loon, K.; Leenen, L.P.H.; Dohmen, D.A.J.; Kalkman, C.J.; Blokhuis, T.J. Reliability of wireless monitoring using a wearable patch sensor in high-risk surgical patients at a step-down unit in the Netherlands: A clinical validation study. BMJ Open 2018, 8, e020162. [Google Scholar] [CrossRef] [PubMed]














| Group | Average Lung Volume (mL) | Tidal Volume (mL) | Normal Respiration Rate (BPM) | Average Volume Strain (%) |
|---|---|---|---|---|
| Neonates | 75.4–110.2 | 15.6–38 | 30–60 | 14.2–50.4 |
| Adults | 4000–6000 | 500 | 12–20 | 8.3–12.5 |
| Volume (mL) | Mode | Volume Strain (%) | Speed (mm/s) | RR (BPM) | Volume Flow Rate (mL/s) | |||
|---|---|---|---|---|---|---|---|---|
| 200 PWM | 150 PWM | 200 PWM | 150 PWM | 200 PWM | 150 PWM | |||
| 43.3 | 1 | 17.3 | 101.5 | 52.2 | 154.2 | 58.2 | 219.7 | 113.0 |
| 100.6 | 2 | 40.3 | 101.5 | 52.2 | 70.2 | 31.8 | 219.7 | 113.0 |
| 149.4 | 3 | 59.7 | 101.5 | 52.2 | 51 | 23.46 | 219.7 | 113.0 |
| Design # | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Resistance (Ohm) | 18–30 | 10–15 | 15–26 | 8–15 | 19–25 | 30–42 |
| Volume Strain (%) | Actual RR (BPM) | Measured RR (BPM) | Difference (BPM) |
|---|---|---|---|
| 17.3 | 58.2 | 58.2 | 0 |
| 154.2 | 152.34 | 1.86 | |
| 40.3 | 31.8 | 31.2 | 0.6 |
| 70.2 | 70.2 | 0 | |
| 59.7 | 23.46 | 23.4 | 0.06 |
| 51 | 50.76 | 0.24 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Halhouli, A.; Al-Ghussain, L.; El Bouri, S.; Liu, H.; Zheng, D. Fabrication and Evaluation of a Novel Non-Invasive Stretchable and Wearable Respiratory Rate Sensor Based on Silver Nanoparticles Using Inkjet Printing Technology. Polymers 2019, 11, 1518. https://doi.org/10.3390/polym11091518
Al-Halhouli A, Al-Ghussain L, El Bouri S, Liu H, Zheng D. Fabrication and Evaluation of a Novel Non-Invasive Stretchable and Wearable Respiratory Rate Sensor Based on Silver Nanoparticles Using Inkjet Printing Technology. Polymers. 2019; 11(9):1518. https://doi.org/10.3390/polym11091518
Chicago/Turabian StyleAl-Halhouli, Ala’aldeen, Loiy Al-Ghussain, Saleem El Bouri, Haipeng Liu, and Dingchang Zheng. 2019. "Fabrication and Evaluation of a Novel Non-Invasive Stretchable and Wearable Respiratory Rate Sensor Based on Silver Nanoparticles Using Inkjet Printing Technology" Polymers 11, no. 9: 1518. https://doi.org/10.3390/polym11091518