Beneficial Roles of Cellulose Patch-Mediated Cell Therapy in Myocardial Infarction: A Preclinical Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Experimental Design
2.3. Acute Myocardial Infarction Model
2.4. Euthanasia
2.5. Echocardiographic Analysis
2.6. Cell Isolation Procedures
2.7. MTT Assay
2.8. Cytometric Analysis
2.9. Histopathological Analysis
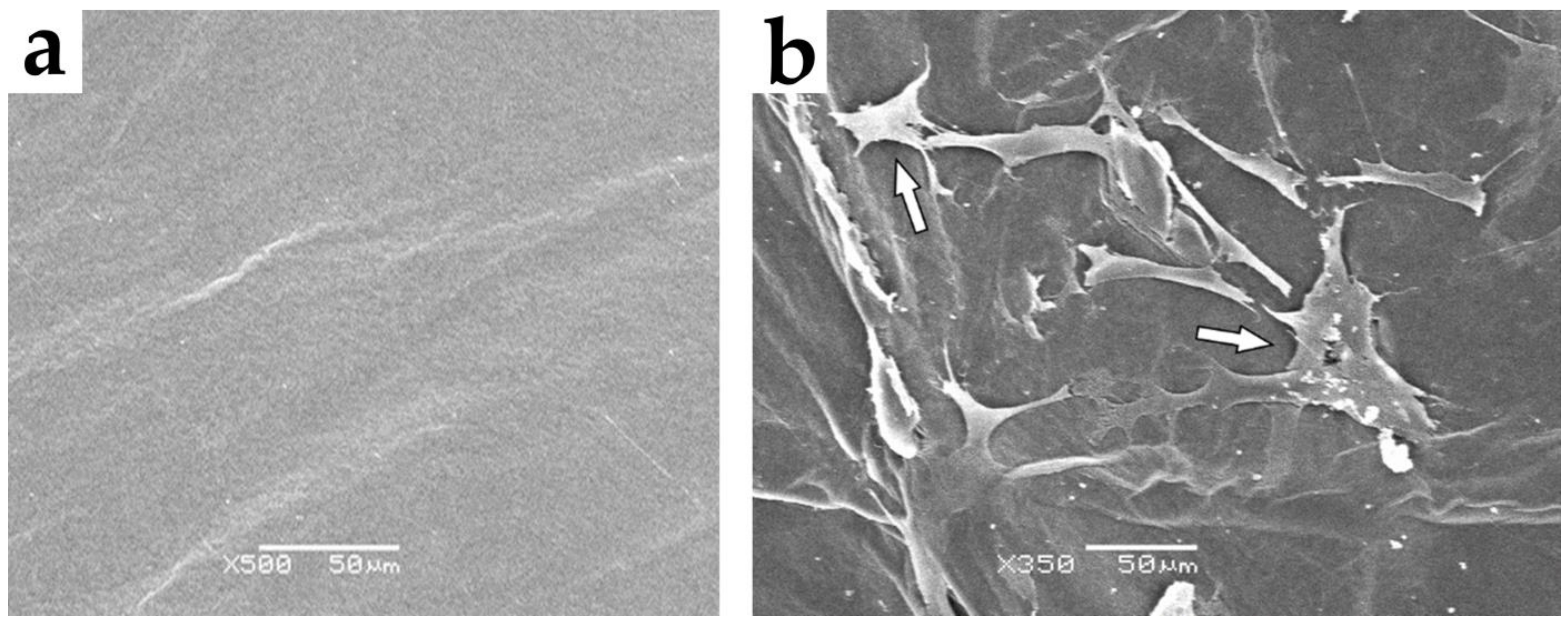
2.10. Scanning Electron Microscopy (SEM) Analysis
2.11. Statistical Analysis
3. Results
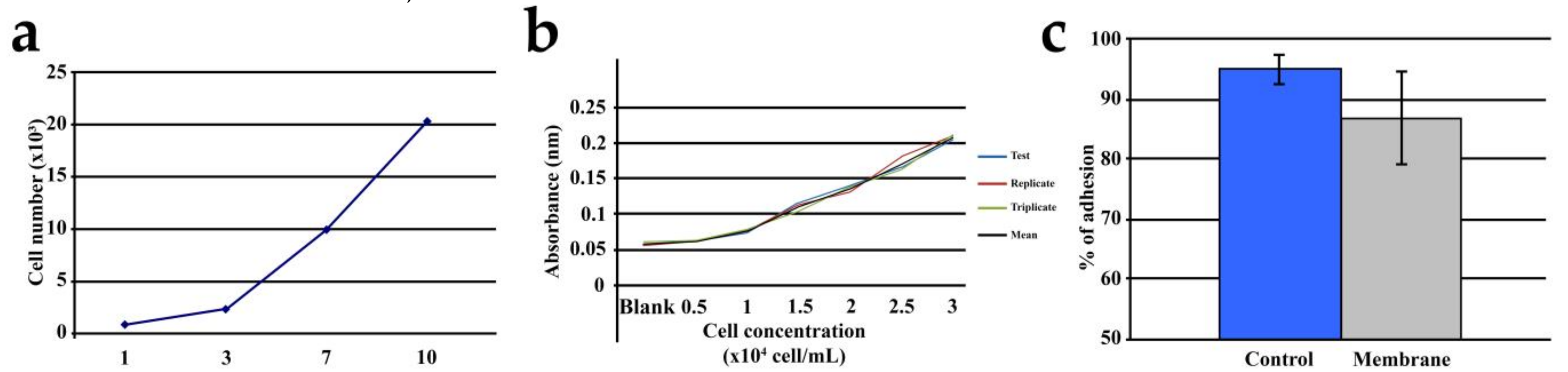
3.1. Cell Adhesion and Proliferation
3.2. Echocardiographic Findings
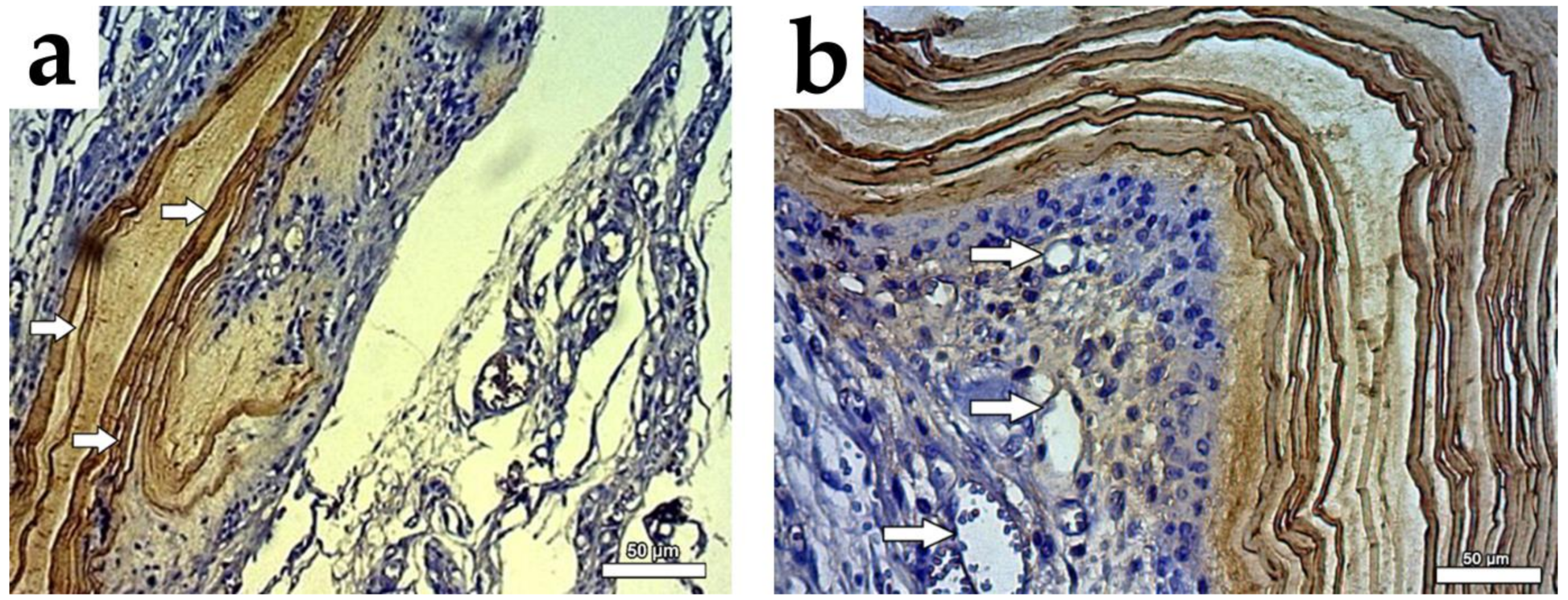
3.3. Histopathological Findings
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cunningham, J.W.; Vaduganathan, M.; Claggett, B.L.; John, J.E.; Desai, A.S.; Lewis, E.F.; Zile, M.R.; Carson, P.; Jhund, P.S.; Kober, L.; et al. Myocardial Infarction in Heart Failure With Preserved Ejection Fraction: Pooled Analysis of 3 Clinical Trials. JACC Hear. Fail. 2020, 8, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, D.W.; Jacobsen, S.J.; Rodeheffer, R.J.; Burnett, J.C., Jr.; Redfield, M.M.; Bailey, K.R. Burden of Systolic and Diastolic Ventricular Dysfunction in the Community. JAMA 2003, 289, 194. [Google Scholar]
- Pfeffer, M.A.; Braunwald, E. Ventricular remodeling after myocardial infarction: Experimental observations and clinical implications. Circulation 1990, 81, 1161–1172. [Google Scholar] [CrossRef]
- Abdelwahid, E.; Kalvelyte, A.; Stulpinas, A.; De Carvalho, K.A.T.; Guarita-Souza, L.C.; Foldes, G. Stem cell death and survival in heart regeneration and repair. Apoptosis 2016, 21, 252–268. [Google Scholar] [CrossRef]
- Granero-Molto, F.; Weis, J.A.; Longobardi, L.; Spagnoli, A. Role of mesenchymal stem cells in regenerative medicine: Application to bone and cartilage repair. Expert Opin. Biol. Ther. 2008, 8, 255–268. [Google Scholar] [CrossRef]
- Melchels, F.P.W.; Tonnarelli, B.; Olivares, A.L.; Martin, I.; Lacroix, D.; Feijen, J.; Wendt, D.J.; Grijpma, D.W. The influence of the scaffold design on the distribution of adhering cells after perfusion cell seeding. Biomaterials 2011, 32, 2878–2884. [Google Scholar] [CrossRef]
- Su, G.; Zhao, Y.; Wei, J.; Han, J.; Chen, L.; Xiao, Z.; Chen, B.; Dai, J. The effect of forced growth of cells into 3D spheres using low attachment surfaces on the acquisition of stemness properties. Biomaterials 2013, 34, 3215–3222. [Google Scholar] [CrossRef] [PubMed]
- Chen, R. A paradigm shift in biomass technology from complete to partial cellulose hydrolysis: Lessons learned from nature. Bioengineered 2015, 6, 69–72. [Google Scholar] [CrossRef]
- Ross, P.; Mayer, R.; Benziman, A.N.D.M. Cellulose biosynthesis and function in bacteria positive control. Microbiol. Rev. 1991, 55, 35–58. [Google Scholar] [CrossRef]
- Svensson, A.; Nicklasson, E.; Harrah, T.; Panilaitis, B.; Kaplan, D.L.; Brittberg, M.; Gatenholm, P. Bacterial cellulose as a potential scaffold for tissue engineering of cartilage. Biomaterials 2005, 26, 419–431. [Google Scholar] [CrossRef] [PubMed]
- Tabata, Y. Biomaterial technology for tissue engineering applications. J. R. Soc. Interface 2009, 6. [Google Scholar] [CrossRef] [PubMed]
- Frazier, T.; Alarcon, A.; Wu, X.; Mohiuddin, O.A.; Motherwell, J.M.; Carlsson, A.H.; Christy, R.J.; Edwards, J.V.; Mackin, R.T.; Prevost, N.; et al. Clinical translational potential in skin wound regeneration for adipose-derived, blood-derived, and cellulose materials: Cells, exosomes, and hydrogels. Biomolecules 2020, 10, 1373. [Google Scholar] [CrossRef] [PubMed]
- Feil, G.; Horres, R.; Schulte, J.; Mack, A.F.; Petzoldt, S.; Arnold, C.; Meng, C.; Jost, L.; Boxleitner, J.; Kiessling-Wolf, N.; et al. Bacterial cellulose shifts transcriptome and proteome of cultured endothelial cells towards native differentiation. Mol. Cell. Proteomics 2017, 16, 1563–1577. [Google Scholar] [CrossRef]
- Fengel, D.; Wegner, G. Wood Chemistry, Ultrastructure, Reactions; de Gruyter: Berlin, Germany; New York, NY, USA, 1989; ISBN 3110120593. [Google Scholar]
- Shafizadeh, F. Wood chemistry: Fundamentals and applications. Carbohydr. Res. 1983, 111, c24–c25. [Google Scholar] [CrossRef]
- Solomons, T.W.G.; Fryhle, C.B.; Snyder, S.A. Carbohydrates. In Organic Chemistry, 2nd ed.; John Wiley: Hoboken, NY, USA, 1996; ISBN 978-1119248972. [Google Scholar]
- Klemm, D.; Heublein, B.; Fink, H.P.; Bohn, A. Cellulose: Fascinating biopolymer and sustainable raw material. Angew. Chem. Int. Ed. 2005, 44, 3358–3393. [Google Scholar] [CrossRef]
- Zugenmaier, P. Conformation and packing of various crystalline cellulose fibers. Prog. Polym. Sci. 2001, 26, 1341–1417. [Google Scholar] [CrossRef]
- George, J.; Ramana, K.V.; Bawa, A.S. Siddaramaiah Bacterial cellulose nanocrystals exhibiting high thermal stability and their polymer nanocomposites. Int. J. Biol. Macromol. 2011, 48, 50–57. [Google Scholar] [CrossRef]
- Koizumi, S.; Yue, Z.; Tomita, Y.; Kondo, T.; Iwase, H.; Yamaguchi, D.; Hashimoto, T. Bacterium organizes hierarchical amorphous structure in microbial cellulose. Eur. Phys. J. E 2008, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Klemm, D.; Schumann, D.; Udhardt, U.; Marsch, S. Bacterial synthesized cellulose - Artificial blood vessels for microsurgery. Prog. Polym. Sci. 2001, 26, 1561–1603. [Google Scholar] [CrossRef]
- Fontana, J.D.; De Souza, A.M.; Fontana, C.K.; Torriani, I.L.; Moreschi, J.C.; Gallotti, B.J.; De Souza, S.J.; Narcisco, G.P.; Bichara, J.A.; Farah, L.F.X. Acetobacter cellulose pellicle as a temporary skin substitute. Appl. Biochem. Biotechnol. 1990, 24–25, 253–264. [Google Scholar] [CrossRef]
- Dugan, J.M.; Gough, J.E.; Eichhorn, S.J. Bacterial cellulose scaffolds and cellulose nanowhiskers for tissue engineering. Nanomedicine 2013, 8, 287–298. [Google Scholar] [CrossRef]
- Yang, F.; Murugan, R.; Wang, S.; Ramakrishna, S. Electrospinning of nano/micro scale poly(l-lactic acid) aligned fibers and their potential in neural tissue engineering. Biomaterials 2005, 26, 2603–2610. [Google Scholar] [CrossRef] [PubMed]
- Seidi, A.; Ramalingam, M.; Elloumi-Hannachi, I.; Ostrovidov, S.; Khademhosseini, A. Gradient biomaterials for soft-to-hard interface tissue engineering. Acta Biomater. 2011, 7, 1441–1451. [Google Scholar] [CrossRef]
- Atyabi, S.M.; Sharifi, F.; Irani, S.; Zandi, M.; Mivehchi, H.; Nagheh, Z. Cell Attachment and Viability Study of PCL Nano-fiber Modified by Cold Atmospheric Plasma. Cell Biochem. Biophys. 2016, 74, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Ziaei Amiri, F.; Pashandi, Z.; Lotfibakhshaiesh, N.; Mirzaie Parsa, M.J.; Ghanbari, H.; Faridi-Majidi, R. Cell attachment effects of collagen nanoparticles on crosslinked electrospun nanofibers. Int. J. Artif. Organs 2020. [Google Scholar] [CrossRef] [PubMed]
- Rajwade, J.M.; Paknikar, K.M.; Kumbhar, J.V. Applications of bacterial cellulose and its composites in biomedicine. Appl. Microbiol. Biotechnol. 2015, 99, 2491–2511. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Cui, A.; Li, J.; Gu, C. Folding 2D Structures into 3D Configurations at the Micro/Nanoscale: Principles, Techniques, and Applications. Adv. Mater. 2019, 31, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Ortega, Z.; Alemán, M.E.; Donate, R. Nanofibers and Microfibers for Osteochondral Tissue Engineering. Adv. Exp. Med. Biol. 2018, 1058, 97–123. [Google Scholar] [CrossRef] [PubMed]
- Baggio Simeoni, R.; Cesar Francisco, J.; Cunha, R.; André Cardoso, M.; Athayde T Carvalho, K.; Guarita–Souza, L.C. Co-cultivated cells integration into bacterial cellulose scaffold as a new device for tissue regeneration. Front. Nanosci. Nanotechnol. 2016, 2, 1–2. [Google Scholar] [CrossRef]
- Wang, B.; Lv, X.; Chen, S.; Li, Z.; Yao, J.; Peng, X.; Feng, C.; Xu, Y.; Wang, H. Use of heparinized bacterial cellulose based scaffold for improving angiogenesis in tissue regeneration. Carbohydr. Polym. 2018, 181, 948–956. [Google Scholar] [CrossRef]
- Souza, C.M.C.O.; Mesquita, L.A.F.; Souza, D.; Irioda, A.C.; Francisco, J.C.; Souza, C.F.; Guarita-Souza, L.C.; Sierakowski, M.R.; Carvalho, K.A.T. Regeneration of skin tissue promoted by mesenchymal stem cells seeded in nanostructured membrane. Transplant. Proc. 2014, 46, 1882–1886. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, K.A.T.; Guarita-Souza, L.C.; Hansen, P.; Rebelatto, C.L.K.; Senegaglia, A.C.; Miyague, N.; Olandoski, M.; Francisco, J.C.; Furuta, M.; Gremski, W. Cell Transplantation After The Coculture of Skeletal Myoblasts and Mesenchymal Stem Cells in the Regeneration of the Myocardium Scar: An Experimental Study in Rats. Transplant. Proc. 2006, 38, 1596–1602. [Google Scholar] [CrossRef] [PubMed]
- Schussler, O.; Chachques, J.C.; Mesana, T.G.; Suuronen, E.J.; Lecarpentier, Y.; Ruel, M. 3-Dimensional Structures To Enhance Cell Therapy and Engineer Contractile Tissue. Asian Cardiovasc. Thorac. Ann. 2010, 18, 188–198. [Google Scholar] [CrossRef]
- Kilkenny, C.; Browne, W.J.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Improving bioscience research reporting: The arrive guidelines for reporting animal research. Animals 2013, 4, 35–44. [Google Scholar] [CrossRef]
- Anversa, P.; Capasso, J.M.; Puntillo, E.; Sonnenblick, E.H.; Olivetti, G. Morphometric Analysis of the Infarcted Heart. Pathol. Res. Pract. 1989, 185, 544–550. [Google Scholar] [CrossRef]
- Rudski, L.G.; Lai, W.W.; Afilalo, J.; Hua, L.; Handschumacher, M.D.; Chandrasekaran, K.; Solomon, S.D.; Louie, E.K.; Schiller, N.B. Guidelines for the Echocardiographic Assessment of the Right Heart in Adults: A Report from the American Society of Echocardiography. Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J. Am. Soc. Echocardiogr. 2010, 23, 685–713. [Google Scholar] [CrossRef]
- Delaporte, C.; Fardeau, M. [The effect of serum from a patient with myeloma and diffuse muscular hypertrophy on the growth of human muscle cells in culture]. C. R. Acad. Sci. III 1984, 298, 49–54. [Google Scholar] [PubMed]
- Carvalho, K.A.T.; Guarita-Souza, L.C.; Rebelatto, C.L.K.; Senegaglia, A.C.; Hansen, P.; Mendonça, J.G.R.; Cury, C.C.; Francisco, J.C.; Brofman, P.R.S. Could the coculture of skeletal myoblasts and mesenchymal stem cells be a solution for postinfarction myocardial scar? Transplant. Proc. 2004, 36, 991–992. [Google Scholar] [CrossRef] [PubMed]
- Dominici, M.; Le Blanc, K.; Mueller, I.; Slaper-Cortenbach, I.; Marini, F.C.; Krause, D.S.; Deans, R.J.; Keating, A.; Prockop, D.J.; Horwitz, E.M. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 2006, 8, 315–317. [Google Scholar] [CrossRef]
- Moniri, M.; Moghaddam, A.B.; Azizi, S.; Rahim, R.A.; Zuhainis, S.W.; Navaderi, M.; Mohamad, R. In vitro molecular study of wound healing using biosynthesized bacteria nanocellulose/ silver nanocomposite assisted by bioinformatics databases. Int. J. Nanomedicine 2018, 13, 5097–5112. [Google Scholar] [CrossRef]
- Koike, T.; Sha, J.; Bai, Y.; Matsuda, Y.; Hideshima, K.; Yamada, T.; Kanno, T. Efficacy of bacterial cellulose as a carrier of BMP-2 for bone regeneration in a rabbit frontal sinus model. Materials (Basel) 2019, 12. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.; Chen, M.; Liang, S.; Acha, V.; Liu, D.; Yuan, F.; Hawks, C.L.; Hornsby, P.J. Improving cell therapy-experiments using transplanted telomerase-immortalized cells in immunodeficient mice. Mech. Ageing Dev. 2007, 128, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Donndorf, P.; Kundt, G.; Kaminski, A.; Yerebakan, C.; Liebold, A.; Steinhoff, G.; Glass, A. Intramyocardial bone marrow stem cell transplantation during coronary artery bypass surgery: A meta-analysis. J. Thorac. Cardiovasc. Surg. 2011, 142, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, W.H.; Melnychenko, I.; Wasmeier, G.; Didié, M.; Naito, H.; Nixdorff, U.; Hess, A.; Budinsky, L.; Brune, K.; Michaelis, B.; et al. Engineered heart tissue grafts improve systolic and diastolic function in infarcted rat hearts. Nat. Med. 2006, 12, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, W.; Eschenhagen, T. Cardiac Tissue Engineering for Replacement Therapy. Heart Fail. Rev. 2003, 8, 259–269. [Google Scholar] [CrossRef]
- Langer, R. Tissue Engineering. Mol. Ther. 2000, 1, 12–15. [Google Scholar] [CrossRef]
- Francisco, J.C.; Correa Cunha, R.; Cardoso, M.A.; Baggio Simeoni, R.; Mogharbel, B.F.; Picharski, G.L.; Silva Moreira Dziedzic, D.; Guarita-Souza, L.C.; Carvalho, K.A.T. Decellularized Amniotic Membrane Scaffold as a Pericardial Substitute: An In Vivo Study. Transplant. Proc. 2016, 48, 2845–2849. [Google Scholar] [CrossRef]
- Abdelwahid, E.; Siminiak, T.; Cesar Guarita-Souza, L.; Athayde Teixeira de Carvalho, K.; Gallo, P.; Shim, W.; Condorelli, G. Stem Cell Therapy in Heart Diseases: A Review of Selected New Perspectives, Practical Considerations and Clinical Applications. Curr. Cardiol. Rev. 2011, 7, 201–212. [Google Scholar] [CrossRef]
- Menasché, P.; Hagège, A.; Scorsin, M.; Pouzet, B.; Desnos, M.; Duboc, D.; Schwartz, K.; Vilquin, J.T.; Marolleau, J.P. [Autologous skeletal myoblast transplantation for cardiac insufficiency. First clinical case]. Arch. Mal. Coeur Vaiss. 2001, 94, 180–182. [Google Scholar]
- Siu, C.W.; Liao, S.Y.; Liu, Y.; Lian, Q.; Tse, H.F. Stem cells for myocardial repair. Thromb. Haemost. 2010, 104, 6–12. [Google Scholar] [CrossRef]
- Tamaki, T.; Uchiyama, Y.; Okada, Y.; Tono, K.; Masuda, M.; Nitta, M.; Hoshi, A.; Akatsuka, A. Clonal differentiation of skeletal muscle-derived CD34-/45 - stem cells into cardiomyocytes in vivo. Stem Cells Dev. 2010, 19, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Hagège, A.A.; Marolleau, J.P.; Vilquin, J.T.; Alhéritière, A.; Peyrard, S.; Duboc, D.; Abergel, E.; Messas, E.; Mousseaux, E.; Schwartz, K.; et al. Skeletal myoblast transplantation in ischemic heart failure: Long-term follow-up of the first phase I cohort of patients. Circulation 2006, 114. [Google Scholar] [CrossRef] [PubMed]
- Cortes-Morichetti, M.; Frati, G.; Schussler, O.; Van Huyen, J.P.D.; Lauret, E.; Genovese, J.A.; Carpentier, A.F.; Chachques, J.C. Association between a cell-seeded collagen matrix and cellular cardiomyoplasty for myocardial support and regeneration. Tissue Eng. 2007, 13, 2681–2687. [Google Scholar] [CrossRef]
- Soler-Botija, C.; Bagó, J.R.; Llucià-Valldeperas, A.; Vallés-Lluch, A.; Castells-Sala, C.; Martínez-Ramos, C.; Fernández-Muiños, T.; Chachques, J.C.; Pradas, M.M.P.; Semino, C.E.; et al. Engineered 3D bioimplants using elastomeric scaffold, self-assembling peptide hydrogel, and adipose tissue-derived progenitor cells for cardiac regeneration. Am. J. Transl. Res. 2014, 6, 291–301. [Google Scholar]
- Zhang, R.; Mägel, L.; Jonigk, D.; Länger, F.; Lippmann, T.; Zardo, P.; Pölzing, F. Biosynthetic Nanostructured Cellulose Patch for Chest Wall Reconstruction: Five-Month Follow-up in a Porcine Model. J. Investig. Surg. 2017, 30, 297–302. [Google Scholar] [CrossRef] [PubMed]


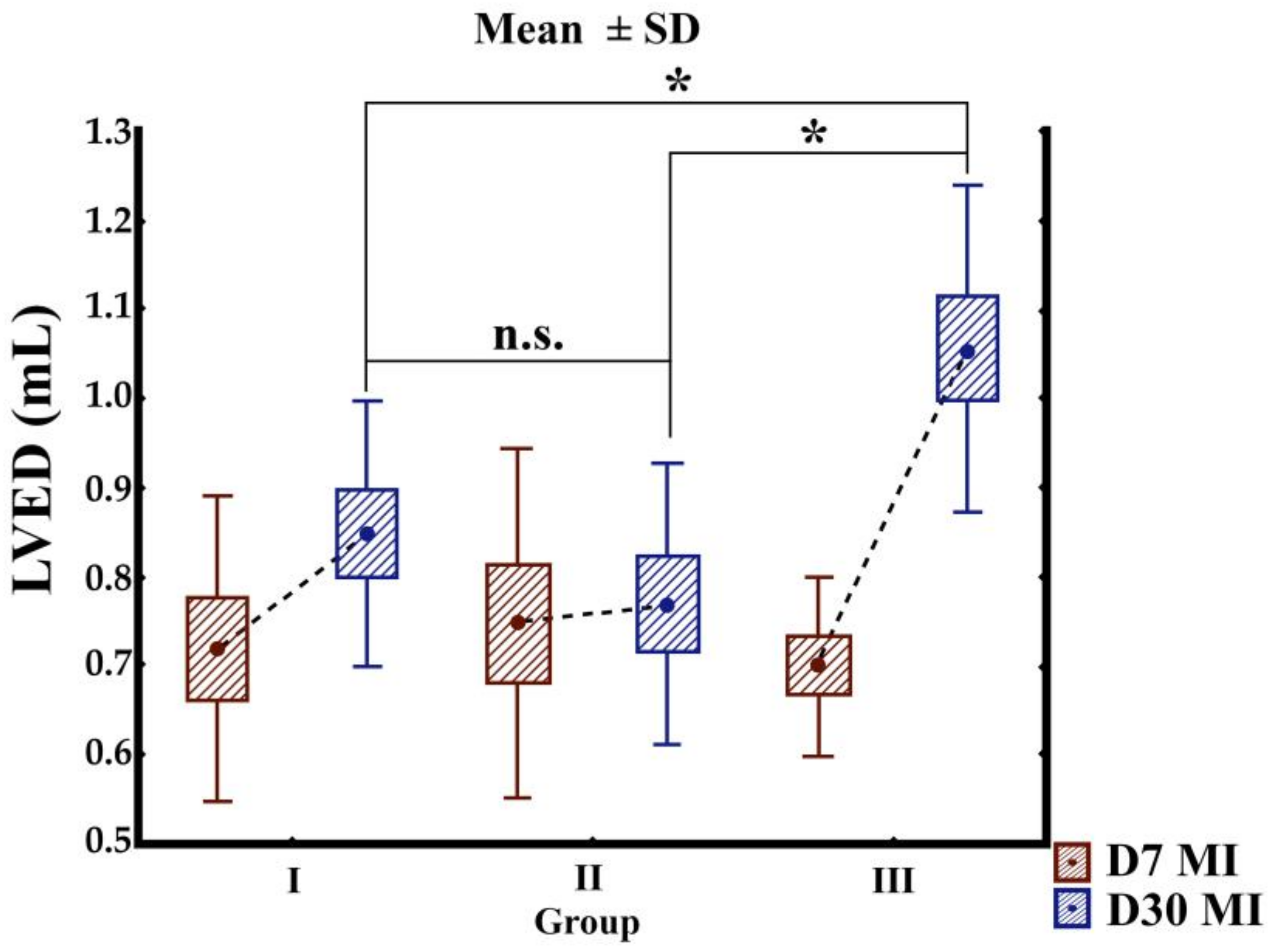
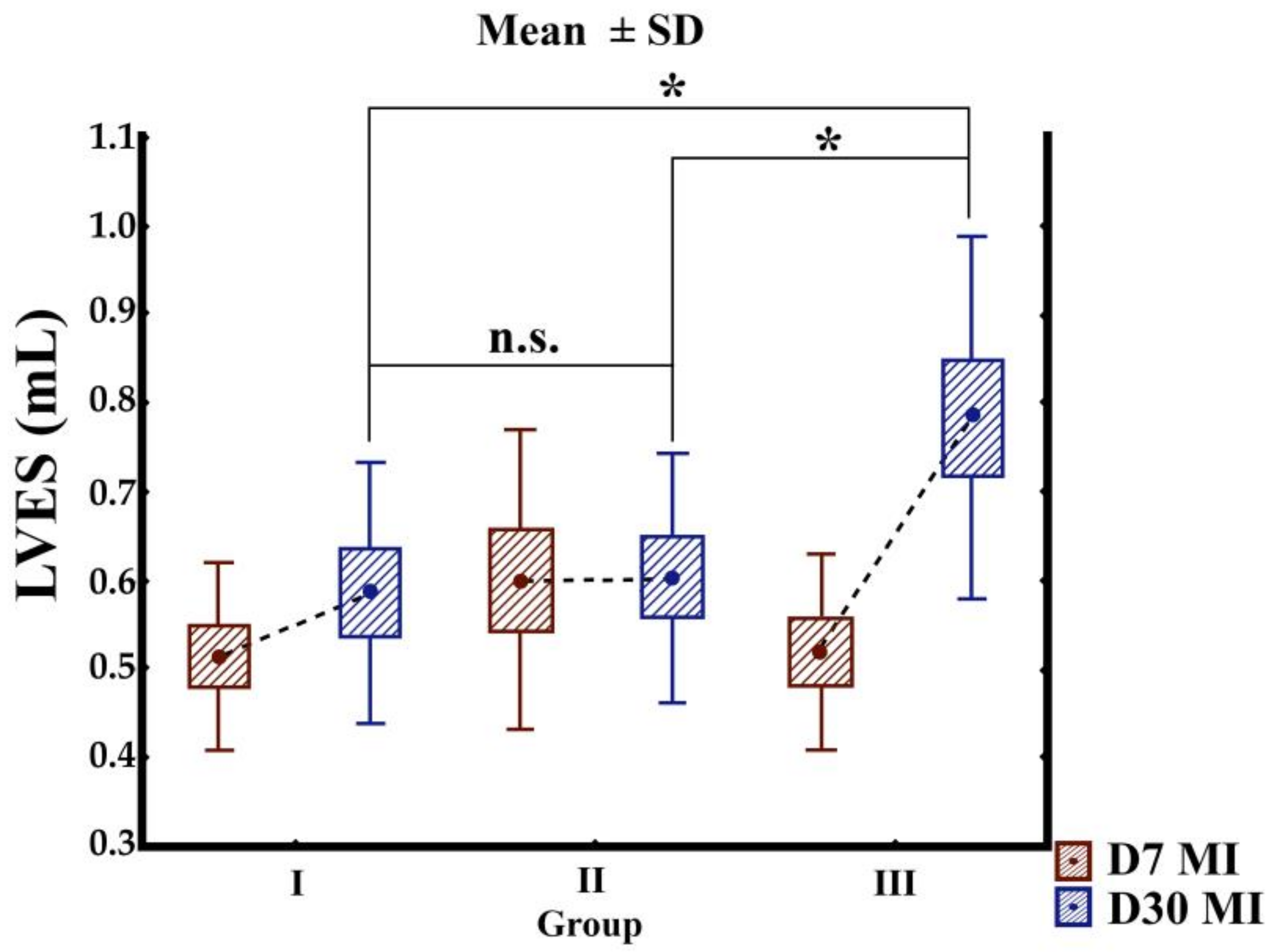
| Variable | Group | D7 | D30 | p-Value (D7 vs. D30) |
|---|---|---|---|---|
| LVEF (%) | I | 28.21 ± 5.07 | 32.72 ± 8.62 | 0.316 |
| II | 22.79 ± 5.80 | 26.74 ± 4.92 | 0.065 | |
| III | 27.37 ± 8.40 | 27.92 ± 9.77 | 0.865 | |
| LVES (mL) | I | 0.509 ± 0.106 | 0.582 ± 0.149 | 0.241 |
| II | 0.596 ± 0.171 | 0.598 ± 0.141 | 0.982 | |
| III | 0.514 ± 0.112 | 0.780 ± 0.206 | 0.001 * | |
| LVED(mL) | I | 0.718 ± 0.170 | 0.848 ± 0.149 | 0.326 |
| II | 0.747 ± 0.196 | 0.768 ± 0.158 | 0.043 | |
| III | 0.698 ± 0.102 | 1.056 ± 0.183 | 0.004 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simeoni, R.B.; Mogharbel, B.F.; Francisco, J.C.; Miyague, N.I.; Irioda, A.C.; Souza, C.M.C.O.; Souza, D.; Stricker, P.E.F.; da Rosa, N.N.; Souza, C.F.; et al. Beneficial Roles of Cellulose Patch-Mediated Cell Therapy in Myocardial Infarction: A Preclinical Study. Cells 2021, 10, 424. https://doi.org/10.3390/cells10020424
Simeoni RB, Mogharbel BF, Francisco JC, Miyague NI, Irioda AC, Souza CMCO, Souza D, Stricker PEF, da Rosa NN, Souza CF, et al. Beneficial Roles of Cellulose Patch-Mediated Cell Therapy in Myocardial Infarction: A Preclinical Study. Cells. 2021; 10(2):424. https://doi.org/10.3390/cells10020424
Chicago/Turabian StyleSimeoni, Rossana B., Bassam F. Mogharbel, Julio C. Francisco, Nelson I. Miyague, Ana C. Irioda, Carolina M. C. O. Souza, Daiany Souza, Priscila E. Ferreira Stricker, Nádia Nascimento da Rosa, Clayton F. Souza, and et al. 2021. "Beneficial Roles of Cellulose Patch-Mediated Cell Therapy in Myocardial Infarction: A Preclinical Study" Cells 10, no. 2: 424. https://doi.org/10.3390/cells10020424
APA StyleSimeoni, R. B., Mogharbel, B. F., Francisco, J. C., Miyague, N. I., Irioda, A. C., Souza, C. M. C. O., Souza, D., Stricker, P. E. F., da Rosa, N. N., Souza, C. F., Franco, C. R. C., Sierakowski, M.-R., Abdelwahid, E., Guarita-Souza, L. C., & Carvalho, K. A. T. (2021). Beneficial Roles of Cellulose Patch-Mediated Cell Therapy in Myocardial Infarction: A Preclinical Study. Cells, 10(2), 424. https://doi.org/10.3390/cells10020424







