Multifunctional Biodegradable Vascular PLLA Scaffold with Improved X-ray Opacity, Anti-Inflammation, and Re-Endothelization
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Multifunctional PLLA Films
2.2.1. The First Coating Layer: TIBA/MH Coating on PLLA Films
2.2.2. The Second Coating Layer: PDA/Cys Coating on PLLA Films
2.3. Characterization of Coated PLLA Films
2.3.1. X-Ray Images of Radiopaque PLLA Films
2.3.2. Quantitative Analysis of MH
2.3.3. Water Contact Angle
2.3.4. NO Release Analysis
2.3.5. Elemental Composition and Chemical Bonding Analysis
2.3.6. Surface Morphology
2.3.7. Degradation Behavior
2.4. In Vitro Study
2.4.1. Cell Culture
2.4.2. Cell Proliferation Assay
2.4.3. Inflammation Response Analysis
2.4.4. Platelet Adhesion Test
2.5. Statistical Analysis
3. Results & Discussion
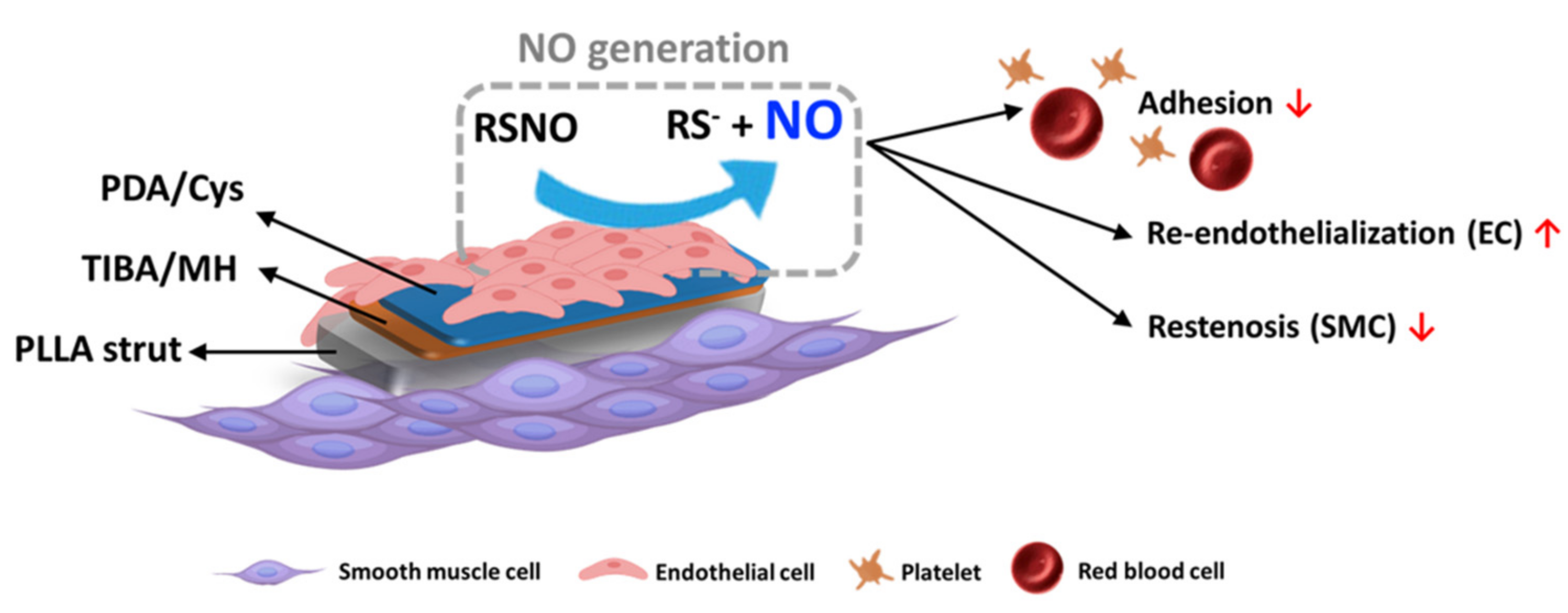
3.1. Preparation and Characterization of Radiopaque and NO Released Film
3.2. Degradation Behavior of the Films and Cumulative Release of TIBA
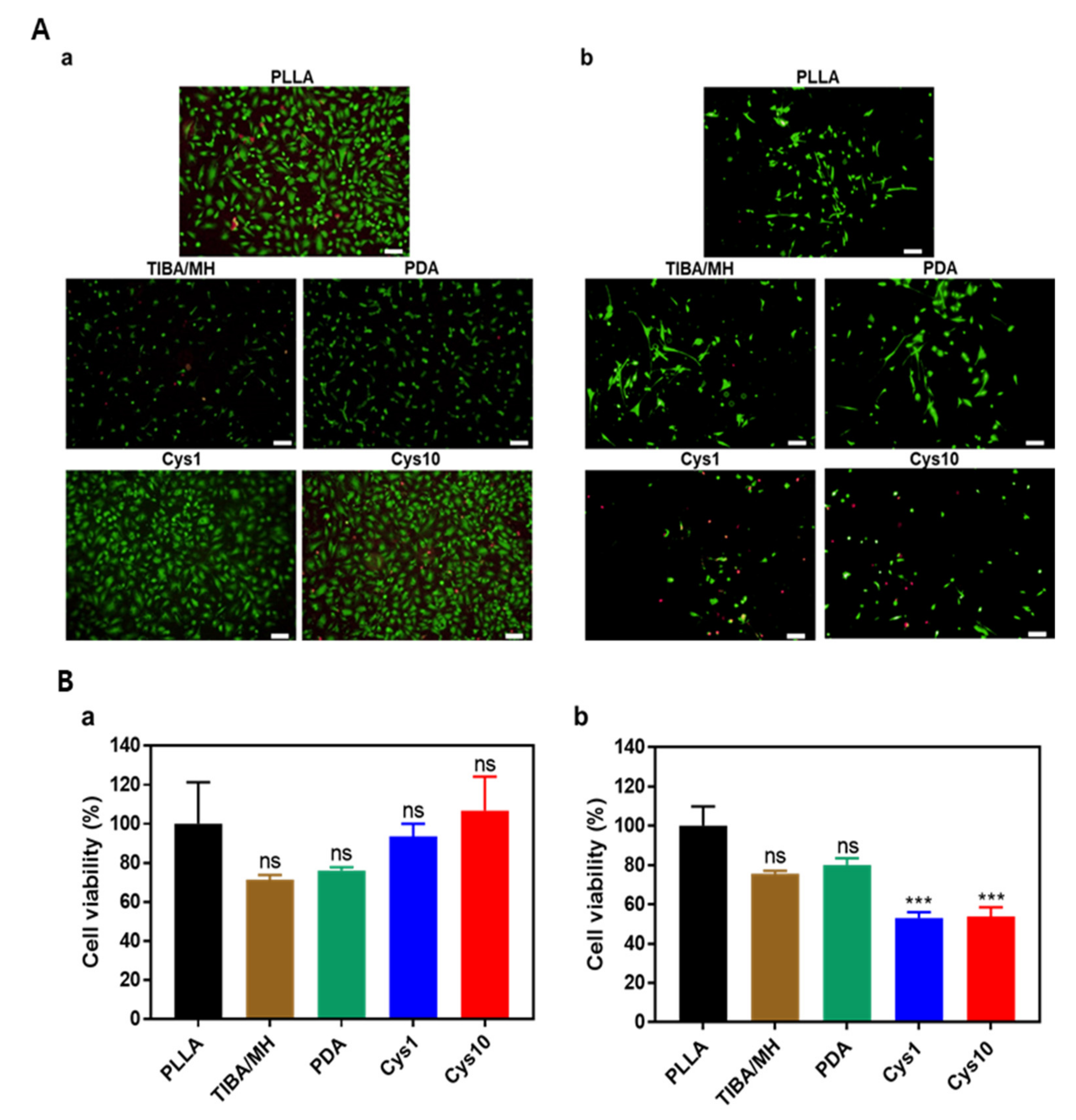
3.3. In Vitro Cell Proliferation
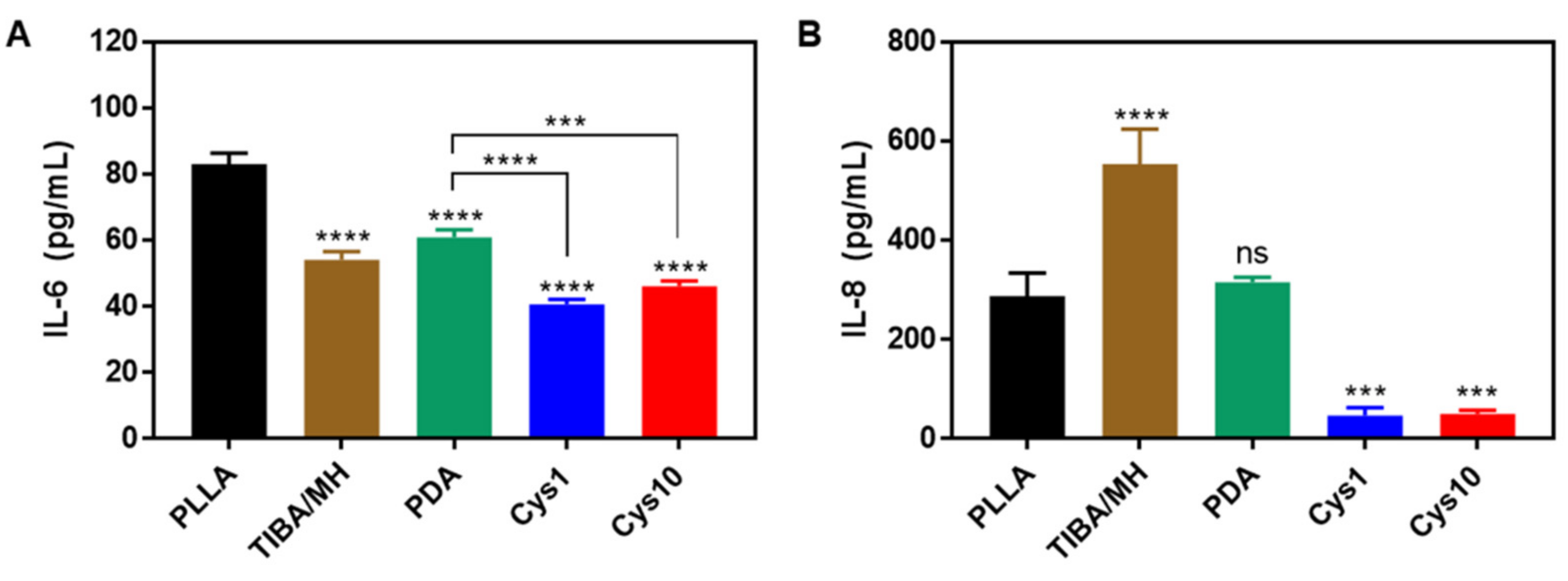
3.4. Inflammation Assay
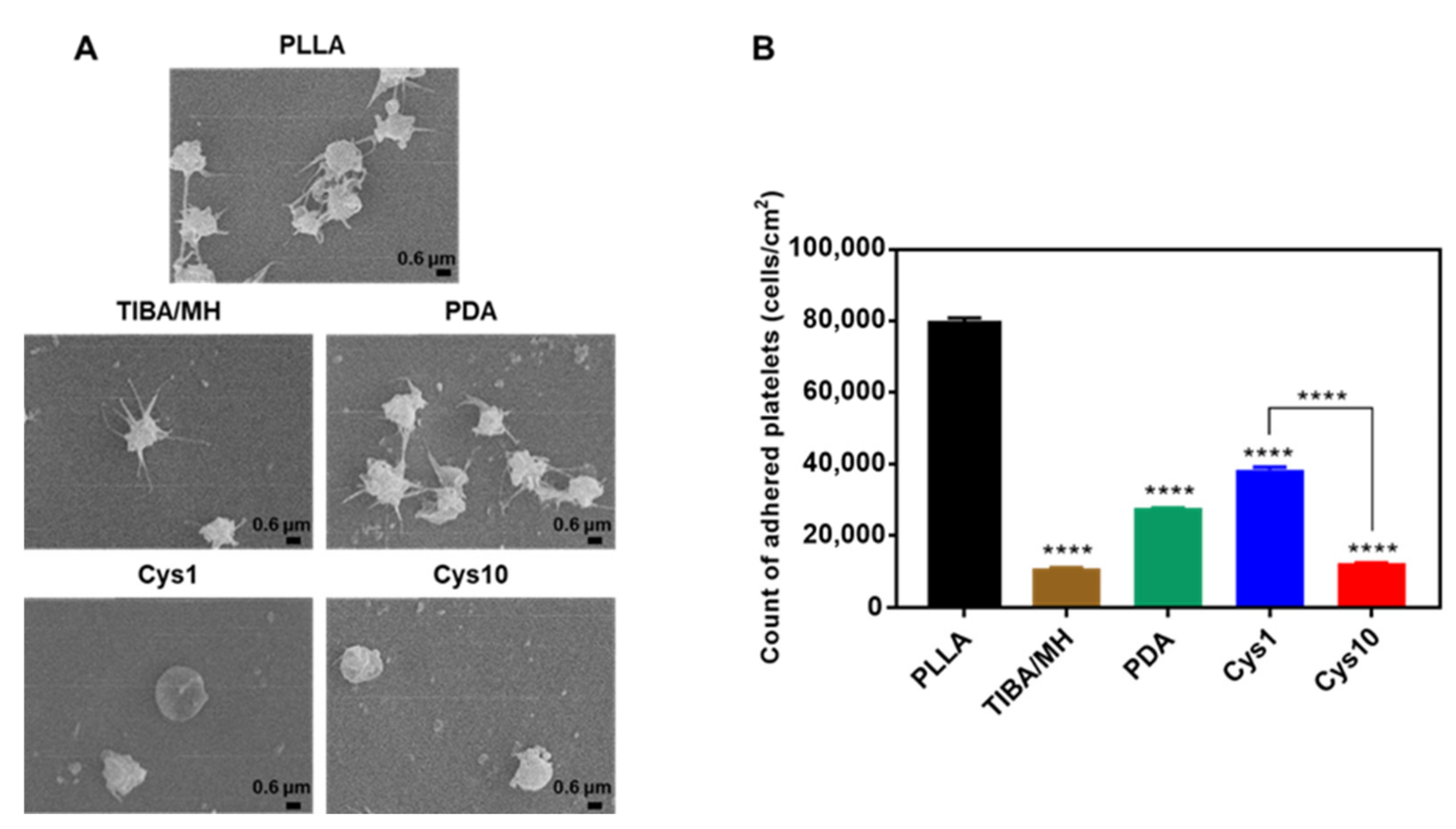
3.5. Platelet Adhesion and Activation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tesfamariam, B. Bioresorbable vascular scaffolds: Biodegradation, drug delivery and vascular remodeling. Pharmacol. Res. 2016, 107, 163–171. [Google Scholar] [CrossRef]
- Sotomi, Y.; Onuma, Y.; Collet, C.; Tenekecioglu, E.; Virmani, R.; Kleiman, N.S.; Serruys, P.W. Bioresorbable scaffold: The emerging reality and future directions. Circ. Res. 2017, 120, 1341–1352. [Google Scholar] [CrossRef] [PubMed]
- Tenekecioglu, E.; Poon, E.K.; Collet, C.; Thondapu, V.; Torii, R.; Bourantas, C.V.; Zeng, Y.; Onuma, Y.; Ooi, A.S.; Serruys, P.W. The nidus for possible thrombus formation: Insight from the microenvironment of bioresorbable vascular scaffold. JACC Cardiovasc. Interv. 2016, 9, 2167–2168. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.-Y.; Choi, D.H.; Jin, Y.M.; Yu, Y.; Kim, H.Y.; Kim, G.; Park, Y.S.; Jo, I. Optimization of Microenvironments Inducing Differentiation of Tonsil-Derived Mesenchymal Stem Cells into Endothelial Cell-Like Cells. Tissue Eng. Regen. Med. 2019, 16, 631–643. [Google Scholar] [CrossRef] [PubMed]
- Parekh, M.; Romano, V.; Hassanin, K.; Testa, V.; Wongvisavavit, R.; Ferrari, S.; Haneef, A.; Willoughby, C.; Ponzin, D.; Jhanji, V.; et al. Biomaterials for corneal endothelial cell culture and tissue engineering. J. Tissue Eng. 2021, 12, 1–19. [Google Scholar] [CrossRef]
- Singhana, B.; Chen, A.; Slattery, P.; Yazdi, I.K.; Qiao, Y.; Tasciotti, E.; Wallace, M.; Huang, S.; Eggers, M.; Melancon, M.P. Infusion of iodine-based contrast agents into poly(p-dioxanone) as a radiopaque resorbable IVC filter. J. Mater. Sci. Mater. Med. 2015, 26, 1–9. [Google Scholar] [CrossRef]
- Samuel, R.; Girard, E.; Chagnon, G.; Dejean, S.; Favier, D.; Coudane, J.; Nottelet, B. Radiopaque poly(ε-caprolactone) as additive for X-ray imaging of temporary implantable medical devices. RSC Adv. 2015, 5, 84125–84133. [Google Scholar] [CrossRef] [Green Version]
- Alexis, F.; Venkatraman, S.; Rath, S.K.; Gan, L.-H.; Venkatraman, S. Some insight into hydrolytic scission mechanisms in bioerodible polyesters. J. Appl. Polym. Sci. 2006, 102, 3111–3117. [Google Scholar] [CrossRef]
- Bedair, T.M.; Lee, C.K.; Kim, D.-S.; Baek, S.-W.; Bedair, H.M.; Joshi, H.P.; Choi, U.Y.; Park, K.-H.; Park, W.; Han, I.; et al. Magnesium hydroxide-incorporated PLGA composite attenuates inflammation and promotes BMP2-induced bone formation in spinal fusion. J. Tissue Eng. 2020, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.Y.; Choi, B.; Park, W.; Kim, I.H.; Han, D.K. One step bulk modification of poly(L-lactic acid) composites with functional additives to improve mechanical and biological properties for cardiovascular implant applications. Colloids Surf. B Biointerfaces 2019, 179, 161–169. [Google Scholar] [CrossRef]
- Elnaggar, M.A.; Seo, S.H.; Gobaa, S.; Lim, K.S.; Bae, I.-H.; Jeong, M.H.; Han, D.K.; Joung, Y.K. Nitric Oxide Releasing Coronary Stent: A New Approach Using Layer-by-Layer Coating and Liposomal Encapsulation. Small 2016, 12, 6012–6023. [Google Scholar] [CrossRef]
- Gkaliagkousi, E.; Ferro, A. Nitric oxide signalling in the regulation of cardiovascular and platelet function. Front. Biosci. 2011, 16, 1873–1897. [Google Scholar] [CrossRef] [Green Version]
- Curtis, B.M.; Leix, K.A.; Ji, Y.; Glaves, R.S.E.; Ash, D.E.; Mohanty, D.K. Slow and sustained nitric oxide releasing compounds inhibit multipotent vascular stem cell proliferation and differentiation without causing cell death. Biochem. Biophys. Res. Commun. 2014, 450, 208–212. [Google Scholar] [CrossRef] [Green Version]
- Liu, G.; Gao, N.; Zhou, Y.; Nie, J.; Cheng, W.; Luo, M.; Mei, L.; Zeng, X.; Deng, W. Polydopamine-Based “Four-in-One&rdquo Versatile Nanoplatforms for Targeted Dual Chemo and Photothermal Synergistic Cancer Therapy. Pharmaceutics 2019, 11, 507. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Jia, F.; Li, Y.; Deng, Y.; Huang, Y.; Liu, W.; Jin, Q.; Ji, J. Nitric oxide-induced stromal depletion for improved nanoparticle penetration in pancreatic cancer treatment. Biomaterials 2020, 246, 119999. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Li, J.-A.; Yao, L.-F.; Li, L.-H.; Yang, P.; Huang, N. Preparation and characterization of Cu-doped TiO 2 thin films and effects on platelet adhesion. Surf. Coat. Technol. 2015, 261, 436–441. [Google Scholar] [CrossRef]
- Jeong, D.-W.; Park, W.; Bedair, T.M.; Kang, E.Y.; Kim, I.H.; Park, D.S.; Sim, D.S.; Hong, Y.J.; Koh, W.-G.; Jeong, M.H.; et al. Augmented re-endothelialization and anti-inflammation of coronary drug-eluting stent by abluminal coating with magnesium hydroxide. Biomater. Sci. 2019, 7, 2499–2510. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Yao, Z.; Wang, J.; Yang, Z.; Ma, X.; Tang, C.Y. Polydopamine coating on a thin film composite forward osmosis membrane for enhanced mass transport and antifouling performance. J. Membr. Sci. 2018, 551, 234–242. [Google Scholar] [CrossRef]
- Kang, E.Y.; Park, S.-B.; Choi, B.; Baek, S.-W.; Ko, K.-W.; Rhim, W.-K.; Park, W.; Kim, I.-H.; Han, D.K. Enhanced mechanical and biological characteristics of PLLA composites through surface grafting of oligolactide on magnesium hydroxide nanoparticles. Biomater. Sci. 2020, 8, 2018–2030. [Google Scholar] [CrossRef]
- Yang, Z.; Yang, Y.; Xiong, K.; Li, X.; Qi, P.; Tu, Q.; Jing, F.; Weng, Y.; Wang, J.; Huang, N. Nitric oxide producing coating mimicking endothelium function for multifunctional vascular stents. Biomaterials 2015, 63, 80–92. [Google Scholar] [CrossRef]
- Bedair, T.M.; Bedair, H.M.; Ko, K.-W.; Park, W.; Joung, Y.K.; Han, D.K. Persulfated flavonoids accelerated re-endothelialization and improved blood compatibility for vascular medical implants. Colloids Surf. B Biointerfaces 2019, 181, 174–184. [Google Scholar] [CrossRef]
- Park, I.-H.; Ju, H.; Kim, K.; Lee, S.S.; Vittal, J.J. Isomerism in double-pillared-layer coordination polymers—Structures and photoreactivity. IUCrJ 2018, 5, 182–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, W.; Xu, L.; Li, X.; Shen, S.; Wu, M.; Bai, Y.; Liu, H. Cysteine-Functionalized Metal–Organic Framework: Facile Synthesis and High Efficient Enrichment of N-Linked Glycopeptides in Cell Lysate. ACS Appl. Mater. Interfaces 2017, 9, 19562–19568. [Google Scholar] [CrossRef]
- Mei, M.L.; Li, Q.-L.; Chu, C.H. Inhibition of Cariogenic Plaque Formation on Root Surface with Polydopamine-Induced-Polyethylene Glycol Coating. Materials 2016, 9, 414. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Qiu, H.; Gao, P.; Yang, Y.; Yang, Z.; Huang, N. Synergetic coordination and catecholamine chemistry for catalytic generation of nitric oxide on vascular stents. NPG Asia Mater. 2018, 10, 482–496. [Google Scholar] [CrossRef]
- Zhang, W.; Yan, L.; Li, Y.; Chen, W.; Hu, N.; Wang, H.; Ou, H. Roles of miRNA-24 in regulating endothelial nitric oxide synthase expression and vascular endothelial cell proliferation. Mol. Cell. Biochem. 2015, 405, 281–289. [Google Scholar] [CrossRef]
- Dormanns, K.; Brown, R.; David, T. The role of nitric oxide in neurovascular coupling. J. Theor. Biol. 2016, 394, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Bedair, T.M.; Heo, Y.; Ryu, J.; Bedair, H.M.; Park, W.; Han, D.K. Biocompatible and functional inorganic magnesium ceramic particles for biomedical applications. Biomater. Sci. 2021, 9, 1903–1923. [Google Scholar] [CrossRef]
- Lih, E.; Kum, C.H.; Park, W.; Chun, S.Y.; Cho, Y.; Joung, Y.K.; Park, K.-S.; Hong, Y.J.; Ahn, D.J.; Kim, B.-S.; et al. Modified Magnesium Hydroxide Nanoparticles Inhibit the Inflammatory Response to Biodegradable Poly(lactide-co-glycolide) Implants. ACS Nano 2018, 12, 6917–6925. [Google Scholar] [CrossRef]
- Mishra, B.B.; Lovewell, R.R.; Olive, A.J.; Zhang, G.; Wang, W.; Eugenin, E.; Smith, C.M.; Phuah, J.Y.; Long, J.E.; Dubuke, M.L.; et al. Nitric oxide prevents a pathogen-permissive granulocytic inflammation during tuberculosis. Nat. Microbiol. 2017, 2, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Simon-Walker, R.; Romero, R.; Staver, J.M.; Zang, Y.; Reynolds, M.M.; Popat, K.C.; Kipper, M.J. Glycocalyx-Inspired Nitric Oxide-Releasing Surfaces Reduce Platelet Adhesion and Activation on Titanium. ACS Biomater. Sci. Eng. 2016, 3, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Fan, Y.; Pan, X.; Wang, K.; Wu, S.; Han, H.; Yang, P.; Luo, R.; Wang, H.; Huang, N.; Tan, W.; et al. Influence of chirality on catalytic generation of nitric oxide and platelet behavior on selenocystine immobilized TiO2 films. Colloids Surf. B Biointerfaces 2016, 145, 122–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]


 , TIBA/MH =
, TIBA/MH =  , PDA =
, PDA =  , Cys1 =
, Cys1 =  , and Cys10 =
, and Cys10 =  ).
).
 , TIBA/MH =
, TIBA/MH =  , PDA =
, PDA =  , Cys1 =
, Cys1 =  , and Cys10 =
, and Cys10 =  ).
).
| Sample | Mg (ppm) a | Atomic Composition (%) b | WCA (θ) c | ||||
|---|---|---|---|---|---|---|---|
| C | O | I | N | S | |||
| PLLA | - | 87.24 | 12.76 | - | - | - | 62.16 ± 1.42 |
| TIBA | 519.03 ± 5.91 | 48.01 | 24.3 | 27.69 | - | - | 59.06 ± 2.22 |
| PDA | 324.08 ± 5.73 | 77.09 | 15.62 | 1.42 | 5.88 | - | 55.18 ± 1.04 |
| Cys1 | 391.26 ± 0.68 | 74.11 | 15.67 | 1.27 | 6.82 | 2.14 | 56.62 ± 1.31 |
| Cys10 | 373.06 ± 0.72 | 71 | 16.43 | 2.5 | 6.46 | 3.61 | 54.08 ± 2.66 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.I.; Heo, Y.; Baek, S.-W.; Kim, D.-S.; Song, D.H.; Han, D.K. Multifunctional Biodegradable Vascular PLLA Scaffold with Improved X-ray Opacity, Anti-Inflammation, and Re-Endothelization. Polymers 2021, 13, 1979. https://doi.org/10.3390/polym13121979
Lee HI, Heo Y, Baek S-W, Kim D-S, Song DH, Han DK. Multifunctional Biodegradable Vascular PLLA Scaffold with Improved X-ray Opacity, Anti-Inflammation, and Re-Endothelization. Polymers. 2021; 13(12):1979. https://doi.org/10.3390/polym13121979
Chicago/Turabian StyleLee, Ho In, Yun Heo, Seung-Woon Baek, Da-Seul Kim, Duck Hyun Song, and Dong Keun Han. 2021. "Multifunctional Biodegradable Vascular PLLA Scaffold with Improved X-ray Opacity, Anti-Inflammation, and Re-Endothelization" Polymers 13, no. 12: 1979. https://doi.org/10.3390/polym13121979






