Deep Learning-Based Reconstruction vs. Iterative Reconstruction for Quality of Low-Dose Head-and-Neck CT Angiography with Different Tube-Voltage Protocols in Emergency-Department Patients
Abstract
:1. Introduction
2. Materials and Methods
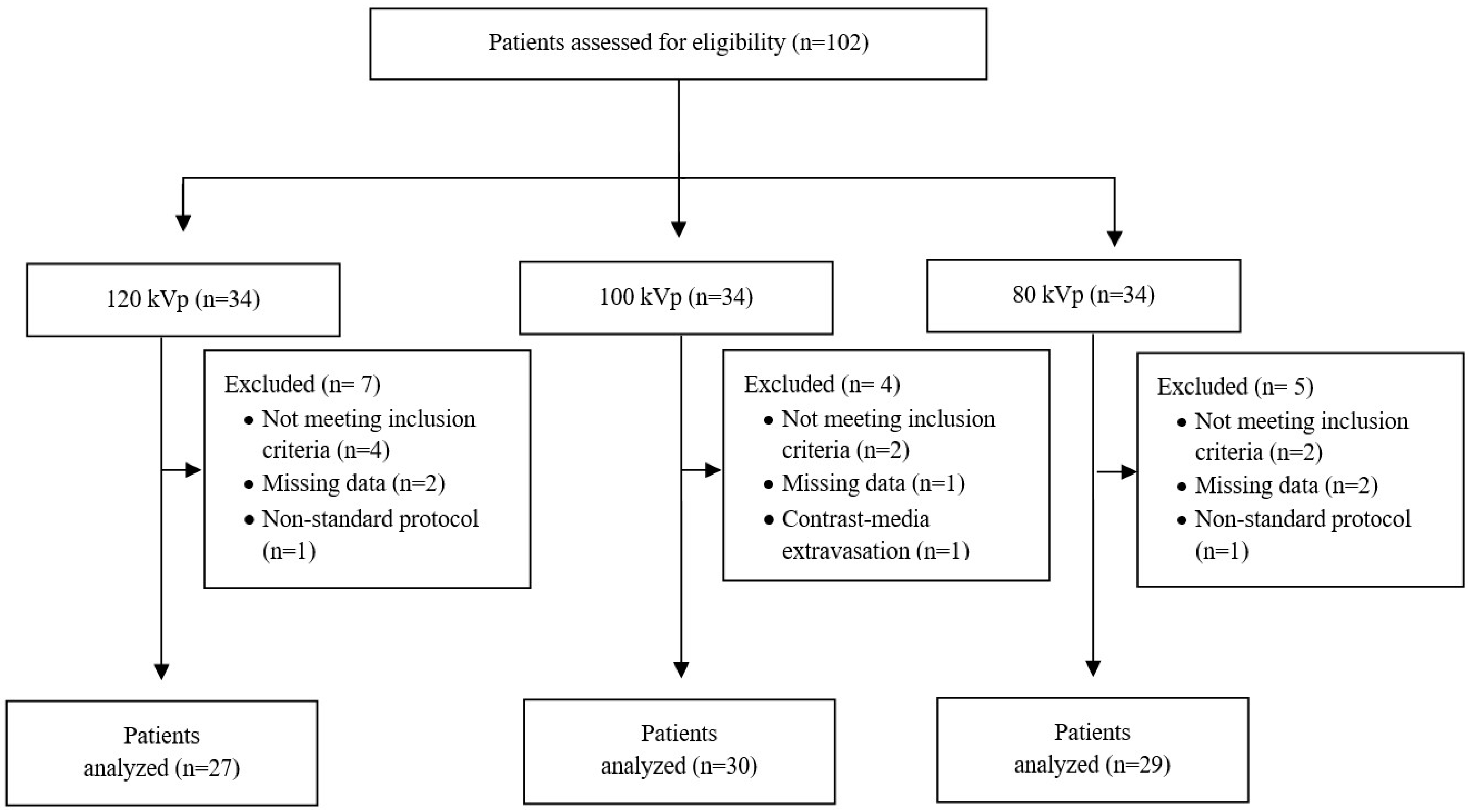
2.1. Study Population
2.2. CT Scanning Protocol
2.3. Image-Quality Assessment
2.3.1. Objective Quantitative Image-Quality Assessment
2.3.2. Subjective Qualitative Image-Quality Assessment
2.4. Radiation Dose Measurements
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Radiation Exposure
3.3. Quantitative Image Analysis
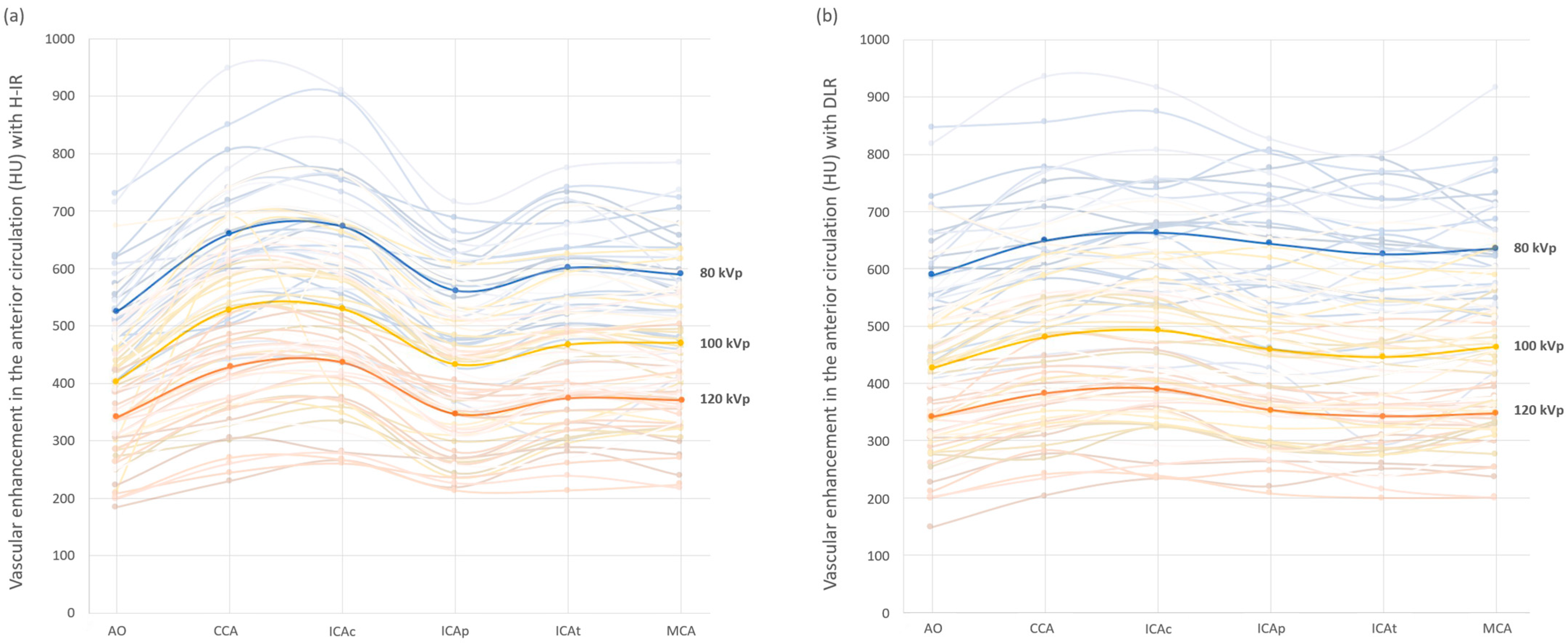
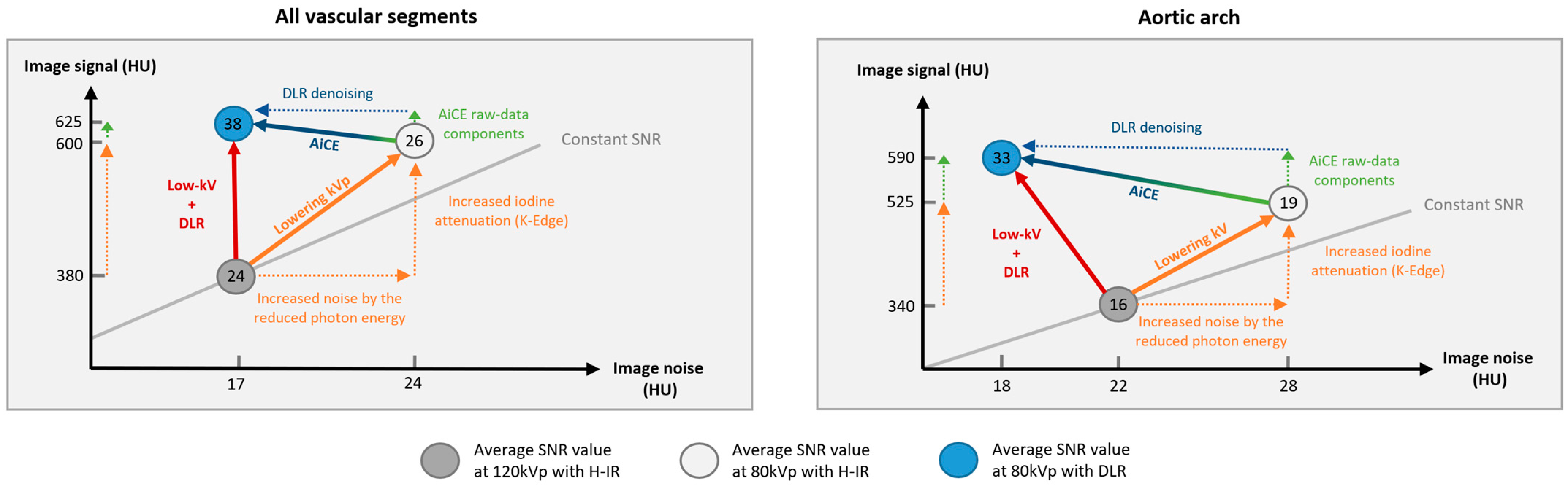
3.3.1. Image Signal Fluctuation with DLR vs. H-IR
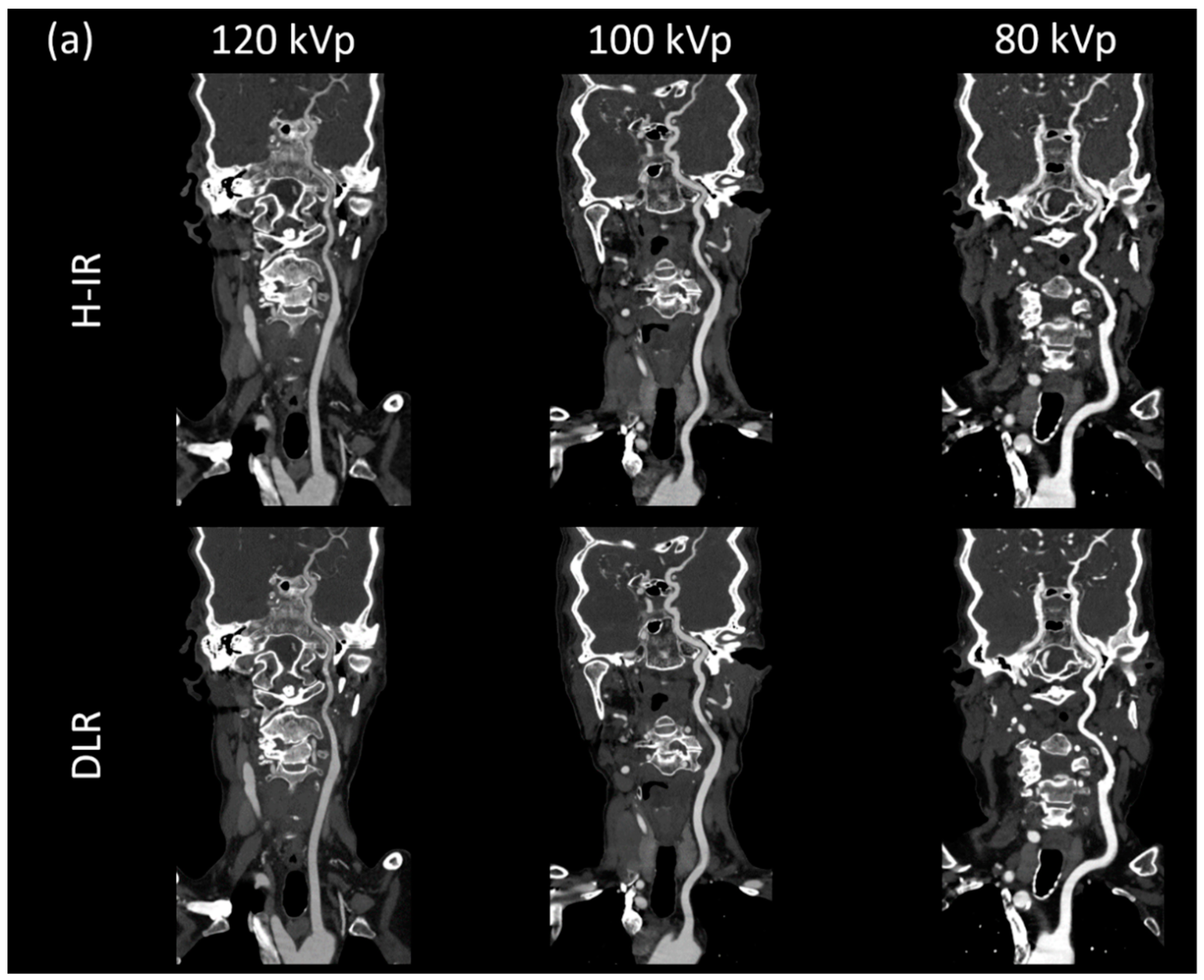
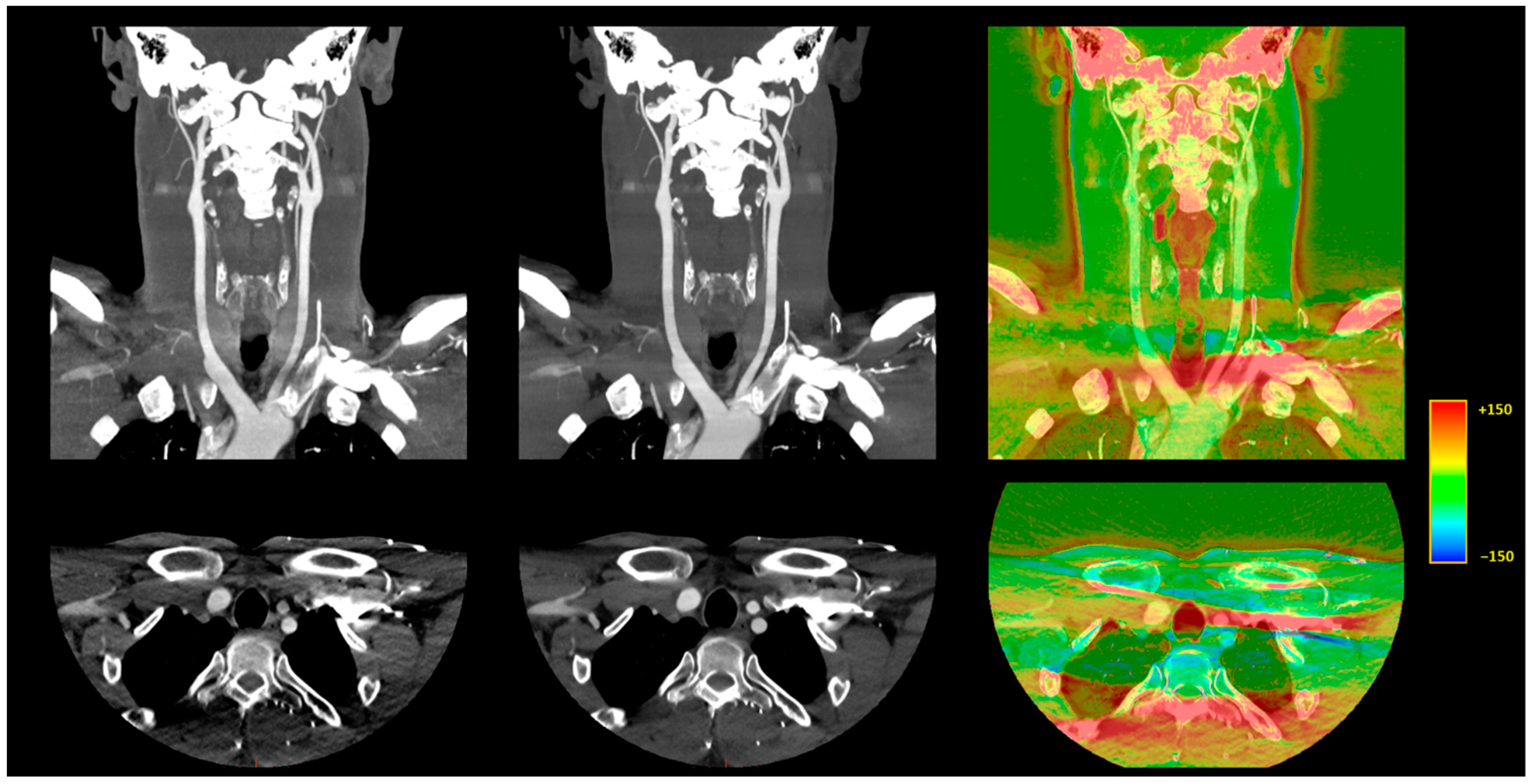
3.3.2. Comparison of the Two Reconstruction Techniques at Constant kVp Value
3.3.3. Comparison of Low kVp plus DLR vs. Standard kVp plus DLR
3.3.4. Comparison of Low kVp plus DLR vs. Standard kVp plus H-IR
3.4. Qualitative Image Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brenner, D.J.; Hall, E.J. Computed tomography--an increasing source of radiation exposure. N. Engl. J. Med. 2007, 357, 2277–2284. [Google Scholar] [CrossRef] [Green Version]
- Yamashita, K.; Higashino, K.; Hayashi, H.; Takegami, K.; Hayashi, F.; Tsuruo, Y.; Sairyo, K. Direct measurement of radiation exposure dose to individual organs during diagnostic computed tomography examination. Sci. Rep. 2021, 11, 5435. [Google Scholar] [CrossRef]
- Kuefner, M.A.; Grudzenski, S.; Schwab, S.A.; Wiederseiner, M.; Heckmann, M.; Bautz, W.; Lobrich, M.; Uder, M. DNA double-strand breaks and their repair in blood lymphocytes of patients undergoing angiographic procedures. Investig. Radiol. 2009, 44, 440–446. [Google Scholar] [CrossRef]
- Berrington de González, A. Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007. Arch. Intern. Med. 2009, 169, 2071. [Google Scholar] [CrossRef]
- Grupp, U.; Schäfer, M.-L.; Meyer, H.; Lembcke, A.; Pöllinger, A.; Wieners, G.; Renz, D.; Schwabe, P.; Streitparth, F. Reducing Radiation Dose in Emergency CT Scans While Maintaining Equal Image Quality: Just a Promise or Reality for Severely Injured Patients? Emerg. Med. Int. 2013, 2013, 1–7. [Google Scholar] [CrossRef]
- Eller, A.; Wiesmüller, M.; Wüst, W.; Heiss, R.; Kopp, M.; Saake, M.; Brand, M.; Uder, M.; May, M. Carotid CTA at the Lowest Tube Voltage (70 kV) in Comparison with Automated Tube Voltage Adaption. Am. J. Neuroradiol. 2019, 40, 1374–1382. [Google Scholar] [CrossRef]
- Beitzke, D.; Wolf, F.; Edelhauser, G.; Plank, C.; Schernthaner, R.; Weber, M.; Nolz, R.; Lammer, J.; Loewe, C. Computed tomography angiography of the carotid arteries at low kV settings: A prospective randomised trial assessing radiation dose and diagnostic confidence. Eur. Radiol. 2011, 21, 2434–2444. [Google Scholar] [CrossRef]
- Moloney, F.; Murphy, K.P.; Twomey, M.; Crush, L.; Canniffe, E.M.; McLaughlin, P.D.; Moore, N.; O’keeffe, M.; O’neill, S.; Manning, B.M.; et al. Low-Dose Carotid Computed Tomography Angiography Using Pure Iterative Reconstruction. J. Comput. Assist. Tomogr. 2016, 40, 833–839. [Google Scholar] [CrossRef]
- Kim, J.J.; Dillon, W.P.; Glastonbury, C.M.; Provenzale, J.; Wintermark, M. Sixty-Four-Section Multidetector CT Angiography of Carotid Arteries: A Systematic Analysis of Image Quality and Artifacts. Am. J. Neuroradiol. 2010, 31, 91–99. [Google Scholar] [CrossRef] [Green Version]
- McCollough, C.H.; Primak, A.N.; Braun, N.; Kofler, J.; Yu, L.; Christner, J. Strategies for Reducing Radiation Dose in CT. Radiol. Clin. N. Am. 2009, 47, 27–40. [Google Scholar] [CrossRef] [Green Version]
- Elojeimy, S.; Tipnis, S.; Huda, W. Relationship between radiographic techniques (kilovolt and milliampere-second) and CTDIVOL. Radiat. Prot. Dosim. 2010, 141, 43–49. [Google Scholar] [CrossRef]
- Van Hamersvelt, R.W.; Eijsvoogel, N.G.; Mihl, C.; de Jong, P.A.; Schilham, A.M.R.; Buls, N.; Das, M.; Leiner, T.; Willemink, M.J. Contrast agent concentration optimization in CTA using low tube voltage and dual-energy CT in multiple vendors: A phantom study. Int. J. Cardiovasc. Imaging 2018, 34, 1265–1275. [Google Scholar] [CrossRef] [Green Version]
- Kalva, S.P.; Sahani, D.V.; Hahn, P.F.; Saini, S. Using the K-edge to Improve Contrast Conspicuity and to Lower Radiation Dose With a 16-MDCT: A Phantom and Human Study. J. Comput. Assist. Tomogr. 2006, 30, 391–397. [Google Scholar] [CrossRef]
- Yu, S.; Zhang, L.; Zheng, J.; Xu, Y.; Chen, Y.; Song, Z. A comparison of adaptive iterative dose reduction 3D and filtered back projection in craniocervical CT angiography. Clin. Radiol. 2017, 72, 96.e1–96.e6. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, Y.; Che, Y.; Xu, Y.-F.; Zheng, J.; Yu, S.-J. The impact of adaptive iterative dose reduction 3D on the improvement of shoulder image quality in head and neck CTA. Curr. Med. Res. Opin. 2019, 35, 887–891. [Google Scholar] [CrossRef]
- Zhang, W.; Li, M.; Zhang, B.; Geng, H.-Y.; Liang, Y.-Q.; Xu, K.; Li, S.-B. CT Angiography of the Head-and-Neck Vessels Acquired with Low Tube Voltage, Low Iodine, and Iterative Image Reconstruction: Clinical Evaluation of Radiation Dose and Image Quality. PLoS ONE 2013, 8, e81486. [Google Scholar] [CrossRef] [Green Version]
- Gervaise, A.; Osemont, B.; Lecocq, S.; Noel, A.; Micard, E.; Felblinger, J.; Blum, A. CT image quality improvement using adaptive iterative dose reduction with wide-volume acquisition on 320-detector CT. Eur. Radiol. 2012, 22, 295–301. [Google Scholar] [CrossRef]
- Angel, E. AIDR 3D Iterative Reconstruction (White Paper). Toshiba Medical Systems; Canon Medical Systems Corporation: Tustin, CA, USA, 2012; Available online: https://us.medical.canon/download/aidr-3d-wp-aidr-3d (accessed on 10 January 2022).
- Boedeker, K. AiCE Deep Learning Reconstruction: Bringing the Power of Ultra-High Resolution CT to Routine Imaging; Canon Medical Systems Corporation: Tustin, CA, USA, 2018; Available online: https://eu.medical.canon/publication/ct/2019WP_AiCE_Deep_Learning (accessed on 10 January 2022).
- Hsieh, J.; Liu, E.; Nett, B.; Tang, J.; Thibault, J.-B.; Sahney, S. A New Era of Image Reconstruction: TrueFidelityTM. Technical White Paper on Deep Learning Image Reconstruction; 2019; Available online: https://www.gehealthcare.com/-/jssmedia/040dd213fa89463287155151fdb01922.pdf (accessed on 10 January 2022).
- Fukushima, Y.; Fushimi, Y.; Funaki, T.; Sakata, A.; Hinoda, T.; Nakajima, S.; Sakamoto, R.; Yoshida, K.; Miyamoto, S.; Nakamoto, Y. Evaluation of moyamoya disease in CT angiography using ultra-high-resolution computed tomography: Application of deep learning reconstruction. Eur. J. Radiol. 2022, 151, 110294. [Google Scholar] [CrossRef]
- Oostveen, L.J.; Meijer, F.J.A.; de Lange, F.; Smit, E.J.; Pegge, S.A.; Steens, S.C.A.; van Amerongen, M.J.; Prokop, M.; Sechopoulos, I. Deep learning–based reconstruction may improve non-contrast cerebral CT imaging compared to other current reconstruction algorithms. Eur. Radiol. 2021, 31, 5498–5506. [Google Scholar] [CrossRef]
- Yokomachi, K.; Tatsugami, F.; Higaki, T.; Kume, S.; Sakamoto, S.; Okazaki, T.; Kurisu, K.; Nakamura, Y.; Baba, Y.; Iida, M.; et al. Neointimal formation after carotid artery stenting: Phantom and clinical evaluation of model-based iterative reconstruction (MBIR). Eur. Radiol. 2019, 29, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Boas, F.E.; Fleischmann, D.C.T. Artifacts: Causes and reduction techniques. Imaging Med. 2012, 4, 229–240. [Google Scholar] [CrossRef] [Green Version]
- Moloney, F.; Kavanagh, R.G.; Ronan, N.J.; Grey, T.; Joyce, S.; Ryan, D.; Moore, N.; O’Connor, O.; Plant, B.; Maher, M. Ultra-low-dose thoracic CT with model-based iterative reconstruction (MBIR) in cystic fibrosis patients undergoing treatment with cystic fibrosis transmembrane conductance regulators (CFTR). Clin. Radiol. 2021, 76, 393.e9–393.e17. [Google Scholar] [CrossRef]
- Ippolito, D.; Maino, C.; Pecorelli, A.; Salemi, I.; Gandola, D.; Riva, L.; Franzesi, C.T.; Sironi, S. Application of low-dose CT combined with model-based iterative reconstruction algorithm in oncologic patients during follow-up: Dose reduction and image quality. Br. J. Radiol. 2021, 94, 20201223. [Google Scholar] [CrossRef]
- Lee, S.-K.; Kim, J.S.; Yoon, S.-W.; Kim, J.M. Development of CT Effective Dose Conversion Factors from Clinical CT Examinations in the Republic of Korea. Diagnostics 2020, 10, 727. [Google Scholar] [CrossRef]
- Nakamura, Y.; Higaki, T.; Tatsugami, F.; Honda, Y.; Narita, K.; Akagi, M.; Awai, K. Possibility of Deep Learning in Medical Imaging Focusing Improvement of Computed Tomography Image Quality. J. Comput. Assist. Tomogr. 2020, 44, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Akagi, M.; Nakamura, Y.; Higaki, T.; Narita, K.; Honda, Y.; Zhou, J.; Yu, Z.; Akino, N.; Awai, K. Deep learning reconstruction improves image quality of abdominal ultra-high-resolution CT. Eur. Radiol. 2019, 29, 6163–6171. [Google Scholar] [CrossRef]
- Singh, R.; Digumarthy, S.R.; Muse, V.V.; Kambadakone, A.R.; Blake, M.A.; Tabari, A.; Hoi, Y.; Akino, N.; Angel, E.; Madan, R.; et al. Image Quality and Lesion Detection on Deep Learning Reconstruction and Iterative Reconstruction of Submillisievert Chest and Abdominal CT. Am. J. Roentgenol. 2020, 214, 566–573. [Google Scholar] [CrossRef]
- Bernard, A.; Comby, P.-O.; Lemogne, B.; Haioun, K.; Ricolfi, F.; Chevallier, O.; Loffroy, R. Deep learning reconstruction versus iterative reconstruction for cardiac CT angiography in a stroke imaging protocol: Reduced radiation dose and improved image quality. Quant. Imaging Med. Surg. 2021, 11, 392–401. [Google Scholar] [CrossRef]
- Greffier, J.; Dabli, D.; Frandon, J.; Hamard, A.; Belaouni, A.; Akessoul, P.; Fuamba, Y.; Le Roy, J.; Guiu, B.; Beregi, J. Comparison of two versions of a deep learning image reconstruction algorithm on CT image quality and dose reduction: A phantom study. Med. Phys. 2021, 48, 5743–5755. [Google Scholar] [CrossRef]

| Parameters | 120 kVp | 100 kVp | 80 kVp |
|---|---|---|---|
| Acquisition mode | Helical | Helical | Helical |
| Tube voltage (kVp) | 120 | 100 | 80 |
| Tube current range (mA) | 200–700 | 200–700 | 200–700 |
| Collimation (mm) | 0.5 × 80 | 0.5 × 80 | 0.5 × 80 |
| Rotation time (s) | 0.35 | 0.35 | 0.35 |
| Field of view (mm) | 320 | 320 | 320 |
| Slice thickness (mm) | 1 | 1 | 1 |
| Interval (mm) | 0.8 | 0.8 | 0.8 |
| Pitch | 0.8 | 0.8 | 0.8 |
| Noise index | 10 | 10 | 10 |
| Grading | Confidence | Artifacts | Sharpness | Noise |
|---|---|---|---|---|
| 1 | Non-diagnostic | Extensive | Very blurry | Very high/Very coarse graininess |
| 2 | Low confidence | Significant | Blurry | High/Coarse graininess |
| 3 | Average | Average | Average | Average |
| 4 | Good confidence | Few | Sharp | Low/Fine graininess |
| 5 | Highest confidence | Very few | Very Sharp | Very low/Very fine graininess |
| Parameters | 120 kVp (N = 27) | 100 kVp (N = 30) | 80 kVp (N = 29) | 100 kVp vs. 120 kVp | 80 kVp vs. 100 kVp | 80 kVp vs. 120 kVp | |||
|---|---|---|---|---|---|---|---|---|---|
| % Change | p-Value | % Change | p-Value | % Change | p-Value | ||||
| Age | 67 ± 17.7 | 65.7 ± 19 | 63.4 ± 18.8 | NS | 0.96 | NS | 0.64 | NS | 0.67 |
| Female/male | 14/13 | 18/12 | 21/8 | NS | 0.54 | NS | 0.32 | NS | 0.12 |
| BMI, kg/m2 | 25.6 ± 4.6 | 25 ± 4.1 | 25.6 ± 3.3 | NS | 0.55 | NS | 0.48 | NS | 0.99 |
| Right/left arm injection | 14/13 | 14/16 | 14/15 | NS | 0.7 | NS | 0.9 | NS | 0.8 |
| CTDIvol, mGy | 4.8 ± 1.1 | 4 ± 1.1 | 2.3 ± 0.2 | −17% | 0.01 | −42% | <0.01 | −51% | <0.01 |
| DLP, mGy.cm | 197.1 ± 51.2 | 150.7 ± 37.8 | 90.4 ± 9.4 | −24% | <0.01 | −40% | <0.01 | −54% | <0.01 |
| ED, mSv | 1.5 ± 0.4 | 1.1 ± 0.3 | 0.68 ± 0.1 | −24% | <0.01 | −40% | <0.01 | −54% | <0.01 |
| Parameters, N | 120 kVp, 27 | 100 kVp, 30 | 80 kVp, 29 | All kVp, 86 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| H-IR | DLR | p-Value | H-IR | DLR | p-Value | H-IR | DLR | p-Value | H-IR | DLR | p-Value | |
| Close to the aorta | ||||||||||||
| Image signal (HU) | 382.8 ± 115.8 | 351.1 ± 102.4 | <0.01 | 474.3 ± 127.7 | 453.6 ± 115.4 | <0.01 | 580.9 ± 124 | 595.8 ± 122.7 | <0.01 | 475.3 ± 144.3 | 465.8 ± 150.4 | <0.01 |
| Image noise (HU) | 18.9 ± 4.7 | 12.2 ± 1.9 | <0.01 | 19.4 ± 6.1 | 12 ± 2.7 | <0.01 | 23.5 ± 6.1 | 15.6 ± 3.1 | <0.01 | 20.8 ± 5.9 | 13.4 ± 3.1 | <0.01 |
| SNR | 21.9 ± 9.9 | 29.5 ± 10.2 | <0.01 | 28.1 ± 15.8 | 39.9 ± 15.3 | <0.01 | 27 ± 11.5 | 39.7 ± 12.4 | <0.01 | 25.1 ± 12.5 | 36 ± 13.3 | <0.01 |
| CNR | 20.5 ± 8.9 | 27.5 ± 10.6 | <0.01 | 25.3 ± 8.0 | 38.3 ± 14 | <0.01 | 26.5 ± 10.1 | 39.5 ± 11.2 | <0.01 | 24 ± 10.4 | 34.9 ± 12.9 | <0.01 |
| Close to bones | ||||||||||||
| Image signal (HU) | 384.2 ± 95.2 | 371.3 ± 86.4 | <0.01 | 490.2 ± 117.4 | 486 ± 117.1 | 0.2 | 612.1 ± 114 | 647.8 ± 121.4 | <0.01 | 491.3 ± 142.2 | 501.1 ± 157.2 | <0.01 |
| Image noise (HU) | 16.9 ± 4.8 | 11.7 ± 2.7 | <0.01 | 17 ± 4.6 | 11.9 ± 3.3 | <0.01 | 22.7 ± 5.5 | 15.8 ± 3.2 | <0.01 | 19.1 ± 5.7 | 13.3 ± 3.6 | <0.01 |
| SNR | 24.2 ± 8.4 | 33.4 ± 11.3 | <0.01 | 30.7 ± 11.2 | 43.1 ± 15.3 | <0.01 | 28 ± 6.8 | 42.7 ± 12.6 | <0.01 | 27.2 ± 6.8 | 39.2 ± 13.7 | <0.01 |
| CNR | 22 ± 7.8 | 30.9 ± 11.4 | <0.01 | 27.6 ± 6.3 | 40.6 ± 11.7 | <0.01 | 27.8 ± 6.2 | 44.8 ± 11.7 | <0.01 | 40.1 ± 6.2 | 57.2 ± 29.4 | <0.01 |
| Intra-dural arteries | ||||||||||||
| Image signal (HU) | 366.7 ± 79.3 | 345.1 ± 79.1 | <0.01 | 456.4 ± 106.9 | 450.1 ± 107.4 | <0.01 | 584.7 ± 107.3 | 618.7 ± 116 | <0.01 | 470.9 ± 133.2 | 472.9 ± 152.6 | 0.3 |
| Image noise (HU) | 18 ± 5.5 | 14.2 ± 4.7 | <0.01 | 18.3 ± 5 | 13.9 ± 3.5 | <0.01 | 26.3 ± 7.3 | 20.6 ± 5.5 | <0.01 | 20.9 ± 7.2 | 16.3 ± 5.6 | <0.01 |
| SNR | 22.1 ± 8.5 | 26.2 ± 8.9 | <0.01 | 26.5 ± 8.8 | 34.5 ± 12.7 | <0.01 | 23.8 ± 7.3 | 32 ± 10.1 | <0.01 | 24.1 ± 8.3 | 30.9 ± 11.2 | <0.01 |
| CNR | 21.7 ± 6.8 | 27.1 ± 10.3 | <0.01 | 26.0 ± 6.0 | 35.9 ± 9.0 | <0.01 | 24.4 ± 5.6 | 36.0 ± 9.2 | <0.01 | 29.1 ± 11.6 | 38.8 ± 13.6 | <0.01 |
| All vascular segments | ||||||||||||
| Image signal (HU) | 382.3 ± 98.6 | 358 ± 90.2 | <0.01 | 468 ± 118.5 | 456.6 ± 113.5 | <0.01 | 597.6 ± 114.9 | 625.9 ± 118.5 | <0.01 | 484.9 ± 141.7 | 482.8 ± 154.4 | 0.16 |
| Image noise (HU) | 17.5 ± 5.2 | 12.6 ± 3.6 | <0.01 | 18.1 ± 5.4 | 12.6 ± 3.2 | <0.01 | 24.4 ± 6.7 | 17.7 ± 4.9 | <0.01 | 20 ± 6.6 | 14.3 ± 4.6 | <0.01 |
| SNR | 23.8 ± 9.7 | 30.3 ± 11.1 | <0.01 | 28.4 ± 12.5 | 38.7 ± 14.7 | <0.01 | 26.4 ± 9.1 | 37.9 ± 12.3 | <0.01 | 26.3 ± 10.7 | 35.8 ± 13.4 | <0.01 |
| CNR | 22.1 ± 7.5 | 28.9 ± 9.5 | <0.01 | 26.9 ± 9.5 | 38.1 ± 13.3 | <0.01 | 26.4 ± 7.7 | 39.6 ± 10.4 | <0.01 | 25.2 ± 8.6 | 35.7 ± 12.2 | <0.01 |
| Parameters | 120 kVp + DLR | 100 kVp + DLR | 80 kVp + DLR | 80 kVp + DLR vs. | |||
|---|---|---|---|---|---|---|---|
| 120 kVp + DLR | 100 kVp + DLR | ||||||
| % Change | p-Value | % Change | p-Value | ||||
| Close to the aorta | |||||||
| Image signal (HU) | 351.1 ± 102.4 | 453.6 ± 115.4 | 595.8 ± 122.7 | +70% | <0.01 | +31% | <0.01 |
| Image noise (HU) | 12.2 ± 1.9 | 12 ± 2.7 | 15.6 ± 3.1 | +28% | <0.01 | +30% | <0.01 |
| SNR | 29.5 ± 10.2 | 39.9 ± 15.3 | 39.7 ± 12.4 | +35% | <0.01 | +0% | 0.9 |
| CNR | 27.5 ± 10.6 | 38.3 ± 14 | 39.5 ± 11.2 | +44% | <0.01 | +3% | 0.62 |
| Close to bones | |||||||
| Image signal (HU) | 371.3 ± 86.4 | 486 ± 117.1 | 647.8 ± 121.4 | +74% | <0.01 | +33% | <0.01 |
| Image noise (HU) | 11.7 ± 2.7 | 11.9 ± 3.3 | 15.8 ± 3.2 | +35% | <0.01 | +33% | <0.01 |
| SNR | 33.4 ± 11.3 | 43.1 ± 15.3 | 42.7 ± 12.6 | +28% | <0.01 | −1% | 0.68 |
| CNR | 30.9 ± 11.4 | 40.6 ± 11.7 | 44.8 ± 11.7 | +45% | <0.01 | +10% | 0.08 |
| Intra-dural arteries | |||||||
| Image signal (HU) | 345.1 ± 79.1 | 450.1 ± 107.4 | 618.7 ± 116 | +79% | <0.01 | +37% | <0.01 |
| Image noise (HU) | 14.2 ± 4.7 | 13.9 ± 3.5 | 20.6 ± 5.5 | +45% | <0.01 | +48% | <0.01 |
| SNR | 26.2 ± 8.9 | 34.5 ± 12.7 | 32 ± 10.1 | +22% | <0.01 | −9% | 0.07 |
| CNR | 27.1 ± 10.3 | 35.9 ± 9.0 | 36.0 ± 9.2 | +33% | <0.01 | +0% | 0.95 |
| All vascular segments | |||||||
| Image signal (HU) | 358 ± 90.2 | 456.6 ± 113.5 | 625.9 ± 118.5 | +75% | <0.01 | +37% | <0.01 |
| Image noise (HU) | 12.6 ± 3.6 | 12.6 ± 3.2 | 17.7 ± 4.9 | +40% | <0.01 | +40% | <0.01 |
| SNR | 30.3 ± 11.1 | 38.7 ± 14.7 | 37.9 ± 12.3 | +25% | <0.01 | −2% | 0.4 |
| CNR | 28.9 ± 9.5 | 38.1 ± 13.3 | 39.6 ± 10.4 | +37% | <0.01 | +4% | 0.76 |
| Parameters | 120 kVp + H-IR | 100 kVp + H-IR | 80 kVp + DLR | 80 kVp + DLR vs. | |||
|---|---|---|---|---|---|---|---|
| 120 kVp + H-IR | 100 kVp + H-IR | ||||||
| % Change | p-Value | % Change | p-Value | ||||
| Close to the aorta | |||||||
| Image signal (HU) | 382.8 ± 115.8 | 474.3 ± 127.7 | 595.8 ± 122.7 | +56% | <0.01 | +26% | <0.01 |
| Image noise (HU) | 18.9 ± 4.7 | 19.4 ± 6.1 | 15.6 ± 3.1 | −17% | <0.01 | −20% | <0.01 |
| SNR | 21.9 ± 9.9 | 28.1 ± 15.8 | 39.7 ± 12.4 | +81% | <0.01 | +41% | <0.01 |
| CNR | 20.5 ± 8.9 | 25.3 ± 8.0 | 39.5 ± 11.2 | +92% | <0.01 | +56% | <0.01 |
| Close to bones | |||||||
| Image signal (HU) | 384.2 ± 95.2 | 490.2 ± 117.4 | 647.8 ± 121.4 | +69% | <0.01 | +32% | <0.01 |
| Image noise (HU) | 16.9 ± 4.8 | 17 ± 4.6 | 15.8 ± 3.2 | −7% | 0.1 | −7% | 0.05 |
| SNR | 24.2 ± 8.4 | 30.7 ± 11.2 | 42.7 ± 12.6 | +76% | <0.01 | +39% | <0.01 |
| CNR | 22 ± 7.8 | 27.6 ± 6.3 | 44.8 ± 11.7 | +104% | <0.01 | +62% | <0.01 |
| Intra-dural arteries | |||||||
| Image signal (HU) | 366.7 ± 79.3 | 456.4 ± 106.9 | 618.7 ± 116 | +69% | <0.01 | +36% | <0.01 |
| Image noise (HU) | 18 ± 5.5 | 18.3 ± 5 | 20.6 ± 5.5 | +14% | <0.01 | +13% | <0.01 |
| SNR | 22.1 ± 8.5 | 26.5 ± 8.8 | 32 ± 10.1 | +45% | <0.01 | +21% | <0.01 |
| CNR | 21.7 ± 6.8 | 26.0 ± 6.0 | 36.0 ± 9.2 | +65% | <0.01 | +38% | <0.01 |
| All vascular segments | |||||||
| Image signal (HU) | 382.3 ± 98.6 | 468 ± 118.5 | 625.9 ± 118.5 | +64% | <0.01 | +34% | <0.01 |
| Image noise (HU) | 17.5 ± 5.2 | 18.1 ± 5.4 | 17.7 ± 4.9 | +1% | 0.7 | −2% | 0.3 |
| SNR | 23.8 ± 9.7 | 28.4 ± 12.5 | 37.9 ± 12.3 | +59% | <0.01 | +33% | <0.01 |
| CNR | 22.1 ± 7.5 | 26.9 ± 9.5 | 39.6 ± 10.4 | +79% | <0.01 | +47% | <0.01 |
| Parameters | 120 kVp | 100 kVp | 80 kVp | All kVp | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| H-IR | DLR | p-Value | H-IR | DLR | p-Value | H-IR | DLR | p-Value | H-IR | DLR | p-Value | |
| Close to the aorta | ||||||||||||
| Confidence | 4.3 ± 0.7 | 4.8 ± 0.4 | <0.01 | 4.2 ± 0.6 | 4.7 ± 0.5 | <0.01 | 3.6 ± 0.8 | 4.4 ± 0.6 | <0.01 | 4 ± 0.8 | 4.6 ± 0.5 | <0.01 |
| Artifacts | 3.9 ± 1.1 | 4.1 ± 1 | <0.01 | 3.9 ± 1.1 | 4.1 ± 1 | <0.01 | 2.5 ± 1.2 | 2.9 ± 1.1 | <0.01 | 3.4 ± 1.3 | 3.7 ± 1.2 | <0.01 |
| Sharpness | 3.6 ± 0.6 | 4.8 ± 0.4 | <0.01 | 3.8 ± 0.5 | 4.8 ± 0.4 | <0.01 | 3 ± 0.7 | 4.5 ± 0.5 | <0.01 | 3.4 ± 0.7 | 4.7 ± 0.5 | <0.01 |
| Noise | 3.2 ± 0.6 | 4.5 ± 0.5 | <0.01 | 3.3 ± 0.6 | 4.8 ± 0.4 | <0.01 | 3 ± 0.5 | 4.9 ± 0.3 | <0.01 | 3.1 ± 0.6 | 4.7 ± 0.4 | <0.01 |
| Close to bones | ||||||||||||
| Confidence | 4.5 ± 0.6 | 4.9 ± 0.3 | <0.01 | 4.3 ± 0.7 | 4.9 ± 0.3 | <0.01 | 4.2 ± 0.7 | 4.9 ± 0.3 | <0.01 | 4.3 ± 0.7 | 4.9 ± 0.3 | <0.01 |
| Artifacts | 4.5 ± 0.6 | 4.9 ± 0.4 | <0.01 | 4.4 ± 0.7 | 4.9 ± 0.3 | <0.01 | 4.3 ± 0.7 | 4.9 ± 0.3 | <0.01 | 4.4 ± 0.7 | 4.9 ± 0.3 | <0.01 |
| Sharpness | 3.6 ± 0.5 | 4.7 ± 0.5 | <0.01 | 3.7 ± 0.5 | 4.8 ± 0.4 | <0.01 | 3.5 ± 0.5 | 4.9 ± 0.3 | <0.01 | 3.6 ± 0.5 | 4.8 ± 0.4 | <0.01 |
| Noise | 3.4 ± 0.6 | 4.8 ± 0.4 | <0.01 | 3.6 ± 0.5 | 4.8 ± 0.4 | <0.01 | 3.4 ± 0.5 | 4.9 ± 0.3 | <0.01 | 3.5 ± 0.5 | 4.8 ± 0.4 | <0.01 |
| Intra-dural arteries | ||||||||||||
| Confidence | 4.6 ± 0.5 | 5 ± 0.2 | <0.01 | 4.4 ± 0.6 | 4.9 ± 0.3 | <0.01 | 4.3 ± 0.7 | 4.9 ± 0.4 | <0.01 | 4.4 ± 0.6 | 4.9 ± 0.3 | <0.01 |
| Artifacts | 5 ± 0.2 | 5 ± 0.2 | - | 4.9 ± 0.4 | 5 ± 0.2 | 0.3 | 4.8 ± 0.4 | 5 ± 0.2 | 0.04 | 4.9 ± 0.3 | 5 ± 0.2 | 0.02 |
| Sharpness | 3.7 ± 0.5 | 4.7 ± 0.5 | <0.01 | 3.8 ± 0.4 | 4.8 ± 0.4 | <0.01 | 3.4 ± 0.6 | 4.8 ± 0.5 | <0.01 | 3.6 ± 0.5 | 4.8 ± 0.5 | <0.01 |
| Noise | 3.4 ± 0.6 | 4.9 ± 0.4 | <0.01 | 3.6 ± 0.5 | 4.9 ± 0.3 | <0.01 | 3.4 ± 0.5 | 5 ± 0.2 | <0.01 | 3.4 ± 0.5 | 4.9 ± 0.3 | <0.01 |
| All vascular segments | ||||||||||||
| Confidence | 4.5 ± 0.6 | 4.9 ± 0.3 | <0.01 | 4.4 ± 0.7 | 4.9 ± 0.3 | <0.01 | 4 ± 0.6 | 4.9 ± 0.3 | <0.01 | 4.3 ± 0.7 | 4.9 ± 0.3 | <0.01 |
| Artifacts | 4.3 ± 0.8 | 4.6 ± 0.5 | <0.01 | 4.1 ± 0.8 | 4.4 ± 0.7 | 0.03 | 3.5 ± 0.8 | 4.1 ± 0.8 | <0.01 | 4 ± 0.8 | 4.4 ± 0.7 | <0.01 |
| Sharpness | 3.7 ± 0.5 | 4.7 ± 0.5 | <0.01 | 3.8 ± 0.4 | 4.8 ± 0.4 | <0.01 | 3.4 ± 0.6 | 4.9 ± 0.3 | <0.01 | 3.6 ± 0.5 | 4.8 ± 0.4 | <0.01 |
| Noise | 3.4 ± 0.6 | 4.8 ± 0.4 | <0.01 | 3.6 ± 0.5 | 4.8 ± 0.4 | <0.01 | 3.3 ± 0.5 | 5 ± 0.2 | <0.01 | 3.4 ± 0.5 | 4.8 ± 0.4 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lenfant, M.; Comby, P.-O.; Guillen, K.; Galissot, F.; Haioun, K.; Thay, A.; Chevallier, O.; Ricolfi, F.; Loffroy, R. Deep Learning-Based Reconstruction vs. Iterative Reconstruction for Quality of Low-Dose Head-and-Neck CT Angiography with Different Tube-Voltage Protocols in Emergency-Department Patients. Diagnostics 2022, 12, 1287. https://doi.org/10.3390/diagnostics12051287
Lenfant M, Comby P-O, Guillen K, Galissot F, Haioun K, Thay A, Chevallier O, Ricolfi F, Loffroy R. Deep Learning-Based Reconstruction vs. Iterative Reconstruction for Quality of Low-Dose Head-and-Neck CT Angiography with Different Tube-Voltage Protocols in Emergency-Department Patients. Diagnostics. 2022; 12(5):1287. https://doi.org/10.3390/diagnostics12051287
Chicago/Turabian StyleLenfant, Marc, Pierre-Olivier Comby, Kevin Guillen, Felix Galissot, Karim Haioun, Anthony Thay, Olivier Chevallier, Frédéric Ricolfi, and Romaric Loffroy. 2022. "Deep Learning-Based Reconstruction vs. Iterative Reconstruction for Quality of Low-Dose Head-and-Neck CT Angiography with Different Tube-Voltage Protocols in Emergency-Department Patients" Diagnostics 12, no. 5: 1287. https://doi.org/10.3390/diagnostics12051287






