Present Status in Polymeric Mouthguards. A Future Area for Additive Manufacturing?
Abstract
:1. Introduction
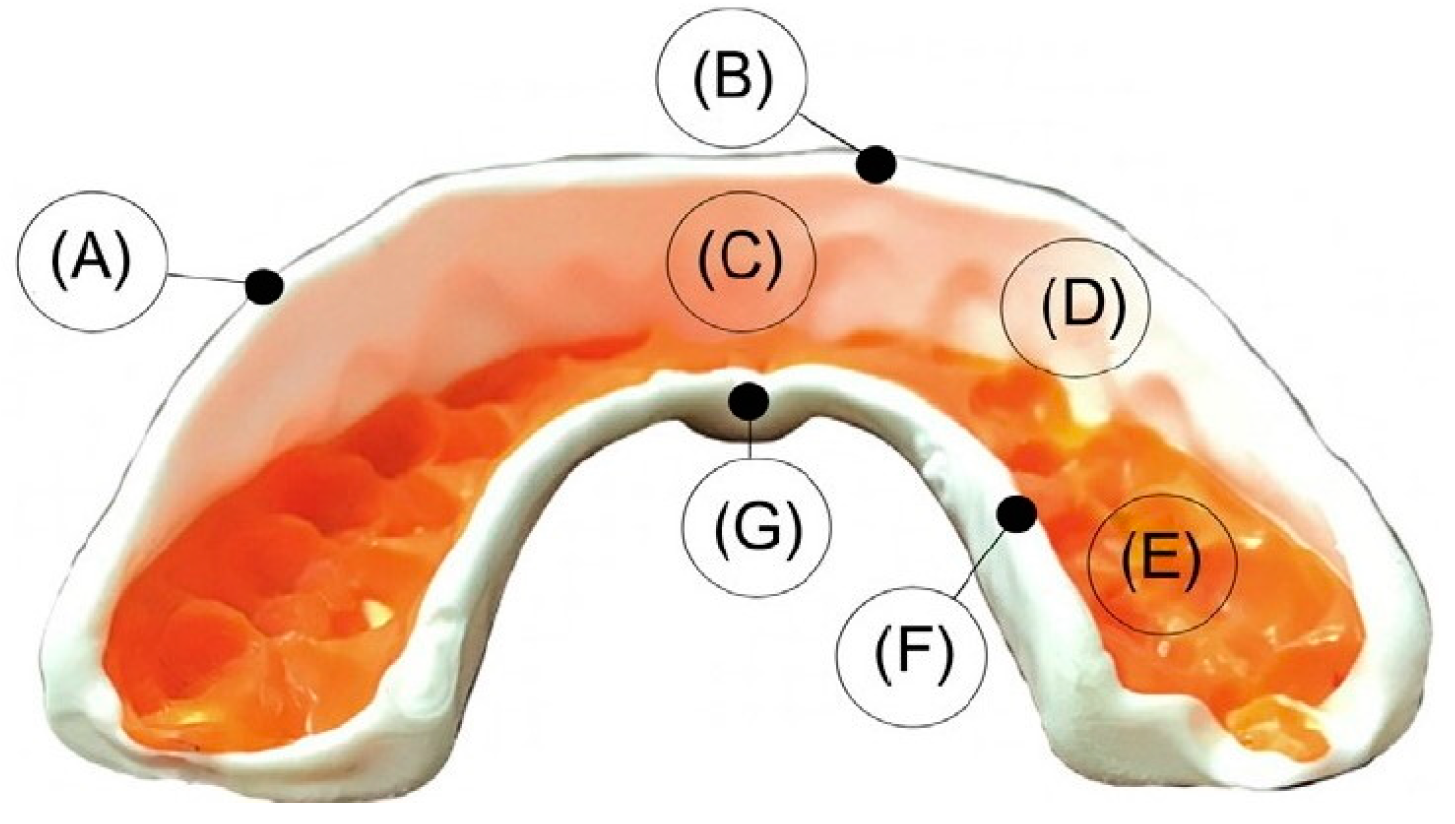
2. Properties and Design of Mouthguards
3. Types of Mouthguards
3.1. Stock Mouthguard
3.2. Mouth-Formed Mouthguard
3.3. Custom-Made Mouthguard
4. Mouthguard Base Material
4.1. Ethylene Vinyl Acetate (EVA) Copolymer
4.2. Polyolefins
4.3. Other Materials
5. Fabrication Techniques of Custom-Made Mouthguards
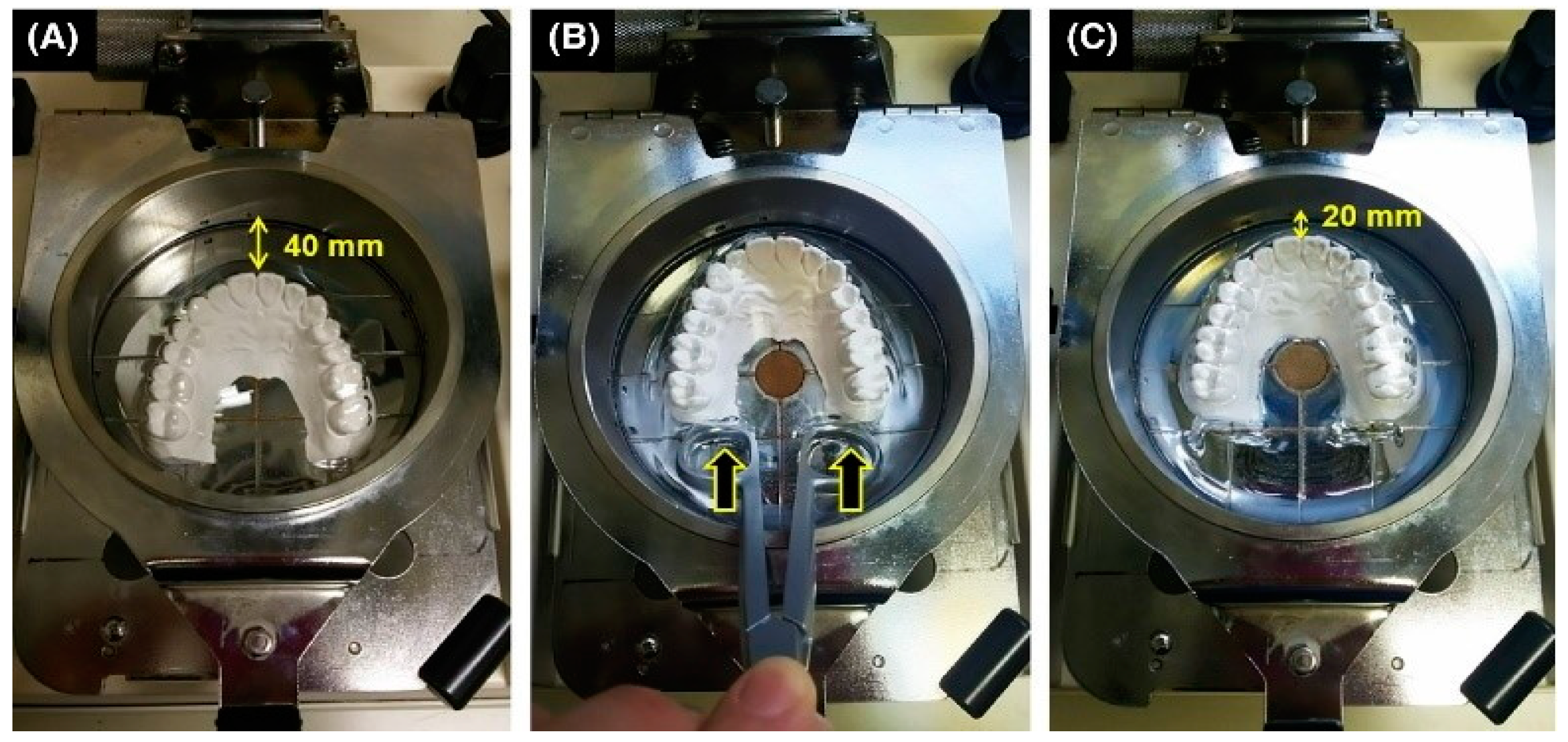
5.1. Pressure-Forming Technique
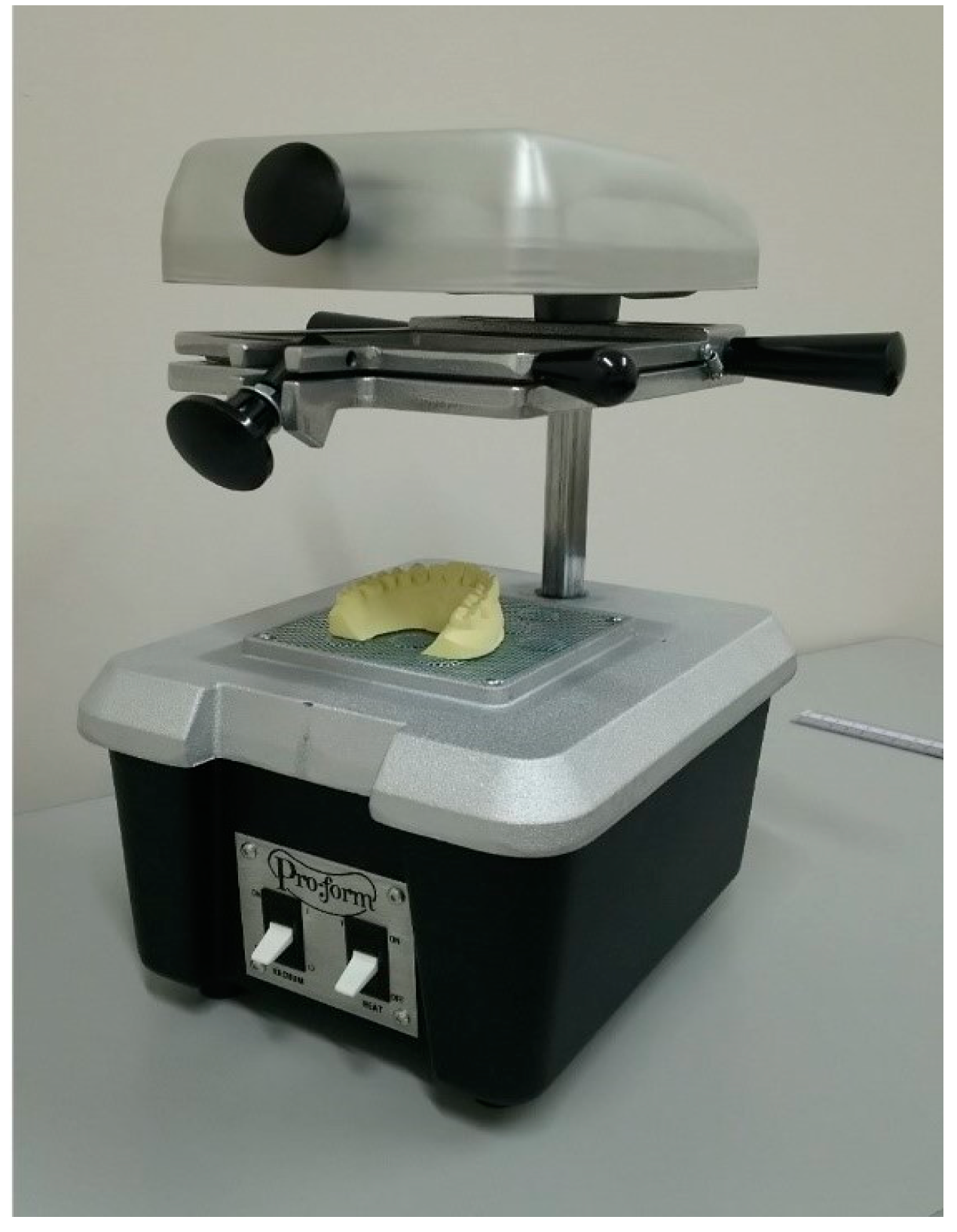
5.2. Vacuum Forming Technique
5.3. 3D Printing
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Emerich, K.; Kaczmarek, J. First Aid for Dental Trauma Caused by Sports Activities. Sports Med. 2010, 40, 361–366. [Google Scholar] [CrossRef]
- Ranalli, D.N.; Demas, P.N. Orofacial Injuries from Sport. Sports Med. 2002, 32, 409–418. [Google Scholar] [CrossRef]
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaBella, C.; Smith, B.; Sigurdsson, A. Effect of mouthguards on dental injuries and concussions in college basketball. Med. Sci. Sports Exerc. 2002, 34, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; Borges, A.L.S.; Bottino, M.A. Influence of custom-made and stock mouthguard thickness on biomechanical response to a simulated impact. Dent. Traumatol. 2018, 34, 429–437. [Google Scholar] [CrossRef] [PubMed]
- Jegier, M.; Smalc, A.; Jegier, A. Selected dental concerns in sports medicine. Med. Sport. 2005, 9, 53–59. [Google Scholar]
- Andrade, R.A.; Evans, P.L.S.; Almeida, A.L.S.; da Silva, J.D.J.R.; Guedes, A.M.L.; Guedes, F.R.; Ranalli, D.N.; Modesto, A.; Tinoco, E.M.B. Prevalence of dental trauma in Pan American Games athletes. Dent. Traumatol. 2010, 26, 248–253. [Google Scholar] [CrossRef]
- Ferrari, C.H.; Ferreira De Medeiros, J.M. Dental trauma and level of information: Mouthguard use in different contact sports. Dent. Traumatol. 2002, 18, 144–147. [Google Scholar] [CrossRef]
- ADA Council. Using mouthguards to reduce the incidence and severity of sports-related oral injuries. J. Am. Dent. Assoc. 2006, 137, 1712–1720. [Google Scholar] [CrossRef]
- Zaman, I.; Rozlan, S.A.M.; Manshoor, B.; Ngali, M.Z.; Khalid, A.; Amin, N.A.M. Study of Mouthguard Design for Endurance and Air-Flow Intake. IOP Conf. Ser. Mater. Sci. Eng. 2017, 226, 012007. [Google Scholar] [CrossRef] [Green Version]
- Knapik, J.J.; Marshall, S.W.; Lee, R.B.; Darakjy, S.S.; Jones, S.B.; Mitchener, T.A.; DelaCruz, G.G.; Jones, B.H. Mouthguards in sport: Activities history, physical properties and injury prevention effectiveness. Sports Med. 2007, 37, 117–144. [Google Scholar] [CrossRef]
- Knapik, J.J.; Hoedebecke, B.L.; Rogers, G.G.; Sharp, M.A.; Marshall, S.W. Effectiveness of Mouthguards for the Prevention of Orofacial Injuries and Concussions in Sports: Systematic Review and Meta-Analysis. Sports Med. 2019, 49, 1217–1232. [Google Scholar] [CrossRef]
- ASTM International ASTM F697-16. Standard Practice for Care and Use of Athletic Mouth Protectors; ASTM International: West Conshohocken, PA, USA, 2016. [Google Scholar]
- Gould, T.E.; Piland, S.G.; Shin, J.; Hoyle, C.E.; Nazarenko, S. Characterization of mouthguard materials: Physical and mechanical properties of commercialized products. Dent. Mater. 2009, 25, 771–780. [Google Scholar] [CrossRef]
- Bergman, L.; Milardović Ortolan, S.; Žarković, D.; Viskić, J.; Jokić, D.; Mehulić, K. Prevalence of dental trauma and use of mouthguards in professional handball players. Dent. Traumatol. 2017, 33, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Mekayarajjananonth, T.; Winkler, S.; Wongthai, P. Improved mouth guard design for protection and comfort. J. Prosthet. Dent. 1999, 82, 627–630. [Google Scholar] [CrossRef]
- Maeda, M.; Takeda, T.; Nakajima, K.; Shibusawa, M.; Kurokawa, K.; Shimada, A.; Takayama, K.; Ishigami, K. In Search of Necessary Mouthguard Thickness. Part 1: From the Viewpoint of Shock Absorption Ability. J. Jpn. Prosthodont. Soc. 2008, 52, 211–219. [Google Scholar] [CrossRef] [Green Version]
- Verissimo, C.; Costa, P.V.M.; Santos-Filho, P.C.F.; Tantbirojn, D.; Versluis, A.; Soares, C.J. Custom-Fitted EVA Mouthguards: What is the ideal thickness? a dynamic finite element impact study. Dent. Traumatol. 2016, 32, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Lunt, D.R.; Mendel, D.A.; Brantley, W.A.; Michael Beck, F.; Huja, S.; Schriever, S.D.; Grentzer, T.H.; Alapati, S.B. Impact energy absorption of three mouthguard materials in three environments. Dent. Traumatol. 2010, 26, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Karaganeva, R.; Pinner, S.; Tomlinson, D.; Burden, A.; Taylor, R.; Yates, J.; Winwood, K. Effect of mouthguard design on retention and potential issues arising with usability in sport. Dent. Traumatol. 2019, 35, 73–79. [Google Scholar] [CrossRef]
- Maeda, Y.; Kumamoto, D.; Yagi, K.; Ikebe, K. Effectiveness and fabrication of mouthguards. Dent. Traumatol. 2009, 25, 556–564. [Google Scholar] [CrossRef]
- Yamada, J.; Maeda, Y.; Satoh, H.; Miura, J. Anterior palatal mouthguard margin location and its effect on shock-absorbing capability. Dent. Traumatol. 2006, 22, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Liebgott, B. The Anatomical Basis of Dentistry, 4th ed.; Elsevier: St. Louis, MI, USA, 2017; pp. 1–465. [Google Scholar]
- Nallaswamy, D. Textbook of Prosthodontics, 2nd ed.; Jaypee Brothers Medical Publishers: New Delhi, India, 2017; pp. 1–1390. [Google Scholar]
- Mosby’s Dictionary of Medicine, Nursing & Health Professions, 10th ed.; Elsevier: St. Louis, MI, USA, 2016; ISBN 9780323414210.
- Morcos, S.; Patel, P. The Vocabulary of Dentofacial Deformities. Clin. Plast. Surg. 2007, 34, 589–599. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.F.; Wahab, M.S.; Rahim, E. Rapid fabrication of functional mouthguard using rapid tooling approach. ARPN J. Eng. Appl. Sci. 2016, 11, 7645–7649. [Google Scholar]
- Parker, K.; Marlow, B.; Patel, N.; Gill, D.S. A review of mouthguards: Effectiveness, types, characteristics and indications for use. Br. Dent. J. 2017, 222, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Rickne, C.; Scheid, G.W. Woelfel’s Dental Anatomy, 8th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012; ISBN 1608317463. [Google Scholar]
- Geary, J.L.; Kinirons, M.J. Post thermoforming dimensional changes of ethylene vinyl acetate used in custom-made mouthguards for trauma prevention–a pilot study. Dent. Traumatol. 2008, 24, 350–355. [Google Scholar] [CrossRef] [PubMed]
- Al-Qahtani, M.; Alrefaie, M.; Altamimi, A.; Aljowyed, I.; Qahtani, M.; AlQahtani, A.; Habib, S. Evaluation of Pre-Alginate Impression Preparation Methods in the Surface Accuracy of Dental Cast. Saudi Dent. J. 2019, 31, 451–456. [Google Scholar] [CrossRef]
- Westerman, B.; Stringfellow, P.; Eccleston, J. EVA mouthguards: How thick should they be? Dent. Traumatol. 2002, 18, 24–27. [Google Scholar] [CrossRef]
- Takeda, T.; Ishigami, K.; Ogawa, T.; Nakajima, K.; Shibusawa, M.; Shimada, A.; Regner, C.W. Are all mouthguards the same and safe to use? The influence of occlusal supporting mouthguards in decreasing bone distortion and fractures. Dent. Traumatol. 2004, 20, 150–156. [Google Scholar] [CrossRef]
- Hoffmann, J.; Alfter, G.; Rudolph, N.K.; GÖZ, G. Experimental comparative study of various mouthguards. Dent. Traumatol. 1999, 15, 157–163. [Google Scholar] [CrossRef] [Green Version]
- Mizuhashi, F.; Koide, K. Formation of vacuum-formed and pressure-formed mouthguards. Dent. Traumatol. 2017, 33, 295–299. [Google Scholar] [CrossRef]
- Patrick, D.G.; van Noort, R.; Found, M.S. Scale of protection and the various types of sports mouthguard. Braz. J. Sports Med. 2005, 39, 278–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guérard, S.; Barou, J.-L.; Petit, J.; Poisson, P. Characterization of mouthguards: Impact performance. Dent. Traumatol. 2017, 33, 281–287. [Google Scholar] [CrossRef] [Green Version]
- Gould, T.E.; Jesunathadas, M.; Nazarenko, S.; Piland, S.G. Mouth Protection in Sports. In Materials in Sports Equipment, 2nd ed.; Woodhead Publishing Series in Composites Science and Engineering; Subic, A., Ed.; Woodhead Publishing: Cambridge, UK, 2019; pp. 199–231. ISBN 978-0-08-102582-6. [Google Scholar]
- Tiwari, U.; Mishra, V.; Bhalla, A.; Singh, N.; Jain, S.; Garg, H.; Suryanarain, R.; Grewal, N.; Kapur, P. A Fiber Bragg Grating Sensor for measurement of impact absorption capabilities of mouthguards. Dent. Traumatol. 2011, 27, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Tuna, E.B.; Ozel, E. Factors Affecting Sports-Related Orofacial Injuries and the Importance of Mouthguards. Sports Med. 2014, 44, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Uzel, I.; Aykut-Yetkiner, A.; Ersin, N.; Ertugrul, F.; Oncag, O.; Attin, R. Dental Trauma and Mouthguard Usage among Soccer Players in Izmir. Turk. Dent. J. 2014, 2, 78–84. [Google Scholar] [CrossRef] [Green Version]
- Takeda, T.; Ishigami, K.; Shintaro, K.; Nakajima, K.; Shimada, A.; Regner, C. The influence of impact object characteristics on impact force and force absorption by mouthguard material. Dent. Traumatol. 2004, 20, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Queiróz, A.F.V.R.; de Brito, R.B., Jr.; Ramacciato, J.C.; Motta, R.H.L.; Flório, F.M. Influence of mouthguards on the physical performance of soccer players. Dent. Traumatol. 2013, 29, 450–454. [Google Scholar] [CrossRef]
- Gawlak, D.; Mierzwińska-Nastalska, E.; Mańka-Malara, K.; Kamiński, T. Comparison of usability properties of custom-made and standard self-adapted mouthguards. Dent. Traumatol. 2014, 30, 306–311. [Google Scholar] [CrossRef]
- Mills, S.; Canal, E. Prevention of Athletic Dental Injuries: The Mouthguard. In Modern Sports Dentistry. Textbooks in Contemporary Dentistry; Roettger, M., Ed.; Springer: Cham, Switzerland, 2018; pp. 111–133. ISBN 978-3-319-44414-7. [Google Scholar]
- Del Rossi, G.; Leyte-Vidal, M.A. Fabricating a better mouthguard. Part I: Factors influencing mouthguard thinning. Dent. Traumatol. 2007, 23, 149–154. [Google Scholar] [CrossRef]
- Dhillon, B.; Sood, N.; Sood, N.; Sah, N.; Arora, D.; Mahendra, A. Guarding the Precious Smile: Incidence and Prevention of Injury in Sports: A Review. J. Int. Oral Health. 2014, 6, 104–107. [Google Scholar]
- Duddy, F.A.; Weissman, J.; Lee, R.A.; Paranjpe, A.; Johnson, J.D.; Cohenca, N. Influence of different types of mouthguards on strength and performance of collegiate athletes: A controlled-randomized trial. Dent. Traumatol. 2012, 28, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Zamora Olave, C.; Willaert, E.; Montero-Blesa, A.; Riera-Puñet, N.; Martínez-Gomis, J. Risk of orofacial injuries and mouthguard use in water polo players. Dent. Traumatol. 2018, 34, 406–412. [Google Scholar] [CrossRef]
- Park, J.B.; Shaull, K.L.; Overton, B.; Donly, K.J. Improving mouth guards. J. Prosthet. Dent. 1994, 72, 373–380. [Google Scholar] [CrossRef]
- McNair, O.D.; Gould, T.E.; Piland, S.G.; Savin, D.A. Characterization of mouthguard materials: A comparison of a commercial material to a novel thiolene family. J. Appl. Polym. Sci. 2014, 131, 40402. [Google Scholar] [CrossRef]
- Moreira, A.; Mendes, J.; Fonte, E.; Ferreira, D.; Pais Clemente, M.; Vasconcelos, M. Implementation of a custom-made mouthguard in a professional basketball team. J. Mech. Eng. Biomech. 2019, 3, 25–32. [Google Scholar] [CrossRef] [Green Version]
- Miura, J.; Maeda, Y.; Machi, H.; Matsuda, S. Mouthguards: Difference in longitudinal dimensional stability between single- and double-laminated fabrication techniques. Dent. Traumatol. 2007, 23, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Bando, Y. Thermoforming method to effectively maintain mouthguard thickness: Effect of moving the model position just before vacuum formation. Dent. Traumatol. 2019, 35, 121–127. [Google Scholar] [CrossRef]
- Yamada, J.; Maeda, Y. Thermoforming Process for Fabricating Oral Appliances: Influence of Heating and Pressure Application Timing on Formability. J. Prosthodont. 2007, 16, 452–456. [Google Scholar] [CrossRef]
- Mihindukulasuriya, S.; Lim, L.-T. Effects of Liquid Contaminants on Heat Seal Strength of low-density polyethylene Film. Packag. Technol. Sci. 2012, 25, 271–284. [Google Scholar] [CrossRef]
- Tanabe, G.; Churei, H.; Wada, T.; Takahashi, H.; Uo, M.; Ueno, T. The influence of temperature on sheet lamination process when fabricating mouthguard on dental thermoforming machine. J. Oral Sci. 2020, 62, 23–27. [Google Scholar] [CrossRef] [Green Version]
- Chaconas, S.J.; Caputo, A.A.; Bakke, N.K. A comparison of athletic mouthguard materials. Am. J. Sports Med. 1985, 13, 193–197. [Google Scholar] [CrossRef]
- Gawlak, D.; Mańka-Malara, K.; Kamiński, T.; Łuniewska, M.; Mierzwińska-Nastalska, E. Comparative evaluation of custom and standard boil and bite (self-adapted) mouthguards and their effect on the functioning of the oral cavity. Dent. Traumatol. 2016, 32, 416–420. [Google Scholar] [CrossRef]
- Cetin, C.; Keçeci, A.D.; Erdòan, A.; Baydar, M.L. Influence of custom-made mouth guards on strength, speed and anaerobic performance of taekwondo athletes. Dent. Traumatol. 2009, 25, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Zamora-Olave, C.; Willaert, E.; Parera, L.; Riera-Puñet, N.; Martinez-Gomis, J. Experience with mouthguards and prevalence of orofacial injuries among field hockey players in Catalonia. Dent. Traumatol. 2019, 36, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Bando, Y. Thermoforming technique for suppressing reduction in mouthguard thickness: Part 2 Effect of model height and model moving distance. Dent. Traumatol. 2020. (accepted). [Google Scholar] [CrossRef] [PubMed]
- Carvalho, D.; Sousa, T.; Morais, P.V.; Piedade, A.P. Polymer/metal nanocomposite coating with antimicrobial activity against hospital isolated pathogen. Appl. Surf. Sci. 2016, 379, 489–496. [Google Scholar] [CrossRef]
- Piedade, A.P.; Gil, M.H.; Cavaco, M.C.; Andrade, M.E. Behaviour of catalase immobilised on poly(acrylonitrile)-g.co-hydroxyethyl methacrylate when used in a continuous system. Polym. Int. 1995, 38, 269–275. [Google Scholar] [CrossRef]
- Brett, A.M.C.F.O.; Gil, M.H.; Piedade, A.P. An electrochemical bienzyme membrane sensor for free cholesterol. Bioelectrochem. Bioenerg. 1992, 28, 105–115. [Google Scholar] [CrossRef]
- Suzuki, H.; Harashima, T.; Asano, T.; Komiyama, O.; Kuroki, T.; Kusaka, K.; Kawara, M. Use of Polyolefin as Mouthguard Material as Compared to Ethylene Vinyl Acetate. Int. J. Oral Med. Sci. 2007, 6, 14–18. [Google Scholar] [CrossRef] [Green Version]
- Carvalho, V.; Soares, P.; Verissimo, C.; Pessoa, R.; Versluis, A.; Soares, C. Mouthguard Biomechanics for Protecting Dental Implants from Impact: Experimental and Finite Element Impact Analysis. Int. J. Oral Maxillofac. Implants. 2018, 33, 335–343. [Google Scholar] [CrossRef] [Green Version]
- Westerman, B.; Stringfellow, P.M.; Eccleston, J.A. Beneficial effects of air inclusions on the performance of ethylene vinyl acetate (EVA) mouthguard material. Braz. J. Sports Med. 2002, 36, 51–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Go, S.-H.; Kim, H.-G.; Shin, H.-J.; Lee, M.-S.; Yoon, H.-G.; Kwac, L. The impact fracture behaviors of CFRP/EVA composites by drop-weight impact test. Carbon Lett. 2017, 21, 23–32. [Google Scholar] [CrossRef] [Green Version]
- Emblem, A. Plastics properties for packaging materials. In Packaging Technology; Emblem, A., Emblem, H., Eds.; Woodhead Publishing: Cambridge, UK, 2012; pp. 287–309. ISBN 978-1-84569-665-8. [Google Scholar]
- Zarrouki, A.; Espinosa, E.; Boisson, C.; Monteil, V. Free Radical Copolymerization of Ethylene with Vinyl Acetate under Mild Conditions. Macromolecules 2017, 50, 3516–3523. [Google Scholar] [CrossRef]
- Akl, M.; Abd Elrazek, H.M.; Abdel Bary, E.M. Poly (Ethylene-Co-Vinyl Acetate) Blends for Controlled Drug Release. Am. J. Adv. Drug Deliv. 2018, 6, 52–60. [Google Scholar] [CrossRef]
- Arsac, A.; Carrot, C.; Guillet, J. Determination of Primary Relaxation Temperatures and Melting Points of Ethylene Vinyl Acetate Copolymers. J. Therm. Anal. Calorim. 2000, 61, 681–685. [Google Scholar] [CrossRef]
- Meng, F.H.; Schricker, S.R.; Brantley, W.A.; Mendel, D.A.; Rashid, R.G.; Fields, H.W.; Vig, K.W.L.; Alapati, S.B. Differential scanning calorimetry (DSC) and temperature-modulated DSC study of three mouthguard materials. Dent. Mater. 2007, 23, 1492–1499. [Google Scholar] [CrossRef]
- Rossi, G.; Lisman, P.; Signorile, J. Fabricating a better mouthguard. Part II: The effect of color on adaptation and fit. Dent. Traumatol. 2008, 24, 197–200. [Google Scholar] [CrossRef]
- Niemczyk, A.; Moszyński, D.; Jędrzejewski, R.; Kwiatkowski, K.; Piwowarczyk, J.; Baranowska, J. Chemical Structure of EVA Films Obtained by Pulsed Electron Beam and Pulse Laser Ablation. Polymers 2019, 11, 1419. [Google Scholar] [CrossRef] [Green Version]
- Go, S.-H.; Lee, M.-S.; Hong, C.-G.; Kwac, L.-K.; Kim, H.-G. Correlation between Drop Impact Energy and Residual Compressive Strength According to the Lamination of CFRP with EVA Sheets. Polymers 2020, 12, 224. [Google Scholar] [CrossRef] [Green Version]
- Coto, N.P.; Dias, R.B.E.; Costa, R.A.; Antoniazzi, T.F.; de Carvalho, E.P.C. Mechanical behavior of Ethylene Vinyl Acetate copolymer (EVA) used for fabrication of mouthguards and interocclusal splints. Braz. Dent. J. 2007, 18, 324–328. [Google Scholar] [CrossRef] [Green Version]
- Bochnig, M.S.; Oh, M.-J.; Nagel, T.; Ziegler, F.; Jost-Brinkmann, P.-G. Comparison of the shock absorption capacities of different mouthguards. Dent. Traumatol. 2017, 33, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Westerman, B.; Stringfellow, P.M.; Eccleston, J.A. An improved mouthguard material. Aust. Dent. J. 1997, 42, 189–191. [Google Scholar] [CrossRef] [PubMed]
- Westerman, B.; Stringfellow, P.; Eccleston, J. The effect on energy absorption of hard inserts in laminated EVA mouthguard. Aust. Dent. J. 2000, 45, 21–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeda, T.; Ishigami, K.; Handa, J.; Naitoh, K.; Kurokawa, K.; Shibusawa, M.; Nakajima, K.; Kawamura, S. Does hard insertion and space improve shock absorption ability of mouthguard? Dent. Traumatol. 2006, 22, 77–82. [Google Scholar] [CrossRef]
- Fukasawa, S.; Churei, H.; Chowdhury, R.; Shirako, T.; Shahrin, S.; Shrestha, A.; Wada, T.; Uo, M.; Takahashi, H.; Ueno, T. Difference among shock-absorbing capabilities of mouthguard materials. Dent. Traumatol. 2016, 32, 474–479. [Google Scholar] [CrossRef]
- Cummins, N.; Spears, I. The effect of mouthguard design on stresses in the tooth-bone complex. Med. Sci. Sports Exerc. 2002, 34, 942–947. [Google Scholar] [CrossRef]
- Sadeghbeigi, R. FCC Feed Characterization, 3rd ed.; Butterworth-Heinemann: Oxford, UK, 2012; pp. 51–86. ISBN 978-0-12-386965-4. [Google Scholar]
- Fahim, M.A.; Alsahhaf, T.A.; Elkilani, A. Refinery Feedstocks and Products; Fahim, M.A., Alsahhaf, T.A., Elkilani, A.B.T.-F.P.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2010; pp. 11–31. ISBN 978-0-444-52785-1. [Google Scholar]
- Posch, W. Polyolefins. In Plastics Design Library; Kutz, M.B.T.-A.P.E.H., Ed.; William Andrew Publishing: Oxford, UK, 2011; pp. 23–48. ISBN 978-1-4377-3514-7. [Google Scholar]
- Agwuncha, S.C.; Ibrahim, I.D.; Sadiku, E.R. 14-Improving the thermal and flame resistance properties of polyolefins. In The Textile Institute Book Series; Ugbolue, S.C.O.B.T.-P.F., Ed.; Woodhead Publishing: Cambridge, UK, 2017; pp. 421–448. ISBN 978-0-08-101132-4. [Google Scholar]
- Wang, X.; Hu, S.; Guo, Y.; Li, G.; Xu, R. Toughened High-Flow Polypropylene with Polyolefin-Based Elastomers. Polymers 2019, 11, 1976. [Google Scholar] [CrossRef] [Green Version]
- Seymour, R.B.; Carraher, C.E. Properties of Polyolefins BT - Structure—Property Relationships in Polymers; Seymour, R.B., Carraher, C.E., Eds.; Springer US: Boston, MA, USA, 1984; pp. 133–145. ISBN 978-1-4684-4748-4. [Google Scholar]
- Lohse, D.J. Polyolefins. In Applied Polymer Science: 21st Century; Craver, C.D., Carraher, C.E.B.T.-A.P.S., Eds.; Pergamon: Oxford, UK, 2000; pp. 73–91. ISBN 978-0-08-043417-9. [Google Scholar]
- Ihara, C.; Takahashi, H.; Matsui, R.; Yamanaka, T.; Ueno, T. Bonding durability of custom-made mouthpiece for scuba diving after water storage under pressure. Dent. Mater. J. 2009, 28, 487–492. [Google Scholar] [CrossRef] [Green Version]
- Chowdhury, R.; Churei, H.; Takahashi, H.; Wada, T.; Uo, M.; Fukasawa, S.; Abe, K.; Shahrin, S.; Ueno, T. Combined analysis of shock absorption capability and force dispersion effect of mouthguard materials with different impact objects. Dent. Mater. J. 2014, 33, 551–556. [Google Scholar] [CrossRef] [Green Version]
- Mizuhashi, F.; Koide, K. Appropriate fabrication method for vacuum-formed mouthguards using polyolefin sheets. Dent. Traumatol. 2020. (accepted). [Google Scholar] [CrossRef]
- Takahashi, M.; Koide, K.; Iwasaki, S. Thickness of mouthguard sheets after vacuum-pressure formation: Influence of mouthguard sheet material. Dent. Traumatol. 2016, 32, 201–205. [Google Scholar] [CrossRef]
- Going, R.E.; Loehman, R.E.; Chan, M.S. Mouthguard materials: Their physical and mechanical properties. J. Am. Dent. Assoc. 1974, 89, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.-Y.; Shin, S.-R.; Lee, S.-H.; Lee, D.-S. Self-Healing and Mechanical Properties of Thermoplastic Polyurethane/Eugenol-Based Phenoxy Resin Blends via Exchange Reactions. Polymers 2020, 12, 1011. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, E.E.; Powers, J.M. Properties of Custom-Made Mouth-Protector Materials. Phys. Sportsmed. 1986, 14, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Bulsara, Y.R.; Matthew, I.R. Forces transmitted through a laminated mouthguard material with a Sorbothane insert. Dent. Traumatol. 1998, 14, 45–47. [Google Scholar] [CrossRef] [Green Version]
- Guevara, P.A.; Ranalli, D.N. Techniques for mouthguard fabrication. Dent. Clin. North. Am. 1991, 35, 667–682. [Google Scholar]
- Bishop, B.M.; Davies, E.H.; von Fraunhofer, J.A. Materials for mouth protectors. J. Prosthet. Dent. 1985, 53, 256–261. [Google Scholar] [CrossRef]
- Auroy, P.; Duchatelard, P.; Zmantar, N.E.; Hennequin, M. Hardness and shock absorption of silicone rubber for mouth guards. J. Prosthet. Dent. 1996, 75, 463–471. [Google Scholar] [CrossRef]
- Murphy, W.; Black, G.H. Handbook of Biomaterial Properties, 2nd ed.; Springer-Verlag: New York, NY, USA, 2016; ISBN 978-1-4939-3305-1. [Google Scholar]
- Maeda, Y.; Yang, T.-C.; Miyanaga, H.; Tanaka, Y.; Ikebe, K.; Akimoto, N. Mouthguard and Sports Drinks on Tooth Surface pH. Int. J. Sports. Med. 2014, 35, 871–873. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Wang, S.; Ye, H.; Lv, L.; Zhao, X.; Liu, Y.; Zhou, Y. Preliminary Clinical Application of Complete Workflow of Digitally Designed and Manufactured Sports Mouthguards. Int. J. Prosthodont. 2020, 33, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Waked, E.; Caputo, A. Thickness and stiffness characteristics of custom-made mouthguard materials. Dent. Dig. 2005, 36, 462–466. [Google Scholar]
- Reza, F.; Churei, H.; Takahashi, H.; Iwasaki, N.; Ueno, T. Flexural impact force absorption of mouthguard materials using film sensor system. Dent. Traumatol. 2013, 30, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Araie, Y.; Satoh, Y.; Iwasaki, S. Influence of continuous use of a vacuum-forming machine for mouthguard thickness after thermoforming. Dent. Traumatol. 2017, 33, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Mizuhashi, F.; Koide, K.; Takahashi, M. Variations in mouthguard thickness according to fabrication method. Dent. Traumatol. 2015, 31, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Koide, K.; Mizuhashi, F. Optimal heating conditions for forming a mouthguard using a circle tray: Effect of different conditions on the thickness and fit of formed mouthguards. J. Prosthodont. Res. 2014, 58, 171–176. [Google Scholar] [CrossRef]
- Mizuhashi, F.; Koide, K. Pressure-forming Method Using a Single-Mouthguard Sheet. Dent. Traumatol. 2018, 34, 41–45. [Google Scholar] [CrossRef]
- Takahashi, M.; Bando, Y. Thermoforming technique for maintaining the thickness of single-layer mouthguard during pressure formation. Dent. Traumatol. 2019, 35, 285–290. [Google Scholar] [CrossRef]
- Kawarai, C.; Satoh, N.; Matsumoto, M.; Yasui, T. Effect of heating temperature on mouthguard fittings. J. Sport. Dent. 2002, 5, 25–29. [Google Scholar]
- Takahashi, M.; Koide, K.; Mizuhashi, F. Influence of sheet material shape on the thickness and fit of mouthguards. Dent. Traumatol. 2014, 30, 455–460. [Google Scholar] [CrossRef]
- Mizuhashi, R.; Ogura, I.; Sugawara, Y.; Oohashi, M.; Sekiguchi, H.; Saegusa, H.; Mizuhashi, F. Forming temperature of ethylene vinyl acetate sheets for fabrication of vacuum-formed mouthguards. Dent. Traumatol. 2020. (accepted). [Google Scholar] [CrossRef]
- Takahashi, M.; Koide, K.; Mizuhashi, F. Variation in mouthguard thickness due to different heating conditions during fabrication. J. Prosthodont. Res. 2013, 57, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Piedade, A.P. 4D Printing: The Shape-Morphing in Additive Manufacturing. J. Funct. Biomater. 2019, 10, 9. [Google Scholar] [CrossRef] [Green Version]
- Pinho, A.C.; Buga, C.S.; Piedade, A.P. The chemistry behind 4D printing. Appl. Mater. Today 2020, 19, 100611. [Google Scholar] [CrossRef]
- Nejatian, T.; Almassi, S.; Shamsabadi, A.F.; Vasudeva, G.; Hancox, Z.; Dhillon, A.S.; Sefat, F. Digital dentistry. In Advanced Dental Biomaterials; Woodhead Publishing: Duxford, UK, 2019; pp. 507–540. [Google Scholar]
- Yanagi, T.; Kakura, K.; Tsuzuki, T.; Isshi, K.; Taniguchi, Y.; Hirofuji, T.; Kido, H.; Yoneda, M. Fabrication of Mouthguard Using Digital Technology. Dentistry 2019, 9, 1000531. [Google Scholar] [CrossRef]
- Liang, K.; Carmone, S.; Brambilla, D.; Leroux, J.C. 3D printing of a wearable personalized oral delivery device: A first-in-human study. Sci. Adv. 2018, 4, 2544. [Google Scholar] [CrossRef] [PubMed] [Green Version]







| Type | Class |
|---|---|
| I–Thermoplastic type | I–Vacuum-formed |
| II–Mouth-formed | |
| II–Thermosetting type | I–Mouth-formed |
| III–Stock type | -- |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa, A.M.; Pinho, A.C.; Messias, A.; Piedade, A.P. Present Status in Polymeric Mouthguards. A Future Area for Additive Manufacturing? Polymers 2020, 12, 1490. https://doi.org/10.3390/polym12071490
Sousa AM, Pinho AC, Messias A, Piedade AP. Present Status in Polymeric Mouthguards. A Future Area for Additive Manufacturing? Polymers. 2020; 12(7):1490. https://doi.org/10.3390/polym12071490
Chicago/Turabian StyleSousa, Ana M., Ana C. Pinho, Ana Messias, and Ana P. Piedade. 2020. "Present Status in Polymeric Mouthguards. A Future Area for Additive Manufacturing?" Polymers 12, no. 7: 1490. https://doi.org/10.3390/polym12071490






