Ice Control during Cryopreservation of Heart Valves and Maintenance of Post-Warming Cell Viability
Abstract
:1. Introduction
2. Materials and Methods
2.1. Tissue Procurement and Preparation
2.2. Cryopreservation Solution Preparation
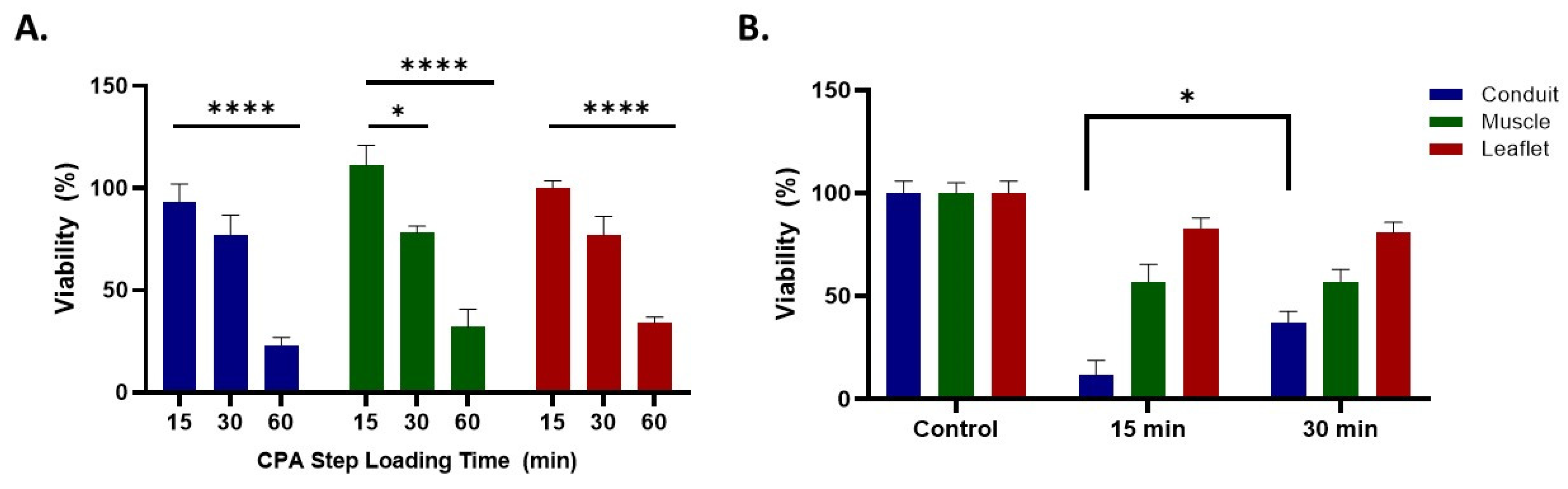
2.3. Cryoprotectant (CPA) Formulations Used for Vitrification
2.4. CPA Addition and Removal
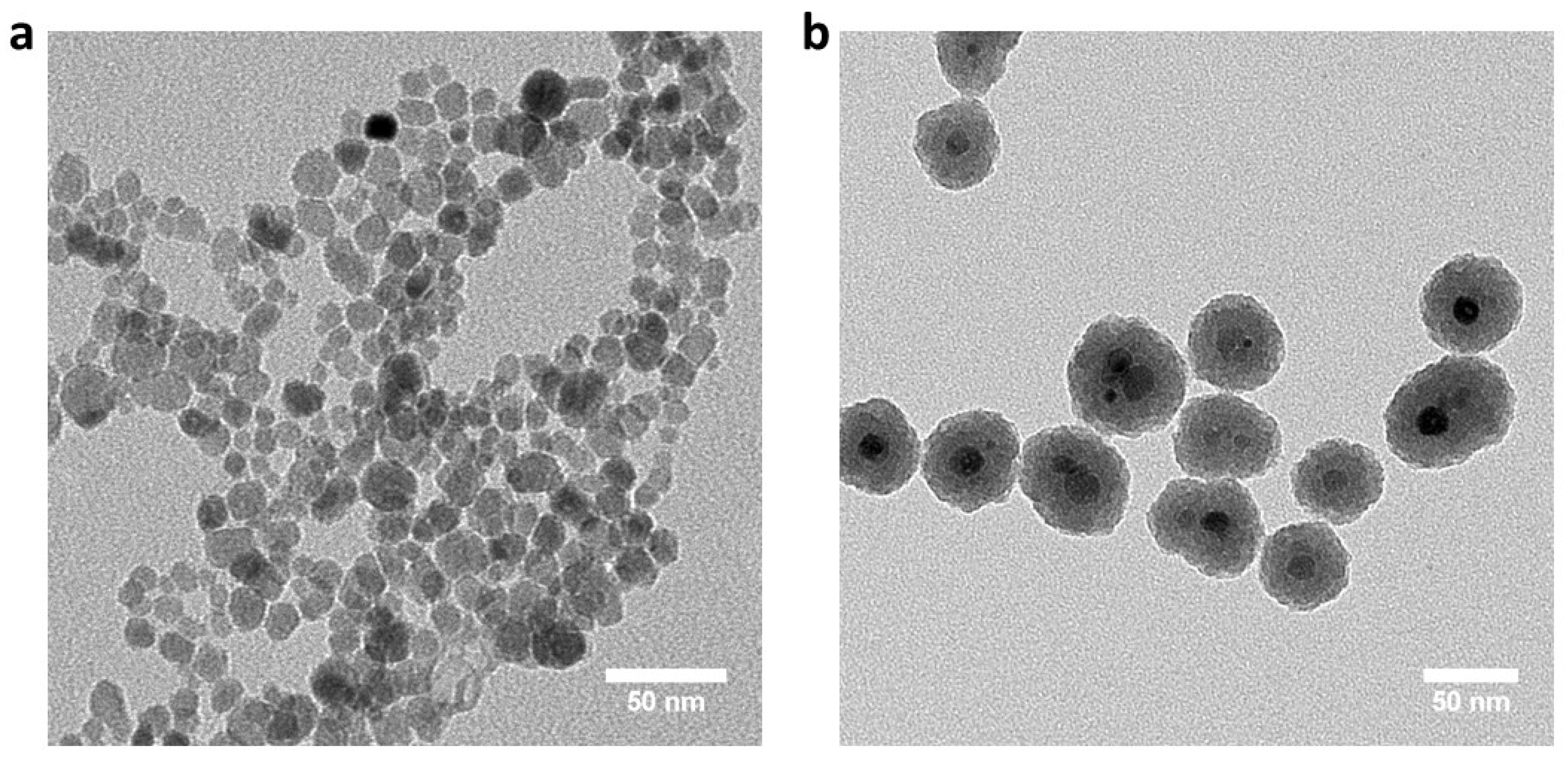
2.5. Silica-Coated Iron Oxide Nanoparticles (Coated mNPs) Synthesis
2.6. CPA Exposure Toxicity on Aortic Heart Valves
2.7. Cooling Steps and Storage
2.8. Convection Warming
2.9. Nanowarming
2.10. Post Warming Treatment
2.11. Viability Assessment
2.12. Statistical Methods
3. Results and Discussion
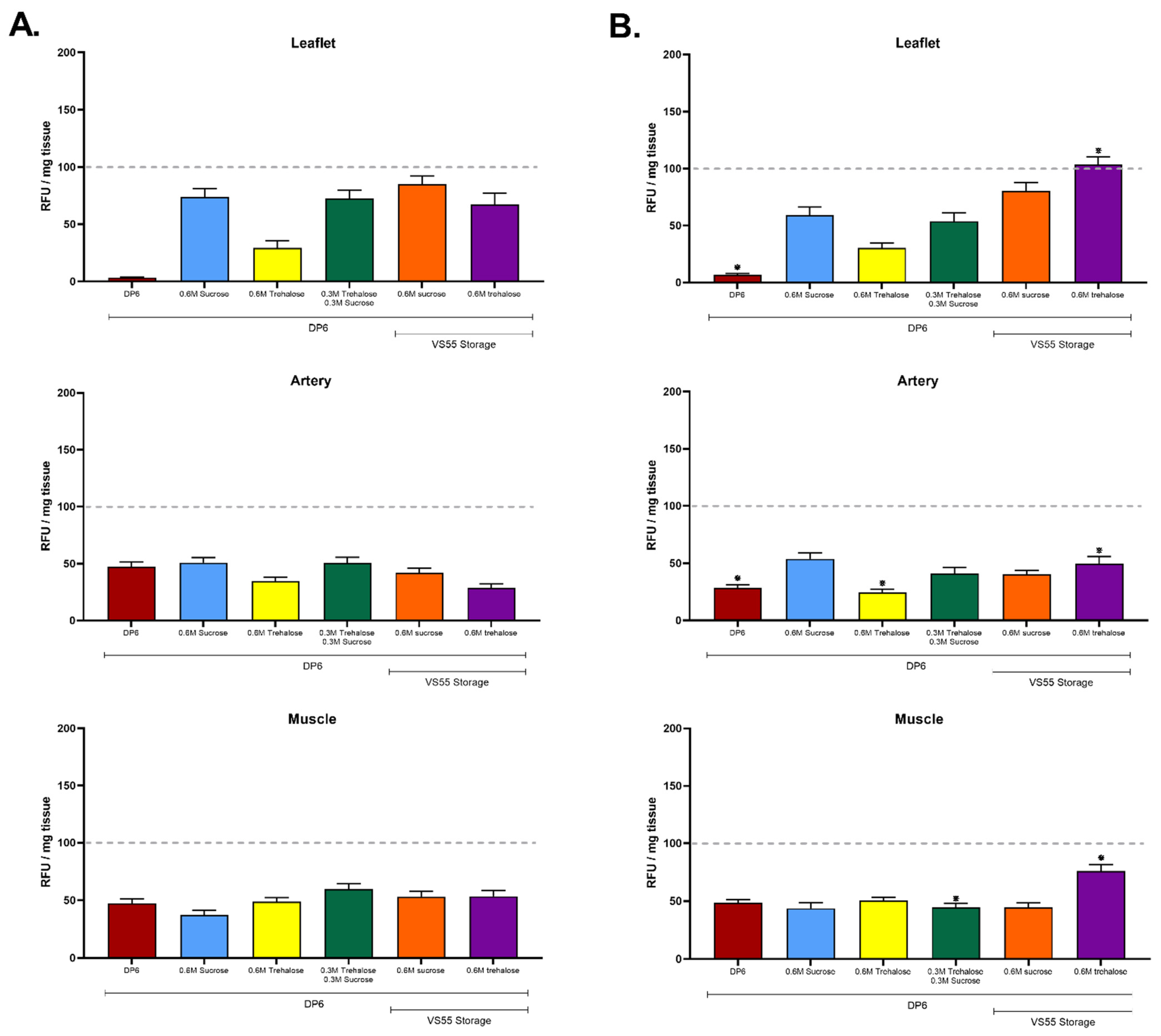
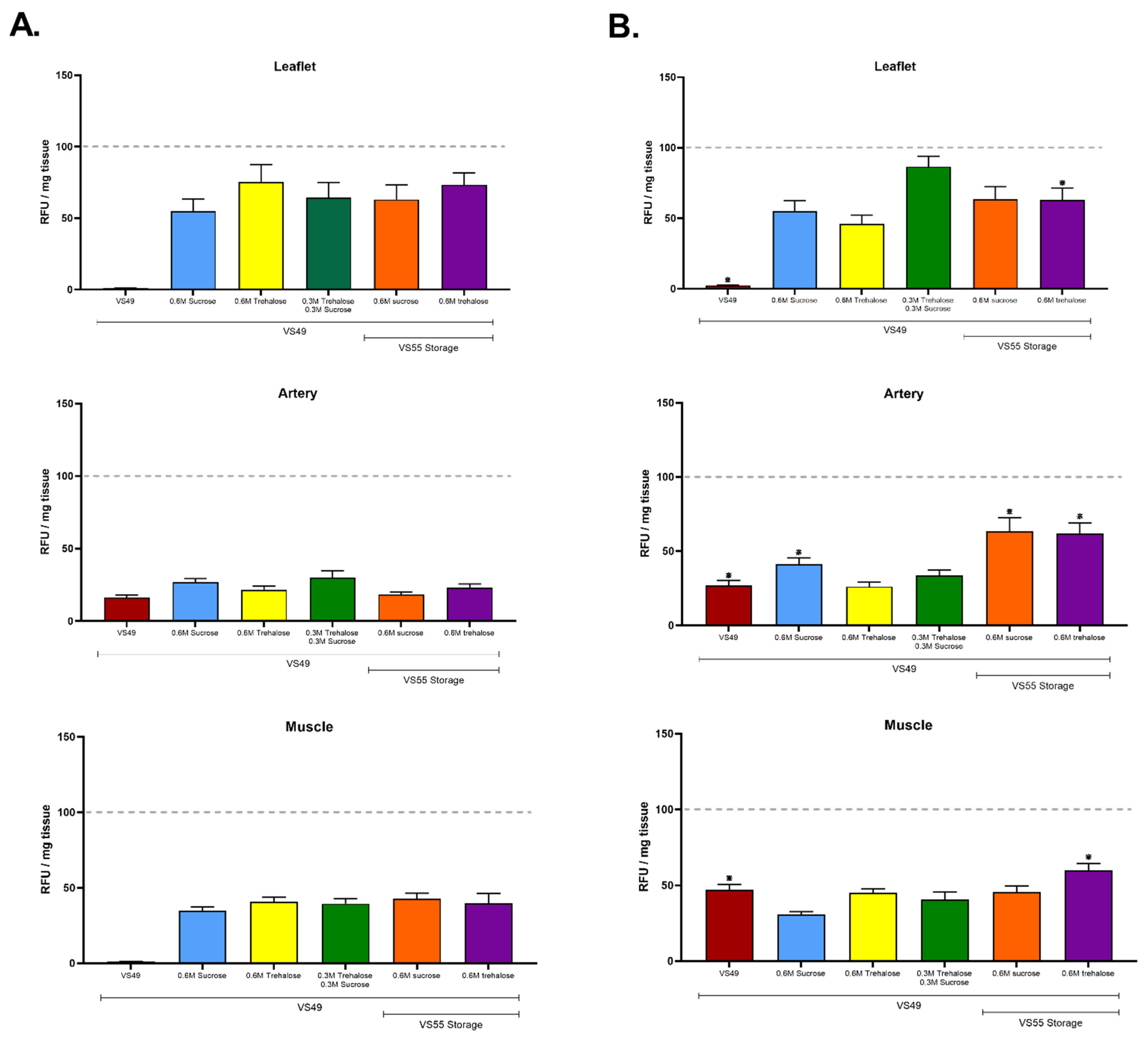
3.1. The First Group of Experiments Evaluated the Hypothesis That a Combination of Disaccharides and Nanowarming Will Permit an Overall Reduction in Cryoprotectants
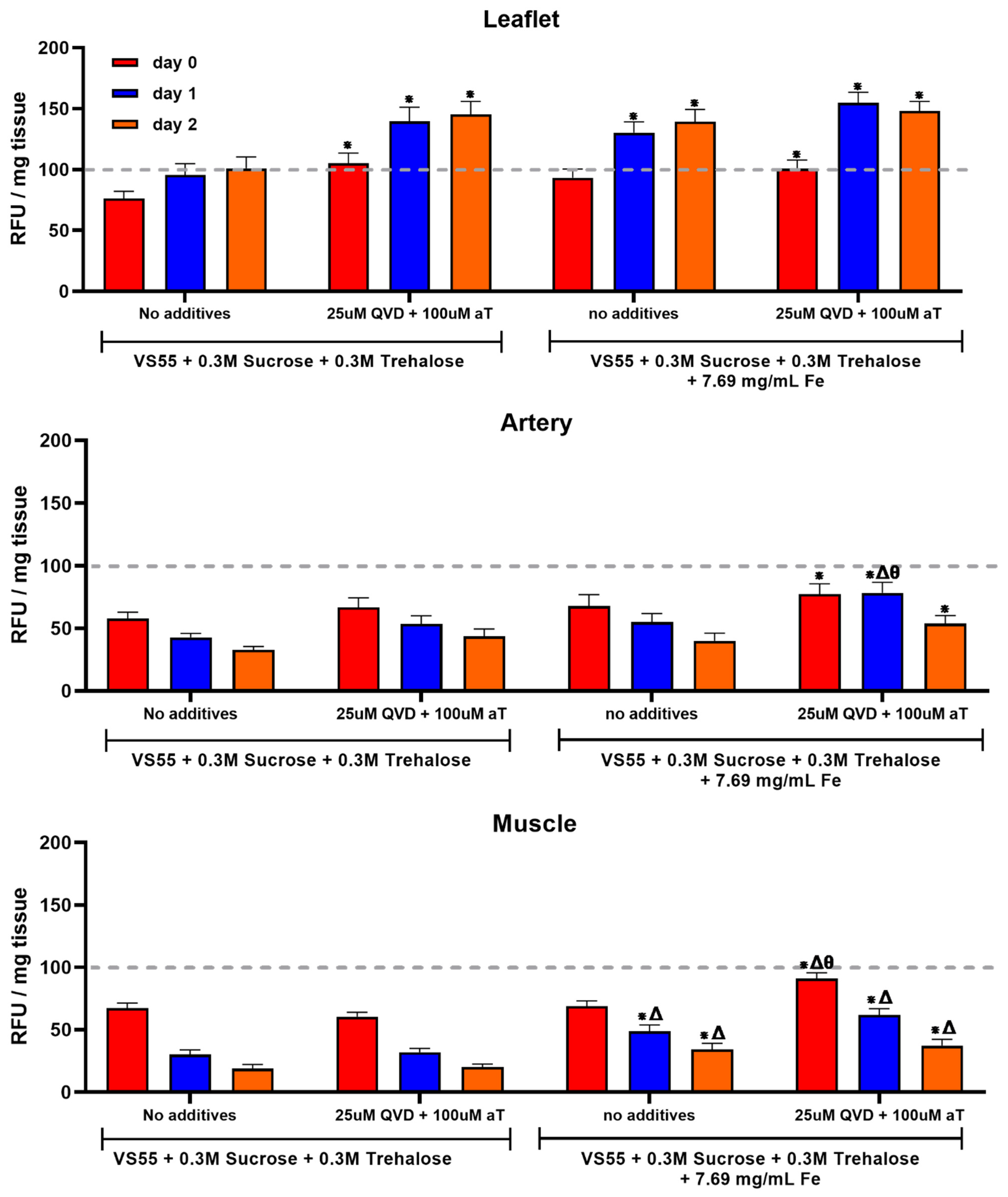
3.2. The Second Series of Experiments Examined the Hypothesis That Post-Warming Treatment of Ice-Free Vitrified Heart Valve Tissues Will Improve Cell Viability
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lewis, J.K.; Bischof, J.C.; Braslavsky, I.; Brockbank, K.G.M.; Fahy, G.M.; Fuller, B.J.; Rabin, Y.; Tocchio, A.; Woods, E.J.; Wowk, B.G.; et al. The Grand Challenges of Organ Banking: Proceedings from the first global summit on complex tissue cryopreservation. Cryobiology 2016, 72, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Giwa, S.; Lewis, J.K.; Alvarez, L.; Langer, R.; Roth, A.E.; Church, G.M.; Markmann, J.F.; Sachs, D.H.; Chandraker, A.; Wertheim, J.A.; et al. The promise of organ and tissue preservation to transform medicine. Nat. Biotechnol. 2017, 35, 530–542. [Google Scholar] [CrossRef] [PubMed]
- Mazur, P. Freezing of living cells: Mechanisms and implications. Am. J. Physiol.-Cell Physiol. 1984, 247, C125–C142. [Google Scholar] [CrossRef] [PubMed]
- Luyet, B.J. The vitrification of organic colloids and of protoplasm. Biodynamica 1937, 1, 1–14. [Google Scholar]
- Rall, W.F.; Fahy, G.M. Ice-free cryopreservation of mouse embryos at −196 degrees C by vitrification. Nature 1985, 313, 573–575. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; Song, Y.C.; Brockbank, K.G.M. Vitrification in Tissue Preservation: New Developments. In Life in the Frozen State; Fuller, B., Lane, N., Benson, E., Eds.; CRC Press: Boca Raton, FL, USA, 2004; pp. 603–641. [Google Scholar] [CrossRef]
- Brockbank, K.G.M.; Chen, Z.; Greene, E.D.; Campbell, L.H. Ice-Free Cryopreservation by Vitrification. Mini Review. MOJ Cell Sci Rep. 2014, 1, 7. [Google Scholar] [CrossRef] [Green Version]
- Brockbank, K.G.M.; Chen, Z.; Greene, E.D.; Campbell, L.H. Vitrification of heart valve tissues. In Methods in Molecular Biology; Springer: New York, NY, USA, 2015; Volume 1257, pp. 399–421. [Google Scholar] [CrossRef] [PubMed]
- Fahy, G.M.; MacFarlane, D.R.; Angell, C.A.; Meryman, H.T. Vitrification as an approach to cryopreservation. Cryobiology 1984, 21, 407–426. [Google Scholar] [CrossRef] [PubMed]
- Fahy, G.M.; Wowk, B. Principles of Ice-Free Cryopreservation by Vitrification. In Methods in Molecular Biology; Humana: New York, NY, USA, 2021; Volume 2180, pp. 27–97. [Google Scholar] [CrossRef] [PubMed]
- Fahy, G.M. Vitrification: A New Approach to Organ Cryopreservation. Prog. Clin. Biol. Res. 1986, 224, 305–335. [Google Scholar] [PubMed]
- Song, Y.C.; Khirabadi, B.S.; Lightfoot, F.; Brockbank, K.G.M.; Taylor, M.J. Vitreous cryopreservation maintains the function of vascular grafts. Nat. Biotechnol. 2000, 18, 296–299. [Google Scholar] [CrossRef] [PubMed]
- Tucker, M.J.; Libermann, J. (Eds.) Vitrification in Assisted Reproduction, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2015; ISBN 9781482242577. [Google Scholar]
- Zeng, M.; Yang, Q.-R.; Fu, G.-B.; Zhang, Y.; Zhou, X.; Huang, W.; Zhang, H.; Li, W.; Wang, Z.; Yan, H.; et al. Maintaining viability and characteristics of cholangiocarcinoma tissue by vitrification-based cryopreservation. Cryobiology 2017, 78, 41–46. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.J.; Banik, P.D.; Nagpal, S.; Weng, L.; Ozer, S.; van Gulik, T.M.; Toner, M.; Tessier, S.N.; Uygun, K. Bulk Droplet Vitrification: An Approach to Improve Large-Scale Hepatocyte Cryopreservation Outcome. Langmuir 2019, 35, 7354–7363. [Google Scholar] [CrossRef] [PubMed]
- Fahy, G.M.; Wowk, B.; Pagotan, R.; Chang, A.; Phan, J.; Bruce, T.; Laura, P. Physical and biological aspects of renal vitrification. Organogenesis 2009, 5, 167–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fahy, G.M.; Saur, J.; Williams, R.J. Physical problems with the vitrification of large biological systems. Cryobiology 1990, 27, 492–510. [Google Scholar] [CrossRef] [PubMed]
- Wusteman, M.; Robinson, M.; Pegg, D. Vitrification of large tissues with dielectric warming: Biological problems and some approaches to their solution. Cryobiology 2004, 48, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Etheridge, M.L.; Bischof, J.C. Optimizing Magnetic Nanoparticle Based Thermal Therapies within the Physical Limits of Heating. Ann. Biomed. Eng. 2013, 41, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Etheridge, M. Understanding the Benefits and Limitations of Magnetic Nanoparticle Heating for Improved Applications in Cancer Hyperthermia and Biomaterial Cryopreservation. Ph.D. Dissertation, University of Minnesota, Minneapolis, MN, USA, 2014. [Google Scholar]
- Manuchehrabadi, N.; Gao, Z.; Zhang, J.; Ring, H.L.; Shao, Q.; Liu, F.; McDermott, M.; Fok, A.; Rabin, Y.; Brockbank, K.G.M.; et al. Improved Tissue Cryopreservation using Nanowarming: Inductive Heating of Magnetic Nanoparticles. Sci. Transl. Med. 2017, 9, eaah4586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phatak, S.; Natesan, H.; Choi, J.; Brockbank, K.G.M.; Bischof, J.C. Measurement of Specific Heat and Crystallization in VS55, DP6 and M22 Cryoprotectant Systems with and without Sucrose. Biopreserv. Biobank. 2018, 16, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Brockbank, K.G.M.; Chen, Z.; Greene, E.D.; Campbell, L.H. Vitrification of heart valve tissues. In Methods in Molecular Biology; Springer: New York, NY, USA, 2021; Volume 2180, pp. 593–605. [Google Scholar] [CrossRef] [PubMed]
- Brockbank, K.G.M.; Chen, Z.; Greene, E.D.; Campbell, L.H. Commentary: Advances in viable ice-free cryopreservation of heart valves. J. Nanomed. Nanotechnol. 2021, 12, 566. [Google Scholar]
- Huber, A.J.T.; Brockbank, K.G.M.; Riemann, I.; Schleicher, M.; Schenke-Layland, K.; Fritze, O.; Wendel, H.-P.; Stock, U.A. Preclinical Evaluation of Ice-free Cryopreserved Arteries: Structural Integrity and Hemocompatibility. Cells Tissues Organs 2012, 196, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Brockbank, K.G.M.; Chen, Z.; Song, Y.C. Vitrification of Porcine Articular Cartilage. Cryobiology 2010, 60, 217–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, Z.; Ring, H.L.; Sharma, A.; Namsrai, B.; Tran, N.; Finger, E.B.; Garwood, M.; Haynes, C.L.; Bischof, J.C. Preparation of Scalable Silica-Coated Iron Oxide Nanoparticles for Nanowarming. Adv. Sci. 2020, 7, 1901624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, J.; Wilson, I.; Orton, T.; Pognan, F. Investigation of the alamar blue (resazurin) fluorescent dye for the assessment of mammalian cell cytotoxicity. Eur. J. Biochem. 2000, 267, 5421–5426. [Google Scholar] [CrossRef] [PubMed]
- Burdette, E.C.; Karow, A.M. Kidney model for study of electromagnetic thawing. Cryobiology 1978, 15, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Burdette, E.C.; Wiggins, S.; Brown, R.; Karow, A.M. Microwave thawing of frozen kidneys: A theoretically based experimentally-effective design. Cryobiology 1980, 17, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, W.J.; Brezovich, I.A.; Chakraborty, D.P. Usable frequencies in hyperthermia with thermal seeds. IEEE Trans. Biomed. Eng. 1984, 31, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Marsland, T.P.; Evans, S.; Pegg, D.E. Dielectric measurements for the design of an electromagnetic rewarming system. Cryobiology 1987, 24, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Evans, S. Electromagnetic rewarming: The effect of CPA concentration and radio source frequency on uniformity and efficiency of heating. Cryobiology 2000, 40, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Yu, C.; He, L.; Lu, C.; Gao, D. Development of a single mode electromagnetic resonant cavity for rewarming of cryopreserved biomaterials. Cryobiology 2006, 53, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.P.; Pegg, D.E. Rapid electromagnetic warming of cells and tissues. IEEE Trans. Biomed. Eng. 1999, 46, 1413–1425. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.P.; Wusteman, M.C.; Wang, L.; Pegg, D.E. Electromagnetic re-warming of cryopreserved tissues: Effect of choice of cryoprotectant and sample shape on uniformity of heating. Phys. Med. Biol. 2002, 47, 2311–2325. [Google Scholar] [CrossRef] [PubMed]
- Wusteman, M.C.; Pegg, D.E.; Robinson, M.P.; Wang, L.-H.; Fitch, P. Vitrification media: Toxicity, permeability, and dielectric properties. Cryobiology 2002, 44, 24–37. [Google Scholar] [CrossRef] [PubMed]
- Brockbank, K.G.M.; Campbell, L.H. Ice-free preservation of large volume tissue samples for viable, functional tissue banking. US Patent No. 11,246,308, 15 February 2022. [Google Scholar]
- Brockbank, K.G.M.; Chen, Z.Z. Ice-free vitrification and nanowarming of large tissue samples. US Provisional Patent Filed November 2019. US-2021-0137099-A1, 13 May 2021. [Google Scholar]
- Han, Z.; Sharma, A.; Gao, Z.; Carlson, T.W.; O’Sullivan, M.G.; Finger, E.B.; Bischof, J.C. Diffusion Limited Cryopreservation of Tissue with Radiofrequency Heated Metal Forms. Adv. Healthc. Mater. 2020, 9, 2000796. [Google Scholar] [CrossRef] [PubMed]
- Best, B.P. Cryoprotectant Toxicity: Facts, Issues, and Questions. Rejuvenation Res. 2015, 18, 422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ampaw, A.; Charlton, T.A.; Briard, J.G.; Ben, R.N. Designing the next generation of cryoprotectants–From proteins to small molecules. Pept. Sci. 2018, 111, e24086. [Google Scholar] [CrossRef]
- Taylor, M.J.; Weegman, B.P.; Baicu, S.C.; Giwa, S.E. New Approaches to Cryopreservation of Cells, Tissues, and Organs. Transfus. Med. Hemother. 2019, 46, 197–215. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.J.; Tessier, S.N.; Banik, P.D.; SoNagpal, n.; Cronin, S.E.J.; Ozer, S.; Hafiz, E.O.A.; van Gulik, T.M.; Yarmush, M.L.; Markmann, J.F.; et al. Supercooling extends preservation time of human livers. Nat. Biotechnol. 2019, 37, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- de Vries, R.J.; Tessier, S.N.; Banik, P.D.; Nagpal, S.; Cronin, S.E.J.; Ozer, S.; Hafiz, E.O.A.; van Gulik, T.M.; Yarmush, M.L.; Markmann, J.F.; et al. Sub-zero non frozen preservation of human livers in the supercooled state. Nat. Protoc. 2020, 15, 2024–2040. [Google Scholar] [CrossRef] [PubMed]
- Fuller, B.J.; Petrenko, A.; Guibert, E. Human organs come out of the deep cold. Nat. Biotechnol. 2019, 37, 1127–1128. [Google Scholar] [CrossRef] [PubMed]
| VS49 | VS55 | DP6 | Units | |
|---|---|---|---|---|
| Component | Quantities | Quantities | Quantities | |
| 5X EuroCollins | 200 | 200 | 200 | mL |
| HEPES buffer | 2.39 | 2.39 | 2.39 | Grams |
| Propylene Glycol * | 150.011 | 168.38 | 228.27 | Grams |
| Formamide * | 124.34 | 139.56 | 0 | Grams |
| DMSO * | 215.72 | 242.14 | 234.39 | Grams |
| Water | To 1 L | To 1 L | To 1 L | mL |
| pH | 7.9–8.1 | 7.9–8.1 | 7.9–8.1 | Units |
| Osmolality ** | 400 ± 5 | 460 ± 5 | 325 ± 5 | mOsm |
| CPA Moles | 7.48 M | 8.4 M | 6 M |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brockbank, K.G.M.; Bischof, J.C.; Chen, Z.; Greene, E.D.; Gao, Z.; Campbell, L.H. Ice Control during Cryopreservation of Heart Valves and Maintenance of Post-Warming Cell Viability. Cells 2022, 11, 1856. https://doi.org/10.3390/cells11121856
Brockbank KGM, Bischof JC, Chen Z, Greene ED, Gao Z, Campbell LH. Ice Control during Cryopreservation of Heart Valves and Maintenance of Post-Warming Cell Viability. Cells. 2022; 11(12):1856. https://doi.org/10.3390/cells11121856
Chicago/Turabian StyleBrockbank, Kelvin G. M., John C. Bischof, Zhenzhen Chen, Elizabeth D. Greene, Zhe Gao, and Lia H. Campbell. 2022. "Ice Control during Cryopreservation of Heart Valves and Maintenance of Post-Warming Cell Viability" Cells 11, no. 12: 1856. https://doi.org/10.3390/cells11121856






