1. Introduction
The biointegration or long-term functional stability of implant materials depends on several factors. The most important ones are the bulk and surface characteristics of the material, the biocompatibility and design of the material. Additionally, the applied surgical technique and the life quality or health awareness of the patient are essential issues [
1].
Although the bulk properties (mechanical and thermal characteristics) of biomaterials are important with respect to their biointegration, the biological responses of the surrounding tissues to orthopedic implants are controlled mostly by their surface characteristics (chemistry and structure) because biorecognition takes place at the interface of the implant and host tissue.
Orthopedic implants are comprised of various materials, dependent upon the function they are intended to replace. Their biological behavior and survival can be controlled at the molecular and cellular level by the modification of the implant surface. Numerous modifications have been applied to medical implants in the past few decades to improve their functionality [
2]. The optimal implant surface is different for any given purpose, thus, when the goal is to develop an implant surface, then the targeted functional part and the purpose of the modification has to be specified.
Many of these surfaces (and their modifications) are in the experimental stage and the in vitro, in vivo or clinical studies are still ahead. It is our belief that these characterizations will represent a huge positive contribution to clinical implant science and will help clinicians in selecting the optimal orthopedic implants for their patients.
Ideally, an orthopedic implant attaches rigidly to the bone during the patient’s remaining lifetime and must sustain strong forces whilst being pain-free. Orthopedic implant fixation can be classified as cemented fixation or biological (cementless) fixation. In cemented prostheses, bone cement poly-methyl-methacrylate (PMMA) is a grouting material positioned between the cement and the bone, resulting in two interfaces: implant–cement interface and cement–bone interface [
3].
Long-term results of cementless joint replacement implants are largely determined by their integration into the receiving bone, known as osseointegration. Development of this biological process is essentially determined by the surface characteristics of the implanted device [
4].
The most widely used metal for load-bearing implants is Titanium (Ti), due to its outstanding mechanical and biological properties. Titanium is a suitable implant material in every area of internal fixation. High corrosion resistance and chemical stability, excellent biocompatibility, bone apposition, lack of allergic reactions, low elastic modulus (high elastic flexibility), low weight and modifiable surface properties all sufficiently characterize Ti. In addition to these characteristics, reduced artifacts with magnetic resonance imaging (MRI) makes Ti a preferable choice for implant osteosynthesis [
5]. Since its introduction as a medical implant in the 1950s, clinical demands have greatly increased. To meet these expectations, numerous modifications have been made regarding the alloy composition and the surface properties to achieve improved function and duration in the human body [
6].
The surface roughness significantly determines the biointegration of a medical implant. In vitro studies and clinical experience proved that increasing the roughness of Ti alloy implants improves their osseointegration and osteogenic potential [
7,
8].
The currently used implant designs commonly seen in hip and knee replacements result in the formation of wearing particles at the articulating contact areas, which can lead to inflammation, osteolysis and inevitably, aseptic loosening of the prosthesis [
9].
Its outstanding wear resistance and availability made Polyethylene (PE) a frequently used material in high-stress applications, such as total hip or total knee replacements. [
10] Goswami and Alhassan developed a prediction model regarding UHMWPE in THR and TKR. The primary predicting factors were head diameter, body weight and head surface roughness (Ra) [
11].
As an articulating surface, highly cross-linked UHMWPE revealed excellent results on wear rates in comparison with the conventional UHMWPEs. Cross-linking deteriorates the mechanical properties of UHMWPE limiting its utilization in high-stress contact applications such as TKA. However, when compared to UHMWPE, HXL showed 90% reduced wear rates [
12,
13].
Buford and Goswani compared wear rates of bearing material types. Titanium alloys and stainless steels resulted in increased wear rates when compared to ceramics and cobalt chromium alloys [
14]. Stainless steels paired with polyethylene produced higher wear rates than when compared with cobalt chromium on polyethylene, and ceramic (Alumina) on polyethylene produced the lowest rates of the materials. Despite its good wear rates, the early ceramics had a high risk of fracture. Increasing its fracture resistance through altered manufacturing resulted in lower failure rates [
15].
Zagra and Gallazzi reviewed bearing surfaces in primary total hip arthroplasty, in which they indicated that the application of the ceramic-on-ceramic or ceramic-on-polyethylene type bearing was dependent upon patient age and activity. Metal-on-polyethylene is still a valid option for older patients with good results lasting up to 15 years. Today, despite its early promising outcomes of hip resurfacing, metal-on-metal bearing is nearly entirely abandoned due to the adverse reactions caused by metal debris [
16].
Total Knee Joint replacement (TKJR) prostheses consist of femoral, tibial and patellar components. The typical material regarding the femoral component is CoCr. Tibia components can be divided into monolith UHMWPE components or modular tibia components. Modular tibia components consist of a titanium alloy tibia tray into which the polyethylene can be inserted. The patellar component is made of UHMWPE with added titanium alloy for cementless use [
3].
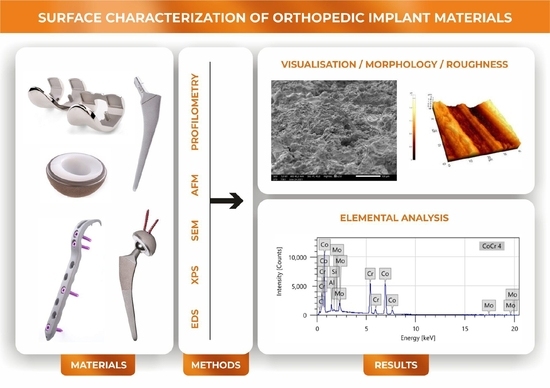
The aim of the present work was to conduct a thorough analysis of the surface characteristics (morphology and composition) of the above-described prostheses materials since their biointegration and long-term survival primarily depend upon their surface features. Determining the significant differences between the surface characteristics of different implant types widely used in orthopedic surgery and traumatology will highlight the importance of the appropriate knowledge of clinicians and adequate implant material choice. To the best of our knowledge, there has not yet been a study comparing these implant materials in this respect.
Material surfaces were visualized using Scanning Electron Microscopy (SEM), Atomic Force Microscopy (AFM) and profilometry. SEM created high resolution images for accurate imaging; furthermore, AFM and profilometry provided topographies and surface roughness values. Combined with the electron microscopic examinations, Energy-dispersive X-ray Spectroscopy (EDS) and X-ray photoelectron spectroscopy (XPS) were utilized for surface chemical characterization.
4. Discussion
SEM, AFM and profilometry studies proved significant differences and typical features of the surface morphology regarding our investigated materials. Profilometry showed different values when compared to AFM due to the different FOVs. EDS and XPS revealed typical elements on the investigated materials.
The Anodized Ti2 surface showed concentric grooves created by the turn mill during the processing of the sample. The granular morphologic structure overlapping the grooves is the result of the anodization process. AFM at the 40 μm × 40 μm areas revealed the overlapping structures, while smaller FOVs revealed the precise characteristics of the granules. Our previous study proved that the surface roughness determined by AFM is dependent upon the field of measurement due to the different macroscopic features of the surfaces [
19].
Therefore, in consideration of a thorough characterization of biomaterials, it is advisable to measure roughness at different scan sizes. Profilometric determination of the roughness gives the characterization of a larger surface of the samples, hence, in case of complex surfaces, it is worthwhile to determine the roughness by both methods (AFM and profilometry).
In its role as bone plate material, titanium provides many advantages when compared with stainless steel. Ti alloys match the modulus of elasticity of the bone better, it provides increased strength, and it is more bioinert. Formation of a self-regenerating TiO
2 layer on its surface provides corrosion resistance. However, removal may be difficult due to good osseointegration of the implant and possible cold welding between the screws and plate [
20].
Anodization offers ideal bioactive surface properties for Titanium implants. It can provide a porous, rough surface with higher surface energy and ideal hydrophilic properties for osseointegration [
21].
Kim et al. and Mühl et al. reported the formation of a rougher and thicker oxide layer as the result of anodization on commercially pure Ti used for orthopedic and dental implants, demonstrated by SEM-EDS, AFM and XPS [
19,
22]. Traini et al. find that anodized titanium surfaces have a high ability inducing fibrin formation thus accelerating osseointegration and it showed a significantly higher bone-implant contact rate compared to non-anodized implants. They also measured the nano-roughness of anodized dental implant surfaces in which they found a value close to the results of our investigation (Ra: 286 ± 40 nm) [
23]. Yildiz et al. performed profilometry measurements on Ti discs with an anodized SLA (sand blasted, large grit, acid etched) surface used as dental implants and also produced similar results (Ra: 1.39 μm) [
24].
Studies showed that anodized dental implants provide promising results with a low rate of marginal bone loss [
25].
TPS discs revealed a much rougher, irregular surface, determined with profilometry and SEM-EDS. Titanium plasma spraying creates typical surfaces with random droplet-shaped scatters. Our SEM-EDS and XPS measurements revealed a high proportion of Ti
4+ on Ti2 and TPS samples, which confirms the presence of a thick oxide layer on their surfaces. In addition to these findings, the anodized sample has a more homogenous and denser oxide layer when compared to the TPS sample. The altered topography generated by Titanium plasma spraying increases its tensile strength on the bone/implant interface, as reported by Buser et al. [
26].
Studies showed that the thick oxide layers detected on TPS samples have an enhancing effect upon bone formation [
27,
28].
Titanium plasma spraying is a common method for increasing the surface in cementless hip prostheses. As mentioned above, increasing the roughness favors osseointegration, yet also facilitates bacterial adhesion [
29].
Lombardi et al. followed up on 2000 tapered titanium-porous-plasma-sprayed THR cementless femoral components. They reported a 95.5% survival rate at 20 years with a low rate of septic revisions (0.4%) [
30].
Stainless steel plates showed a much smoother surface in contrast to the TPS discs.
Wu et al. investigated the bacterial adhesion and microcolony formation on unpolished and differently electropolished stainless steel surfaces. The AFM-measured average roughness of the unpolished surface was in the same range as our R
a value. Their XPS measurements showed the unpolished surface contained similar proportions of C, O, Fe and N, much as in the case of our samples. On their surfaces, there was also a small amount of Cr; however, unlike ours, it did not contain any other elements such as Al or Ni [
31].
Stainless steel was the first class of alloy introduced for orthopedic implants and it is still used as a cemented hip prosthesis material [
32]. Studies demonstrated that, particularly for cemented THR designs, better results are gained with smooth surfaces as compared to rough surfaces [
33]. PMMA is vulnerable to tensile stresses and shear forces, yet it tolerates compressive loads. A polished, smooth surface results in a weak cement–stem bond. Poorly bound, tapered stems do not create tensile and shear stresses in the cement and the cement–bone interface. In contrast, designs with a rough surface can result in detrimental debris formation causing the loss of bony support (osteolysis) of the implant and inevitably, the loosening of the implant [
34].
In the case of cement fixation, the stainless steel hip prosthesis stem shows better long-term results than titanium. The latter bends more easily, which can lead to cement breakage and the formation of fragments, ultimately causing aseptic loosening [
35].
According to the national joint replacement registries, polished, collarless and tapered stems with round edges and a rectangular cross-section provides good clinical outcomes [
36,
37].
Although today the implantation rate of cemented THA stems has decreased significantly compared to cemented stems, evidence shows better outcomes of cemented femoral components in elderly patients especially in females and those with overall poor bone quality [
38].
CoCr proved to have the lowest level of roughness of the samples measured via the profilometer. Our findings are consistent with the data published by Revilla-Léon et al. [
39]. Their study compared chemical composition (EDS), surface roughness (profilometry) and ceramic shear bond stress of milled and selective laser melted (SLE) CoCr surfaces. EDS and profilometry showed similar results when compared with our investigation.
Cobalt-based alloys are nonmagnetic, wear-, corrosion- and heat-resistant. The first medical application of cobalt-based alloys was in the cast of dental implants due to its excellent degradation resistance against the hostile oral environment. Currently, the medical applications of Co alloys are mostly for orthopedic prostheses of the hip, knee and shoulder and also in support of fracture fixation devices [
40].
The main limitation of metal-on-polyethylene bearing was poor wear properties of UHMWPE, which resulted in the aseptic loosening of the components. Furthermore, the use of larger diameters further increased this risk. To solve this problem, the aim of the research in the 1980s and 1990s was to develop a more resistant bearing surface [
41].
Retrospective clinical studies showed that the CoCr-HXLPE bearing type has low wear rates in THR, regardless of femoral head size [
42].
CoCr alloys are the most frequently used materials for TKR femoral components. The procedure facilitates good postoperative joint function recovery and demonstrates excellent long-term follow-up results. Despite the good results, wear debris inducing osteolysis and aseptic loosening is still a concern and one of the major causes of TKR failure [
43].
Its outstanding corrosion resistance is due to the thin Cr2O3 layer that forms on its surface during manufacturing, which reduces the outflow of metal ions into the tissues. According to studies, using additional manufacturing methods, the rate of ion outflow is even lower [
44,
45].
PE wear plays an important role in implant loosening after TKR. Civinini et al. compared the annual reports of the National Joint Registers and found higher 10-year cumulative revision rates for UHMWPE (5.8%) than HXLPE (3.5%) [
46].
The investigated HXLPE and UHMWPE samples showed similar smooth and regular surfaces visualized by SEM. Their measured roughness was in the same range with a relatively low value with both AFM and profilometry. These results are consistent with its function as a bearing surface. EDS and XPS showed that the materials consisted mostly of carbon and oxygen as expected. Disparate O binding states on the investigated PE surfaces proved by XPS, are likely due to the applied radiation crosslinking method in manufacturing HXLPE material.
Particulate wear and delamination wear due to oxidation are historical issues associated with UHMWPE. As a solution to the problem, HXLPE created by irradiation was introduced to clinical practice. Better wear and oxidation resistance makes HXL a good option for THR, yet decreased mechanical properties when compared to UHMWPE are a cause of concern in its application in TKR. Another important phenomenon regarding HXLPE is the production of smaller wear debris particles which can be more biologically active [
47].
Check et al. compared the friction behavior of two PE surfaces with different levels of roughness (Ra: 130 nm ± 19.9 vs. 62.5 nm ± 4.0) against the silicone–nitride interface in air and in the bovine serum. In a similar study, Gispert et al. investigated the wear characteristics of standard (Ra: 126 nm) and smooth (Ra: 22 nm) PE surfaces. They discovered, in the presence of protein, wear is very low, independent of its roughness [
48,
49]. In both studies, roughness measurements were carried out via AFM and one of the tested materials had a similar Ra value as our investigated PE surfaces (HXLPE: 147 ±13, UHMWPE: 144 ± 15).