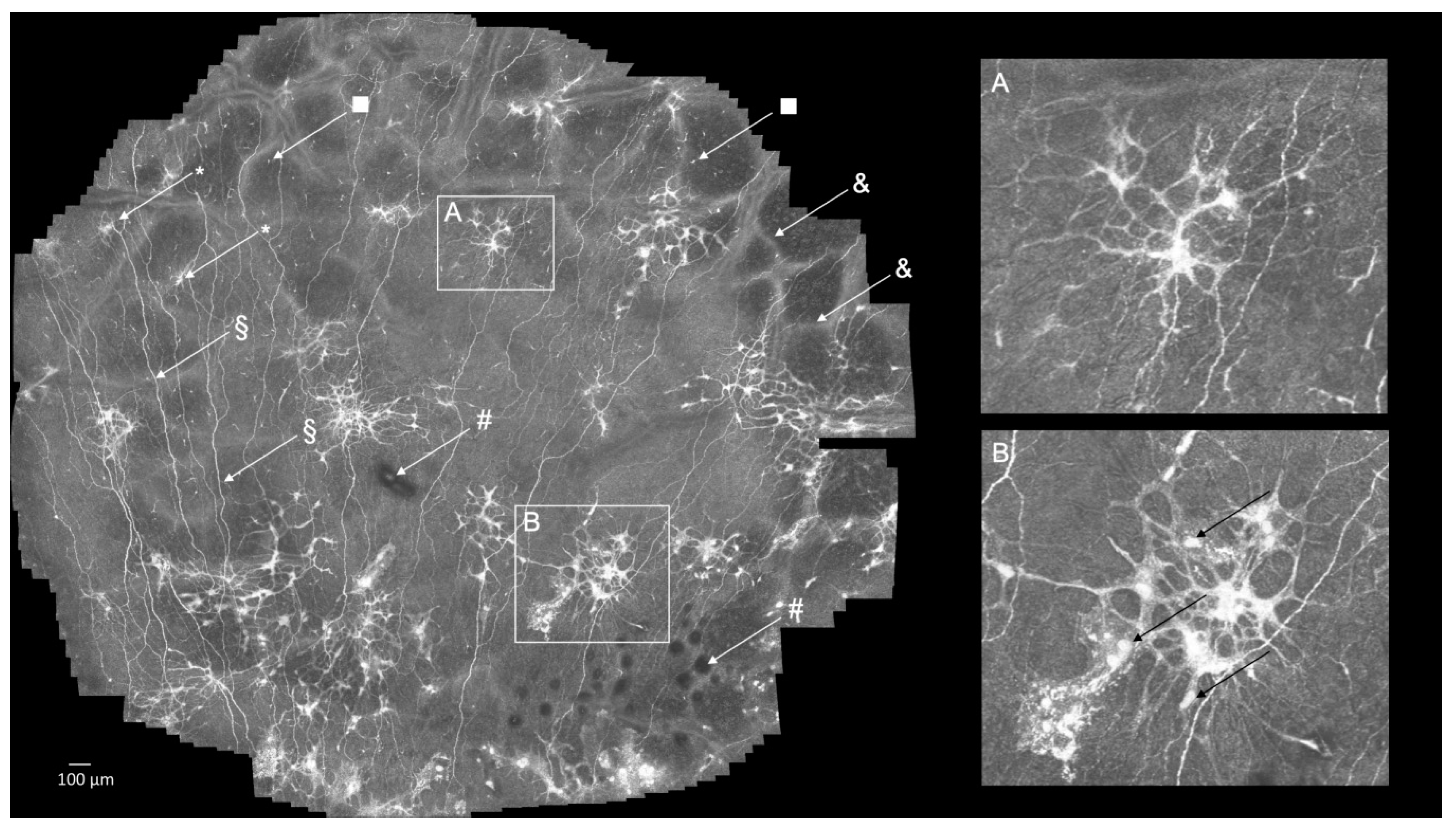
Atypical Cellular Elements of Unknown Origin in the Subbasal Nerve Plexus of a Diabetic Cornea Diagnosed by Large-Area Confocal Laser Scanning Microscopy
Abstract
:Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Levin, L.A.; Nilsson, S.F.E.; Ver-Hoeve, J.; Wu, S.M.; Kaufman, P.L. Cornea and Sclera. In Adler’s Physiology of the Eye; Kaufman, P.L., Adler, F.H., Eds.; Saunders/Elsevier: London, UK, 2011. [Google Scholar]
- Guthoff, R.F.; Baudouin, C.; Stave, J. Corneal Nerves. In Atlas of Confocal Laser Scanning In-Vivo Microscopy in Ophthalmology; Baudouin, C., Guthoff, R.F., Stave, J., Eds.; Springer: Berlin, Heidelberg, 2006; Volume 1, pp. 53–56. [Google Scholar]
- Al-Aqaba, M.A.; Dhillon, V.K.; Mohammed, I.; Said, D.G.; Dua, H.S. Corneal nerves in health and disease. Prog. Retin. Eye Res. 2019, 73, 100762. [Google Scholar] [CrossRef]
- Lagali, N.; Bourghardt, B.; Germundsson, J.; Edén, U.; Danyali, R.; Rinaldo, M.; Fagerholm, M.R.A.P. Laser-Scanning in vivo Confocal Microscopy of the Cornea: Imaging and Analysis Methods for Preclinical and Clinical Applications. In Confocal Laser Microscopy—Principles and Applications in Medicine, Biology, and the Food Sciences; Lagali, N., Ed.; IntechOpen: Rijeka, Croatia, 2013. [Google Scholar]
- Kokot, J.; Wylegała, A.; Wowra, B.; Ojcik, Ł.W.; Dobrowolski, D.; Wylegała, E. Corneal confocal sub-basal nerve plexus evaluation: A review. Acta Ophthalmol. 2018, 96, 232–242. [Google Scholar] [CrossRef] [Green Version]
- Mansoor, H.; Tan, H.C.; Lin, M.T.-Y.; Mehta, J.S.; Liu, Y.-C. Diabetic Corneal Neuropathy. J. Clin. Med. 2020, 9, 3956. [Google Scholar] [CrossRef] [PubMed]
- Koschmieder, A.; Stachs, O.; Kragl, B.; Stahnke, T.; Sterenczak, K.A.; Henze, L.; Jünemann, A.G.; Junghanss, C.; Guthoff, R.F.; Escobar, H.M. Non-invasive detection of corneal sub-basal nerve plexus changes in multiple myeloma patients by confocal laser scanning microscopy. Biosci. Rep. 2020, 40. [Google Scholar] [CrossRef] [PubMed]
- Köhler, B.; Bretthauer, G.; Guthoff, R.F.; Reichert, K.-M.; Sieber, I.; Stachs, O.; Toso, L.; Allgeier, S. Open Access EyeGuidance-a computer controlled system to guide eye movements. Curr. Dir. Biomed. Eng. 2016, 2, 433–436. [Google Scholar] [CrossRef] [Green Version]
- Allgeier, S.; Bartschat, A.; Bohn, S.; Peschel, S.; Reichert, K.-M.; Sperlich, K.; Walckling, M.; Hagenmeyer, V.; Mikut, R.; Stachs, O.; et al. 3D confocal laser-scanning microscopy for large-area imaging of the corneal subbasal nerve plexus. Sci. Rep. 2018, 8, 1–10. [Google Scholar] [CrossRef]
- Bohn, S.; Sperlich, K.; Allgeier, S.; Bartschat, A.; Prakasam, R.; Reichert, K.-M.; Stolz, H.; Guthoff, R.; Mikut, R.; Köhler, B.; et al. Cellular in vivo 3D imaging of the cornea by confocal laser scanning microscopy. Biomed. Opt. Express 2018, 9, 2511–2525. [Google Scholar] [CrossRef]
- Zhao, H.; He, Y.; Ren, Y.-R.; Chen, B.-H. Corneal alteration and pathogenesis in diabetes mellitus. Int. J. Ophthalmol. 2019, 12, 1939–1950. [Google Scholar] [CrossRef]
- Jester, J.V.; Budge, A.; Fisher, S.; Huang, J. Corneal keratocytes: Phenotypic and species differences in abundant protein expression and in vitro light-scattering. Investig. Opthalmol. Vis. Sci. 2005, 46, 2369–2378. [Google Scholar] [CrossRef] [Green Version]
- Shen, S.; Wang, F.; Fernandez, A.; Hu, W. Role of platelet-derived growth factor in type II diabetes mellitus and its com-plications. Diabetes Vasc. Dis. Res. 2020, 17, 1479164120942119. [Google Scholar] [CrossRef]
- Wilson, S.E.; Marino, G.K.; Torricelli, A.A.; Medeiros, C.S. Injury and defective regeneration of the epithelial basement membrane in corneal fibrosis: A paradigm for fibrosis in other organs? Matrix Biol. 2017, 64, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.E.; Torricelli, A.A.; Marino, G.K. Corneal epithelial basement membrane: Structure, function and regeneration. Exp. Eye Res. 2020, 194, 108002. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.E. Bowman’s layer in the cornea–structure and function and regeneration. Exp. Eye Res. 2020, 195, 108033. [Google Scholar] [CrossRef] [PubMed]
- Shetty, R.; Deshpande, K.; Deshmukh, R.; Jayadev, C.; Shroff, R. Bowman Break and Subbasal Nerve Plexus Changes in a Patient with Dry Eye Presenting with Chronic Ocular Pain and Vitamin D Deficiency. Cornea 2016, 35, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Marfurt, C.F.; Cox, J.; Deek, S.; Dvorscak, L. Anatomy of the human corneal innervation. Exp. Eye Res. 2010, 90, 478–492. [Google Scholar] [CrossRef] [PubMed]
- Guthoff, R.F.; Wienss, H.; Hahnel, C.; Wree, A. Epithelial innervation of human cornea: A three-dimensional study using confocal laser scanning fluorescence microscopy. Cornea 2005, 24, 608–613. [Google Scholar] [CrossRef]
- Müller, L.J.; Marfurt, C.F.; Kruse, F.; Tervo, T.M. Corneal nerves: Structure, contents and function. Exp. Eye Res. 2003, 76, 521–542. [Google Scholar] [CrossRef]
- Medeiros, C.S.; Santhiago, M.R. Corneal nerves anatomy, function, injury and regeneration. Exp. Eye Res. 2020, 200, 108243. [Google Scholar] [CrossRef]
- Shaheen, B.S.; Bakir, M.; Jain, S. Corneal nerves in health and disease. Surv. Ophthalmol. 2014, 59, 263–285. [Google Scholar] [CrossRef] [Green Version]
- Stepp, M.A.; Tadvalkar, G.; Hakh, R.; Pal-Ghosh, S. Corneal epithelial cells function as surrogate Schwann cells for their sensory nerves. Glia 2017, 65, 851–863. [Google Scholar] [CrossRef]
- Jessen, K.R.; Mirsky, R. The repair Schwann cell and its function in regenerating nerves. J. Physiol. 2016, 594, 3521–3531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melcangi, R.C.; Giatti, S.; Pesaresi, M.; Calabrese, D.; Mitro, N.; Caruso, D.; Garcia-Segura, L.M. Role of Neuroactive Steroids in the Peripheral Nervous System. Front. Endocrinol. 2011, 2, 104. [Google Scholar] [CrossRef] [Green Version]
- Eastlake, K.; Banerjee, P.J.; Angbohang, A.; Charteris, D.G.; Khaw, P.T.; Limb, G.A. Müller glia as an important source of cytokines and inflammatory factors present in the gliotic retina during proliferative vitreoretinopathy. Glia 2015, 64, 495–506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Hoz, R.; Rojas, B.; Ramírez, A.I.; Salazar, J.J.; Gallego, B.I.; Triviño, A.; Ramírez, J.M. Retinal Macroglial Responses in Health and Disease. BioMed Res. Int. 2016, 2016, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sterenczak, K.A.; Stachs, O.; Marfurt, C.; Matuszewska-Iwanicka, A.; Stratmann, B.; Sperlich, K.; Guthoff, R.F.; Hettlich, H.-J.; Allgeier, S.; Stahnke, T. Atypical Cellular Elements of Unknown Origin in the Subbasal Nerve Plexus of a Diabetic Cornea Diagnosed by Large-Area Confocal Laser Scanning Microscopy. Diagnostics 2021, 11, 154. https://doi.org/10.3390/diagnostics11020154
Sterenczak KA, Stachs O, Marfurt C, Matuszewska-Iwanicka A, Stratmann B, Sperlich K, Guthoff RF, Hettlich H-J, Allgeier S, Stahnke T. Atypical Cellular Elements of Unknown Origin in the Subbasal Nerve Plexus of a Diabetic Cornea Diagnosed by Large-Area Confocal Laser Scanning Microscopy. Diagnostics. 2021; 11(2):154. https://doi.org/10.3390/diagnostics11020154
Chicago/Turabian StyleSterenczak, Katharina A., Oliver Stachs, Carl Marfurt, Aleksandra Matuszewska-Iwanicka, Bernd Stratmann, Karsten Sperlich, Rudolf F. Guthoff, Hans-Joachim Hettlich, Stephan Allgeier, and Thomas Stahnke. 2021. "Atypical Cellular Elements of Unknown Origin in the Subbasal Nerve Plexus of a Diabetic Cornea Diagnosed by Large-Area Confocal Laser Scanning Microscopy" Diagnostics 11, no. 2: 154. https://doi.org/10.3390/diagnostics11020154






