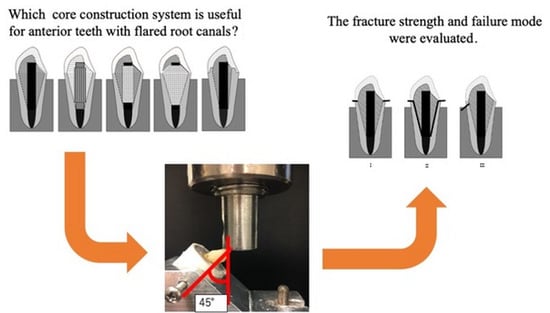
Influence of New Sleeve Composite on Fracture Behavior of Anterior Teeth with Flared Root Canals
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Experimental Groups
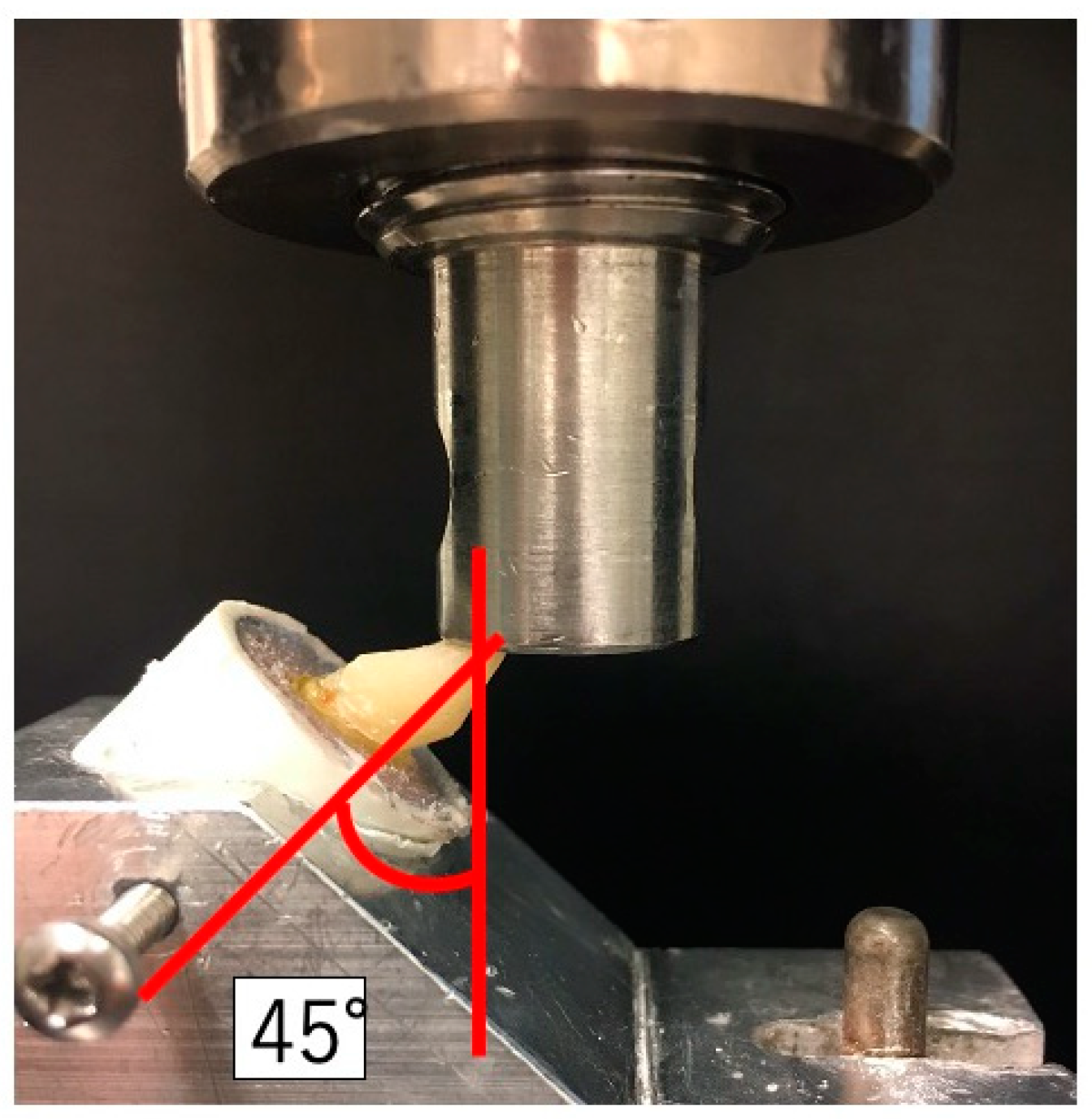
2.3. Loading Test
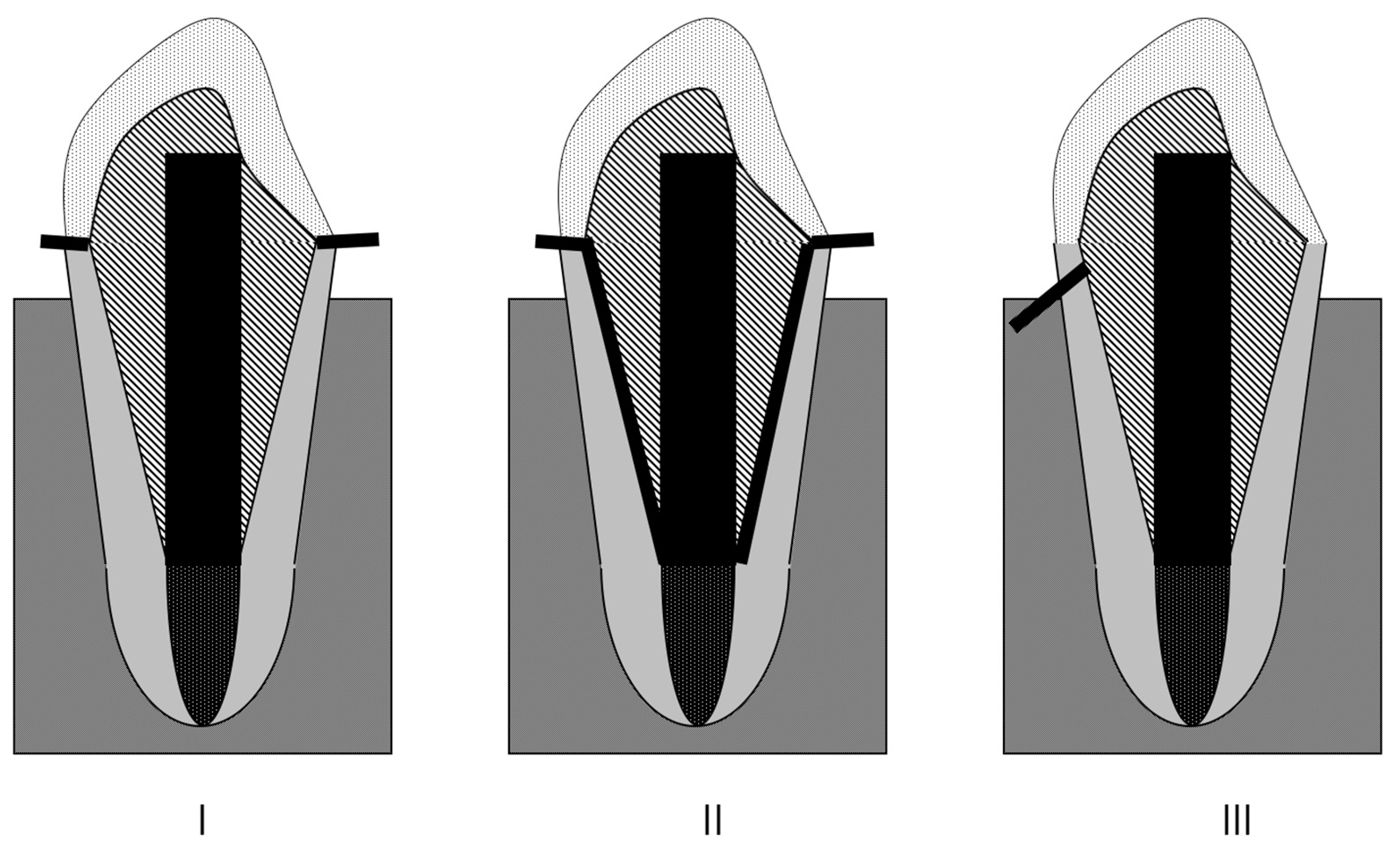
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pegoretti, A.; Fambri, L.; Zappini, G.; Bianchetti, M. Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials 2002, 23, 2667–2682. [Google Scholar] [CrossRef]
- Duret, B.; Duret, F.; Reynaud, M. Long-life physical property preservation and postendodontic rehabilitation with the composipost. Compend. Contin. Educ. Dent. Suppl. 1996, 20, 50–56. [Google Scholar]
- Lanza, A.; Aversa, R.; Rengo, S.; Apicella, D.; Apicella, A. 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent. Mater. 2005, 21, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Fukui, Y.; Komada, W.; Yoshida, K.; Otake, S.; Okada, D.; Mıura, H. Effect of reinforcement with resin composite on fracture strength of structurally compromised roots. Dent. Mater. J. 2009, 28, 602–609. [Google Scholar] [CrossRef]
- Pinto, C.L.; Bhering, C.L.B.; de Oliveir, G.R.; Maroli, A.; Reginato, V.F.; Caldas, R.A.; Bacchi, A. The Influence of Post System Design and Material on the Biomechanical Behavior of Teeth with Little Remaining Coronal Structure. J. Prosthodont. 2019, 28, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Grandini, S.; Goracci, C.; Monticelli, F.; Tay, F.R.; Ferrari, M. Fatigue resistance and structural characteristics of fiber posts: Three-point bending test and SEM evaluation. Dent. Mater. 2005, 21, 75–82. [Google Scholar] [CrossRef]
- Amižić, I.P.; Miletić, I.; Baraba, A.; Fan, Y.; Nathanson, D. In vitro retention of prefabricated and individually formed posts: A pilot study. J. Prosthet. Dent. 2018, 120, 553–557. [Google Scholar] [CrossRef]
- Ruschel, G.H.; Gomes, É.A.; Silva-Sousa, Y.T.; Pinelli, R.G.; Sousa-Neto, M.D.; Pereira, G.K.; Spazzin, A.O. Mechanical properties and superficial characterization of a milled CAD-CAM glass fiber post. J. Mech. Behav. Biomed. Mater. 2018, 82, 187–192. [Google Scholar] [CrossRef]
- Gomes, G.M.; Gomes, O.M.; Gomes, J.C.; Loguercio, A.D.; Calixto, A.L.; Reis, A. Evaluation of different restorative techniques for filling flared root canals: Fracture resistance and bond strength after mechanical fatigue. J. Adhes. Dent. 2014, 16, 267–276. [Google Scholar]
- Frater, M.; Forster, A.; Jantyik, A.; Braunitzer, G.; Nagy, K.; Grandini, S. In vitro fracture resistance of premolar teeth restored with fibrereinforced composite posts using a single or a multi-post technique. Aust. Endod. J. 2017, 43, 16–22. [Google Scholar] [CrossRef]
- Inaba, Y.; Teraoka, F.; Nakagawa, M.; Imazato, S. Development of a new direct core build-up method using a hollow fiber-reinforced post. Dent. Mater. J. 2013, 32, 718–724. [Google Scholar] [CrossRef] [PubMed]
- Kubo, M.; Komada, W.; Otake, S.; Inagaki, T.; Omori, S.; Miura, H. The effect of glass fiber posts and ribbons on the fracture strength of teeth with flared root canals restored using composite resin post and cores. J. Prosthodont. Res. 2018, 62, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Boudrias, P.; Sakkal, S.; Petrova, Y. Anatomical post design meets quartz fiber technology: Rationale and case report. Compend. Cont. Educ. Dent. 2001, 22, 337–340. [Google Scholar]
- Grandini, S.; Sapio, S.; Simonetti, M. Use of anatomic post and core for reconstructing an endodontically treated tooth: A case report. J. Adhes. Dent. 2003, 5, 243–247. [Google Scholar] [PubMed]
- Feilzer, A.J.; Dauvillier, B.S. Effect of TEGDMA/BisGMA ratio on stress development and viscoelastic properties of experimental two-paste composites. J. Dent. Res. 2003, 82, 824–828. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Carvalho, C.A.; Goracci, C.; Antoniolli, F.; Mazzoni, A.; Mazzotti, G.; Cadenaro, M.; Breschi, L. Influence of luting material filler content on post cementation. J. Dent. Res. 2009, 88, 951–956. [Google Scholar] [CrossRef]
- Cagidiaco, M.C.; Goracci, C.; Garcia-Godoy, F.; Ferrari, M. Clinical studies of fiber posts: A literature review. Int. J. Prosthodont. 2008, 21, 328–336. [Google Scholar]
- Fontana, P.E.; Bohrer, T.C.; Wandscher, V.F.; Valandro, L.F.; Limberger, I.F.; Kaizer, O.B. Effect of Ferrule Thickness on Fracture Resistance of Teeth Restored With a Glass Fiber Post or Cast Post. Oper. Dent. 2019, 44, E299–E308. [Google Scholar] [CrossRef]
- Marchionatti, A.M.E.; Wandscher, V.F.; Rippe, M.P.; Kaizer, O.B.; Valandro, L.F. Clinical performance and failure modes of pulpless teeth restored with posts: A systematic review. Braz. Oral. Res. 2017, 31, e64. [Google Scholar] [CrossRef]
- Santos Pantaleón, D.; Valenzuela, F.M.; Morrow, B.R.; Pameijer, C.H.; García-Godoy, F. Effect of Ferrule Location with Varying Heights on Fracture Resistance and Failure Mode of Restored Endodontically Treated Maxillary Incisors. J. Prosthodont. 2019, 28, 677–683. [Google Scholar] [CrossRef]
- Yoshii, S.; Garoushi, S.; Kitamura, C.; Vallittu, P.K.; Lassila, L.V. Evaluation of new hollow sleeve composites for direct post-core construction. Materials 2021, 14, 7397. [Google Scholar] [CrossRef] [PubMed]
- Hatta, M.; Shinya, A.; Vallittu, P.K.; Shinya, A.; Lassila, L.V. High volume individual fiber post versus low volume fiber post: The fracture load of the restored tooth. J. Dent. 2011, 39, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Uctasli, S.; Boz, Y.; Sungur, S.; Vallittu, P.K.; Garoushi, S.; Lassila, L.V. Influence of Post-Core and Crown Type on the Fracture Resistance of Incisors Submitted to Quasistatic Loading. Polymers 2021, 13, 1130. [Google Scholar] [CrossRef]
- Nothdurft FPSchmitt TRupf SPospiech, P.R. Influence of fatigue testing and cementation mode on the load-bearing capability of bovine incisors restored with crowns and FRC posts. Dent. Mater. J. 2011, 30, 109–114. [Google Scholar]
- Hattori, M.; Takemoto, S.; Yoshinari, M.; Kawada, E.; Oda, Y. Durability of fiber-post and resin core build-up systems. Dent. Mater. J. 2010, 29, 224–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagase, D.Y.; Takemoto, S.; Hattori, M.; Yoshinari, M.; Kawada, E.; Oda, Y. Influence of fabrication techniques on retention force of fiber-reinforced composite posts. Dent. Mater. J. 2005, 24, 280–285. [Google Scholar] [CrossRef]
- Öztürk, C.; Polat, S.; Tunçdemir, M.; Gönüldaş, F.; Şeker, E. Evaluation of the fracture resistance of root filled thin walled teeth restored with different post systems. Biomed. J. 2019, 42, 53–58. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Özcan, M. Clinical Guide to Principles of Fiber-Reinforced Composites in Dentistry; Woodhead Publishing: Duxford, UK, 2017; pp. 11–16. [Google Scholar]
- Fráter, M.; Sáry, T.; Braunitzer, G.; Balázs Szabó, P.; Lassila, L.; Vallittu, P.K.; Garoushi, S. Fatigue failure of anterior teeth without ferrule restored with individualized fiber-reinforced post-core foundations. J. Mech. Behav. Biomed. Mater. 2021, 118, 104440. [Google Scholar] [CrossRef]
- Bijelic, J.; Garoushi, S.; Vallittu, P.K.; Lassila, L.V. Fracture load of tooth restored with fiber post and experimental short fiber composite. Open Dent. J. 2011, 29, 58–65. [Google Scholar] [CrossRef]
- Magne, P.; Goldberg, J.; Edelhoff, D.; Güth, J.F. Composite Resin Core Buildups With and Without Post for the Restoration of Endodontically Treated Molars Without Ferrule. Oper. Dent. 2016, 41, 64–75. [Google Scholar] [CrossRef]
- Säilynoja, E.; Garoushi, S.; Vallittu, P.K.; Lassila, L. Characterization of Experimental Short-Fiber-Reinforced Dual-Cure Core Build-Up Resin Composites. Polymers 2021, 13, 2281. [Google Scholar] [CrossRef] [PubMed]
- Fráter, M.; Sáry, T.; Néma, V.; Braunitzer, G.; Vallittu, P.; Lassila, L.; Garoushi, S. Fatigue failure load of immature anterior teeth: Influence of different fiber post-core systems. Odontology 2021, 109, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Franciosa, P.; Martorelli, M.; Watts, D.C. Mechanical behavior of post-restored upper canine teeth: A 3D FE analysis. Dent. Mater. 2011, 27, 1285–1294. [Google Scholar] [CrossRef] [PubMed]
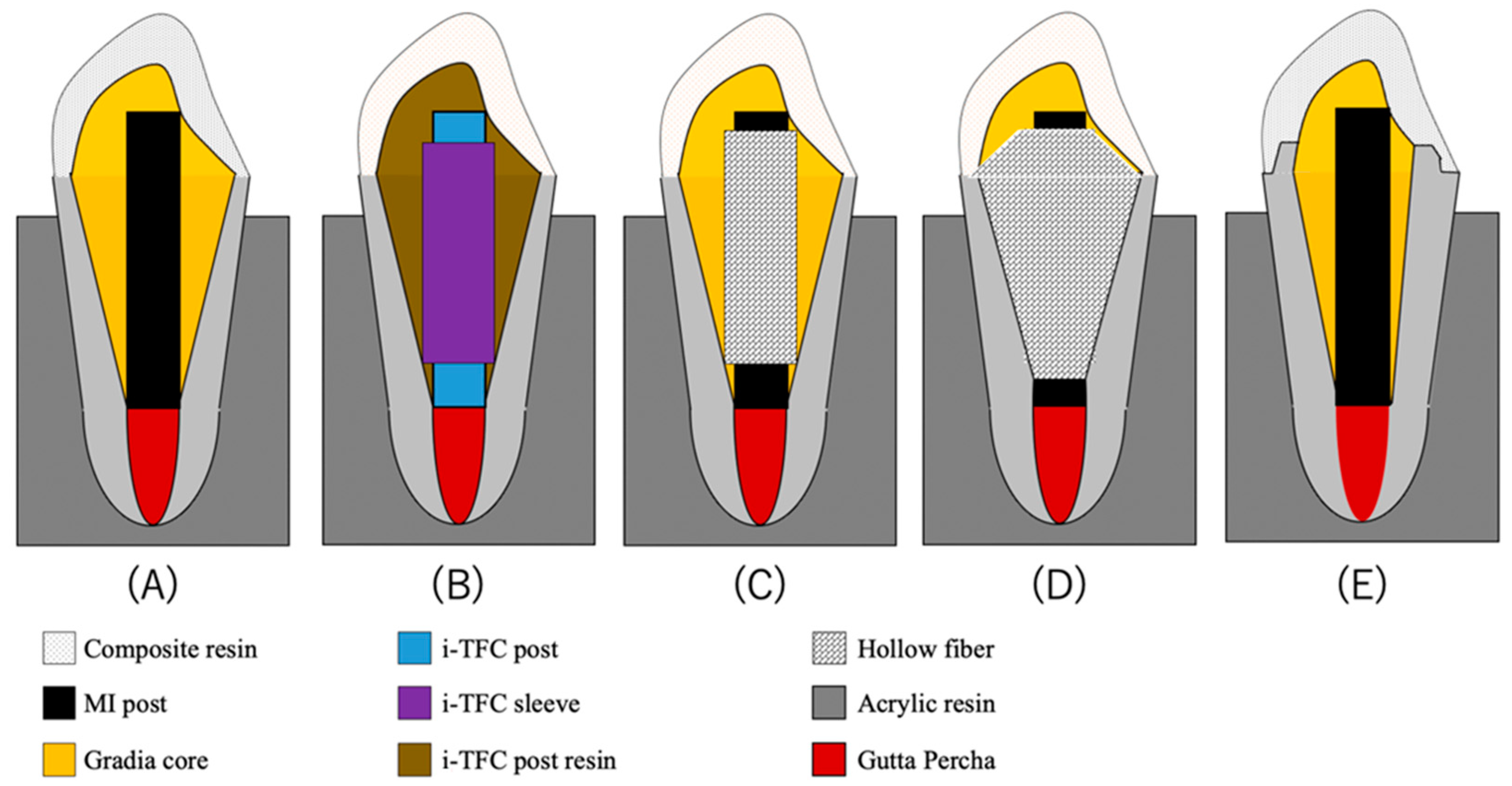
| Materials | Manufacture | Lot Number | Characteristic | Composition |
|---|---|---|---|---|
| E-glass sheet | Hexcel | 85M208171309 | E-glass | |
| i-TFC post | Sun Medical | SL1 | Diameter: 1.5 mm | Glass fiber, Optical fiber UDMA-based matrix resin |
| i-TFC sleeve | SK1 | Inner Diameter: 1.5 mm Outer Diameter: 2.0 mm | Glass fiber UDMA-based matrix resin | |
| i-TFC post resin | SL12 | Bis-MPEPP, PDMA, TEGDMA, UDMA, PI, Barium Silica Glass | ||
| i-TFC Bond | Bond; SR1R Brush; SR11 | Bond: 4-META, Bis-MPEPP, PI, Acetone, Water, Silica Bond brushes: Sodyum p-toluenesulfinate, Aromatic amine | ||
| Gradia core | GC Europe | 1804161 | Fluoroaluminosilicate glass filler Bismethacrylate | |
| MI post | 20170728 | Diameter: 1.5 mm | E-glass, PMMA | |
| G-ænial Anterior | 180605A | UDMA, Dimethacrylate co-monomer, slica | ||
| G-Premio Bond | 1510291 | 10-MDP, 4-META, thiophosphate, methacrylate adicester, distilled water, acetone, photo initiators, silica fine powder | ||
| Ceramic primer II | 1712062S | silane, MDP, ethanol | ||
| ScotchbondTM Universal Etchant | 3M ESPE | 564429 | Water, Phosphoric Acid, Synthetic Amorphous Silica, Fumed, Crystalline free, Polyethylene Glycol, Aluminum Oxide |
| Group | Fracture Load (N) MEAN ± SD |
|---|---|
| A (MI) | 381.06 ± 85.0 a |
| B (i-TFC) | 390.47 ± 112.32 a |
| C (Sleeve composite) | 641.81 ± 105.54 b |
| D (Tapered E-glass filling) | 443.55 ± 85.75 a |
| E (Ferrule) | 843.79 ± 83.18 c |
| Group | Favorable Fracture | Non-Favorable Fracture | |
|---|---|---|---|
| I | II | III | |
| A (MI) | 2 | 0 | 8 |
| B (i-TFC) | 8 | 1 | 1 |
| C (Sleeve composite) | 9 | 0 | 1 |
| D (Tapered E-glass filling) | 6 | 0 | 4 |
| E (Ferrule) | 9 | 0 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshii, S.; Garoushi, S.; Kitamura, C.; Vallittu, P.K.; Lassila, L. Influence of New Sleeve Composite on Fracture Behavior of Anterior Teeth with Flared Root Canals. Polymers 2022, 14, 4073. https://doi.org/10.3390/polym14194073
Yoshii S, Garoushi S, Kitamura C, Vallittu PK, Lassila L. Influence of New Sleeve Composite on Fracture Behavior of Anterior Teeth with Flared Root Canals. Polymers. 2022; 14(19):4073. https://doi.org/10.3390/polym14194073
Chicago/Turabian StyleYoshii, Shinji, Sufyan Garoushi, Chiaki Kitamura, Pekka K. Vallittu, and Lippo Lassila. 2022. "Influence of New Sleeve Composite on Fracture Behavior of Anterior Teeth with Flared Root Canals" Polymers 14, no. 19: 4073. https://doi.org/10.3390/polym14194073