Evaluation of Impact of Factors Affecting CT Radiation Dose for Optimizing Patient Dose Levels
Abstract
:1. Introduction
2. Materials and Methods
2.1. CT Examinations
2.2. Patient Characteristics, Scan Parameters, and Dose Metrics
2.3. Multivariate Analysis
3. Results
3.1. Radiation Dose Metrics
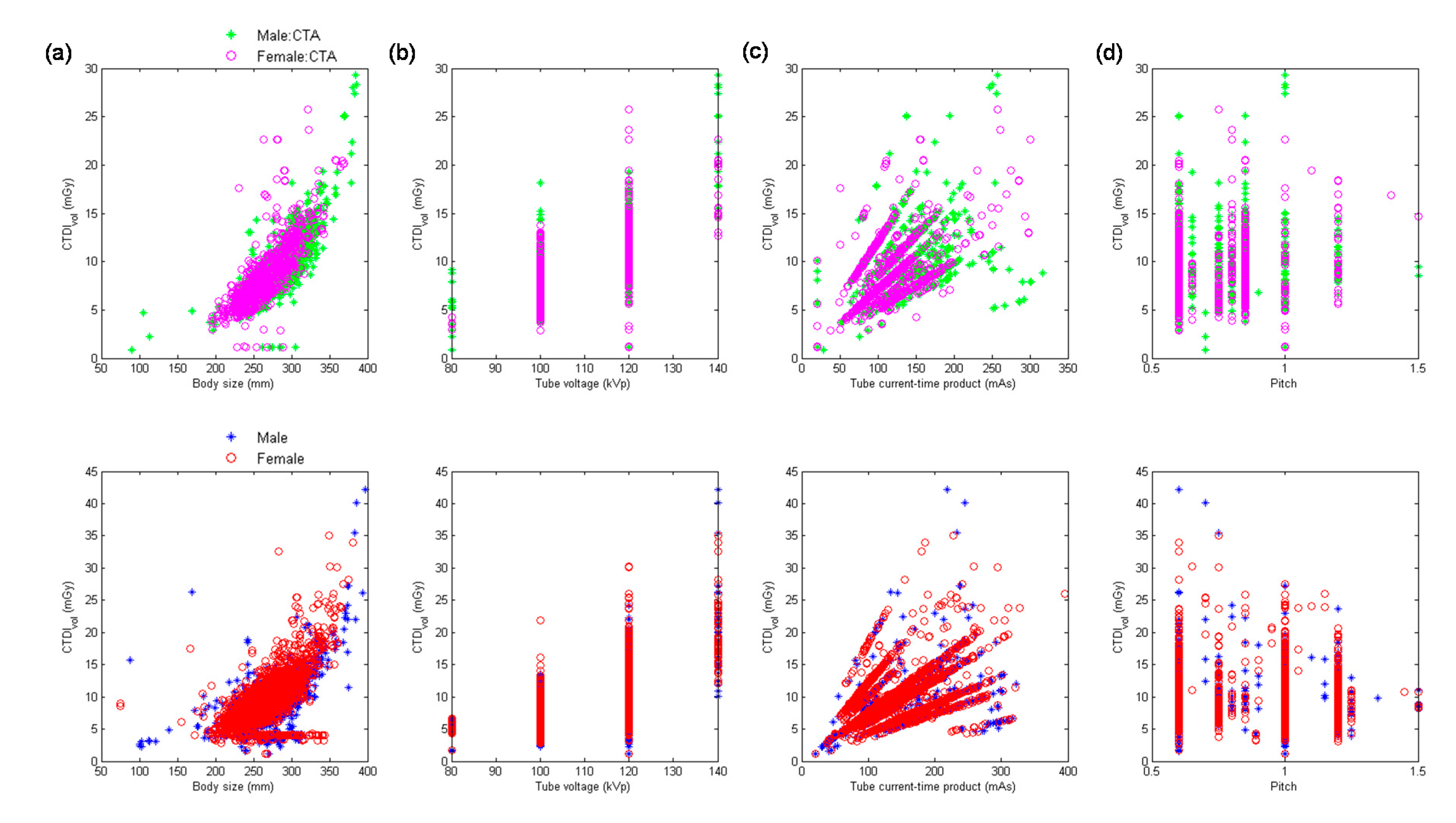
3.2. Multivariate Analysis for MDCT64
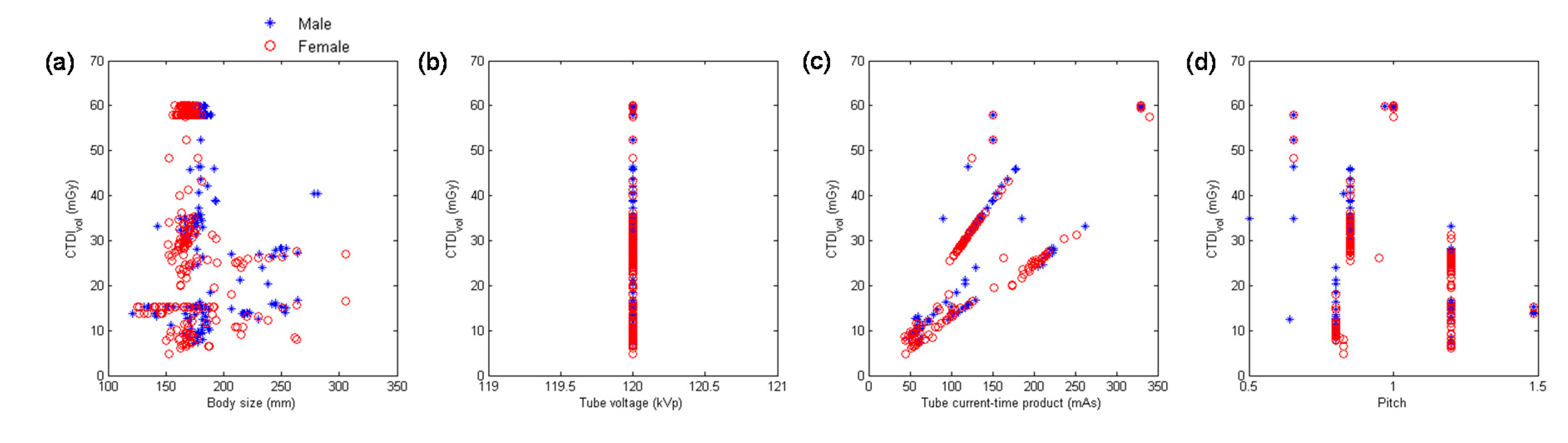
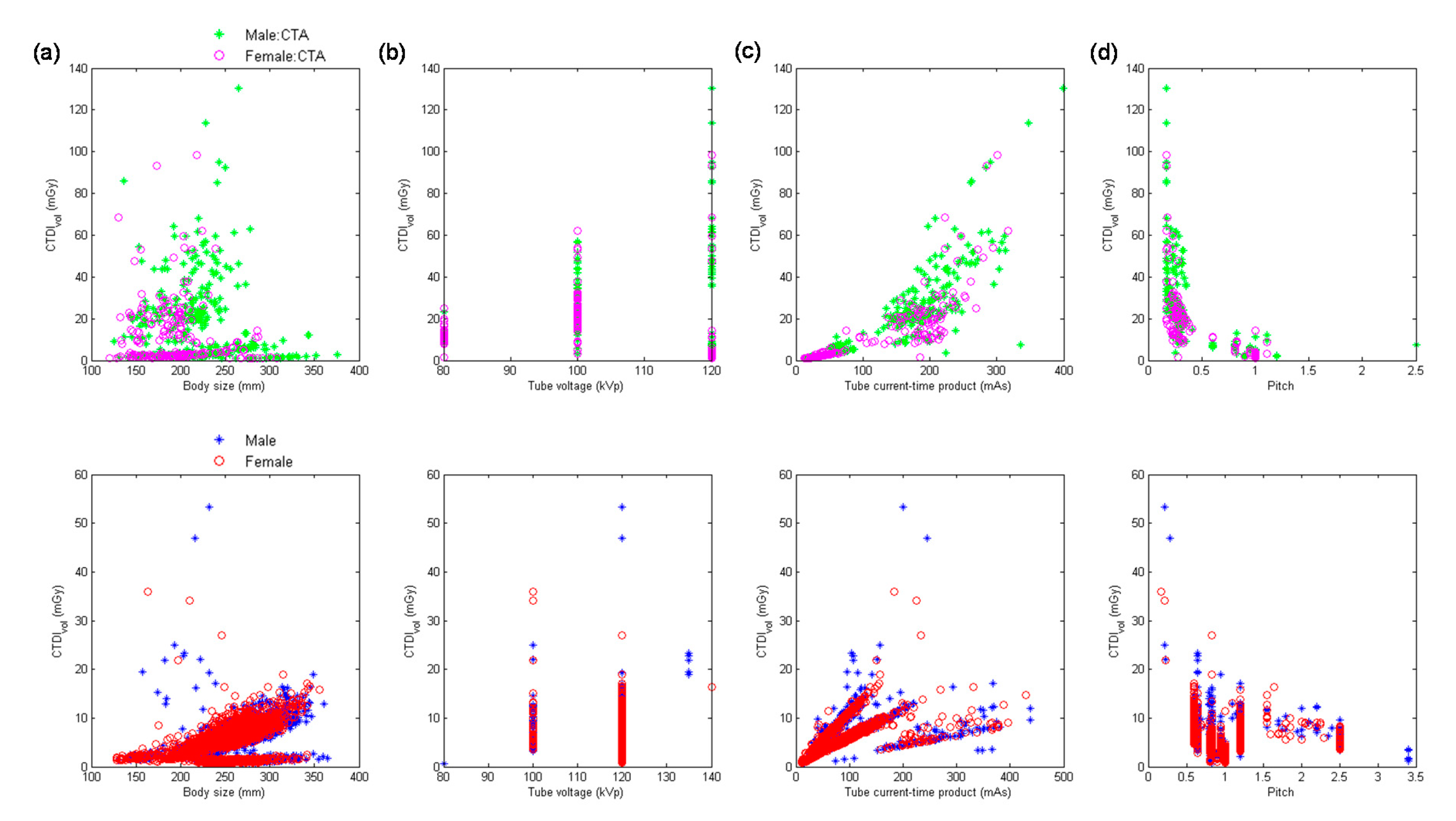
3.3. Multivariate Analysis for MDCTH
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Aroua, A.; Samara, E.T.; Bochud, F.O.; Meuli, R.; Verdun, F.R. Exposure of the Swiss population to computed tomography. BMC Med. Imaging 2013, 13, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalender, W.A. Dose in x-ray computed tomography. Phys. Med. Biol. 2014, 59, R129–R150. [Google Scholar] [CrossRef] [PubMed]
- Mettler, F.A., Jr.; Bhargavan, M.; Faulkner, K.; Gilley, D.B.; Gray, J.E.; Ibbott, G.S.; Lipoti, J.A.; Mahesh, M.; McCrohan, J.L.; Stabin, M.G.; et al. Radiologic and nuclear medicine studies in the United States and worldwide: Frequency, radiation dose, and comparison with other radiation sources—1950–2007. Radiology 2009, 253, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Goldman, L.W. Principles of CT and CT technology. J. Nucl. Med. Technol. 2007, 35, 115–128. [Google Scholar] [CrossRef] [Green Version]
- Goldman, L.W. Principles of CT: Multislice CT. J. Nucl. Med. Technol. 2008, 36, 57–68. [Google Scholar] [CrossRef] [Green Version]
- Tonkopi, E.; Duffy, S.; Abdolell, M.; Manos, D. Diagnostic Reference Levels and Monitoring Practice Can Help Reduce Patient Dose From CT Examinations. Am. J. Roentgenol. 2017, 208, 1073–1081. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Moghadassi, M.; Wilson, N.; Nelson, T.R.; Boone, J.M.; Cagnon, C.H.; Gould, R.; Hall, D.J.; Krishnam, M.; Lamba, R.; et al. Radiation Doses in Consecutive CT Examinations from Five University of California Medical Centers. Radiology 2015, 277, 134–141. [Google Scholar] [CrossRef]
- 1990 Recommendations of the International Commission on Radiological Protection. Ann. ICRP 1991, 21, 1–201.
- Diagnostic reference levels in medical imaging: Review and additional advice. Ann. ICRP 2001, 31, 33–52.
- Roch, P.; Aubert, B. French diagnostic reference levels in diagnostic radiology, computed tomography and nuclear medicine: 2004-2008 review. Radiat. Prot. Dosimetry. 2013, 154, 52–75. [Google Scholar] [CrossRef]
- Simantirakis, G.; Hourdakis, C.J.; Economides, S.; Kaisas, I.; Kalathaki, M.; Koukorava, C.; Manousaridis, G.; Pafilis, C.; Tritakis, P.; Vogiatzi, S.; et al. Diagnostic reference levels and patient doses in computed tomography examinations in Greece. Radiat. Prot. Dosimetry. 2015, 163, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Foley, S.J.; McEntee, M.F.; Rainford, L.A. Establishment of CT diagnostic reference levels in Ireland. Br. J. Radiol. 2012, 85, 1390–1397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palorini, F.; Origgi, D.; Granata, C.; Matranga, D.; Salerno, S. Adult exposures from MDCT including multiphase studies: First Italian nationwide survey. Eur. Radiol. 2014, 24, 469–483. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.C.; Han, D.K.; Nam, Y.C.; Kim, Y.M.; Yoon, J. Patient dose for computed tomography examination: Dose reference levels and effective doses based on a national survey of 2013 in Korea. Radiat. Prot. Dosimetry 2015, 164, 383–391. [Google Scholar] [CrossRef]
- Santos, J.; Foley, S.; Paulo, G.; McEntee, M.F.; Rainford, L. The establishment of computed tomography diagnostic reference levels in Portugal. Radiat. Prot. Dosimetry 2014, 158, 307–317. [Google Scholar] [CrossRef] [Green Version]
- Treier, R.; Aroua, A.; Verdun, F.R.; Samara, E.; Stuessi, A.; Trueb, P.R. Patient doses in CT examinations in Switzerland: Implementation of national diagnostic reference levels. Radiat. Prot. Dosimetry 2010, 142, 244–254. [Google Scholar] [CrossRef] [Green Version]
- Thakur, Y.; Bjarnason, T.A.; Baxter, P.; Griffith, M.; Eaton, K. Radiation Dose Survey for Common Computed Tomography Exams: 2013 British Columbia Results. Can. Assoc. Radiol. J. 2016, 67, 88–95. [Google Scholar] [CrossRef] [Green Version]
- Matsunaga, Y.; Kawaguchi, A.; Kobayashi, K.; Kinomura, Y.; Kobayashi, M.; Asada, Y.; Minami, K.; Suzuki, S.; Chida, K. Survey of volume CT dose index in Japan in 2014. Br. J. Radiol. 2015, 88, 20150219. [Google Scholar] [CrossRef] [Green Version]
- Charnock, P.; Dunn, A.F.; Moores, B.M.; Murphy, J.; Wilde, R. Establishment of a comprehensive set of regional DRLs for CT by means of electronic X-ray examination records. Radiat. Prot. Dosimetry 2015, 163, 509–520. [Google Scholar] [CrossRef]
- The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann. ICRP 2007, 37, 1–332. [CrossRef]
- MacDougall, R.D.; Kleinman, P.L.; Callahan, M.J. Size-based protocol optimization using automatic tube current modulation and automatic kV selection in computed tomography. J. Appl. Clin. Med. Phys. 2016, 17, 5756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, C.J.; Sookpeng, S. Setting up computed tomography automatic tube current modulation systems. J. Radiol. Prot. 2016, 36, R74–R95. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Bruesewitz, M.R.; Thomas, K.B.; Fletcher, J.G.; Kofler, J.M.; McCollough, C.H. Optimal tube potential for radiation dose reduction in pediatric CT: Principles, clinical implementations, and pitfalls. Radiographics 2011, 31, 835–848. [Google Scholar] [CrossRef] [PubMed]
- Zacharias, C.; Alessio, A.M.; Otto, R.K.; Iyer, R.S.; Philips, G.S.; Swanson, J.O.; Thapa, M.M. Pediatric CT: Strategies to lower radiation dose. Am. J. Roentgenol. 2013, 200, 950–956. [Google Scholar] [CrossRef] [Green Version]
- You, S.K.; Choi, Y.H.; Cheon, J.E.; Kim, W.S.; Kim, I.O.; Lee, S.M.; Cho, H.H. Effect of low tube voltage and low iodine concentration abdominal CT on image quality and radiation dose in children: Preliminary study. Abdom. Radiol. 2019, 44, 1928–1935. [Google Scholar] [CrossRef]
- Geyer, L.L.; Schoepf, U.J.; Meinel, F.G.; Nance, J.W., Jr.; Bastarrika, G.; Leipsic, J.A.; Paul, N.S.; Rengo, M.; Laghi, A.; De Cecco, C.N. State of the Art: Iterative CT Reconstruction Techniques. Radiology 2015, 276, 339–357. [Google Scholar] [CrossRef]
- Klink, T.; Obmann, V.; Heverhagen, J.; Stork, A.; Adam, G.; Begemann, P. Reducing CT radiation dose with iterative reconstruction algorithms: The influence of scan and reconstruction parameters on image quality and CTDIvol. Eur. J. Radiol. 2014, 83, 1645–1654. [Google Scholar] [CrossRef]
- Padole, A.; Ali Khawaja, R.D.; Kalra, M.K.; Singh, S. CT radiation dose and iterative reconstruction techniques. Am. J. Roentgenol. 2015, 204, W384–W392. [Google Scholar] [CrossRef]
- Shan, H.; Padole, A.; Homayounieh, F.; Kruger, U.; Khera, R.D.; Nitiwarangkul, C.; Kalra, M.K.; Wang, G. Competitive performance of a modularized deep neural network compared to commercial algorithms for low-dose CT image reconstruction. Nat. Mach. Intell. 2019, 1, 269–276. [Google Scholar] [CrossRef] [Green Version]
- Shan, H.; Zhang, Y.; Yang, Q.; Kruger, U.; Kalra, M.K.; Sun, L.; Cong, W.; Wang, G. 3-D Convolutional Encoder-Decoder Network for Low-Dose CT via Transfer Learning From a 2-D Trained Network. IEEE Trans. Med. Imaging 2018, 37, 1522–1534. [Google Scholar] [CrossRef]
- Wolterink, J.M.; Leiner, T.; Viergever, M.A.; Išgum, I. Generative Adversarial Networks for Noise Reduction in Low-Dose CT. IEEE Trans. Med. Imaging 2017, 36, 2536–2545. [Google Scholar] [CrossRef] [PubMed]
- Halliburton, S.; Arbab-Zadeh, A.; Dey, D.; Einstein, A.J.; Gentry, R.; George, R.T.; Gerber, T.; Mahesh, M.; Weigold, W.G. State-of-the-art in CT hardware and scan modes for cardiovascular CT. J. Cardiovasc. Comput. Tomogr. 2012, 6, 154–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, M.A.; Pascoal, A.; Keevil, S.F.; Lewis, C.A. Selecting a CT scanner for cardiac imaging: The heart of the matter. Br. J. Radiol. 2016, 89, 20160376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dey, D.; Slomka, P.J.; Berman, D.S. Achieving very-low-dose radiation exposure in cardiac computed tomography, single-photon emission computed tomography, and positron emission tomography. Circ. Cardiovasc. Imaging 2014, 7, 723–734. [Google Scholar] [CrossRef] [PubMed] [Green Version]





| MDCT64 | MDCTH | |||||
|---|---|---|---|---|---|---|
| Head | Chest | Abdomen | Head | Chest | Abdomen | |
| Number of Acquisition | n = 4984 | n = 3670 | n = 8243 | n = 546 | n = 5421 | n = 5283 |
| 25th percentile | 39.57 | 5.74 | 7.03 | 15.20 | 2.66 | 6.40 |
| 50th percentile | 50.82 | 7.29 | 8.72 | 34.49 | 5.74 | 7.94 |
| 75th percentile | 59.32 | 9.24 | 10.64 | 57.90 | 7.67 | 9.86 |
| Mean | 48.40 | 7.87 | 9.09 | 37.68 | 6.58 | 8.44 |
| MDCT64 | MDCTH | |||||
|---|---|---|---|---|---|---|
| Head | Chest | Abdomen | Head | Chest | Abdomen | |
| Number of Acquisition | n = 4984 | n = 3670 | n = 8243 | n = 546 | n = 5421 | n = 5283 |
| 25th percentile | 668.00 | 190.00 | 203.00 | 260.40 | 57.00 | 161.30 |
| 50th percentile | 807.00 | 261.00 | 325.50 | 711.50 | 200.20 | 248.00 |
| 75th percentile | 908.00 | 411.40 | 452.98 | 954.00 | 324.25 | 386.95 |
| Mean | 851.84 | 332.64 | 350.14 | 646.39 | 234.88 | 292.29 |
| MDCT64 | MDCTH | |||||
|---|---|---|---|---|---|---|
| Head | Chest | Abdomen | Head | Chest | Abdomen | |
| Number of Acquisition | n = 4984 | n = 3670 | n = 8243 | n = 546 | n = 5421 | n = 5283 |
| 25th percentile | 1.68 | 4.43 | 3.41 | 0.74 | 1.24 | 3.05 |
| 50th percentile | 2.07 | 5.66 | 5.87 | 2.02 | 4.59 | 4.54 |
| 75th percentile | 2.30 | 7.57 | 8.41 | 2.42 | 6.38 | 7.44 |
| Mean | 2.30 | 6.44 | 6.13 | 1.77 | 4.76 | 5.31 |
| Predictor | B | β | ta | VIF b | |
|---|---|---|---|---|---|
| Head CTA (R2 = 0.9618) | Body size | −0.0197 | −0.0276 | −1.82 | 1.08 |
| kVp2 | 0.0031 | 0.6285 | 41.66 | 1.07 | |
| mAs | 0.1484 | 0.6552 | 44.24 | 1.03 | |
| 1/pitch | 29.9818 | 0.4221 | 28.45 | 1.04 | |
| Head scan excluding CTA (R2 = 0.9068) | Body size | −0.0074 | −0.0060 | −1.35 | 1.04 |
| kVp2 | 0.0047 | 0.4438 | 83.54 | 1.45 | |
| mAs | 0.1667 | 0.8993 | 176.61 | 1.33 | |
| 1/pitch | 31.9752 | 0.5067 | 91.81 | 1.57 |
| Predictor | B | β | ta | VIF b | |
|---|---|---|---|---|---|
| Chest CTA (R2 = 0.8218) | Body size | 0.0085 | 0.0808 | 3.56 | 1.26 |
| kVp2 | 0.0010 | 0.3303 | 15.28 | 1.14 | |
| mAs | 0.0568 | 0.8709 | 37.51 | 1.31 | |
| 1/pitch | 11.5789 | 0.2922 | 13.81 | 1.09 | |
| Chest scan excluding CTA (R2 = 0.8223) | Body size | 0.0074 | 0.0651 | 7.21 | 1.48 |
| kVp2 | 0.0010 | 0.3189 | 39.41 | 1.12 | |
| mAs | 0.0609 | 0.8239 | 89.53 | 1.54 | |
| 1/pitch | 9.8958 | 0.3064 | 41.15 | 1.01 |
| Predictor | B | β | ta | VIF b | |
|---|---|---|---|---|---|
| Abdominal CTA (R2 = 0.9146) | Body size | 0.0125 | 0.1236 | 12.25 | 2.97 |
| kVp2 | 0.0010 | 0.7781 | 82.72 | 2.58 | |
| mAs | 0.0566 | 0.7250 | 68.62 | 3.26 | |
| 1/pitch | 5.0738 | 0.4329 | 45.80 | 2.61 | |
| Abdominal scan excluding CTA (R2 = 0.9096) | Body size | 0.0075 | 0.0666 | 13.12 | 1.63 |
| kVp2 | 0.0011 | 0.7576 | 147.97 | 1.66 | |
| mAs | 0.0628 | 0.9698 | 165.19 | 2.18 | |
| 1/pitch | 6.5695 | 0.6559 | 130.98 | 1.59 |
| Predictor | B | β | t a | VIF b |
|---|---|---|---|---|
| Body size | −0.0621 | 0.0758 | −1.95 | 1.02 |
| kVp2 | --- c | --- | --- | --- |
| mAs | 0.1777 | 0.6700 | 48.98 | 1.00 |
| 1/pitch | 44.0395 | 0.6851 | 46.53 | 1.03 |
| Predictor | B | β | ta | VIF b | |
|---|---|---|---|---|---|
| Chest CTA (R2 = 0.9296) | Body size | 0.0086 | 0.0214 | 2.01 | 1.12 |
| kVp2 | 0.0042 | 0.6232 | 40.62 | 2.10 | |
| mAs | 0.1444 | 0.6945 | 31.17 | 4.43 | |
| 1/pitch | 7.0585 | 0.6492 | 27.85 | 4.84 | |
| Chest scan excluding CTA (R2 = 0.7903) | Body size | 0.0143 | 0.1456 | 20.37 | 1.06 |
| kVp2 | 0.0004 | 0.0817 | 11.50 | 1.05 | |
| mAs | 0.0481 | 0.7914 | 105.02 | 1.18 | |
| 1/pitch | 5.7302 | 0.6219 | 82.83 | 1.17 |
| Predictor | B | β | ta | VIF b | |
|---|---|---|---|---|---|
| Abdominal CTA (R2 = 0.9167) | Body size | 0.0141 | 0.1817 | 13.84 | 4.49 |
| kVp2 | 0.0003 | 0.0990 | 10.99 | 2.11 | |
| mAs | 0.0932 | 0.7816 | 73.91 | 2.91 | |
| 1/pitch | 0.2939 | 0.0206 | 3.27 | 1.03 | |
| Abdominal scan excluding CTA (R2 = 0.7879) | Body size | 0.0393 | 0.3626 | 35.22 | 1.30 |
| kVp2 | 0.0008 | 0.0842 | 9.33 | 1.00 | |
| mAs | 0.0475 | 0.5910 | 56.92 | 1.33 | |
| 1/pitch | 3.8132 | 0.3130 | 33.71 | 1.06 |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, C.-C. Evaluation of Impact of Factors Affecting CT Radiation Dose for Optimizing Patient Dose Levels. Diagnostics 2020, 10, 787. https://doi.org/10.3390/diagnostics10100787
Yang C-C. Evaluation of Impact of Factors Affecting CT Radiation Dose for Optimizing Patient Dose Levels. Diagnostics. 2020; 10(10):787. https://doi.org/10.3390/diagnostics10100787
Chicago/Turabian StyleYang, Ching-Ching. 2020. "Evaluation of Impact of Factors Affecting CT Radiation Dose for Optimizing Patient Dose Levels" Diagnostics 10, no. 10: 787. https://doi.org/10.3390/diagnostics10100787





