Improved Task Performance, Low Workload, and User-Centered Design in Medical Diagnostic Equipment Enhance Decision Confidence of Anesthesia Providers: A Meta-Analysis and a Multicenter Online Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Studies for Pooled-Data Analysis
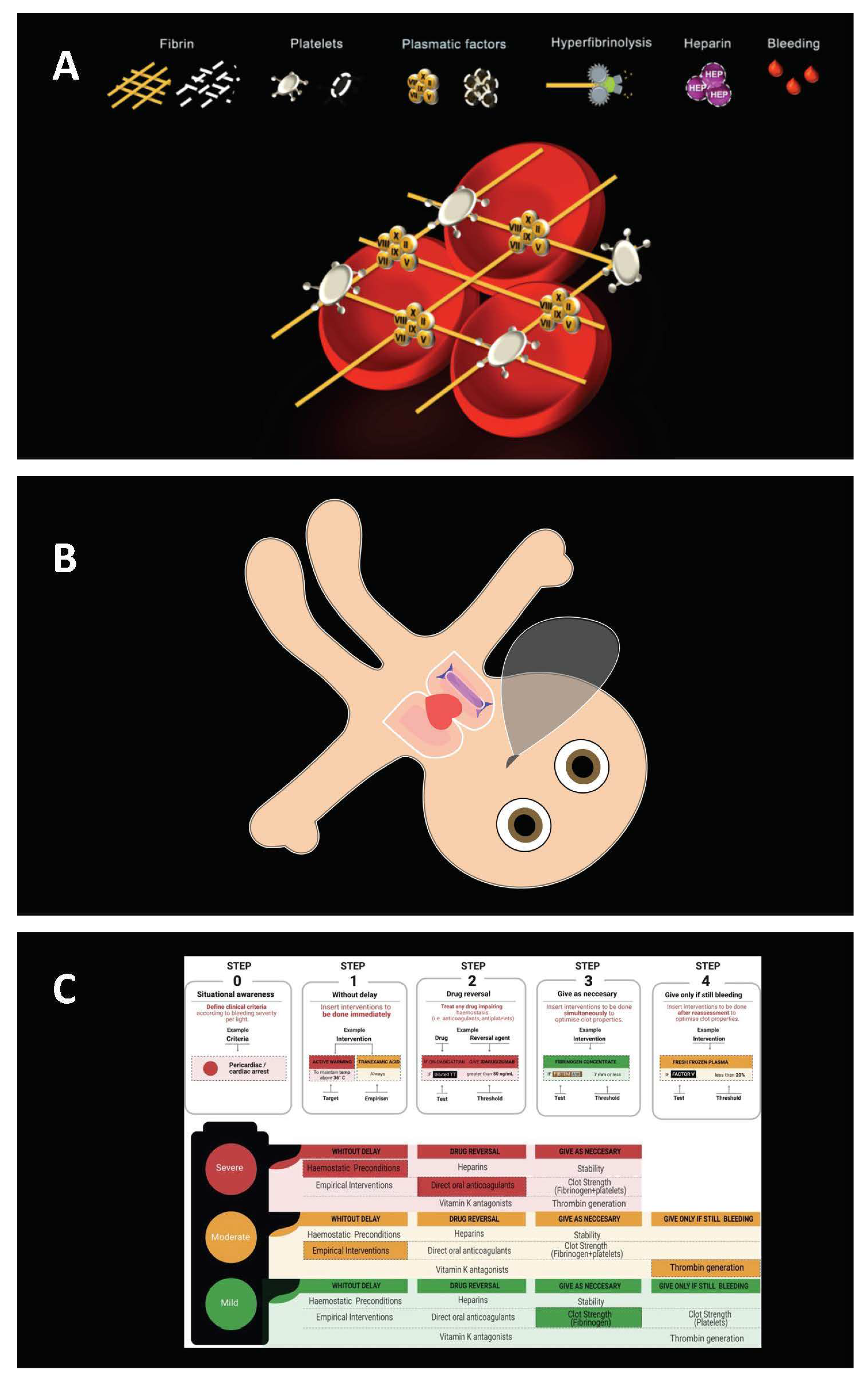
2.2. Investigated User-Centered Diagnostic Technologies
2.3. Outcomes for Pooled-Data Analysis
2.4. Online Survey
2.5. Statistical Analysis
3. Results
3.1. Decision Confidence and Task Performance
3.2. Decision Confidence and Perceived Workload
3.3. Decision Confidence and User-Centered Diagnostic Technology
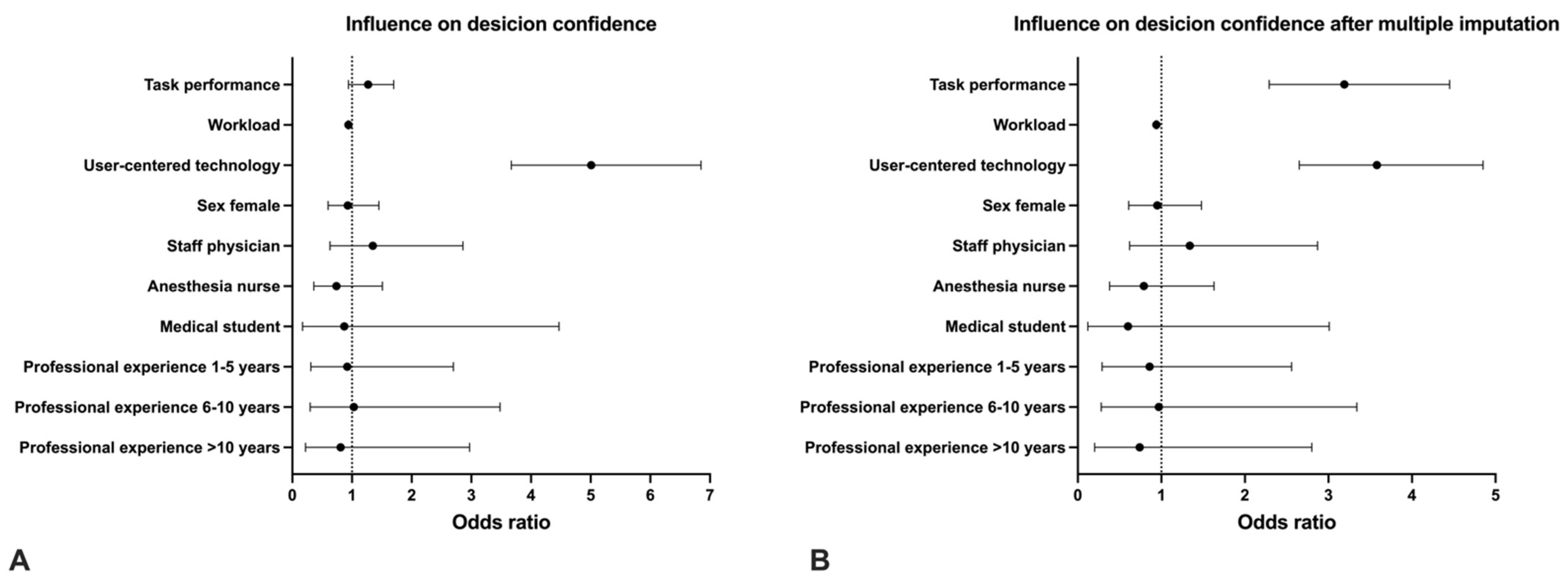
3.4. Other Potential Influencing Factors on Decision Confidence
3.5. Over- and Under-Confidence by Gender
3.6. Online Survey
4. Discussion
Strength and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pouget, A.; Drugowitsch, J.; Kepecs, A. Confidence and certainty: Distinct probabilistic quantities for different goals. Nat. Neurosci. 2016, 19, 366–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiani, R.; Shadlen, M.N. Representation of confidence associated with a decision by neurons in the parietal cortex. Science 2009, 324, 759–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daw, N.D.; Niv, Y.; Dayan, P. Uncertainty-based competition between prefrontal and dorsolateral striatal systems for behavioral control. Nat. Neurosci. 2005, 8, 1704–1711. [Google Scholar] [CrossRef] [PubMed]
- Dayan, P.; Daw, N.D. Decision theory, reinforcement learning, and the brain. Cogn. Affect. Behav. Neurosci. 2008, 8, 429–453. [Google Scholar] [CrossRef] [PubMed]
- Kepecs, A.; Uchida, N.; Zariwala, H.A.; Mainen, Z.F. Neural correlates, computation and behavioural impact of decision confidence. Nature 2008, 455, 227–231. [Google Scholar] [CrossRef]
- Meyniel, F.; Sigman, M.; Mainen, Z.F. Confidence as Bayesian Probability: From Neural Origins to Behavior. Neuron 2015, 88, 78–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, K.A.; Monuteaux, M.C.; Roussin, C.; Nagler, J. Self-Confidence in Endotracheal Intubation Among Pediatric Interns: Associations with Gender, Experience, and Performance. Acad. Pediatr. 2019, 19, 822–827. [Google Scholar] [CrossRef]
- Brinkman, D.J.; Tichelaar, J.; van Agtmael, M.A.; de Vries, T.P.; Richir, M.C. Self-reported confidence in prescribing skills correlates poorly with assessed competence in fourth-year medical students. J. Clin. Pharm. 2015, 55, 825–830. [Google Scholar] [CrossRef] [PubMed]
- Bommer, C.; Sullivan, S.; Campbell, K.; Ahola, Z.; Agarwal, S.; O’Rourke, A.; Jung, H.S.; Gibson, A.; Leverson, G.; Liepert, A.E. Pre-simulation orientation for medical trainees: An approach to decrease anxiety and improve confidence and performance. Am. J. Surg. 2018, 215, 266–271. [Google Scholar] [CrossRef]
- Rezaiefar, P.; Forse, K.; Burns, J.K.; Johnston, S.; Muggah, E.; Kendall, C.; Archibald, D. Does general experience affect self-assessment? Clin. Teach. 2019, 16, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Thompson, C.; Bland, M. The effect of clinical experience, judgment task difficulty and time pressure on nurses’ confidence calibration in a high fidelity clinical simulation. BMC Med. Inform. Decis. Mak. 2012, 12, 113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruger, J.; Dunning, D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J. Pers. Soc. Psychol. 1999, 77, 1121–1134. [Google Scholar] [CrossRef]
- Beldhuis, I.E.; Marapin, R.S.; Jiang, Y.Y.; de Souza, N.F.S.; Georgiou, A.; Kaufmann, T.; Forte, J.C.; van der Horst, I.C. Cognitive biases, environmental, patient and personal factors associated with critical care decision making: A scoping review. J. Crit. Care 2021, 64, 144–153. [Google Scholar] [CrossRef]
- Saposnik, G.; Redelmeier, D.; Ruff, C.C.; Tobler, P.N. Cognitive biases associated with medical decisions: A systematic review. BMC Med. Inform. Decis. Mak. 2016, 16, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minter, R.M.; Gruppen, L.D.; Napolitano, K.S.; Gauger, P.G. Gender differences in the self-assessment of surgical residents. Am. J. Surg. 2005, 189, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Said, S.; Gozdzik, M.; Roche, T.R.; Braun, J.; Rössler, J.; Kaserer, A.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Validation of the Raw National Aeronautics and Space Administration Task Load Index (NASA-TLX) Questionnaire to Assess Perceived Workload in Patient Monitoring Tasks: Pooled Analysis Study Using Mixed Models. J. Med. Internet Res. 2020, 22, e19472. [Google Scholar] [CrossRef] [PubMed]
- Tscholl, D.W.; Weiss, M.; Handschin, L.; Spahn, D.R.; Nöthiger, C.B. User perceptions of avatar-based patient monitoring: A mixed qualitative and quantitative study. BMC Anesth. 2018, 18, 188. [Google Scholar] [CrossRef]
- Garot, O.; Rössler, J.; Pfarr, J.; Ganter, M.T.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Avatar-based versus conventional vital sign display in a central monitor for monitoring multiple patients: A multicenter computer-based laboratory study. BMC Med. Inform. Decis. Mak. 2020, 20, 26. [Google Scholar] [CrossRef] [Green Version]
- Pfarr, J.; Ganter, M.T.; Spahn, D.R.; Noethiger, C.B.; Tscholl, D.W. Effects of a standardized distraction on caregivers’ perceptive performance with avatar-based and conventional patient monitoring: A multicenter comparative study. J. Clin. Monit. Comput. 2020, 34, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Rössler, J.; Meybohm, P.; Spahn, D.R.; Zacharowski, K.; Braun, J.; Nöthiger, C.B.; Tscholl, D.W. Improving decision making through presentation of viscoelastic tests as a 3D animated blood clot: The Visual Clot. Anaesthesia 2020, 75, 1059–1069. [Google Scholar] [CrossRef]
- Kataife, E.D.; Said, S.; Braun, J.; Roche, T.R.; Rössler, J.; Kaserer, A.; Spahn, D.R.; Mileo, F.G.; Tscholl, D.W. The Haemostasis Traffic Light, a user-centred coagulation management tool for acute bleeding situations: A simulation-based randomised dual-centre trial. Anaesthesia 2020, 76, 902–910. [Google Scholar] [CrossRef]
- Roche, T.R.; Said, S.; Braun, J.; Maas, E.J.; Machado, C.; Grande, B.; Kolbe, M.; Spahn, D.R.; Nöthiger, C.B.; Tscholl, D.W. Avatar-based patient monitoring in critical anaesthesia events: A randomised high-fidelity simulation study. Br. J. Anaesth. 2021, 126, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Said, S.; Roche, T.R.; Braun, J.; Ganter, M.T.; Meybohm, P.; Herrmann, J.; Zacharowski, K.; Raimann, F.J.; Piekarski, F.; Rivas, E.; et al. Effects of an Animated Blood Clot Technology (Visual Clot) on the Decision-Making of Users Inexperienced in Viscoelastic Testing: Multicenter Trial. J. Med. Internet Res. 2021, 23, e27124. [Google Scholar] [CrossRef]
- Roche, T.R.; Braun, J.; Ganter, M.T.; Meybohm, P.; Herrmann, J.; Zacharowski, K.; Raimann, F.J.; Piekarski, F.; Spahn, D.R.; Nöthiger, C.B.; et al. Voice alerting as a medical alarm modality for next-generation patient monitoring: A randomised international multicentre trial. Br. J. Anaesth. 2021, 127, 769–777. [Google Scholar] [CrossRef]
- Endsley, M.R. Designing for Situation Awareness, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Castellucci, C.; Braun, J.; Said, S.; Roche, T.R.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Akbas, S. Faster Time to Treatment Decision of Viscoelastic Coagulation Test Results through Improved Perception with the Animated Visual Clot: A Multicenter Comparative Eye-Tracking Study. Diagnostics 2022, 12, 1269. [Google Scholar] [CrossRef] [PubMed]
- McNeer, R.R.; Horn, D.B.; Bennett, C.L.; Edworthy, J.R.; Dudaryk, R. Auditory Icon Alarms Are More Accurately and Quickly Identified than Current Standard Melodic Alarms in a Simulated Clinical Setting. Anesthesiology 2018, 129, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Drugowitsch, J.; Moreno-Bote, R.; Pouget, A. Relation between belief and performance in perceptual decision making. PLoS ONE 2014, 9, e96511. [Google Scholar] [CrossRef]
- Grinband, J.; Hirsch, J.; Ferrera, V.P. A neural representation of categorization uncertainty in the human brain. Neuron 2006, 49, 757–763. [Google Scholar] [CrossRef] [Green Version]
- Merkle, E.C. The disutility of the hard-easy effect in choice confidence. Psychon. Bull. Rev. 2009, 16, 204–213. [Google Scholar] [CrossRef]
- Juslin, P.; Winman, A.; Olsson, H. Naive empiricism and dogmatism in confidence research: A critical examination of the hard-easy effect. Psychol. Rev. 2000, 107, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Krannich, M.; Goetz, T.; Lipnevich, A.A.; Bieg, M.; Roos, A.-L.; Becker, E.; Morger, V. Being over- or underchallenged in class: Effects on students’ career aspirations via academic self-concept and boredom. Learn. Individ. Differ. 2018, 69, 206–218. [Google Scholar] [CrossRef]
- Webster, C.S. Evidence and efficacy: Time to think beyond the traditional randomised controlled trial in patient safety studies. Br. J. Anaesth. 2019, 122, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Van der Steen, J.; Kruse, R.; Szafara, K.; Mehr, D.; van der Wal, G.; Ribbe, M.; D’Agostino, R. Benefits and pitfalls of pooling datasets from comparable observational studies: Combining US and Dutch nursing home studies. Palliat. Med. 2008, 22, 750–759. [Google Scholar] [CrossRef] [PubMed]

| Study | Location | Participants | Tasks Processed Per Participant | Assessed Confidence Levels | Endpoint of Assessed Confidence |
|---|---|---|---|---|---|
| Tscholl et al., 2018 [17] | USZ, KSW | 32 | 4 | 128 | Four nominal scale-levels |
| Garot et al., 2020 [18] | USZ, KSW | 39 | 4 | 156 | Continuous data from 0 to 100 |
| Pfarr et al., 2020 [19] | USZ, KSW | 39 | 4 | 156 | Continuous data from 0 to 100 |
| Rössler et al., 2020 [20] | USZ, UKF | 60 | 12 | 720 | Four nominal scale-levels |
| Kataife et al., 2020 [21] | USZ, BA | 84 | 6 | 504 | Four nominal scale-levels |
| Roche et al., 2021 [22] | USZ | 104 | 3 | 312 | Binary |
| Said et al., 2021 [23] | USZ, KSW, UKF, UKW, BCN | 35 | 18 | 630 | Binary |
| Roche et al., 2021 [24] | USZ, KSW, UKF, UKW | 28 | 42 | 1176 | Binary |
| Study Characteristics | Number |
|---|---|
| Studies included, | 8 |
| Study centers included | 6 |
| Decision confidence data points analyzed | 3782 |
| Missing workload data points accounted for by multiple imputation. | 1202 |
| Participant characteristics of pooled-data analysis | |
| Participants, N | 421 |
| Sex female | 197 (47%) |
| Job | |
| Resident physician | 175 (41.6%) |
| Staff physician | 125 (29.7%) |
| Anesthesia nurse | 95 (22.6%) |
| Medical student | 26 (6.1%) |
| Work experience, in years, median (IQR (range)) | 4 (1–9) |
| Participant characteristics of online survey | |
| Participants, N | 30 |
| Sex female | 12 (40%) |
| Job | |
| Resident physician | 6 (20%) |
| Staff physician | 15 (50%) |
| Anesthesia nurse | 9 (30%) |
| Age in years | 34 (30–39) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Budowski, A.D.; Bergauer, L.; Castellucci, C.; Braun, J.; Nöthiger, C.B.; Spahn, D.R.; Tscholl, D.W.; Roche, T.R. Improved Task Performance, Low Workload, and User-Centered Design in Medical Diagnostic Equipment Enhance Decision Confidence of Anesthesia Providers: A Meta-Analysis and a Multicenter Online Survey. Diagnostics 2022, 12, 1835. https://doi.org/10.3390/diagnostics12081835
Budowski AD, Bergauer L, Castellucci C, Braun J, Nöthiger CB, Spahn DR, Tscholl DW, Roche TR. Improved Task Performance, Low Workload, and User-Centered Design in Medical Diagnostic Equipment Enhance Decision Confidence of Anesthesia Providers: A Meta-Analysis and a Multicenter Online Survey. Diagnostics. 2022; 12(8):1835. https://doi.org/10.3390/diagnostics12081835
Chicago/Turabian StyleBudowski, Alexandra D., Lisa Bergauer, Clara Castellucci, Julia Braun, Christoph B. Nöthiger, Donat R. Spahn, David W. Tscholl, and Tadzio R. Roche. 2022. "Improved Task Performance, Low Workload, and User-Centered Design in Medical Diagnostic Equipment Enhance Decision Confidence of Anesthesia Providers: A Meta-Analysis and a Multicenter Online Survey" Diagnostics 12, no. 8: 1835. https://doi.org/10.3390/diagnostics12081835







